Published online Aug 16, 2020. doi: 10.4253/wjge.v12.i8.220
Peer-review started: March 21, 2020
First decision: April 25, 2020
Revised: May 19, 2020
Accepted: July 19, 2020
Article in press: July 19, 2020
Published online: August 16, 2020
Processing time: 144 Days and 18.4 Hours
Recently, with the advent of more advanced devices and endoscopic techniques, endoscopic retrograde cholangiopancreatography (ERCP) in Billroth II (B-II) patients has been increasingly performed. However, the procedures are difficult, and the techniques and strategies have not been defined.
To reveal the appropriate scope for ERCP in B-II patients.
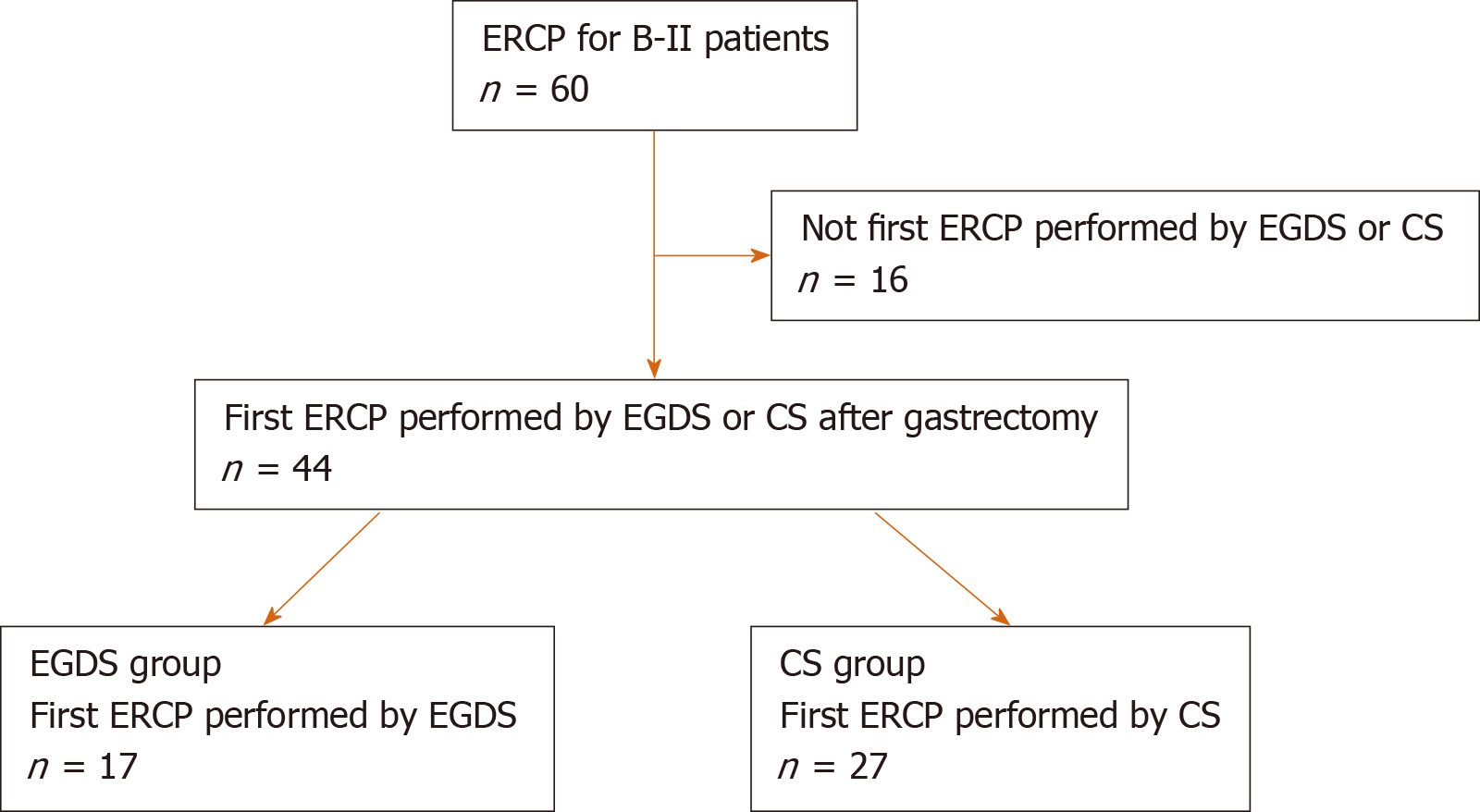
Sixty ERCP procedures were performed on B-II patients between June 2005 and May 2018 at Fukushima Medical University Hospital, and in 44 cases, this was the first ERCP procedure performed by esophagogastroduodenoscopy (EGDS) or colonoscopy (CS) after B-II gastrectomy. These cases were divided into two groups: 17 cases of ERCP performed by EGDS (EGDS group) and 27 cases of ERCP performed by CS (CS group). The patient characteristics and ERCP procedures were compared between the EGDS and CS groups.
The procedural time was significantly shorter in the EGDS group than in the CS group [median (range): 60 (20-100) vs 90 (40-128) min, P value < 0.01]. CS was an independent factor of a longer ERCP procedural time according to the univariate and multivariate analyses (odds ratio: 3.97, 95%CI: 1.05-15.0, P value = 0.04).
Compared to CS, EGDS shortened the procedural time of ERCP in B-II patients.
Core tip: This study aimed to reveal the appropriate scope for endoscopic retrograde cholangiopancreatography (ERCP) in Billroth II (B-II) patients. Sixty ERCP procedures were performed in B-II patients, and in 44 cases, this was the first ERCP procedure performed by esophagogastroduodenoscopy (EGDS) or colonoscopy (CS) after B-II gastrectomy. The procedural time was significantly shorter in the EGDS group than in the CS group. CS was an independent factor of a longer ERCP procedural time according to the univariate and multivariate analyses. Compared to CS, EGDS shortened the procedural time of ERCP in B-II patients.
