Published online Oct 16, 2021. doi: 10.4253/wjge.v13.i10.543
Peer-review started: March 30, 2021
First decision: June 25, 2021
Revised: July 10, 2021
Accepted: September 8, 2021
Article in press: September 8, 2021
Published online: October 16, 2021
Processing time: 197 Days and 17.6 Hours
Bowel perforation from biliary stent migration is a serious potential complication of biliary stents, but fortunately has an incidence of less than 1%.
We report a case of a 54-year-old Caucasian woman with a history of Human Immunodeficiency virus with acquired immunodeficiency syndrome, chronic obstructive pulmonary disease, alcoholic liver cirrhosis, portal vein thrombosis and extensive past surgical history who presented with acute abdominal pain and local peritonitis. On further evaluation she was diagnosed with small bowel perforation secondary to migrated biliary stents and underwent exploratory laparotomy with therapeutic intervention.
This case presentation reports on the unusual finding of two migrated biliary stents, with one causing perforation. In addition, we review the relevant literature on migrated stents.
Core Tip: Bowel perforation from biliary stent migration is a serious potential complication of biliary stents, but fortunately has an incidence of less than 1%. From this review of literature, we can see that most common types of migrated stents entailing bowel perforation are the plastic stents and the most common site of perforation is duodenum. A significant finding is the mortality after bowel perforation from biliary stent which is as high as 10.3%. The main treatment is surgical stent removal, but a growing body of literature shows that endoscopic removal and mucosal repair is feasible in select cases. This has still not been accomplished in the mid portion of the bowel.
- Citation: Zorbas KA, Ashmeade S, Lois W, Farkas DT. Small bowel perforation from a migrated biliary stent: A case report and review of literature. World J Gastrointest Endosc 2021; 13(10): 543-554
- URL: https://www.wjgnet.com/1948-5190/full/v13/i10/543.htm
- DOI: https://dx.doi.org/10.4253/wjge.v13.i10.543
Endoscopic biliary stents placement is a well-established therapeutic intervention in the era of modern medicine. It has been used either for temporary or permanent decompression of biliary system, for benign or malignant diseases. Biliary stents are classified by material into two categories: plastic and metallic stents, with the former being less expensive and easier to remove or change[1]. However, this technologically advanced treatment has not been free from complications. The complication rate ranges between 8% and 10% and serious common complications are stent occlusion, cholangitis, bleeding, pancreatitis, duodenal perforation and stent migration[2]. Biliary stent migration is well known with a rate of 5%-10% and can be either proximal or distal[2].
A serious potential consequence of stent migration is bowel perforation which can happen at any part of the small or large bowel, but fortunately has an incidence of less than 1%[3,4]. The majority of the case reports with bowel perforation secondary to migrated biliary stent describe duodenal or colonic perforations, with very few cases of small bowel perforations. Herein we report a case of a patient with multiple comorbidities and surgical interventions, who presents with two migrated biliary stents, one of which was perforating through the small bowel. Both stents were removed uneventfully with laparotomy and a single small bowel resection.
Diffuse abdominal pain.
We present the case of a 54-year-old Caucasian female, who presented in the emergency department of our hospital with diffuse abdominal pain for one week, which had become severe in the last day.
She initially presented in October 2019 with hyperbilirubinemia. At the time she had an ultrasound that showed gallstones as well as a dilated common bile duct of 10 mm. She underwent an magnetic resonance cholangiopacreatography (MRCP) which showed an 8mm duct, but no definite filling defects. Following this she underwent a diagnostic ERCP, at which time a distal stricture was noted, and a plastic stent [7 French (Fr) 7 cm single external and single internal flap] was placed. A second ERCP was done in February 2020, at which time choledocholithiasis was identified and felt to be the cause of the stricture. At that time a new plastic stent was placed (8.5 Fr 7 cm). The original stent was not seen at that time. In August 2020 she went for another ERCP at which time she had a normal cholangiogram, and the stent was not seen at that time. She presented to our Emergency Department in November 2020.
Her past medical history was significant for human immunodeficiency virus (HIV) infection with acquired immunodeficiency syndrome, chronic obstructive pulmonary disease, alcoholic liver cirrhosis, and portal vein thrombosis. Her past surgical history was significant for colectomy with end ileostomy for toxic megacolon from Clostridium difficile, followed later by a re-exploration and ileorectal anastomosis with proximal diverting loop ileostomy, which was still in place.
On initial evaluation the patient had temperature 98.2 °F (36.7 °C), pulse 87 per minute, blood pressure 115/83 mmHg. Her clinical examination revealed diffuse abdominal tenderness and focal peritonitis in the left lower quadrant of the abdomen.
From laboratory evaluation the patient had WBC 6.1 k/μL and total bilirubin 0.7 mg/dL.
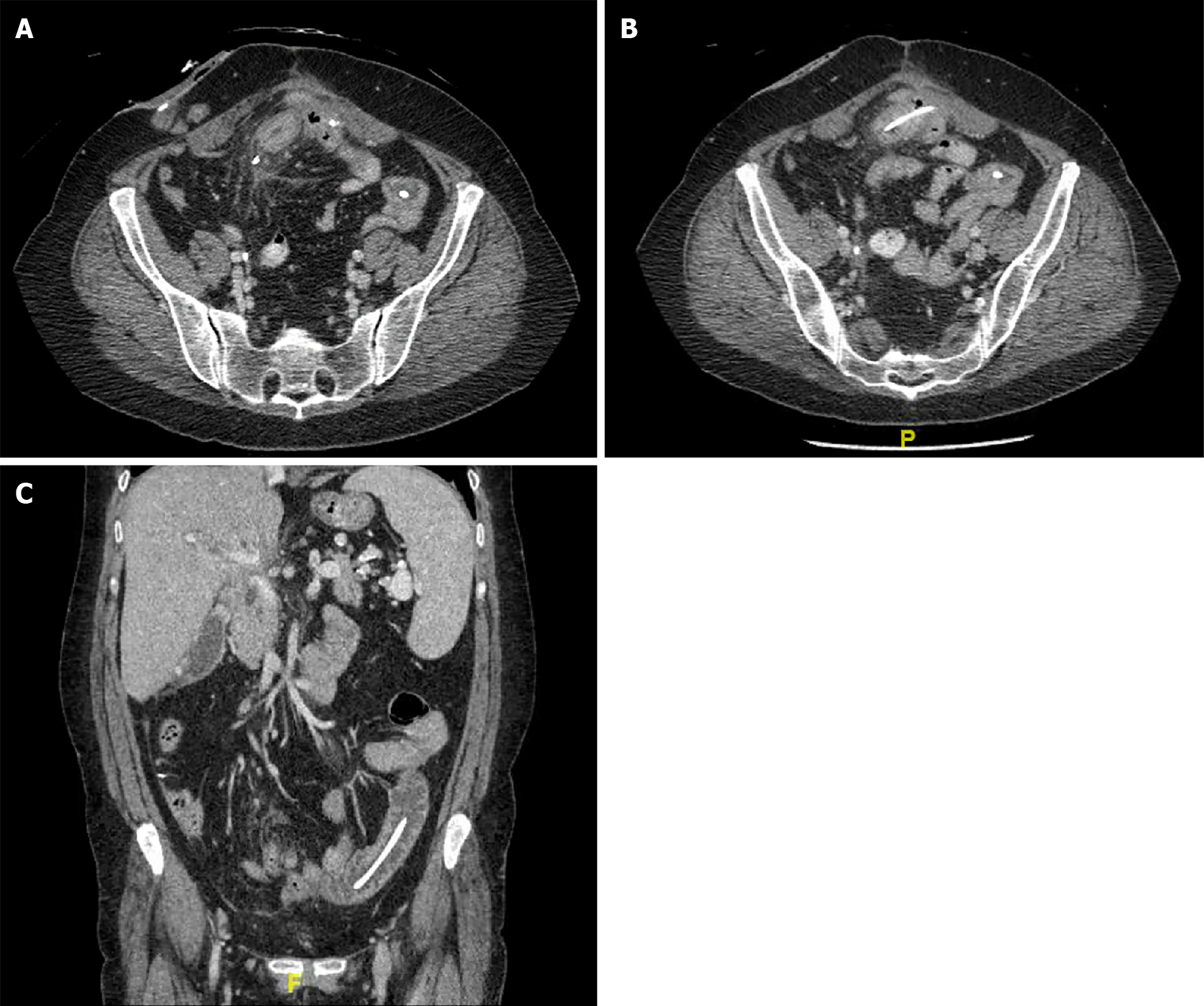
Computed tomography (CT) scan of the abdomen and pelvis with intravenous contrast showed two migrated biliary stents. The first was in an ileal loop and was perforating through the bowel wall into the mesentery (Figure 1A) and a second stent within a mid-jejunal loop (Figure 1B, C). The CT scan showed significant surrounding inflammatory phlegmon, but no free air or focal abscess was noted. After discussion with the patient, it was decided to proceed with surgical treatment of the bowel perforation and removal of both biliary stents.
The gastroenterology team was consulted, and they agreed with surgical exploration.
Small bowel perforation from a migrated biliary stent.
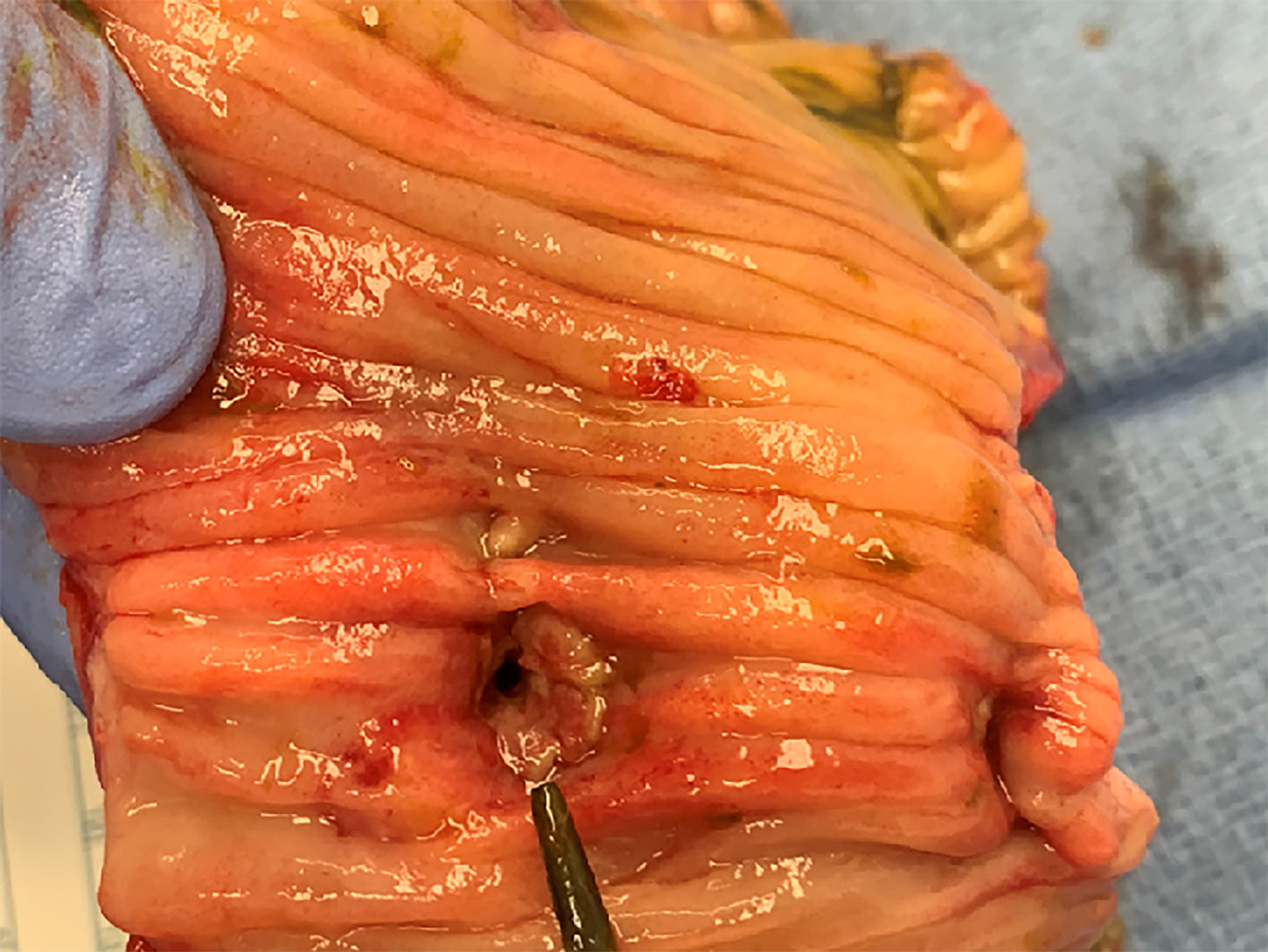
The patient underwent a laparotomy at which time extensive adhesions were noted. The bowel was cocooned in most of the abdomen, with multiple interloop adhesions, as well as adhesions to the abdominal wall. The segment of bowel with the perforation was planned for resection due to the extensive inflammation. The second stent was milked within the bowel lumen to the area of the first stent, and both stents were removed in a single resection, after which a primary anastomosis was done. As a result of the extensive adhesions, and the urgent nature of the surgery, the right upper quadrant was not explored at this time. On detailed examination of the specimen, the resected small bowel had hypertrophic changes of the luminal mucosa at the internal opening of the perforation track (Figures 2, 3).
The patient had an uneventful recovery and she was discharged eight days later to a rehab facility.
Endoscopic placement of stents in common bile duct of pancreatic duct has been an important scientific achievement of modern medicine and is a frequently employed method to relieve either benign or malignant stenosis/obstruction of biliary or pancreatic tract. It was first described in 1980 by Soehandra et al[5] as an alternative method of decompressing the biliary system for high risk or inoperable cases instead of surgical choledochoduodenostomy. After the first description of endoscopic biliary stent placement, the whole procedure and the available stents have been significantly improved and the popularity of this technique is gradually increasing as it constitutes a less morbid intervention comparing to a surgical operation[6]. Despite its clear benefit and the significant improvements in this field, there is always the risk of significant complications during or after endoscopic procedures like upper endoscopy and biliary tract cannulation.
Well described complications of biliary stent placement include stent occlusion by clogging with possible subsequent cholecystitis or cholangitis, pancreatitis from duct manipulation, hemorrhage, stent fracture and stent migration[1,2,6,7]. The total rate of biliary stent complications varies among different institutes because of different level of experience, different available equipment and different etiologic reasons for the intervention. According to Arhan et al[2] the complication rete for biliary stents is between 8% and 10%. Stent migration rate ranges from 5% to 10%, with the migration rates in plastic stents higher compared to others[2,7,8]. Biliary stent migration can be further categorized