Published online Dec 16, 2020. doi: 10.4253/wjge.v12.i12.555
Peer-review started: August 18, 2020
First decision: September 18, 2020
Revised: September 28, 2020
Accepted: November 4, 2020
Article in press: November 4, 2020
Published online: December 16, 2020
Processing time: 116 Days and 14.7 Hours
Intraductal papillary neoplasm of the bile duct (IPNB) is a rare variant of bile duct tumors, characterized by an exophytic growth exhibiting a papillary mass within the bile duct lumen and it can be localized anywhere along the biliary tree, with morphological variations and occasional invasion.
We present a patient with obstructive jaundice who was diagnosed with IPNB using cholangioscopy during endoscopic retrograde cholangio-pancreatography. Using the SpyGlass DS II technology, we were able to define tumor extension and obtain targeted Spy-byte biopsies. After multidisciplinary evaluation, the patient was scheduled for surgical resection of the tumor, which was radically removed.
Cholangioscopy appears to be crucial for the rapid and clear diagnosis of lesions in the bile duct to achieve radical surgical resection.
Core Tip: Intraductal papillary neoplasm of the bile duct (IPNB) is a rare variant of bile duct tumors, characterized by an exophytic growth exhibiting a papillary mass within the bile duct lumen and it can be localized anywhere along the biliary tree, with morphological variations and occasional invasion. We present a patient with obstructive jaundice who was diagnosed with IPNB using cholangioscopy during endoscopic retrograde cholangio-pancreatography. Using the SpyGlass DS II technology we were able to define tumor extension and to obtain targeted Spy-byte biopsies. The patient underwent successful surgical rsection of the tumor.
- Citation: Cocca S, Grande G, Reggiani Bonetti L, Magistri P, Di Sandro S, Di Benedetto F, Conigliaro R, Bertani H. Common bile duct lesions - how cholangioscopy helps rule out intraductal papillary neoplasms of the bile duct: A case report. World J Gastrointest Endosc 2020; 12(12): 555-559
- URL: https://www.wjgnet.com/1948-5190/full/v12/i12/555.htm
- DOI: https://dx.doi.org/10.4253/wjge.v12.i12.555
Intraductal papillary neoplasm of the bile duct (IPNB) is a rare variant of bile duct tumors, characterized by an exophytic growth exhibiting a papillary mass within the bile duct lumen and it can be localized anywhere along the biliary tree, with morphological variations and occasional invasion. IPNB can be classified into extra-hepatic IPNB and intra-hepatic IPNB. Surgical resection is the first-line treatment and the prognosis of this tumor is better than that of cholangiocarcinoma[1,2].
A 72-year-old male patient was admitted to our hospital due to obstructive jaundice and abdominal pain.
He was a pacemaker carrier and had a history of significant cardiovascular comorbidities.
No significant past illnesses, apart from cardiovascular disorders.
No family history of gastrointestinal tumors.
On physical examination there was tenderness in the right upper quadrant of the abdomen. Temperature was normal and blood pressure was 100/60 mmHg.
Blood tests showed high direct bilirubin levels (6.5 mg/dL) and altered liver function tests.
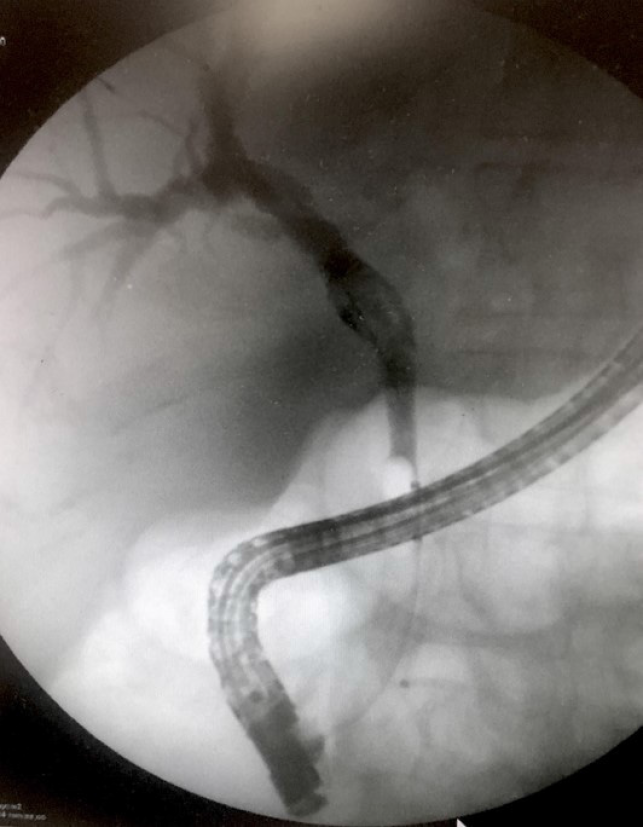
Computed tomography scan revealed a 3 cm hyperdense mass within the common hepatic duct (CHD). Cholangiography during endoscopic retrograde cholangio-pancreatography (ERCP) confirmed the presence of segmental CHD dilation without clear filling defects in the distal tract (Figure 1).
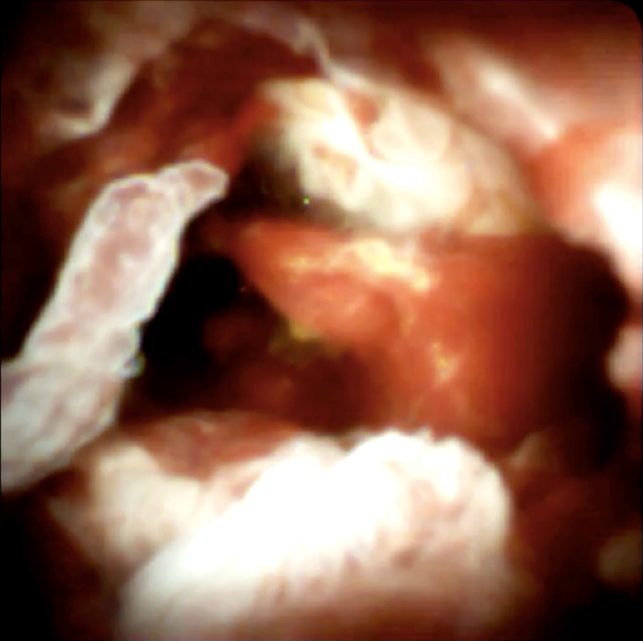
Peroral cholangioscopy (POC), using the SpyGlass DS II technology (Boston Scientific Ltd., Ireland) was performed. After extensive irrigation due to the presence of secretions, an intraductal papillary mass, characterized by papillary projections with fine vascular cores protruding into the lumen was visualized (Figure 2). The mass involved the CHD and was 1 cm from the hilar bifurcation (Klatskin Tumor type I), extending 1 cm up to the cystic insertion in the CHD. Targeted Spy-byte biopsies were obtained, and the results of pathologic examination were consistent with IPNB.
After multidisciplinary evaluation, the patient was scheduled for CHD surgical resection, cholecystectomy and hepatico-jejunostomy.
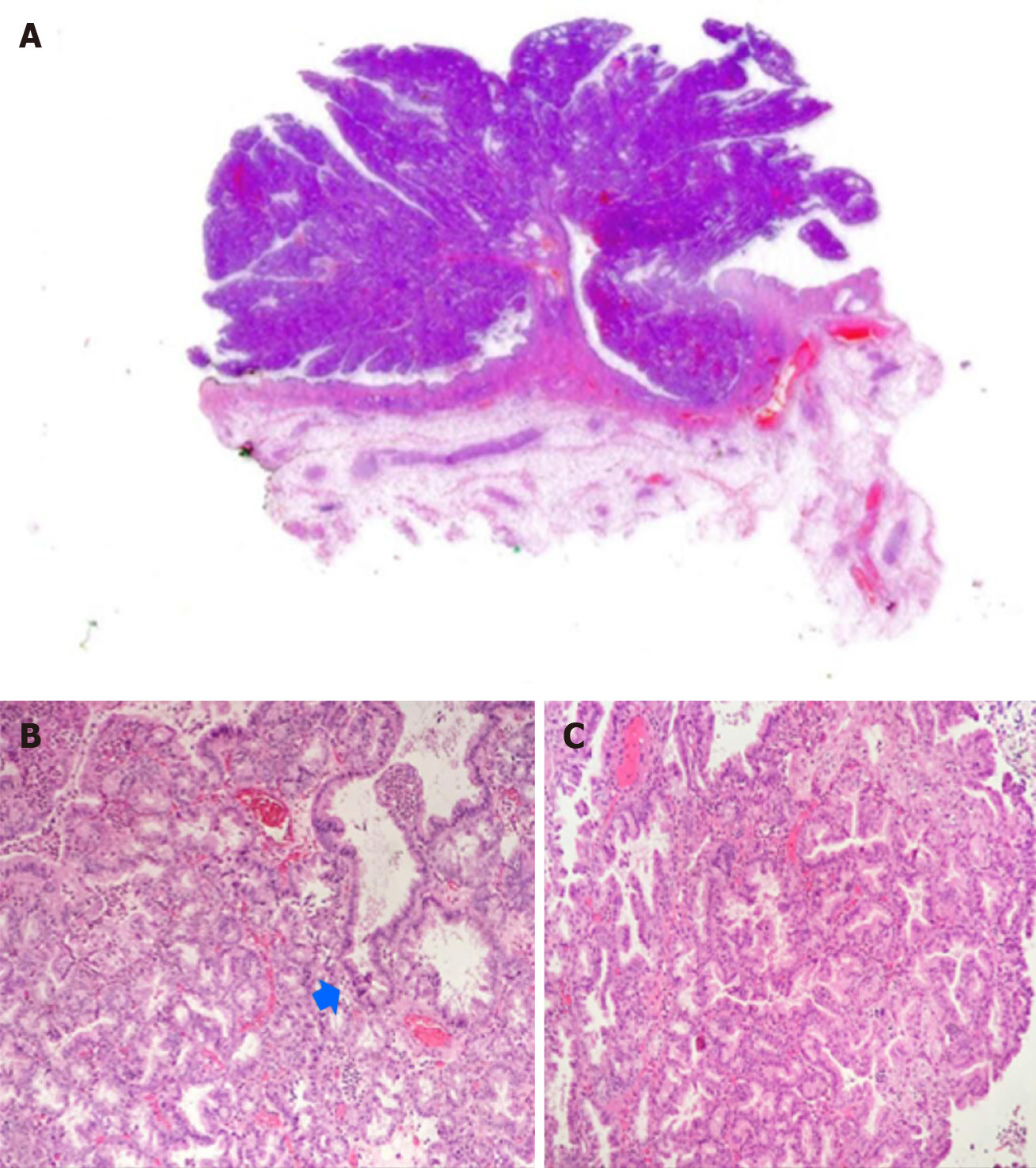
Final pathology showed IPNB within different grades of dysplasia and invasive cancer involving 3% of the lesion, which was radically resected (R0 margins) (Figure 3). The post-operative course was uneventful and a good prognosis is expected at this stage.
POC is an essential tool in the diagnosis and management of undetermined biliary strictures or filling defects, and the accuracy of the direct visual impression during cholangioscopy seems to be greater than that with ERCP. Moreover, POC allows exact localization of the tumor, which is crucial for surgical planning in order to perform a radical resection[3-6].
The SpyGlass technology appears to be crucial for the rapid diagnosis and a clear evaluation of the extension of lesions such as IPNB, which can easily be misdiagnosed due to their mucin production and flat appearance.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Rerknimitr R S-Editor: Chen XF L-Editor: Webster JR P-Editor: Liu JH
| 1. | Nakanuma Y, Kakuda Y, Uesaka K. Characterization of Intraductal Papillary Neoplasm of the Bile Duct with Respect to the Histopathologic Similarities to Pancreatic Intraductal Papillary Mucinous Neoplasm. Gut Liver. 2019;13:617-627. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 43] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 2. | Lendvai G, Szekerczés T, Illyés I, Dóra R, Kontsek E, Gógl A, Kiss A, Werling K, Kovalszky I, Schaff Z, Borka K. Cholangiocarcinoma: Classification, Histopathology and Molecular Carcinogenesis. Pathol Oncol Res. 2020;26:3-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 77] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 3. | Bill JG, Chaterjee D, Mullady DK. Using peroral cholangioscopy to diagnose an intraductal papillary neoplasm of the bile duct. VideoGIE. 2020;5:68-71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Korrapati P, Ciolino J, Wani S, Shah J, Watson R, Muthusamy VR, Klapman J, Komanduri S. The efficacy of peroral cholangioscopy for difficult bile duct stones and indeterminate strictures: a systematic review and meta-analysis. Endosc Int Open. 2016;4:E263-E275. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 81] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 5. | Nanashima A, Imamura N, Hiyoshi M, Hamada T, Yano K, Wada T, Kawakami H, Ban T, Kubota Y, Sato Y, Harada K. Planned limited resection of the extrahepatic bile duct in a case of intraductal papillary neoplasm of the bile duct based on preoperative examinations. Clin J Gastroenterol. 2020;13:233-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Ogawa T, Ito K, Koshita S, Kanno Y, Masu K, Kusunose H, Sakai T, Murabayashi T, Hasegawa S, Noda Y. Usefulness of cholangioscopic-guided mapping biopsy using SpyGlass DS for preoperative evaluation of extrahepatic cholangiocarcinoma: a pilot study. Endosc Int Open. 2018;6:E199-E204. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |