Published online Dec 16, 2020. doi: 10.4253/wjge.v12.i12.532
Peer-review started: August 10, 2020
First decision: September 17, 2020
Revised: October 10, 2020
Accepted: November 29, 2020
Article in press: November 29, 2020
Published online: December 16, 2020
Processing time: 125 Days and 4.6 Hours
Per-oral endoscopic myotomy (POEM) is safe and effective for the treatment of achalasia. There is limited data on performance of POEM in patients with altered upper gastrointestinal anatomy, especially after bariatric surgery. Outcomes in patients with prior sleeve gastrectomy have not been reported.
To assess the efficacy and safety of POEM in patients with prior bariatric surgery.
A prospective POEM database was reviewed from 3/2017-5/2020 to identify patients who underwent POEM after prior bariatric surgery. Efficacy was assessed by technical success (defined as the ability to successfully complete the procedure) and clinical success [decrease in Eckardt score (ES) to ≤ 3 post procedure]. Safety was evaluated by recording adverse events.
Six patients (50% male, mean age 48 years) with a history of prior bariatric surgery who underwent POEM were included. Three had prior sleeve gastrectomy (SG) and three prior Roux-en-Y gastric bypass (RYGB). Four patients had achalasia subtype II and 2 had type I. Most (4) patients had undergone previous achalasia therapy. Technical success was 100%. Clinical success was achieved in 4 (67%) patients at mean follow-up of 21 mo. In one of the clinical failures, EndoFLIP evaluation demonstrated adequate treatment and candida esophagitis was noted as the likely cause of dysphagia. There were no major adverse events.
POEM is technically feasible after both RYGB and SG and offers an effective treatment for this rare group of patients where surgical options for achalasia are limited.
Core Tip: There is limited data on performance of per-oral endoscopic myotomy (POEM) in patients with altered upper gastrointestinal anatomy, especially after bariatric surgery. To our knowledge, performance and outcomes of POEM have not been reported after sleeve gastrectomy, which is the most common surgical bariatric procedure. Given the worldwide epidemic of obesity, gastroenterologists may be increasingly faced with achalasia after bariatric surgery, for which POEM may be a viable endoscopic option. Our results show that POEM can be safely performed for achalasia in the setting of prior bariatric surgery and offers a safe and effective treatment for these patients with limited surgical options.
- Citation: Kolb JM, Jonas D, Funari MP, Hammad H, Menard-Katcher P, Wagh MS. Efficacy and safety of peroral endoscopic myotomy after prior sleeve gastrectomy and gastric bypass surgery. World J Gastrointest Endosc 2020; 12(12): 532-541
- URL: https://www.wjgnet.com/1948-5190/full/v12/i12/532.htm
- DOI: https://dx.doi.org/10.4253/wjge.v12.i12.532
Achalasia is a chronic debilitating condition with an incidence rate of approximately 1.07 per 100000 and likely much higher with increasing awareness and advancements in diagnostic tools for evaluation of dysphagia[1]. It is characterized by loss of peristalsis of the esophageal body and failure of relaxation of the lower esophageal sphincter (LES). Traditional therapies include pneumatic dilation, endoscopic injection of botulinum toxin, and laparoscopic Heller myotomy (LHM), however per-oral endoscopic myotomy (POEM) has more recently emerged as a safe and effective treatment modality for achalasia[2-5]. Randomized clinical trials have demonstrated treatment success with POEM (superior to PD[6] and non-inferior to LHM[7]) though with greater likelihood for reflux esophagitis[8]. POEM can be successfully performed in patients who have had prior endoscopic interventions[9] such as botulinum toxin injection and pneumatic dilation, previous POEM[10], and even after LHM[11]. There is limited data on performance of POEM in patients with altered upper gastrointestinal anatomy, especially after bariatric surgery.
Achalasia can result in dramatic weight loss and thus is not typically thought of as a disease that coexists with obesity. However, reports of achalasia occurring after bariatric surgery exist. Boules et al[12] analyzed patients diagnosed with achalasia over a 12-year period and found a history of bariatric surgery in 3%. While in general the etiology of achalasia is unknown, in this clinical scenario it has been hypothesized that iatrogenic injury from bariatric surgery alters neuromuscular systems creating achalasia-like motility disorders[13]. Additionally, obesity is a known risk factor for esophageal disorders, with approximately 50% of obese patients in one prospective cohort study demonstrating dysmotility on esophageal manometry[14]. Given the worldwide epidemic of obesity, gastroenterologists may be increasingly faced with achalasia after bariatric surgery, for which POEM may be a viable endoscopic option.