- Citation: Sugimoto M, Takagi T, Suzuki R, Konno N, Asama H, Sato Y, Irie H, Watanabe K, Nakamura J, Kikuchi H, Takasumi M, Hashimoto M, Kato T, Hikichi T, Ohira H. Which scope is appropriate for endoscopic retrograde cholangiopancreatography after Billroth II reconstruction: An esophagogastroduodenoscope or a colonoscope? World J Gastrointest Endosc 2020; 12(8): 220-230
- URL: https://www.wjgnet.com/1948-5190/full/v12/i8/220.htm
- DOI: https://dx.doi.org/10.4253/wjge.v12.i8.220
In the past, percutaneous cholangiography or biliary drainage was mainly performed in patients who underwent gastrectomy or intestinal reconstructive surgery[1]. Recently, with the advent of more advanced devices and endoscopic techniques, endoscopic cholangiography and biliary drainage have been increasingly performed in these patients. Although endoscopic retrograde cholangiopancreatography (ERCP) in Billroth II (B-II) patients has been previously reported[2-19], the procedures are difficult, and the techniques and strategies have not been defined.
Initially, ERCP was performed in B-II patients using a side-viewing endoscope[2,3]. However, it is difficult to insert the side-viewing endoscope into the afferent loop, and the risk of bowel perforation was reported to be greater for ERCP in B-II patients when a side-viewing endoscope was used than when a forward-viewing endoscope was used[20]. Therefore, a forward-viewing endoscope has recently been used for this procedure and has been shown to be as effective as a side-viewing endoscope for ERCP in B-II patients[20-22].
Among the reports describing the use of a forward-viewing endoscope, some have described the use of esophagogastroduodenoscopy (EGDS)[9,12,15,17,19], and others have described the use of long endoscopes (e.g., a colonoscope, single-balloon endoscope, or double-balloon endoscope)[7,8,16,19]. Therefore, this study aimed to reveal which scope (an esophagogastroduodenoscope or a colonoscope) is appropriate for ERCP in B-II patients.
This study was a retrospective study to investigate the appropriate scope for ERCP in B-II patients. This study was approved by the Institutional Review Board of Fukushima Medical University.