into proximal and distal migration. Distally migrated stents usually pass through the bowel without any complication[1,9]. In our case the patient had multiple previous laparotomies which led to adhesions, thereby making the bowel less mobile. This led to an increased likelihood that the stent would get impacted and not pass. In general, most institutions have policies in place to make sure all stent patients are called back for stent removal, including our own. At the last ERCP there was a normal cholangiogram and the stent was no longer in place. It was felt to have migrated, but without symptoms the impression was that it had completely passed through and eliminated from the GI tract safely. In retrospect an X-ray or further imaging at that time would have been helpful.
Bowel perforation from a migrated stent is a serious complication, which can occur in any part of the small or large bowel. The vast majority of reported cases with bowel perforation from migrated biliary stent describe either duodenal perforation or large bowel perforation, with very few cases of small bowel perforation. Most patients with perforation will present with diffuse peritonitis and signs of sepsis. In our patient, we believe the amount of infection was limited by the perforation happening slowly over time, and her septic response was also blunted by her HIV with a low CD4 count.A growing body of literature exists on this topic and different treatment approaches have been proposed. Diller et al[10] reported a case series of stent migration necessitating surgical intervention in 2003. The size of the stents varied between 7 and 14 Fr and the lengths ranged from 7 to 12 cm. Two patients had Polyurethane stents, one patient had Teflon stent placement and the other two patients had metallic stents. The diagnosis was biliary obstruction from acute pancreatitis in 4 patients and the fifth patient received a prophylactic stent after liver transplantation. One of those five patients died from postoperative respiratory failure. In this study they reported a stent migration rate of 3.7% among 987 patients. Namdar et al[1] reported a case of rectal perforation from migrated biliary stent and review of literature with 12 cases in total and 7 cases from 2000. Several studies have shown that downstream migration is more frequent in benign than in malignant biliary disease, with the possible explanation being the resolution of the stenosis after regression of inflammation[1]. In addition, they state that any migrated biliary stent should be removed immediately regardless of the patient’s clinical status[1]. An early growing body of literature describes endoscopic techniques for treatment of bowel perforation from migrated stent, but the majority focus on duodenal perforation or distal large bowel perforation. Bureau et al[11] recently described a case series of six patients with lateral duodenal wall perforation from displaced plastic biliary stent that were treated with over-the-scope clip. Given that in our case the bowel perforation was in a mid-jejunal loop, the endoscopic approach was less feasible. In addition, there was already significant inflammation seen around the bowel on CT scan, and we were concerned that an endoscopic mucosal repair would not hold. As such, we proceeded directly to surgery.
We performed a systematic review of literature from 2000 until 2020 for bowel perforation from migrated biliary stents and we found 81 cases (Table 1). Eligible articles were identified by a search of MEDLINE bibliographical database (last search: July 4th, 2021) using the following search algorithm: (("intestinal perforation"[MeSH Terms] OR ("intestinal"[All Fields] AND "perforation"[All Fields]) OR "intestinal perforation"[All Fields] OR ("bowel"[All Fields] AND "perforation"[All Fields]) OR "bowel perforation"[All Fields]) AND ("migrate"[All Fields] OR "migrated"[All Fields] OR "migrates"[All Fields] OR "migrating"[All Fields] OR "migration"[All Fields] OR "migrational"[All Fields] OR "migrations"[All Fields] OR "migrator"[All Fields] OR "migrators"[All Fields]) AND "biliary"[All Fields] AND ("stent s"[All Fields] OR "stentings"[All Fields] OR "stents"[MeSH Terms] OR "stents"[All Fields] OR "stent"[All Fields] OR "stented"[All Fields] OR "stenting"[All Fields])) AND (2000:2020[pdat]). Further search was performed in the references of related articles and relative articles with our topic were included. Manuscripts with full text available online were used and E-Videos, E-pictures and not English manuscripts were excluded. Cases were also excluded if there was not full text available online. Wang et al[3] in 2020 reported three cases of duodenal perforation due to biliary stent migration and performed a review of literature of duodenal perforation from migrated stents. In this study they reported that duodenal perforation from migrated biliary stents are mainly caused by distal stent migration[3]. Kawaguchi et al[12] studied 396 patients with bile duct stenosis between June 2003 and March 2009, retrospectively examined the frequency of stent migration and analyzed the patient factors and stent characteristics. They found that potential risk factors for stent migration are stent with large diameter, straight-type stents, stent duration > 1 mo, and common bile duct diameter > 10 mm[12].
| No | Year | Age, yr | Gender | Type of stent1 | Site of perforation | Treatment | Country | Mortality | Stent length | Stent size | Ref. |
| 1 | 2000 | 81 | M | P | SB | ST | Norway | Y | 6.5 | 10 Fr | [13] |
| 2 | 2000 | 86 | M | P | LB | ST | Norway | N | 5 | 7 Fr | [13] |
| 3 | 2000 | 74 | M | P | DU | ET | Spain | N | 15 | 10 Fr | [14] |
| 4 | 2001 | 58 | M | P | DU | ET | Italy | N | 12 | 10 Fr | [15] |
| 5 | 2001 | 43 | F | P | DU | ET | India | N | NA | 10 Fr | [16] |
| 6 | 2001 | NA | NA | P | SB | ST | United States | N | 12 | 11.5 Fr | [17] |
| 7 | 2001 | 88 | F | P | DU | ST | Germany | N | 10 | 7 Fr | [18] |
| 9 | 2001 | 31 | F | NA | BD | ST | Denmark | N | NA | NA | [19] |
| 10 | 2001 | 47 | M | P | LB | ST | Spain | N | 10 | 10 Fr | [20] |
| 11 | 2002 | 72 | F | P | SB | ST | Italy | N | NA | 12 Fr | [21] |
| 12 | 2002 | NA | NA | P | SB | ST | United States | N | 7 | 8.5 Fr | [22] |
| 13 | 2003 | 85 | F | P | LB | ST | Germany | N | NA | NA | [23] |
| 14 | 2003 | 86 | M | P | DU | ET | Italy | Y | 15 | 10 Fr | [24] |
| 15 | 2003 | 27 | F | P | SB | ST | Germany | N | 12 | 12 Fr | [10] |
| 16 | 2003 | 58 | M | P | LB | ET-ST | Germany | N | 10 | 7 Fr | [10] |
| 17 | 2003 | 60 | F | P | SB | ST | Germany | N | 12 | 14 Fr | [10] |
| 18 | 2003 | 64 | M | M | LB | ST | Germany | Y | 7 | 10 Fr | [10] |
| 19 | 2003 | 65 | M | M | NA | ST | Germany | N | 7 | 10 Fr | [10] |
| 20 | 2003 | 62 | F | P | LB | ST | Argentina | N | NA | 8 Fr | [25] |
| 21 | 2003 | 62 | F | P | SB | ST | Argentina | N | NA | 5.5/10 Fr | [25] |
| 22 | 2003 | 80 | F | P | LB | ST | Australia | N | 10 | 10 Fr | [26] |
| 23 | 2004 | 65 | F | P | LB | ST | United States | N | NA | NA | [27] |
| 24 | 2005 | 69 | M | M | DU | ST | United States | N | NA | NA | [28] |
| 25 | 2006 | 55 | M | P | DU | ET | Greece | Y | NA | NA | [29] |
| 26 | 2006 | 74 | M | P | DU | ST | India | NA | 10 | 7 Fr | [30] |
| 27 | 2006 | 54 | F | P | SB | ST | United Kingdom | N | 7 | 10 Fr | [31] |
| 28 | 2006 | 85 | M | P | DU | ST | Italy | N | 10 | 9 Fr | [32] |
| 29 | 2007 | 65 | F | P | LB | ST | Germany | N | 10 | 12 Fr | [1] |
| 30 | 2008 | 75 | M | P | DU | ST | Taiwan | N | NA | NA | [33] |
| 31 | 2008 | 52 | F | P | DU | ST | Turkey | N | 10 | 8.5 Fr | [34] |
| 32 | 2008 | 67 | M | P | DU | ST | Australia | Y | NA | 5/10 Fr | [35] |
| 33 | 2008 | 43 | M | P | DU | ET | Belgium | N | NA | NA | [36] |
| 34 | 2008 | 71 | F | P | SB | ST | Belgium | N | NA | NA | [36] |
| 35 | 2009 | 77 | M | P | LB | PI | United States | N | 12 | 10 Fr | [37] |
| 36 | 2009 | 76 | F | P | SB | PI | United States | N | NA | 10 Fr | [38] |
| 37 | 2009 | 59 | F | P | SB | ST | Turkey | N | 7 | 11 Fr | [39] |
| 38 | 2011 | 58 | M | P | DU | PI | United Kingdom | N | 10 | 8.5 Fr | [40] |
| 39 | 2011 | 65 | F | P | LB | ST | Germany | N | 10 | 10 F Fr | [41] |
| 40 | 2011 | 73 | NA | P | LB | ST | France | N | 5 | 10 Fr | [42] |
| 41 | 2011 | 75 | M | P | SB | ST | United Kingdom | N | NA | NA | [43] |
| 42 | 2011 | 70 | M | P | DU | ET | China | N | NA | 8.5 Fr | [44] |
| 43 | 2011 | 82 | F | P | LB | ET | United Kingdom | N | 7 | 7 Fr | [45] |
| 44 | 2012 | 55 | M | P | DU | ET | South Korea | N | 7/5 | 5 Fr | [46] |
| 45 | 2012 | 27 | F | P | DU | ST | United Kingdom | N | 12 | 7 Fr | [47] |
| 46 | 2012 | 87 | F | P | DU | ET | United States | N | 15 | 8.5 Fr | [48] |
| 47 | 2012 | 73 | M | P | LB | ET | Spain | N | 12 | 10 Fr | [49] |
| 48 | 2012 | 50 | NA | P | LB | ET | Belgium | N | NA | NA | [50] |
| 49 | 2013 | 51 | M | P | DU | ST | S. Arabia | N | 10 | 10 Fr | [51] |
| 50 | 2013 | 66 | M | P | LB | ET | United Kingdom | N | NA | NA | [52] |
| 51 | 2013 | 50 | M | M | SB | ST | India | N | NA | NA | [53] |
| 52 | 2014 | 67 | M | P | DU | ST | United States | Y | 12 | 10 Fr | [54] |
| 53 | 2014 | 73 | M | P | LB | ST | Australia | N | 5 | 10 Fr | [55] |
| 54 | 2014 | 66 | F | P | DU | ET | The Netherlands | N | 15 | NA | [56] |
| 55 | 2015 | 48 | M | P | DU | ET | United States | N | NA | NA | [57] |
| 56 | 2015 | NA | F | P | LB | ST | Italy | N | 12 | 12 Fr | [58] |
| 57 | 2015 | NA | F | P | LB | ET | Italy | N | 12 | 12 Fr | [58] |
| 58 | 2015 | 52 | F | P | SB | ST | Turkey | N | NA | NA | [7] |
| 59 | 2015 | NA | M | P | LB | ST | United Kingdom | Y | NA | NA | [59] |
| 60 | 2016 | 85 | F | P | SB | NA | Turkey | Y | NA | NA | [6] |
| 61 | 2017 | 75 | F | P | LB | ST | Greece | N | NA | NA | [60] |
| 62 | 2018 | 57 | M | P | DU | ET | United States | N | 15 | 8.5 Fr | [61] |
| 63 | 2018 | 79 | F | P | DU | ET | United States | N | 12+15 | 7+10 Fr | [62] |
| 64 | 2018 | 87 | M | P | DU | ST | Greece | N | 15 | 10F | [63] |
| 65 | 2018 | 20 | M | P | SB | ST | Turkey | N | NA | NA | [64] |
| 66 | 2019 | 71 | M | P | DU | ET | France | N | 12 | 8.5 Fr | [65] |
| 67 | 2019 | 50 | M | P | DU | ET | South Korea | N | 10 | 10F | [66] |
| 68 | 2019 | 78 | M | P | DU | ET | South Korea | N | 10 | 7 Fr | [66] |
| 69 | 2019 | 72 | M | P | DU | ET | South Korea | N | 12 | 10 Fr | [66] |
| 70 | 2019 | 84 | F | P | DU | ET | South Korea | N | 12 | 10 Fr | [66] |
| 71 | 2019 | 73 | F | P | DU | ET | South Korea | N | 15 | 10 Fr | [66] |
| 72 | 2019 | 63 | F | P | DU | ST | Jordan | N | 10 | 10 Fr | [67] |
| 73 | 2019 | 65 | F | P | LB | ST | Portugal | N | 5 | 10 Fr | [68] |
| 74 | 2019 | 79 | F | P | LB | ST | United States | N | 10 | 7+10 Fr | [69] |
| 75 | 2020 | 90 | F | P | SB | ST | Australia | N | 9 | 10 Fr | [70] |
| 76 | 2020 | 84 | F | P | SB | ST | Australia | N | 7 | 10 Fr | [71] |
| 77 | 2020 | 72 | M | P | DU | ET | China | N | 9 | 8.5 Fr | [3] |
| 78 | 2020 | 84 | M | P | DU | ET | China | N | 12 | 7 Fr | [3] |
| 79 | 2020 | 52 | M | P | DU | ET | China | N | 9 | 8.5 Fr | [3] |
In our review of literature (Table 1) there were 39 (50%) of male gender, 35 (44.9%) of female gender and 4 (5.1%) patients with missing data. The mean age of the total population was 66 (± 15.5) and the median 67 (IQR-56-77.5). The majority of patients had a plastic stent (93.6%). The stent length ranged from 5 to 15 cm and the stent size from 5 to 14 Fr. However, the majority of patients (50%) had a stent of 10 Fr or 12 Fr size. From the total population 35 patients (44.9%) had duodenal perforation, 23 patients (29.5%) had large bowel perforation, 18 patients (23.1%) had small bowel perforation, one patient had bile duct perforation and the last patient had no available information regarding the site of perforation. From the whole cohort, 47 patients (60.3%) had surgical intervention, 27 patients (34.6%) had endoscopic removal of the stent and 3 patients (3.8) had percutaneous removal of the stent. The overall mortality among the 54 patients was 8 patients (10.1%). Finally, the distribution of case reports was 38 (48.7%) from Europe, 21 (26.9%) from Asia-Middle East, 12 (15.4%) from the United States, 5 (6.4%) from Australia and 2 (2.6%) from South America.