Achalasia after bariatric surgery represents a technical challenge for surgical repair. LHM is difficult in this population due to post-surgical anatomy and adhesions[15,16]. In addition, the advantage of combining an anti-reflux procedure during LHM is lost since fundoplication is not feasible after bariatric surgery. POEM after Roux-en-Y gastric bypass (RYGB) has been described in small case series[17,18] with reasonably high technical and clinical success rates and acceptable rates of acid reflux. Performance and outcomes of POEM have not been reported after sleeve gastrectomy (SG), which is the most common bariatric procedure and more likely than RYGB to result in acid reflux[19]. As rates of obesity and bariatric surgery continue to increase, data on the feasibility of POEM after SG will become more important. To address this gap, we assessed efficacy and safety of POEM for achalasia after bariatric surgery.
The study was performed at a tertiary care academic medical center. The prospective POEM database at the University of Colorado Hospital was reviewed to identify patients with a prior history of bariatric surgery who underwent POEM between 3/2017-5/2020. Achalasia was diagnosed by high resolution manometry (HRM) meeting Chicago Classification version 3.0 criteria for Achalasia (type 1, 2 or 3). Pre procedure symptom assessment was performed using the validated Eckardt score (ES) which measures symptoms in 4 categories (dysphagia, regurgitation, chest pain, weight loss) according to frequency (0-3)[20,21] with higher scores indicating more severe symptoms. Patient demographics and clinical data including radiologic examination, diagnostic testing, endoscopy and surgery reports were recorded. This study was approved by the Institutional Review Board.
Patients were asked to stay on a liquid diet for 2 d before the procedure to allow adequate esophageal clearance for visualization during POEM and to minimize risk of adverse events. All procedures were performed in the supine position in the endoscopy unit under general anesthesia with endotracheal intubation. Technique for POEM was as previously described[22,23]. A posterior submucosal tunnel with a posterior myotomy in the 5 o’clock position was performed with the T-type Hybrid knife (ERBE USA, Marietta, GA, United States). Bleeding during the procedure was treated with the dissection knife and/or Coagrasper (Olympus America, Center Valley, PA, United States). The mucosal incision was closed with endoscopic clips (Quick Clip Pro, Olympus America, Center Valley, PA, United States).
As per routine practice in our unit, patients were admitted after their procedure for overnight observation and underwent an esophagram the following morning. If there was no evidence of leak on esophagram patients were started on a clear liquid diet and discharged home. All patients were prescribed one week of oral antibiotics, typically amoxicillin with clavulanic acid (or ciprofloxacin and metronidazole if allergic to penicillin) upon discharge. All patients received a phone call within 72 h after their procedure as per our endoscopy unit protocol to assess for early adverse events. Follow-up data on symptoms and adverse events were obtained from clinical encounters or phone calls through the end of the study period (6/2020). Patients who had recurrent symptoms or asymptomatic individuals who were logistically able to return for endoscopic evaluation underwent upper endoscopy and endoluminal functional lumen imaging probe (EndoFLIP). Reflux esophagitis was categorized according to the Los Angeles Classification and grade C or D were considered significant as per the Lyon consensus[24]. The 16-cm EndoFLIP EF-322N balloon catheter (Medtronic, Minneapolis, MN, United States) was used and a post procedure DI > 2.8 mm2/mmHg at 60 mL was considered as adequate treatment[25].
The main outcomes were efficacy (technical and clinical success) and safety of POEM after prior bariatric surgery. Technical success was defined as the ability to successfully complete submucosal tunneling and endoscopic myotomy of the lower esophagus across the esophagogastric junction (EGJ) and at least 2 cm into the cardia. Clinical success was defined as symptom relief with an ES ≤ 3, which is the most widely used metric for assessing clinical outcomes in achalasia[26]. Intraprocedural and post procedural adverse events were recorded as per published ASGE criteria[27]. Descriptive statistics were used to report continuous variables and time to event data.
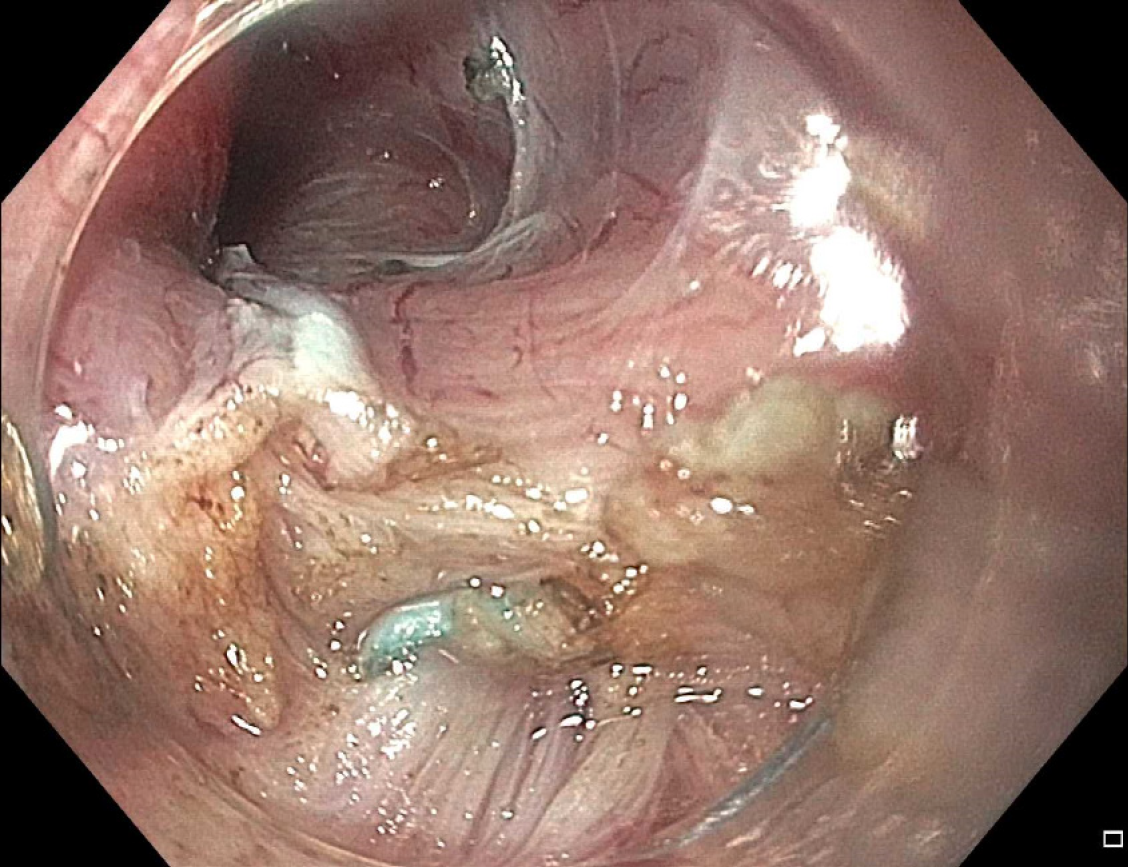
Six patients (50% male, mean age 48 years) with a history of prior bariatric surgery (3 SG, 3 RYGB) who underwent POEM were included (Table 1). Patients had either achalasia subtype 1 (33%) or 2 (67%). Four patients (67%) had undergone prior therapies for achalasia: One patient had prior Heller myotomy, one had botulinum toxin injection and aborted Heller myotomy due to adhesions found during surgery, two patients had previous botulinum toxin injection, and two patients had no previous treatment for achalasia. Mean ES before POEM was 7.6 (range 4-10). POEM was performed at a mean of 84.8 mo after bariatric surgery (range 8-165). The mean myotomy length was 9.3 cm with 2.2 cm extension into the cardia (Table 2). Mean procedure duration was 79.8 min (Range 47-105). During submucosal tunneling in post SG patients, there was appreciable tortuosity and scarring near the EGJ and in one case surgical sutures were encountered and left intact while complete myotomy was performed around them. (Figure 1). Technical success was achieved in all cases (100%).
| Case | Age Sex | Type of bariatric surgery | Pre-POEM Eckardt Score | Achalasia subtype | IRP (normal < 15) | Prior achalasia treatment1 | Months from bariatric surgery to POEM |
| 1 | 54 M | SG | 9 | 1 | NA2 | Heller myotomy | 47 |
| 2 | 68 M | SG | 6 | 2 | 22.2 | Botulinum toxin injection | 71 |
| 3 | 53 F | SG | 7 | 1 | 23.7 | Botulinum toxin injection; Heller myotomy3 | 165 |
| 4 | 43 F | RYGB | 10 | 2 | 21.2 | None | 96 |
| 5 | 31 M | RYGB | 44 | 2 | 28 | Botulinum toxin injection | 84 |
| 6 | 37 F | RYGB | 10 | 2 | 36 | None | 122 |
| POEM Procedural data (n = 6) | Mean (range) |
| Submucosal Tunnel length, cm | 12.3 (11-14) |
| Myotomy length, cm | 9.3 (9-10) |
| Extension of myotomy into cardia, cm | 2.2 (2-3) |
| Clips, number | 5 (3-7) |
| POEM time, min | 79.8 (47-105) |
Clinical success was achieved in 4 (67%) patients (2 SG and 2 RYGB) at a mean follow-up time of 21 mo (1.5-37) (Table 3). One of the clinical failures was in a patient with previous SG whose endoscopic evaluation post-POEM demonstrated recurrent candida esophagitis (white exudates confirmed on pathology) thought to be the cause of persistent dysphagia. EndoFLIP evaluation demonstrated EGJ distensibility index (DI) of 10.2 mm2/mmHg at 60 mL balloon inflation, consistent with adequate treatment. The second clinical failure occurred in a patient with prior RYGB who had a follow up evaluation by telephone and reported ongoing symptoms however despite multiple attempts to schedule her for endoscopic evaluation and further workup she was lost to follow up. Three patients underwent routine post POEM endoscopy (all of whom had prior SG) and LA grade A/B reflux esophagitis was seen in two patients and candida esophagitis in the third patient as described.
| Case | Type of bariatric surgery | Technical success | Clinical success | Post-POEM Eckardt score | Adverse events | Follow up, mo | Endoscopy findings | Medical comorbities |
| 1 | SG | Yes | Yes | 3 | No | 37 | Grade A esophagitis | HTN, HLD |
| 2 | SG | Yes | No | 6 | Minor1 | 21 | Candida esophagitis; EndoFLIP DI: 10.22 | COPD, TIA, OSA, HTN, type 2 diabetes |
| 3 | SG | Yes | Yes | 2 | No | 13 | Grade B esophagitisEndoFLIP DI: 5.13 | None |
| 4 | RYGB | Yes | No | 10 | No | 21 | NA | Major depressive disorder, chronic migraines |
| 5 | RYGB | Yes | Yes | 2 | No | 33 | NA | None |
| 6 | RYGB | Yes | Yes | 2 | No | 1.5 | NA | Hypothyroidism |
There were no intraprocedural adverse events. Esophagram on post-procedure day 1 showed no leak and patients were discharged from the hospital. One patient presented to the emergency room 5 days later due to chest pain and had a negative workup and was discharged home. There were no other adverse events.
Our results show that POEM can be safely performed for achalasia in the setting of prior bariatric surgery and offers a viable treatment for these patients with limited surgical options. In addition, to the best of our knowledge, POEM after SG has not been previously reported.
The main disadvantage of POEM over LHM is that it may cause acid reflux in up to 40% of patients[8]. There have been several published case reports of POEM performed after RYGB[28-30]. In the largest series to date with 10 patients, none experienced regurgitation and the six patients who underwent pH testing had normal results[18]. The present study included 3 patients who had history of RYGB and none developed clinical symptoms of acid reflux during the follow up period. SG is known to promote acid reflux likely as a result of EGJ disruption (more obtuse EGJ insertion angle) and specifically when there is > 80% reduction in gastric capacity[31]. In theory after SG it might be preferable to combine achalasia therapy with anti-reflux treatment through a traditional surgical approach with concomitant Heller myotomy and fundoplication. However, fundoplication is not feasible after SG so surgery no longer offers this benefit over an endoscopic approach. In the 3 patients who had POEM after prior SG, 2 had endoscopic evidence of mild (grade A/B) esophagitis during the follow up period.
There were two patients who did not meet criteria for clinical success at 1 year. The first was a 68-year-old male with a history of SG and an initial ES of 6. This patient noted dramatic improvement after POEM with ES 0 at 6 mo but subsequently developed recurrent dysphagia and regurgitation. Upper endoscopy demonstrated candida esophagitis that was treated with fluconazole resulting in mild improvement in symptoms. Post POEM EndoFLIP findings indicated adequate treatment at the LES (DI 10.2 mm2/mmHg) suggesting that candida infection was potentially causing the symptoms. An alternative possibility for clinical failure is a secondary achalasia from a more distal obstructive process related to the sleeve analogous to the scenario described after lap-band[32,33] Notably, this patient’s pre POEM manometry demonstrated a dual high-pressure zone at the EGJ which could be consistent with a hiatal hernia or with increased pressure distal to the EGJ (i.e., at the sleeve). Additional testing is in progress to elucidate the exact cause for continued symptoms. This case highlights the importance of close collaboration between the endoscopist and esophageal motility expert performing the diagnostic workup.
The second clinical failure was a 43-year-old female with history of RYGB and comorbidities including depression, chronic pain, fibromyalgia, and migraines. This patient was evaluated at our esophageal multidisciplinary clinic and it was unclear if her symptoms were purely related to achalasia or multifactorial. POEM was performed for documented achalasia type II with predominant symptoms of dysphagia and regurgitation (ES 10). Although she did not have clinical success with POEM, symptoms shifted towards less dysphagia and regurgitation, and more chest pain and weight loss. These findings are unusual and highlight the possibility that other underlying conditions may be contributing to ongoing symptoms, especially in bariatric patients with coexistent comorbidities. As highlighted in this case, objective evaluation such as EndoFLIP, HRM, and pH testing should be performed in patients with clinical failure, to determine if symptoms are related to ineffective POEM or other causes.
It would be quite unusual for achalasia patients to develop obesity requiring bariatric surgery. Indeed, most published reports indicate that achalasia developed after bariatric surgery. One proposed theory is that iatrogenic injury during bariatric surgery may promote development of achalasia. This chronology was true for most patients in the present study except for one who had known achalasia preceding RYGB, a sequence that has only been demonstrated in a small number of cases[17]. This patient had been planned to undergo Heller myotomy at the time of bariatric surgery but for unknown reasons this was not done at their local hospital. The best management of concomitant achalasia and obesity is unclear as it is uncommon for these two conditions to co-exist. Oviedo et al[34] reported an interesting case of a young female with obesity and achalasia who chose POEM followed by SG (instead of LHM with RYGB) mainly due to risk of malabsorption in the context of a future planned pregnancy. Recent data suggests that esophageal motility disorders in bariatric patients may be underrecognized or a possible consequence postoperatively, therefore we suggest considering motility testing prior to surgery to assess for silent disease[35], Given the increasing number of bariatric procedures being performed for obesity, surgeons and endoscopists will likely be faced with similarly challenging situations as reported here. Additionally, as POEM gains widespread acceptance for management of achalasia, endoscopists will need to adapt current procedural techniques to unique cases such as surgically altered anatomy. These cases demonstrate that although technically challenging, POEM can be performed after bariatric surgery including sleeve gastrectomy and may be potentially safer than repeat surgery.
It should be mentioned that POEM after bariatric surgery is technically challenging due to surgically altered anatomy with concurrent tortuosity, angulation and scarring, and presence of surgical sutures in the dissection plane. However, careful dissection was feasible. The orientation of the submucosal dissection with reference to the mucosa on one side and the muscle on the other, and direction of the tunnel was constantly checked to ensure safe tunneling without mucosal injury. Also, the reduced gastric lumen in the setting of RYGB or SG did not affect the technical feasibility of performing POEM.
We also acknowledge the limitations of this study. This was a single center series with a small number of patients which may limit generalizability. However, POEM for achalasia after bariatric surgery is a rare clinical scenario with limited reports and therefore sharing each case is valuable. For patients who develop achalasia in the short-term period after bariatric surgery when they have not yet reached their nadir, application of the Eckardt score should take into context ongoing intentional post-operative weight loss. All patients in our series had reached their weight loss nadir except potentially patient number 5 who had POEM 8 mo after RYGB. However, his Eckardt score (4) comprised of dysphagia (2) and regurgitation (2) without weight loss contributing to the ES. Another limitation is the lack of HRM/EndoFLIP and esophageal pH testing in all patients after POEM. This information would be helpful especially in patients with SG which is associated with increased acid reflux, though we did not find any significant grade C/D esophagitis in these patients. Additionally, post-POEM testing was only performed in some patients since these cases were performed at a tertiary referral center, and thus due to geographic distance and insurance restrictions not all patients were able to follow up at our institution. To mitigate this limitation, we communicated with all patients by phone to obtain symptom assessment. Lastly, this study was performed at a tertiary academic medical center with an established POEM program and results may not be applicable to other centers. Due to the technical complexity associated with these cases, we suggest that POEM after bariatric surgery should be performed by endoscopists with significant experience in standard POEM.
In the past 2 decades, the age-adjusted prevalence of obesity in the United States increased from 30.5% to 42.4% and severe obesity nearly doubled from 4.7% to 9.2%[36]. This increase is coupled with a parallel 10.8% increase in utilization of bariatric surgery from 2017 to 2018 alone[19]. Therefore this clinical scenario of achalasia post bariatric surgery may become more common. As more evidence accumulates regarding the safety and efficacy of POEM, these cases add to the growing scientific literature regarding performance of POEM in surgically altered anatomy. In conclusion, these cases demonstrate the safety and feasibility of POEM after RYGB and SG.
Per-oral endoscopic myotomy (POEM) is a safe and effective treatment for achalasia, but in patients with prior bariatric surgery the altered gastrointestinal tract anatomy can pose a technical challenge.
Currently there is sparse published data on efficacy and feasibility of POEM in patients with prior Roux-en-Y gastric bypass (RYGB) and no published reports in patients with prior sleeve gastrectomy (SG).
To describe the safety, feasibility and clinical outcomes of POEM in patients with history of bariatric surgery.
Six patients with prior bariatric surgery who underwent POEM for achalasia were included. Technical success defined as the ability to successfully complete the procedure and clinical success defined as a post procedure Eckardt score ≤ 3 were evaluated. Adverse events were recorded for safety outcomes.
Six patients (50% male, mean age 48 years) with a history of prior bariatric surgery (3 RYGB, 3 SG) underwent POEM. Four patients had Achalasia Type II and two had Achalasia Type 1. Technical success was 100%. Clinical success was achieved in 4 (67%) patients at mean follow-up of 21 mo. One clinical failure was likely a result of candida esophagitis causing dysphagia since EndoFLIP demonstrated adequate myotomy. There were no major adverse events.
POEM is technically feasible after both RYGB and SG and offers an effective treatment for this rare group of patients where surgical options for achalasia are limited.
Future prospective studies are needed to compare outcomes in patients undergoing POEM after RYGB vs SG and to define predictors for clinical success.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: American Society for Gastrointestinal Endoscopy, No. 101273; and American College of Gastroenterology, No. 22367.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Borbély Y, Tartaglia N S-Editor: Gao CC L-Editor: A P-Editor: Wang LL
| 1. | Samo S, Carlson DA, Gregory DL, Gawel SH, Pandolfino JE, Kahrilas PJ. Incidence and Prevalence of Achalasia in Central Chicago, 2004-2014, Since the Widespread Use of High-Resolution Manometry. Clin Gastroenterol Hepatol. 2017;15:366-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 107] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 2. | Akintoye E, Kumar N, Obaitan I, Alayo QA, Thompson CC. Peroral endoscopic myotomy: a meta-analysis. Endoscopy. 2016;48:1059-1068. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 173] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 3. | Inoue H, Sato H, Ikeda H, Onimaru M, Sato C, Minami H, Yokomichi H, Kobayashi Y, Grimes KL, Kudo SE. Per-Oral Endoscopic Myotomy: A Series of 500 Patients. J Am Coll Surg. 2015;221:256-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 328] [Cited by in RCA: 349] [Article Influence: 34.9] [Reference Citation Analysis (0)] |
| 4. | Crespin OM, Liu LWC, Parmar A, Jackson TD, Hamid J, Shlomovitz E, Okrainec A. Safety and efficacy of POEM for treatment of achalasia: a systematic review of the literature. Surg Endosc. 2017;31:2187-2201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 71] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 5. | Shiwaku H, Inoue H, Sato H, Onimaru M, Minami H, Tanaka S, Sato C, Ogawa R, Okushima N, Yokomichi H. Peroral endoscopic myotomy for achalasia: a prospective multicenter study in Japan. Gastrointest Endosc 2020; 91: 1037-1044. e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 61] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 6. | Ponds FA, Fockens P, Lei A, Neuhaus H, Beyna T, Kandler J, Frieling T, Chiu PWY, Wu JCY, Wong VWY, Costamagna G, Familiari P, Kahrilas PJ, Pandolfino JE, Smout AJPM, Bredenoord AJ. Effect of Peroral Endoscopic Myotomy vs Pneumatic Dilation on Symptom Severity and Treatment Outcomes Among Treatment-Naive Patients With Achalasia: A Randomized Clinical Trial. JAMA. 2019;322:134-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 260] [Article Influence: 43.3] [Reference Citation Analysis (0)] |
| 7. | Werner YB, Hakanson B, Martinek J, Repici A, von Rahden BHA, Bredenoord AJ, Bisschops R, Messmann H, Vollberg MC, Noder T, Kersten JF, Mann O, Izbicki J, Pazdro A, Fumagalli U, Rosati R, Germer CT, Schijven MP, Emmermann A, von Renteln D, Fockens P, Boeckxstaens G, Rösch T. Endoscopic or Surgical Myotomy in Patients with Idiopathic Achalasia. N Engl J Med. 2019;381:2219-2229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 398] [Cited by in RCA: 345] [Article Influence: 57.5] [Reference Citation Analysis (1)] |
| 8. | Repici A, Fuccio L, Maselli R, Mazza F, Correale L, Mandolesi D, Bellisario C, Sethi A, Khashab MA, Rösch T, Hassan C. GERD after per-oral endoscopic myotomy as compared with Heller's myotomy with fundoplication: a systematic review with meta-analysis. Gastrointest Endosc 2018; 87: 934-943. e18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 182] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 9. | Tang X, Gong W, Deng Z, Zhou J, Ren Y, Zhang Q, Chen Z, Jiang B. Feasibility and safety of peroral endoscopic myotomy for achalasia after failed endoscopic interventions. Dis Esophagus. 2017;30:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Tyberg A, Seewald S, Sharaiha RZ, Martinez G, Desai AP, Kumta NA, Lambroza A, Sethi A, Reavis KM, DeRoche K, Gaidhane M, Talbot M, Saxena P, Zamarripa F, Barret M, Eleftheriadis N, Balassone V, Inoue H, Kahaleh M. A multicenter international registry of redo per-oral endoscopic myotomy (POEM) after failed POEM. Gastrointest Endosc. 2017;85:1208-1211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 58] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 11. | Ngamruengphong S, Inoue H, Ujiki MB, Patel LY, Bapaye A, Desai PN, Dorwat S, Nakamura J, Hata Y, Balassone V, Onimaru M, Ponchon T, Pioche M, Roman S, Rivory J, Mion F, Garros A, Draganov PV, Perbtani Y, Abbas A, Pannu D, Yang D, Perretta S, Romanelli J, Desilets D, Hayee B, Haji A, Hajiyeva G, Ismail A, Chen YI, Bukhari M, Haito-Chavez Y, Kumbhari V, Saxena P, Talbot M, Chiu PW, Yip HC, Wong VW, Hernaez R, Maselli R, Repici A, Khashab MA. Efficacy and Safety of Peroral Endoscopic Myotomy for Treatment of Achalasia After Failed Heller Myotomy. Clin Gastroenterol Hepatol 2017; 15: 1531-1537. e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 105] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 12. | Boules M, Corcelles R, Zelisko A, Batayyah E, Froylich D, Rodriguez J, Brethauer S, El-Hayek K, Kroh M. Achalasia After Bariatric Surgery. J Laparoendosc Adv Surg Tech A. 2016;26:428-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 13. | Shah RN, Izanec JL, Friedel DM, Axelrod P, Parkman HP, Fisher RS. Achalasia presenting after operative and nonoperative trauma. Dig Dis Sci. 2004;49:1818-1821. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Côté-Daigneault J, Leclerc P, Joubert J, Bouin M. High prevalence of esophageal dysmotility in asymptomatic obese patients. Can J Gastroenterol Hepatol. 2014;28:311-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 15. | Aiolfi A, Tornese S, Bonitta G, Rausa E, Micheletto G, Bona D. Management of Esophageal Achalasia after Roux-en-Y Gastric Bypass: Narrative Review of the Literature. Obes Surg. 2019;29:1632-1637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Andolfi C, Fisichella PM. Laparoscopic Heller Myotomy and Dor Fundoplication for Esophageal Achalasia: Technique and Perioperative Management. J Laparoendosc Adv Surg Tech A. 2016;26:916-920. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Bashir U, El Abiad R, Gerke H, Keech J, Parekh K, Nau P. Peroral Endoscopic Myotomy Is Feasible and Safe in a Gastric Bypass Population. Obes Surg. 2019;29:3523-3526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Sanaei O, Draganov P, Kunda R, Yang D, Khashab MA. Peroral endoscopic myotomy for the treatment of achalasia patients with Roux-en-Y gastric bypass anatomy. Endoscopy. 2019;51:342-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 19. | English WJ, DeMaria EJ, Hutter MM, Kothari SN, Mattar SG, Brethauer SA, Morton JM. American Society for Metabolic and Bariatric Surgery 2018 estimate of metabolic and bariatric procedures performed in the United States. Surg Obes Relat Dis. 2020;16:457-463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 227] [Article Influence: 45.4] [Reference Citation Analysis (0)] |
| 20. | Taft TH, Carlson DA, Triggs J, Craft J, Starkey K, Yadlapati R, Gregory D, Pandolfino JE. Evaluating the reliability and construct validity of the Eckardt symptom score as a measure of achalasia severity. Neurogastroenterol Motil. 2018;30:e13287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 81] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 21. | Eckardt VF, Aignherr C, Bernhard G. Predictors of outcome in patients with achalasia treated by pneumatic dilation. Gastroenterology. 1992;103:1732-1738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 483] [Cited by in RCA: 523] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 22. | Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42:265-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1168] [Cited by in RCA: 1234] [Article Influence: 82.3] [Reference Citation Analysis (1)] |
| 23. | Mittal C, Wagh MS. Technical Advances in Per-Oral Endoscopic Myotomy (POEM). Am J Gastroenterol. 2017;112:1627-1631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Gyawali CP, Kahrilas PJ, Savarino E, Zerbib F, Mion F, Smout AJPM, Vaezi M, Sifrim D, Fox MR, Vela MF, Tutuian R, Tack J, Bredenoord AJ, Pandolfino J, Roman S. Modern diagnosis of GERD: the Lyon Consensus. Gut. 2018;67:1351-1362. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 672] [Cited by in RCA: 945] [Article Influence: 135.0] [Reference Citation Analysis (0)] |
| 25. | Carlson DA, Gyawali CP, Kahrilas PJ, Triggs JR, Falmagne S, Prescott J, Dorian E, Kou W, Lin Z, Pandolfino JE. Esophageal motility classification can be established at the time of endoscopy: a study evaluating real-time functional luminal imaging probe panometry. Gastrointest Endosc 2019; 90: 915-923. e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 49] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 26. | Khashab MA, Vela MF, Thosani N, Agrawal D, Buxbaum JL, Abbas Fehmi SM, Fishman DS, Gurudu SR, Jamil LH, Jue TL, Kannadath BS, Law JK, Lee JK, Naveed M, Qumseya BJ, Sawhney MS, Yang J, Wani S. ASGE guideline on the management of achalasia. Gastrointest Endosc 2020; 91: 213-227. e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 133] [Article Influence: 26.6] [Reference Citation Analysis (0)] |
| 27. | Cotton PB, Eisen GM, Aabakken L, Baron TH, Hutter MM, Jacobson BC, Mergener K, Nemcek A Jr, Petersen BT, Petrini JL, Pike IM, Rabeneck L, Romagnuolo J, Vargo JJ. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc. 2010;71:446-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1238] [Cited by in RCA: 1850] [Article Influence: 123.3] [Reference Citation Analysis (1)] |
| 28. | Lyngsø J, Pedersen JB, Rask P, Kunda R, Bjerregaard NC. [Concurrent achalasia and severe obesity]. Ugeskr Laeger. 2016;178. [PubMed] |
| 29. | Yang D, Draganov PV. Peroral endoscopic myotomy (POEM) for achalasia after Roux-en-Y gastric bypass. Endoscopy. 2014;46 Suppl 1 UCTN:E11-E12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 30. | Luo RB, Montalvo D, Horgan S. Peroral endoscopic myotomy after gastric bypass: An effective solution for de novo achalasia. Surg Obes Relat Dis. 2017;13:e1-e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 31. | Quero G, Fiorillo C, Dallemagne B, Mascagni P, Curcic J, Fox M, Perretta S. The Causes of Gastroesophageal Reflux after Laparoscopic Sleeve Gastrectomy: Quantitative Assessment of the Structure and Function of the Esophagogastric Junction by Magnetic Resonance Imaging and High-Resolution Manometry. Obes Surg. 2020;30:2108-2117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 43] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 32. | Kia L, Kahrilas PJ. An unusual complication after laparoscopic gastric lap band placement. Gastroenterology. 2014;147:e9-e10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 33. | Khan A, Ren-Fielding C, Traube M. Potentially reversible pseudoachalasia after laparoscopic adjustable gastric banding. J Clin Gastroenterol. 2011;45:775-779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 46] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 34. | Oviedo RJ, Sofiak CW, Dixon BM. Achalasia: A case report on its effect during surgical decision making for laparoscopic sleeve gastrectomy in the young morbidly obese patient. Int J Surg Case Rep. 2016;26:4-6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 35. | Miller AT, Matar R, Abu Dayyeh BK, Beran A, Vela MF, Lacy BE, Crowell MD, Geno DM, Lavey CJ, Katzka DA, Ravi K. Postobesity Surgery Esophageal Dysfunction: A Combined Cross-Sectional Prevalence Study and Retrospective Analysis. Am J Gastroenterol. 2020;115:1669-1680. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 38] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 36. | Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of Obesity and Severe Obesity Among Adults: United States, 2017-2018. NCHS Data Brief. 2020;(360):1-8. [PubMed] |