Sixty ERCP procedures were performed in B-II patients between June 2005 and May 2018 at Fukushima Medical University Hospital (Figure 1). Among these cases, 44 involved ERCP by EGDS or colonoscopy (CS) after B-II gastrectomy. Sixteen cases were excluded from this study because in these cases, this was not the first ERCP performed by EGDS or CS. Five cases involved ERCP by both EGDS and CS. The 44 patients were divided into two groups: 17 cases of ERCP by EGDS (EGDS group) and 27 cases of ERCP by CS (CS group). Patients were not required to provide informed consent for this study because this investigation used anonymous clinical data obtained after each patient had agreed to examination or treatment by written consent. For full disclosure, see the details of this study published on the home page of Fukushima Medical University.
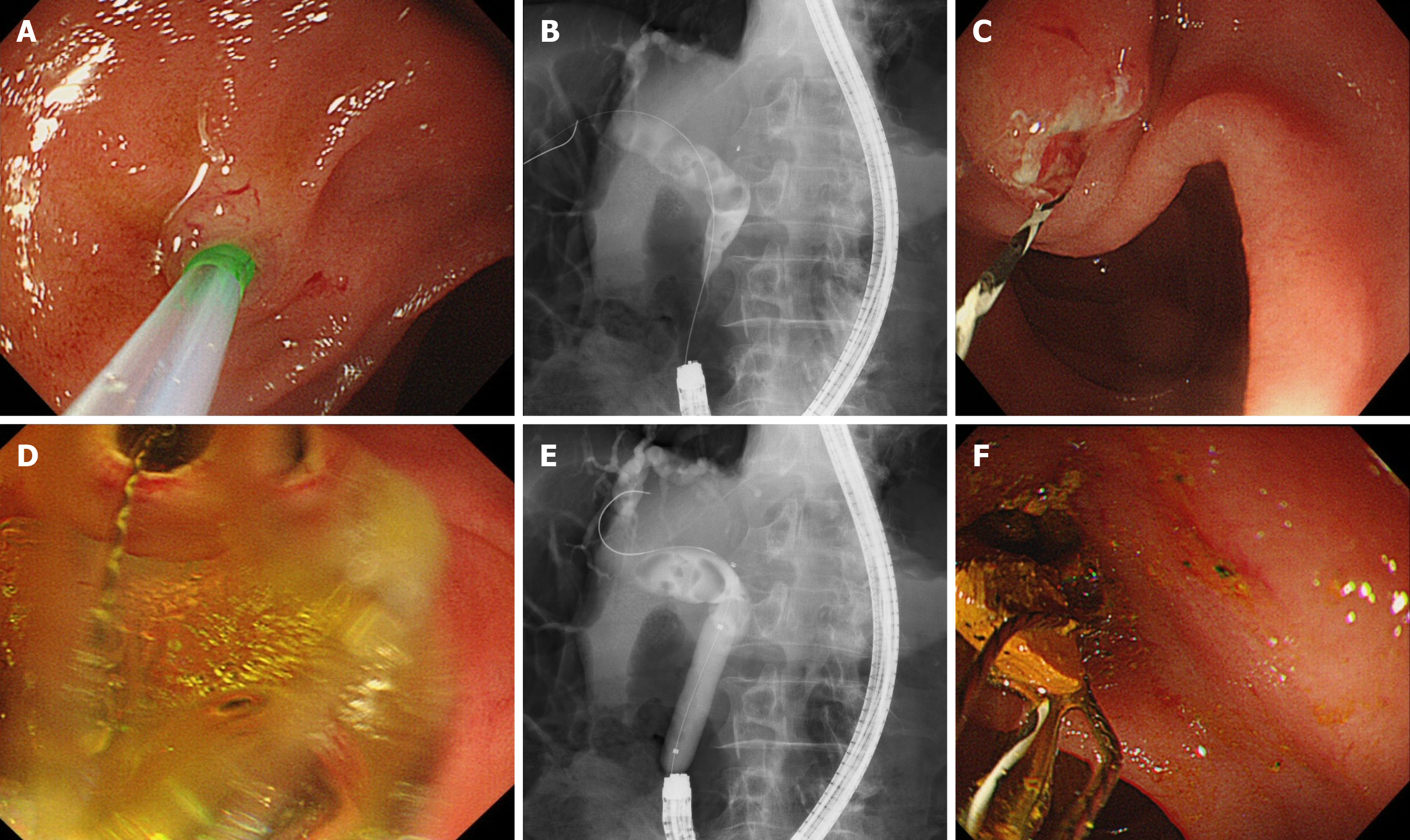
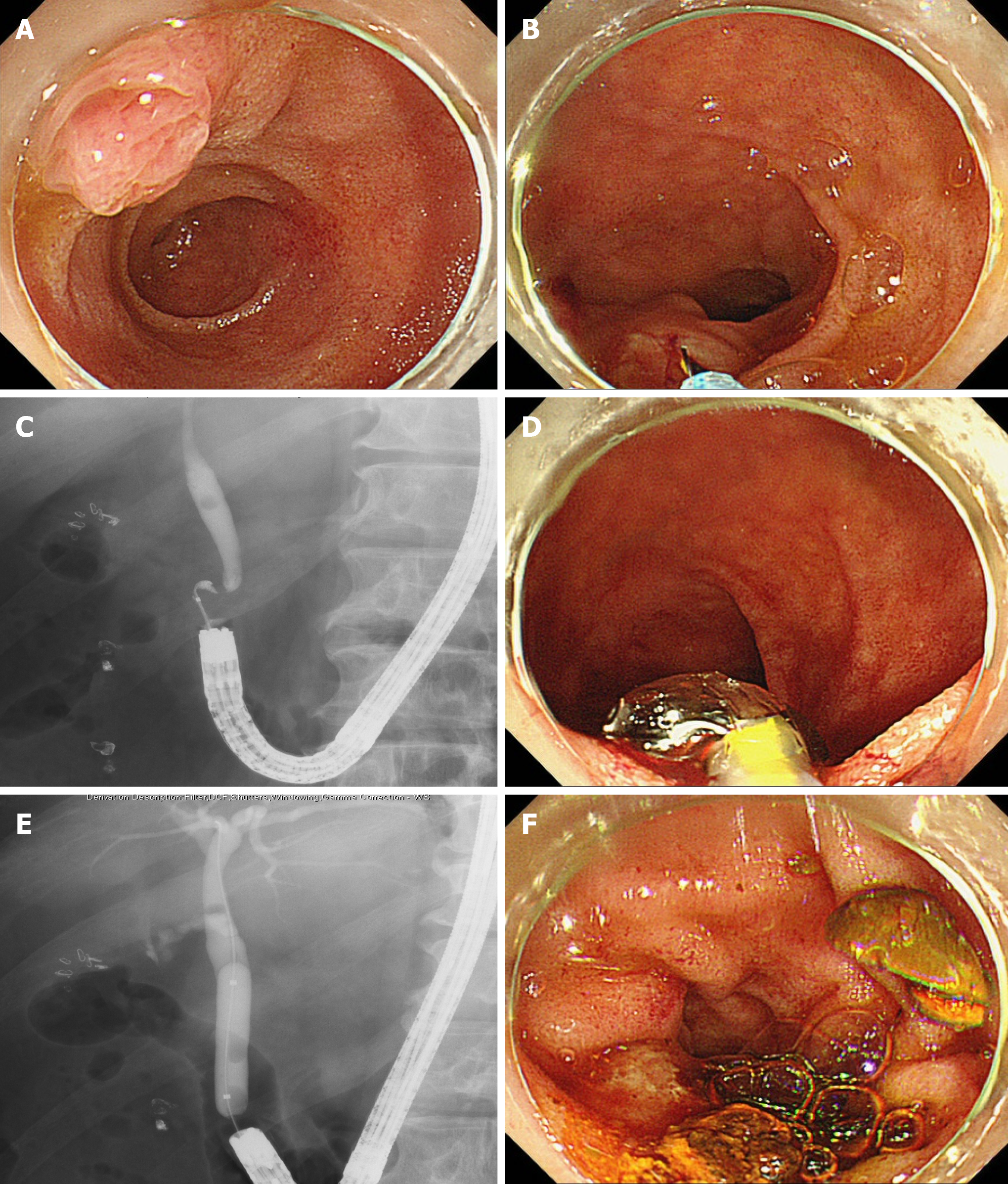
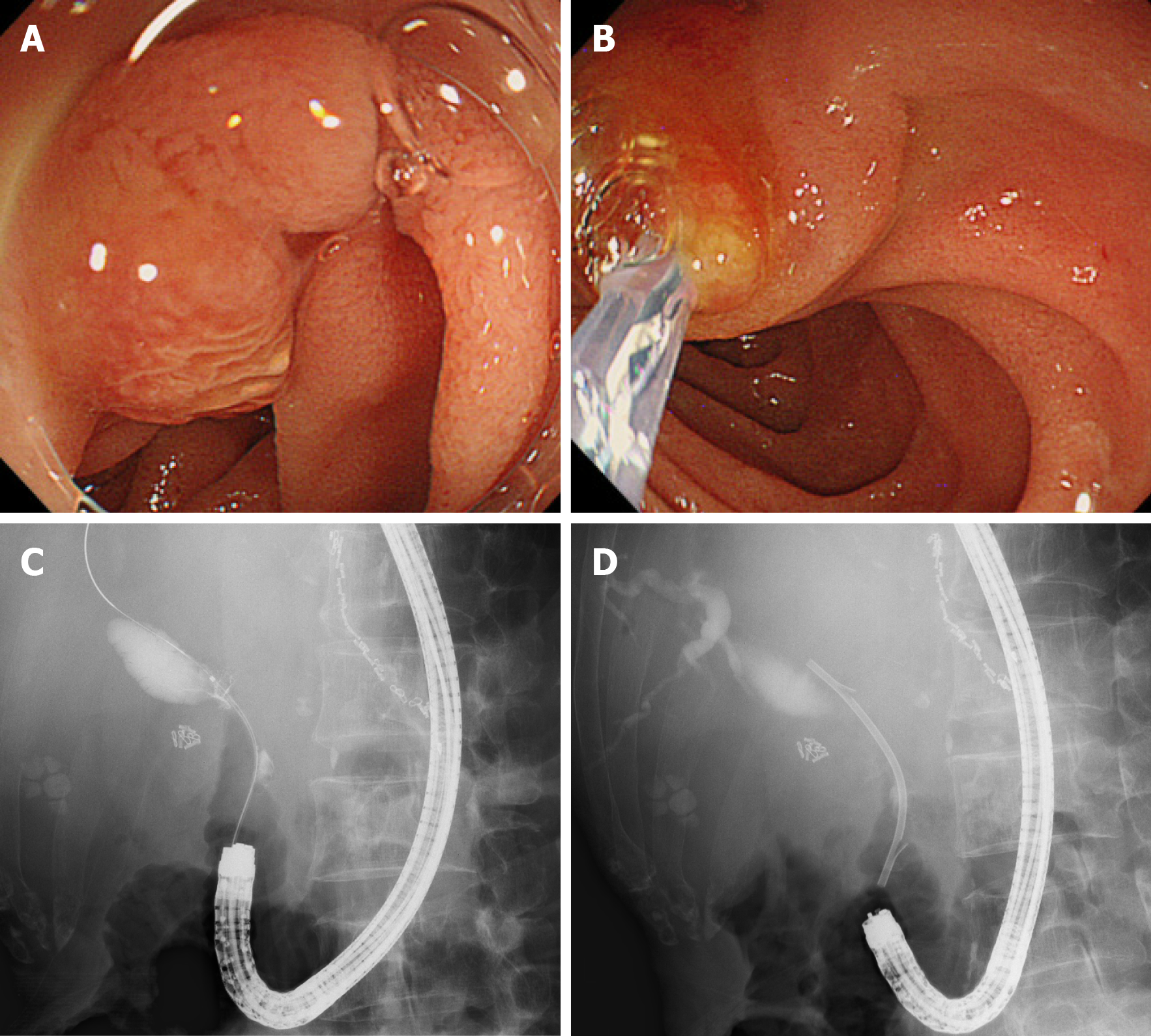
Before ERCP was started, patients were intravenously administered 300 mg of gabexate mesylate. After the patients were sedated with midazolam under blood pressure and oxygen saturation monitoring, an endoscope with a cap attached to the tip was inserted. The endoscope used was randomly chosen by each endoscopist. After the entrance of both the afferent loop and the efferent loop was observed, the endoscope was advanced to the afferent loop, reaching the papilla of Vater. Insertion into the afferent loop was performed with confirmation of the running direction by X-ray images. In the EGDS group, cannulation was initiated after the papilla was turned to the 9 to 11 o’clock position (Figure 2A). In the CS group, cannulation was initiated after the papilla was turned to the 6 o’clock position (Figure 3A and B). In patients with biliary or pancreatic ductal strictures, a biliary stent was inserted after endoscopic sphincterotomy (EST).
In patients with biliary ductal stones, EST and endoscopic papillary balloon dilation (EPBD) or endoscopic papillary large balloon dilation (EPLBD) were performed, as appropriate (Figures 2 and 3). EPBD was performed if the transverse diameter of the largest stone was > 8 mm and bile duct stones were difficult to remove by EST alone or if a peripapillary diverticulum was present. EPLBD was performed if the transverse diameter of the largest stone was > 12 mm, if many bile duct stones were difficult to remove by EST alone or if sufficient EST was difficult because of a peripapillary diverticulum. Stones that were too large to be ejected after EPBD or EPLBD were destroyed by catheter fragmentation. If complete stone clearance was difficult, then a biliary stent was inserted.
A GIF-Q240X, GIF-Q260, or GIF-Q260J (Olympus, Tokyo, Japan) scope was used in the EGDS group. A PCF-Q260AI, PCF-Q260AL, PCF-PQ260L, or SIF-Q260 (Olympus) scope was used in the CS group. PCF-PQ260L and SIF-Q260 scopes were used in one patient each. A D-201-11304 (Olympus) was used as the cap attached to the tip of the GIF-Q240 scope. A D-201-10704 (Olympus) was used as the cap attached to the tip of the GIF-Q260 scope. A D-201-12704 (Olympus) was used as the cap attached to the tip of the PCF-Q260AI and PCF-Q260AL scopes. A D-201-10704 (Olympus) was used as the cap attached to the tip of the PCF-PQ260L and SIF-Q260 scopes. A Tandem XL (Boston Scientific Japan, Tokyo, Japan), MTW ERCP tapered catheter (MTW Endoskopie, Wesel, Germany) or a Swing Tip PR-233Q (Olympus) was used as the ERCP catheter. EST was performed using an RX needle knife XL (Boston Scientific) or Billroth II sphincterotome (Cook Japan, Tokyo, Japan). A Hurricane RX biliary balloon dilatation catheter (Boston Scientific) was used for EPBD. A CRE biliary balloon dilatation catheter (Boston Scientific) or a Giga or Giga II balloon (Century Medical, Tokyo, Japan) was used for EPLBD. A Trapezoid RX basket catheter (Boston Scientific) or an FG-V425PR basket catheter (Olympus) was used to crush and remove stones. A Flexima biliary stent (Boston Scientific) or a Zimmon biliary stent (Cook Japan, Tokyo, Japan) was used as the biliary stent. All of these devices can be used with both the GIF-Q260J and PCF-Q260AI colonoscopes. The Swing Tip PR-233Q, Hurricane RX biliary balloon dilatation catheter, Giga balloon, Trapezoid RX basket catheter, and Flexima biliary stent cannot be used with both the GIF-Q240X and the GIF-Q260 scopes. The Swing Tip PR-233Q, Hurricane RX biliary balloon dilatation catheter, and Trapezoid RX basket catheter cannot be used with the PCF-Q260AL scope. In the two patients in whom the PCF-PQ260AL or SIF-Q260 scope was used, the papilla of Vater could not be observed, and ERCP devices were not used with the scope.
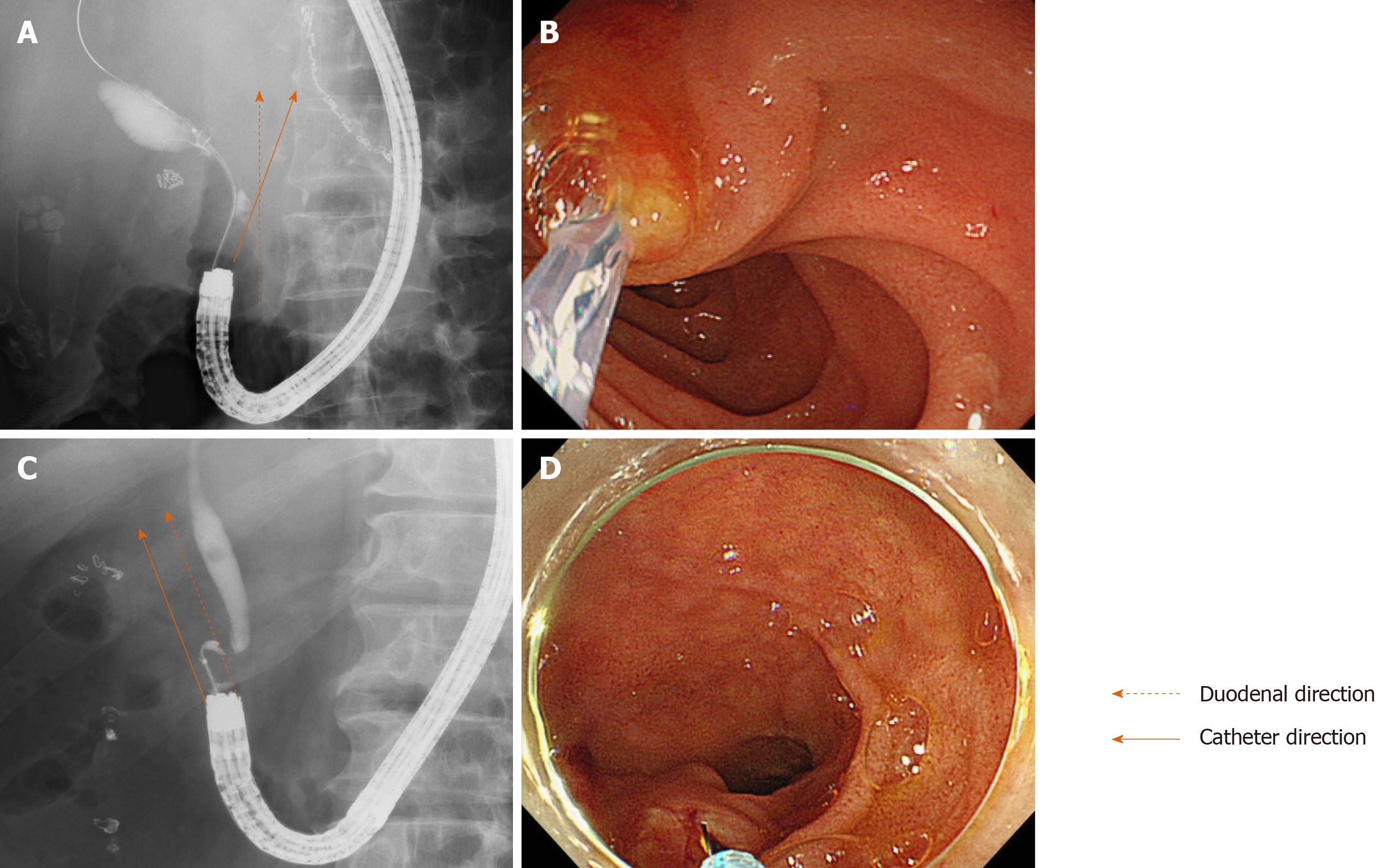
The characteristics of the patients (age, sex, period after B-II reconstruction, diseases treated with B-II reconstruction, untreated papilla of Vater, antithrombotic drug use, periampullary diverticulum, diseases, transverse diameter of the largest stone, and number of stones) and ERCP procedure details [EST, EPBD or EPLBD, procedural time, papilla of Vater access, stone clearance, stone destruction, procedural success, and post-ERCP pancreatitis (PEP)] were compared between the EGDS and CS groups. Additionally, the relationship between the duodenal and catheter directions (cross or parallel) and the observation of papilla of Vater in the front were compared as factors of scope usability between the EGDS and CS groups (Figure 4). The duodenal and catheter directions were determined from the X-ray images of the biliary cannulation. An untreated papilla of Vater was defined as one that had not undergone incision or dilation. If all biliary stones were removed, the intended procedures (for example, biliary duct or pancreatic duct investigation or stenting) were performed using the first endoscope, and this was defined as stone clearance or procedural success. The diagnosis of PEP was performed according to Cotton’s criteria[23]. If patients were observed to have an elevated serum amylase level more than three times the normal upper limit with abdominal pain at more than 24 h after ERCP, they were diagnosed with PEP. Furthermore, peripancreatic inflammation was confirmed in all PEP cases by contrast-enhanced CT.
Age, period after B-II reconstruction, and transverse diameter of the largest stone were compared by Student’s t test. The procedural time and number of stones were compared using the Mann-Whitney U test. Nominal variables were compared by Fisher’s exact test. Factors influencing the ERCP procedural time were investigated by logistic regression analysis. A P value < 0.05 was defined as statistically significant. All statistical analyses were performed using the EZR platform (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria). EZR is a modified version of the R commander, which was designed to perform functions that are frequently used in biostatistics[24].
The patient characteristics were not significantly different between the two groups (Table 1). The ERCP procedural time was significantly shorter in the EGDS group than in the CS group [median (range): 60 (20-100) vs 90 (40-128) min, P value < 0.01] (Table 2).
| EGDS group (n = 17) | CS group (n = 27) | P value | |
| Age (yr, mean ± SD) | 75.2 ± 13.0 | 75.7 ± 13.0 | 0.88 |
| Sex, male/female | 15/2 | 22/5 | 0.69 |
| Period after B-II reconstruction (yr, mean ± SD) | 36.8 ± 13.8 | 36.8 ± 13.8 | 1.0 |
| Diseases treated with B-II reconstruction | |||
| Gastric ulcer, n | 10 | 11 | |
| Duodenal ulcer, n | 3 | 9 | |
| Gastric cancer, n | 2 | 4 | |
| Pyloric stenosis, n | 1 | 1 | |
| Gastric ptosis, n | 1 | 1 | |
| Unknown, n | 1 | ||
| Untreated papilla of Vater, n (%) | 15 (88.2) | 27 (100) | 0.14 |
| Antithrombotic drugs, n (%) | 2 (11.8) | 5 (18.5) | 0.69 |
| Periampullary diverticulum, n (%) | 1 (5.9) | 3 (11.1) | 1.0 |
| Disease, n | |||
| Bile duct stone | 11 | 20 | 0.52 |
| Others | 6 | 7 | |
| Biliary ductal cancer | 3 | 2 | |
| Pancreatic cancer | 1 | 3 | |
| Chronic pancreatitis | 1 | 1 | |
| Benign biliary stricture | 1 | 1 | |
| Transverse diameter of the largest stone (mm, mean ± SD) | 10.2 ± 4.8 | 12.2 ± 3.8 | 0.24 |
| Number of stones [n, median (range)] | 4 (1 - 30) | 2 (1 - 6) | 0.18 |
| EGDS group (n = 17) | CS group (n = 27) | P value | |
| EST, n (%) | 7 (41.2) | 19 (70.4) | 0.07 |
| EPBD or EPLBD, n (%) | 6 (35.3) | 13 (48.1) | 0.54 |
| Procedural time [min, median (range)] | 60 (20-100) | 90 (40-128) | < 0.01 |
| Papilla of Vater access, n (%) | 14 (82.4) | 25 (92.6) | 0.36 |
| Stone clearance, n (%) | 6/11 (54.5) | 8/19 (42.1) | 1.0 |
| Stone destruction, n (%) | 3/11 (27.3) | 6/19 (31.6) | 1.0 |
| Procedural success, n (%) | 14 (82.4) | 17 (63.0) | 0.20 |
| Adverse events, n (%) | 0 (0) | 0 (0) | |
| PEP, n (%) | 0 (0) | 0 (0) |
The procedural success rate was not significantly different between the EGDS group and the CS group (82.4% vs 63.0%, P value = 0.20). Procedural success was difficult to achieve in three patients in the EGDS group. Among them, one patient underwent surgery; in another patient, procedural success by ERCP was not achieved using an SIF-H290-S (Olympus) single-balloon scope, and the patient finally underwent conservative treatment; in the last patient, procedural success was not achieved by ERCP using an SIF-H290-S scope but was finally achieved by ERCP using a PCF-Q260AL scope. Procedural success was not achieved in ten patients in the CS group. Among them, procedural success was achieved in four patients by ERCP using a Q260J scope and in one patient by a second ERCP procedure using a PCF-Q260AI scope. Percutaneous transhepatic biliary drainage was performed in four patients (procedural success was achieved in two patients by ERCP with the rendezvous technique). One patient subsequently underwent conservative treatment.
CS was an independent factor of a longer ERCP procedural time, as determined by univariate and multivariate analyses (Table 3).
| Univariate analysis | Multivariate analysis | ||||||
| Procedural time ≥ 70 min, n (yes/no) | OR | 95%CI | P value | OR | 95%CI | P value | |
| Age ≥ 76 yr | 13/9 | 2.09 | 0.63–6.94 | 0.23 | |||
| Sex, male | 17/20 | 0.34 | 0.06–1.98 | 0.23 | |||
| Period after B-II reconstruction ≥ 40 | 11/11 | 1.0 | 0.31–3.26 | 1.0 | |||
| Untreated papilla of Vater | 21/21 | 1.0 | 0.06–17.1 | 1.0 | |||
| Antithrombotic drug use | 3/4 | 0.71 | 0.14–3.63 | 0.68 | |||
| Periampullary diverticulum | 1/3 | 0.30 | 0.03–3.15 | 0.32 | |||
| Bile duct stone | 15/16 | 0.8 | 0.22–2.94 | 0.74 | |||
| Transverse diameter of largest stone ≥ 12.2 mm | 7/8 | 0.77 | 0.18–3.21 | 0.72 | |||
| Number of stones ≥ 2 | 10/7 | 2.29 | 0.52–10.0 | 0.27 | |||
| CS group | 17/10 | 4.08 | 1.11–5.0 | 0.035 | 3.97 | 1.05–15.0 | 0.04 |
| EST | 14/12 | 1.46 | 0.44–4.88 | 0.54 | |||
| EPBD or EPLBD | 10/9 | 1.20 | 0.37–3.97 | 0.76 | |||
| Papilla of Vater access | 20/19 | 1.58 | 0.24–10.5 | 0.64 | |||
| Stone clearance | 8/8 | 1.0 | 0.24–4.2 | 1.0 | |||
| Stone destruction | 6/3 | 2.67 | 0.52–13.7 | 0.24 | |||
| Procedural success | 15/19 | 0.34 | 0.07–1.54 | 0.16 | 0.36 | 0.07–1.74 | 0.2 |
Regarding the factors influencing scope usability, crossing of the duodenal and catheter directions was observed more often in the EGDS group than in the CS group (cross/parallel: 11/3 vs 8/15, P value = 0.02) (Table 4). Observation of the papilla of Vater in the front was achieved more often in the EGDS group than in the CS group.
In this study, EGDS was compared with CS for performing ERCP in B-II patients. The results showed that compared to CS, EGDS shortened the ERCP procedural time.
An increasing number of ERCP procedures after gastrectomy have been performed in patients who have undergone B-II reconstruction, and several scopes have been used. As mentioned in the introduction, the side-viewing endoscope was initially used for ERCP in B-II patients[2,3]. However, recently, forward-viewing endoscopes have been used. Byun et al[9], Park et al[12], Ki et al[17], and Jang et al[15] used an esophagogastroduodenoscope. However, Abdelhafez et al[19] used a colonoscope, and Itoi et al[7] and Kawamura et al[16] used a single-balloon enteroscope. Lin et al[8] used a double-balloon endoscope. Although it is unknown which scope is most efficient, the esophagogastroduodenoscope was reported to shorten the procedural time. In most reports, the procedural time was not described. However, a study reported that the average EGDS procedural time was 36.3 min[15], which is a short time. EGDS was superior to procedures with a longer scope because the papilla of Vater can be observed in the front (Figures 2A, 3A, 3B, 4A, 4B, 4E, 5A, and 5B) because the esophagogastroduodenoscope can be curved up to 210 degrees, while a colonoscope can be curved up to 180 degrees. The duodenal direction and the catheter direction could easily be crossed in ERCP using EGDS (Figure 4 and Table 4). However, these two directions tended to run parallel in ERCP using CS. In fact, in three cases, it was difficult to cannulate the bile duct by CS, whereas bile duct cannulation was successful by EGDS (Figure 5).
Interestingly, although the procedural success rate was not significantly different between the two groups, the procedural time was shorter in the EGDS group. For patients who have undergone B-II reconstruction, the radiation exposure dose is decreased with EGDS. The exposure dose is also lower for the medical staff, who can thus perform more ERCP procedures. As such, EGDS is the first choice for ERCP in patients who have undergone B-II reconstruction.
There are several limitations to this study. First, this study was a retrospective and small study, and it was performed at a single institute. In the future, prospective and multicenter studies are needed. Second, due to the retrospective nature of this study, ERCP procedures were not performed by specified endoscopists. However, ERCP was performed by pancreaticobiliary specialists who had experience performing at least 2000 ERCP procedures or by trainees under the guidance of these specialists. Therefore, the quality of the ERCP procedure was constant. Third, the exact cannulation time was not recorded. However, as described above, the scope was chosen randomly. Additionally, the patient characteristics, diameter or number of stones, and factors related to ERCP were not significantly different between the two groups. Therefore, if EGDS is used for ERCP in B-II patients, the duration of the whole procedure, including insertion and cannulation, could be shortened.
Compared to a longer scope, the esophagogastroduodenoscope shortened the procedural time of ERCP for patients who had undergone B-II reconstruction.
Recently, with the advent of more advanced devices and endoscopic techniques, endoscopic retrograde cholangiopancreatography (ERCP) in Billroth II (B-II) patients has been increasingly performed. However, the procedures are difficult, and the techniques and strategies have not been defined.
The forward-viewing endoscope has been used for ERCP in B-II patients. By using the forward-viewing endoscope, ERCP in B-II patients was performed safely and as effectively as ERCP using a side-viewing endoscope. As forward-viewing endoscopes, esophagogastroduodenoscopy (EGDS) or colonoscopy (CS) is used for ERCP in B-II patients. However, which scope (EGDS or CS) should be used remains unknown.
To reveal the appropriate scope for ERCP in B-II patients.
For the 44 included cases, this was the first ERCP procedure performed by EGDS or CS after B-II gastrectomy. These cases were divided into two groups: 17 cases of ERCP by EGDS (EGDS group) and 27 cases of ERCP by CS (CS group). The patient characteristics and ERCP procedures were compared between the EGDS and CS groups.
The procedural time was significantly shorter in the EGDS group than in the CS group. CS was an independent factor of a longer ERCP procedural time.
Compared with CS, EGDS shortened the procedural time of ERCP for patients who had undergone B-II reconstruction.
The results in this study could contribute to choosing an ERCP scope for patients who have undergone B-II reconstruction.
We thank all of the staff at the Department of Gastroenterology of Fukushima Medical University, the Department of Endoscopy of Fukushima Medical University Hospital, and the gastroenterology ward of Fukushima Medical University Hospital. We also thank American Journal Experts for providing English language editing.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Amornyotin S, Kayaalp C, Shi H S-Editor: Zhang L L-Editor: A P-Editor: Wang LL
| 1. | Jeong EJ, Kang DH, Kim DU, Choi CW, Eum JS, Jung WJ, Kim PJ, Kim YW, Jung KS, Bae YM, Cho M. Percutaneous transhepatic choledochoscopic lithotomy as a rescue therapy for removal of bile duct stones in Billroth II gastrectomy patients who are difficult to perform ERCP. Eur J Gastroenterol Hepatol. 2009;21:1358-1362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Forbes A, Cotton PB. ERCP and sphincterotomy after Billroth II gastrectomy. Gut. 1984;25:971-974. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 64] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | Osnes M, Rosseland AR, Aabakken L. Endoscopic retrograde cholangiography and endoscopic papillotomy in patients with a previous Billroth-II resection. Gut. 1986;27:1193-1198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 77] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Ciçek B, Parlak E, Dişibeyaz S, Koksal AS, Sahin B. Endoscopic retrograde cholangiopancreatography in patients with Billroth II gastroenterostomy. J Gastroenterol Hepatol. 2007;22:1210-1213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 48] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 5. | Nakahara K, Horaguchi J, Fujita N, Noda Y, Kobayashi G, Ito K, Obana T, Takasawa O. Therapeutic endoscopic retrograde cholangiopancreatography using an anterior oblique-viewing endoscope for bile duct stones in patients with prior Billroth II gastrectomy. J Gastroenterol. 2009;44:212-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 6. | Itoi T, Ishii K, Itokawa F, Kurihara T, Sofuni A. Large balloon papillary dilation for removal of bile duct stones in patients who have undergone a billroth ii gastrectomy. Dig Endosc. 2010;22 Suppl 1:S98-S102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 42] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Itoi T, Ishii K, Sofuni A, Itokawa F, Tsuchiya T, Kurihara T, Tsuji S, Ikeuchi N, Umeda J, Moriyasu F. Single-balloon enteroscopy-assisted ERCP in patients with Billroth II gastrectomy or Roux-en-Y anastomosis (with video). Am J Gastroenterol. 2010;105:93-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 124] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 8. | Lin CH, Tang JH, Cheng CL, Tsou YK, Cheng HT, Lee MH, Sung KF, Lee CS, Liu NJ. Double balloon endoscopy increases the ERCP success rate in patients with a history of Billroth II gastrectomy. World J Gastroenterol. 2010;16:4594-4598. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 14] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Byun JW, Kim JW, Sung SY, Jung HY, Jeon HK, Park HJ, Kim MY, Kim HS, Baik SK. Usefulness of Forward-Viewing Endoscope for Endoscopic Retrograde Cholangiopancreatography in Patients with Billroth II Gastrectomy. Clin Endosc. 2012;45:397-403. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Choi CW, Choi JS, Kang DH, Kim BG, Kim HW, Park SB, Yoon KT, Cho M. Endoscopic papillary large balloon dilation in Billroth II gastrectomy patients with bile duct stones. J Gastroenterol Hepatol. 2012;27:256-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 44] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 11. | Jang HW, Lee KJ, Jung MJ, Jung JW, Park JY, Park SW, Song SY, Chung JB, Bang S. Endoscopic papillary large balloon dilatation alone is safe and effective for the treatment of difficult choledocholithiasis in cases of Billroth II gastrectomy: a single center experience. Dig Dis Sci. 2013;58:1737-1743. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 12. | Park SB, Kim HW, Kang DH, Choi CW, Yoon KT, Cho M, Song BJ. Sphincterotomy by triple lumen needle knife using guide wire in patients with Billroth II gastrectomy. World J Gastroenterol. 2013;19:9405-9409. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Yamauchi H, Kida M, Okuwaki K, Miyazawa S, Iwai T, Takezawa M, Kikuchi H, Watanabe M, Imaizumi H, Koizumi W. Short-type single balloon enteroscope for endoscopic retrograde cholangiopancreatography with altered gastrointestinal anatomy. World J Gastroenterol. 2013;19:1728-1735. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 55] [Cited by in RCA: 53] [Article Influence: 4.4] [Reference Citation Analysis (1)] |
| 14. | Okabe Y, Ishida Y, Kuraoka K, Ushijima T, Tsuruta O. Endoscopic bile duct and/or pancreatic duct cannulation technique for patients with surgically altered gastrointestinal anatomy. Dig Endosc. 2014;26 Suppl 2:122-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Jang JS, Lee S, Lee HS, Yeon MH, Han JH, Yoon SM, Chae HB, Youn SJ, Park SM. Efficacy and Safety of Endoscopic Papillary Balloon Dilation Using Cap-Fitted Forward-Viewing Endoscope in Patients Who Underwent Billroth II Gastrectomy. Clin Endosc. 2015;48:421-427. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 16. | Kawamura T, Uno K, Suzuki A, Mandai K, Nakase K, Tanaka K, Yasuda K. Clinical usefulness of a short-type, prototype single-balloon enteroscope for endoscopic retrograde cholangiopancreatography in patients with altered gastrointestinal anatomy: preliminary experiences. Dig Endosc. 2015;27:82-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 17. | Ki HS, Park CH, Jun CH, Park SY, Kim HS, Choi SK, Rew JS. Feasibility of cap-assisted endoscopic retrograde cholangiopancreatography in patients with altered gastrointestinal anatomy. Gut Liver. 2015;9:109-112. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 18. | Frimberger E, Abdelhafez M, Schmid RM, von Delius S. A novel mechanical simulator for cannulation and sphincterotomy after Billroth II or Roux-en-Y reconstruction. Endosc Int Open. 2016;4:E922-E926. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Abdelhafez M, Frimberger E, Klare P, Haller B, Schmid RM, von Delius S. Comparison of endoscopic sphincterotomy techniques after Billroth II gastrectomy using a novel mechanical simulator. Surg Endosc. 2017;31:5342-5347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (1)] |
| 20. | Park TY, Bang CS, Choi SH, Yang YJ, Shin SP, Suk KT, Baik GH, Kim DJ, Yoon JH. Forward-viewing endoscope for ERCP in patients with Billroth II gastrectomy: a systematic review and meta-analysis. Surg Endosc. 2018;32:4598-4613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (1)] |
| 21. | El Hajj II, Al-Haddad M. Challenges in ERCP post-Billroth II gastrectomy: Is it the scope, tools or technique? Saudi J Gastroenterol. 2019;25:333-334. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 22. | Li JS, Zou DW, Jin ZD, Chen J, Shi XG, Li ZS, Liu F. Endoscopic retrograde cholangiopancreatography in Billroth II gastrectomy patients: Outcomes and potential factors affecting technical failure. Saudi J Gastroenterol. 2019;25:355-361. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 23. | Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1890] [Cited by in RCA: 2037] [Article Influence: 59.9] [Reference Citation Analysis (1)] |
| 24. | Kanda Y. Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transplant. 2013;48:452-458. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9275] [Cited by in RCA: 13329] [Article Influence: 1110.8] [Reference Citation Analysis (0)] |