From this review of literature, we can see that most common types of migrated stents entailing bowel perforation are the plastic stents and the most common site of perforation is duodenum. A significant finding is the mortality after bowel perforation from biliary stent which is as high as 10.3%. The main treatment is surgical stent removal, but a growing body of literature shows that endoscopic removal and mucosal repair is feasible in select cases. This has still not been accomplished in the mid portion of the bowel, however this might be an area for future innovation and research.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: The Society for Surgery of the Alimentary Tract.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Gkolfakis P, Kitamura K, Kumar S, Nunes TF, Zhang WH S-Editor: Ma YJ L-Editor: A P-Editor:Guo X
| 1. | Namdar T, Raffel AM, Topp SA, Namdar L, Alldinger I, Schmitt M, Knoefel WT, Eisenberger CF. Complications and treatment of migrated biliary endoprostheses: a review of the literature. World J Gastroenterol. 2007;13:5397-5399. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 58] [Cited by in RCA: 57] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 2. | Arhan M, Odemiş B, Parlak E, Ertuğrul I, Başar O. Migration of biliary plastic stents: experience of a tertiary center. Surg Endosc. 2009;23:769-775. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 75] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 3. | Wang X, Qu J, Li K. Duodenal perforations secondary to a migrated biliary plastic stent successfully treated by endoscope: case-report and review of the literature. BMC Gastroenterol. 2020;20:149. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 4. | Johanson JF, Schmalz MJ, Geenen JE. Incidence and risk factors for biliary and pancreatic stent migration. Gastrointest Endosc. 1992;38:341-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 235] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 5. | Soehendra N, Reynders-Frederix V. Palliative bile duct drainage - a new endoscopic method of introducing a transpapillary drain. Endoscopy. 1980;12:8-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 283] [Cited by in RCA: 245] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 6. | Güngör G, Okur N. A Fatal Complication: Intestinal Perforation Secondary to Migration of a Biliary Stent. Pol J Radiol. 2016;81:170-172. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Yilmaz Ö, Kiziltan R, Aydin O, Bayrak V, Kotan Ç. A Rare Complication of Biliary Stent Migration: Small Bowel Perforation in a Patient with Incisional Hernia. Case Rep Surg. 2015;2015:860286. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Görich J, Rilinger N, Krämer S, Aschoff AJ, Vogel J, Brambs HJ, Sokiranski R. Displaced metallic biliary stents: technique and rationale for interventional radiologic retrieval. AJR Am J Roentgenol. 1997;169:1529-1533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Garg K, Zagzag J, Khaykis I, Liang H. Surgical relief of small bowel obstruction by migrated biliary stent: extraction without enterotomy. JSLS. 2011;15:232-235. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Diller R, Senninger N, Kautz G, Tübergen D. Stent migration necessitating surgical intervention. Surg Endosc. 2003;17:1803-1807. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 63] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 11. | Bureau MA, Gkolfakis P, Blero D, Pezzullo M, Devière J, Lemmers A. Lateral duodenal wall perforation due to plastic biliary stent migration: a case series of endoscopic closure. Endosc Int Open. 2020;8:E573-E577. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Kawaguchi Y, Ogawa M, Kawashima Y, Mizukami H, Maruno A, Ito H, Mine T. Risk factors for proximal migration of biliary tube stents. World J Gastroenterol. 2014;20:1318-1324. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 27] [Cited by in RCA: 32] [Article Influence: 2.9] [Reference Citation Analysis (2)] |
| 13. | Størkson RH, Edwin B, Reiertsen O, Faerden AE, Sortland O, Rosseland AR. Gut perforation caused by biliary endoprosthesis. Endoscopy. 2000;32:87-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 33] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Rosés LL, Ramirez AG, Seco AL, Blanco ES, Alonso DI, Avila S, Lopez BU. Clip closure of a duodenal perforation secondary to a biliary stent. Gastrointest Endosc. 2000;51:487-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 45] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 15. | Distefano M, Bonanno G, Russo A. Biliocutaneous fistula following biliary stent migration. Endoscopy. 2001;33:97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Pathak KA, de Souza LJ. Duodenocolic fistula: an unusual sequela of stent migration. Endoscopy. 2001;33:731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 17. | Mistry BM, Memon MA, Silverman R, Burton FR, Varma CR, Solomon H, Garvin PJ. Small bowel perforation from a migrated biliary stent. Surg Endosc. 2001;15:1043. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Liebich-Bartholain L, Kleinau U, Elsbernd H, Büchsel R. Biliary pneumonitis after proximal stent migration. Gastrointest Endosc. 2001;54:382-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 19. | Jendresen MB, Svendsen LB. Proximal displacement of biliary stent with distal perforation and impaction in the pancreas. Endoscopy. 2001;33:195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 21] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 20. | Figueiras RG, Echart MO, Figueiras AG, González GP. Colocutaneous fistula relating to the migration of a biliary stent. Eur J Gastroenterol Hepatol. 2001;13:1251-1253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 21. | Fiori E, Mazzoni G, Galati G, Lutzu SE, Cesare A, Bononi M, Bolognese A, Tocchi A. Unusual breakage of a plastic biliary endoprosthesis causing an enterocutaneous fistula. Surg Endosc. 2002;16:870. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 22. | Levey JM. Intestinal perforation in a parastomal hernia by a migrated plastic biliary stent. Surg Endosc. 2002;16:1636-1637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 21] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 23. | Wilhelm A, Langer C, Zoeller G, Nustede R, Becker H. Complex colovesicular fistula: A severe complication caused by biliary stent migration. Gastrointest Endosc. 2003;57:124-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 29] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 24. | Basile A, Macri' A, Lamberto S, Caloggero S, Versaci A, Famulari C. Duodenoscrotal fistula secondary to retroperitoneal migration of an endoscopically placed plastic biliary stent. Gastrointest Endosc. 2003;57:136-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 25. | Cerisoli C, Diez J, Giménez M, Oria M, Pardo R, Pujato M. Implantation of migrated biliary stents in the digestive tract. HPB (Oxford). 2003;5:180-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 26. | Elliott M, Boland S. Sigmoid colon perforation following a migrated biliary stent. ANZ J Surg. 2003;73:669-670. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 27. | Blake AM, Monga N, Dunn EM. Biliary stent causing colovaginal fistula: case report. JSLS. 2004;8:73-75. [PubMed] |
| 28. | Miller G, Yim D, Macari M, Harris M, Shamamian P. Retroperitoneal perforation of the duodenum from biliary stent erosion. Curr Surg. 2005;62:512-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 29. | Paikos D, Gatopoulou A, Moschos J, Soufleris K, Tarpagos A, Katsos I. Migrated biliary stent predisposing to fatal ERCP-related perforation of the duodenum. J Gastrointestin Liver Dis. 2006;15:387-388. [PubMed] |
| 30. | Bharathi RS, Rao PP, Ghosh K. Intra-peritoneal duodenal perforation caused by delayed migration of endobiliary stent: a case report. Int J Surg. 2008;6:478-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 31. | Akimboye F, Lloyd T, Hobson S, Garcea G. Migration of endoscopic biliary stent and small bowel perforation within an incisional hernia. Surg Laparosc Endosc Percutan Tech. 2006;16:39-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 32. | Lanteri R, Naso P, Rapisarda C, Santangelo M, Di Cataldo A, Licata A. Jejunal perforation for biliary stent dislocation. Am J Gastroenterol. 2006;101:908-909. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 33. | Hsu YC, Wu YM, Wang HP. Education of imaging. Hepatobiliary and pancreatic: biliary stent causing imminent duodenal perforation. J Gastroenterol Hepatol. 2008;23:817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 34. | Yaprak M, Mesci A, Colak T, Yildirim B. Biliary stent migration with duodenal perforation. Eurasian J Med. 2008;40:154-156. [PubMed] |
| 35. | Lo CH, Chung S, Bohmer RD. A devastating complication: duodenal perforation due to biliary stent migration. Surg Laparosc Endosc Percutan Tech. 2008;18:608-610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 36. | Seerden TC, Moreels TG, Salgado RA, Francque SM, Michielsen PP, Parizel PM, Pelckmans PA. Intestinal bowel perforation and bacterial peritonitis secondary to migrated biliary and pancreatic stents. Endoscopy. 2008;40 Suppl 2:E25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 37. | Brinkley M, Wible BC, Hong K, Georgiades C. Colonic perforation by a percutaneously displaced biliary stent: report of a case and a review of current practice. J Vasc Interv Radiol. 2009;20:680-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 38. | Culnan DM, Cicuto BJ, Singh H, Cherry RA. Percutaneous retrieval of a biliary stent after migration and ileal perforation. World J Emerg Surg. 2009;4:6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 39. | Akbulut S, Cakabay B, Ozmen CA, Sezgin A, Sevinc MM. An unusual cause of ileal perforation: report of a case and literature review. World J Gastroenterol. 2009;15:2672-2674. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 19] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 40. | Papadopoulou I, Fotiadis NI, Ahmed I, Thurley P, Hutchins RR, Fotheringham T. Perforation and abscess formation after radiological placement of a retrievable plastic biliary stent. J Med Case Rep. 2011;5:103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 41. | Lankisch TO, Alten TA, Lehner F, Knitsch W. Biliary stent migration with colonic perforation: a very rare complication and the lesson that should be learned from it. Gastrointest Endosc. 2011;74:924-5; discussion 925. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 42. | Malgras B, Pierret C, Tourtier JP, Olagui G, Nizou C, Duverger V. Double Sigmoid colon perforation due to migration of a biliary stent. J Visc Sur. 148:e397-e399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 43. | Abela JE, Anderson JE, Whalen HR, Mitchell KG. Endo-biliary stents for benign disease: not always benign after all! Clin Pract. 2011;1:e102. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 44. | Lin H, Li ZS, Zhan XB. Asymptomatic duodenal perforation from obstructed and migrated biliary stent. Endoscopy. 2011;43 Suppl 2 UCTN:E40-E41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 45. | Jafferbhoy SF, Scriven P, Bannister J, Shiwani MH, Hurlstone P. Endoscopic management of migrated biliary stent causing sigmoid perforation. BMJ Case Rep. 2011;2011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 46. | Oh HC, Kim SW, Do JH, Kim G. Duodenal perforation caused by a cutting-induced sharp-edged plastic stent (with video). Gastrointest Endosc. 2012;76:1050; discussion 1050-1050; discussion 1051. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 47. | Smart P, Keenan D, Campbell W, Morris-Stiff G. Duodenal perforation secondary to migration of endobiliary prosthesis. BMJ Case Rep. 2012;2012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 48. | O'Connor R, Agrawal S, Aoun E, Kulkarni A. Biliary stent migration presenting with leg pain. BMJ Case Rep. 2012;2012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 49. | Alcaide N, Lorenzo-Pelayo S, Herranz-Bachiller MT, de la Serna-Higuera C, Barrio J, Perez-Miranda M. Sigmoid perforation caused by a migrated biliary stent and closed with clips. Endoscopy. 2012;44 Suppl 2 UCTN:E274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 50. | Depuydt P, Aerts R, Van Steenbergen W, Verslype C, Laleman W, Cassiman D, Nevens F, Pirenne J, Monbaliu D. An unusual case of rectal perforation after liver transplantation. Acta Chir Belg. 2012;112:232-233. [PubMed] |
| 51. | Issa H, Nahawi M, Bseiso B, Al-Salem A. Migration of a biliary stent causing duodenal perforation and biliary peritonitis. World J Gastrointest Endosc. 2013;5:523-526. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 17] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 52. | Jones M, George B, Jameson J, Garcea G. Biliary stent migration causing perforation of the caecum and chronic abdominal pain. BMJ Case Rep. 2013;2013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (1)] |
| 53. | Saravanan MN, Mathai V, Kapoor D, Singh B. Fractured metallic biliary stent causing obstruction and jejunal perforation. Asian J Endosc Surg. 2013;6:234-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 54. | El Zein MH, Kumbhari V, Tieu A, Saxena P, Messallam AA, Azola A, Li Z, Weiss M, Khashab MA. Duodenal perforation as a consequence of biliary stent migration can occur regardless of stent type or duration. Endoscopy. 2014;46 Suppl 1 UCTN: E281-E282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 55. | Chittleborough TJ, Mgaieth S, Kirkby B, Zakon J. Remove the migrated stent: sigmoid colon perforation from migrated biliary stent. ANZ J Surg. 2016;86:947-948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 56. | Kusters PJ, Keulen ET, Peters FP. Duodenal perforation following bile duct endoprosthesis placement. Endoscopy. 2014;46 Suppl 1 UCTN:E646-E647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 57. | Kriss M, Yen R, Fukami N, Bambha K, Wani S. Duodenal perforation secondary to migrated biliary stent in a liver transplant patient: successful endoscopic closure with an over-the-scope clip. Gastrointest Endosc. 2015;81:1258-1259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 58. | Virgilio E, Pascarella G, Scandavini CM, Frezza B, Bocchetti T, Balducci G. Colonic perforations caused by migrated plastic biliary stents. Korean J Radiol. 2015;16:444-445. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 59. | Mady RF, Niaz OS, Assal MM. Migrated biliary stent causing perforation of sigmoid colon and pelvic abscess. BMJ Case Rep. 2015;2015. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 60. | Siaperas P, Ioannidis A, Skarpas A, Angelopoulos A, Drikos I, Karanikas I. A rare cause for Hartmann's procedure due to biliary stent migration: A case report. Int J Surg Case Rep. 2017;31:83-85. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 61. | Barakat MT, Kothari S, Banerjee S. Cut and Paste: Endoscopic Management of a Perforating Biliary Stent Utilizing Scissors and Clips. Dig Dis Sci. 2018;63:2202-2205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 62. | Ferm S, Fisher C, Hassam A, Rubin M, Kim SH, Hussain SA. Primary Endoscopic Closure of Duodenal Perforation Secondary to Biliary Stent Migration: A Case Report and Review of the Literature. J Investig Med High Impact Case Rep. 2018;6:2324709618792031. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 63. | Ekmektzoglou K, Nikou E, Apostolopoulos P, Grigoraki D, Manesis K, Alexandrakis G. Size does matter: when a large plastic biliary stent ends up in the root of the mesentery. Clin J Gastroenterol. 2019;12:102-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 64. | Topal U, Ülkü A, Sarıtaş AG, Akçam AT. A rare complication in a liver transplant patient: Meckel diverticulum perforation due to biliary stent. Int J Surg Case Rep. 2018;53:35-38. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 65. | Le Mouel JP, Hakim S, Thiebault H. Duodenal Perforation Caused by Early Migration of a Biliary Plastic Stent: Closure With Over-the-Scope Clip. Clin Gastroenterol Hepatol. 2019;17:e6-e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 66. | Kim HS, Moon HJ, Lee NY, Lee HT, Woo MS, Lee JW, Jang IS, Lee KD. Endoscopic management of duodenal perforations caused by migrated biliary plastic stents. Endosc Int Open. 2019;7:E792-E795. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 67. | Jadallah K, Alzubi B, Sweidan A, Almanasra AR. Intraperitoneal duodenal perforation secondary to early migration of biliary stent: closure with through-the-scope clip. BMJ Case Rep. 2019;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 68. | Marcos P, Capelão G, Atalaia-Martins C, Clara P, Eliseu L, Vasconcelos H. Sigmoid Perforation by a Migrated Plastic Biliary Stent. GE Port J Gastroenterol. 2020;27:215-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 69. | Riccardi M, Deters K, Jabbar F. Sigmoid Diverticulitis and Perforation Secondary to Biliary Stent Migration. Case Rep Surg. 2019;2019:2549170. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 70. | Tsang CLN, O'Neill RS, Joseph CM, Palasovski T. Small Bowel Perforation Secondary to Biliary Stent Migration in an Incarcerated Inguinal Hernia. Cureus. 2020;12:e7268. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 71. | Ip CCK, Hong M. Small bowel perforation from migrated biliary stent: why did it happen? ANZ J Surg. 2020;90:1779-1780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |