Published online Nov 16, 2020. doi: 10.4253/wjge.v12.i11.488
Peer-review started: June 19, 2020
First decision: August 22, 2020
Revised: September 15, 2020
Accepted: October 9, 2020
Article in press: October 9, 2020
Published online: November 16, 2020
Processing time: 149 Days and 22.9 Hours
Head pancreatic cancers often present with clinical challenges requiring biliary drainage for chemotherapy or palliative scope. If usual endoscopic modalities fail or if percutaneous approach is not feasible, endoscopic ultrasound (EUS) guided biliary drainage can be considered. Here we describe and discuss an interesting clinical case in which EUS-guided gallbladder drainage (EUS-GBD) was chosen to treat acute severe cholangitis in a patient with advanced pancreatic cancer.
An 84-year-old female with a previous EUS-biopsy proven diagnosis of head pancreatic cancer presented with clinical signs of acute cholangitis. In September 2018 she had positioned a biliary and duodenal stent to relieve jaundice and an initial duodenal substenosis. In the emergency ward, an abdominal computed tomography scan showed proximal biliary stent occlusion due to neoplastic progression, but endoscopic retrograde cholangiopancreatography was impossible because of worsening duodenal stenosis and the absence of a chance to reach the Vater’s papilla area. EUS-guided choledocoduodenostomy was not technically feasible but because the cystic duct was free of neoplastic infiltration, an EUS-GBD using an Axios™ stent was successfully performed. The patient started to feed after 48 h and was discharged 1 wk later. No other hospitalizations due to cholangitis or symptoms of Axios™ stent occlusion/dysfunction were observed up until her death 6 mo later due to underlying disease.
This case demonstrated how different EUS therapeutic approaches could have a key role to treat critical and seemingly unsolvable situations and that they could play a more fundamental role in the next future.
Core Tip: The present case explored the feasibility, safety and efficacy of an endoscopic ultrasound-guided gallbladder drainage to decompress the biliary tree and treat severe cholangitis in a patient with advanced pancreatic cancer. Endoscopic ultrasound-guided gallbladder drainage could be effective to drain the biliary tree if the cystic duct is free from neoplastic tissue. Using the new lumen-apposing self-expandable metallic stent, the procedure could be technically and clinically feasible, safe and an effective alternative to conventional endoscopic retrograde cholangiopancreatography or percutaneous drainage.
- Citation: de Nucci G, Imperatore N, Picascia D, Mandelli ED, Bezzio C, Omazzi B, Arena I, Larghi A, Manes G. Endoscopic ultrasound-guided gallbladder drainage in pancreatic cancer and cholangitis: A case report. World J Gastrointest Endosc 2020; 12(11): 488-492
- URL: https://www.wjgnet.com/1948-5190/full/v12/i11/488.htm
- DOI: https://dx.doi.org/10.4253/wjge.v12.i11.488
Malignant neoplasms of the pancreatic head often present with clinical challenges requiring biliary drainage before upfront chemotherapy or palliative treatment[1]. When endoscopic retrograde cholangiopancreatography (ERCP) fails due to anatomical or technical difficulties, the use of endoscopic ultrasound (EUS)-guided biliary drainage could be more appropriate than the percutaneous approach[2]. Moreover, some authors have proposed EUS-guided gallbladder drainage (EUS-GBD) as another alternative to drain the biliary tree if the cystic duct is not entrapped by neoplastic tissue[3,4]. Gallbladder drainage has been simplified by the development of dedicated enhanced lumen-apposing self-expandable metallic stents that create a stable fistula between the gallbladder and the lumen of the stomach or the duodenum. This approach has been recently reported to be more effective than percutaneous drainage to treat high-risk surgical patients with acute cholecystitis[5]. We herein report a case of a patient with a known pancreatic head cancer already previously treated with endoscopic stenting who required urgent biliary decompression through cholecystoduodenostomy for severe acute cholangitis.
An 84-year-old female presented to our Emergency Unit with fever (max 39.5 C), jaundice and leukocytosis.
The clinical data suggested a diagnosis of acute cholangitis due to the occlusion of a biliary metal stent positioned previously.
In September 2018, the patient had a diagnosis of an EUS biopsy proven unresectable pancreatic head cancer with biliary, and a duodenal stent was placed to relieve jaundice and symptomatic duodenal substenosis.
She had a familial history of colorectal cancer (her sister).
On presentation her vital signs were temperature of 39.5 °C, pulse of 115 bpm, respiratory rate of 17 rpm, blood pressure of 80/50 mmHg and oxygen saturation of 92%. On general physical examination she looked pale and dehydrated. Abdominal examination revealed nondistended, tender abdomen in the right hypochondrium with a reduction of bowel sounds. The cardiovascular, pulmonary and neurological examination were unremarkable.
Complete blood count analysis revealed a huge increase of the white blood cells (24754 cells/mL) and a significant increase of liver cytolysis and cholestasis enzymes: Aspartate aminotransferase 123 U/L, alanine aminotransferase 234 U/L and gamma-glutamyltransferase 431 U/L.
Abdominal computed tomography scan showed proximal biliary stent occlusion due to neoplastic progression with presence of stones above it. An ERCP was attempted, but access to the biliary tree was impossible because of worsening duodenal stenosis with complete incorporation of the metallic duodenal stent.
In an effort to avoid placement of a percutaneous drainage and due to the presence of new metastatic hepatic lesions, a multidisciplinary team discussed the case and decided to propose a further EUS evaluation with the aim of performing an alternative drainage procedure.
Acute cholangitis due to biliary metallic stent occlusion in advanced pancreatic cancer with duodenal infiltration and stenosis.
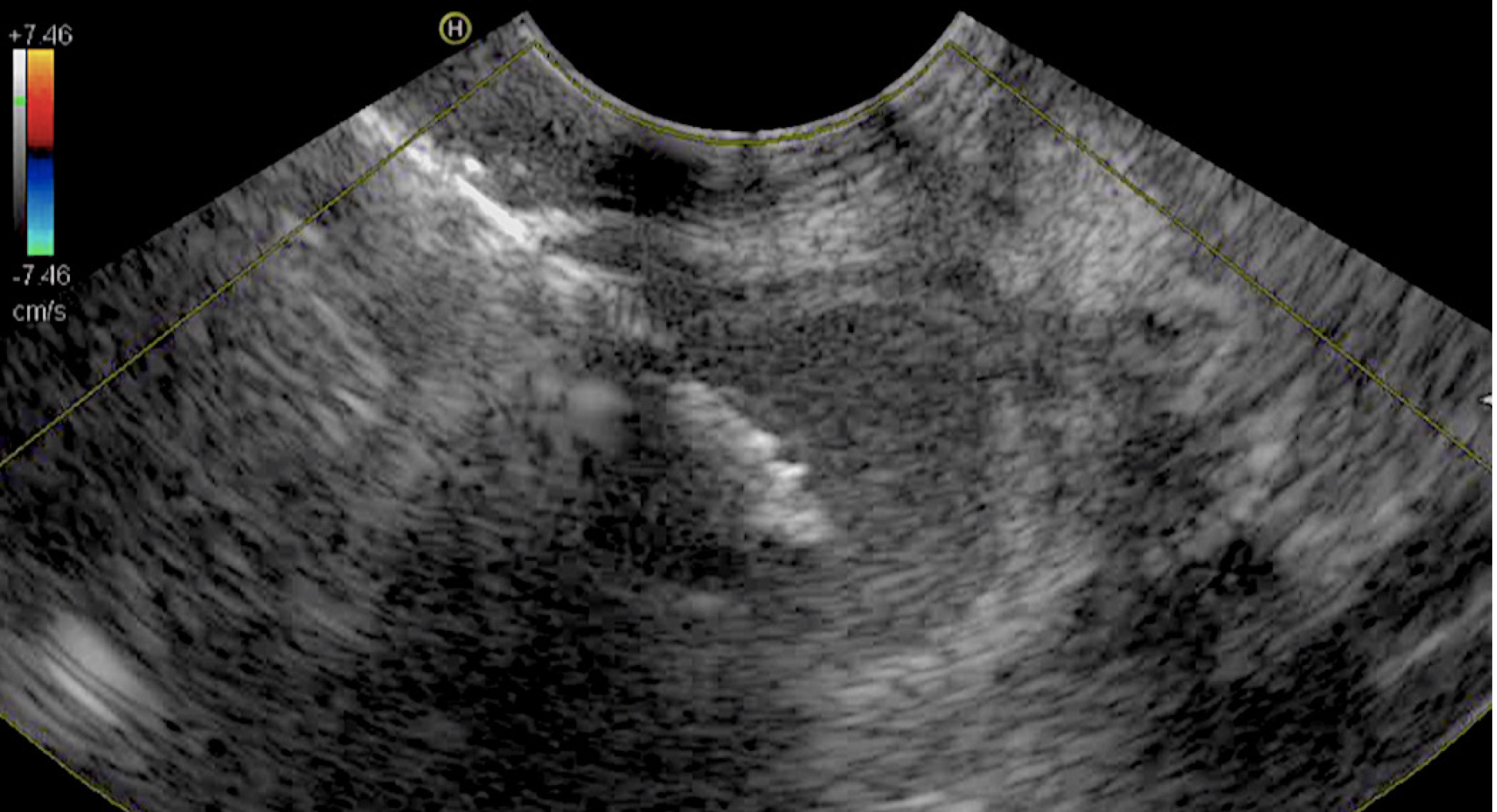
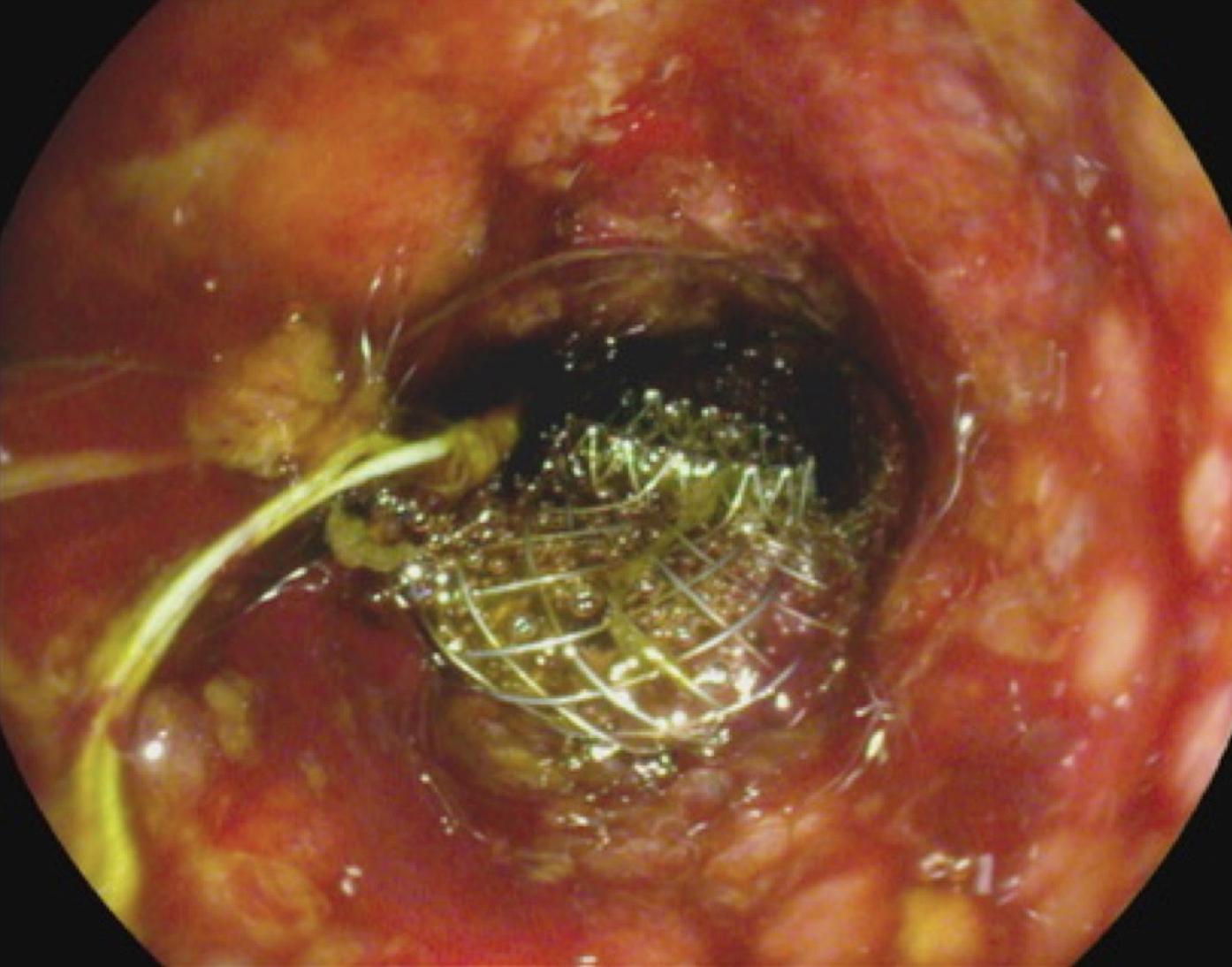
Because of the absence of a suitable sonographic window above the biliary obstruction, EUS-guided choledocoduodenostomy was not technically feasible. On the other hand, the cystic duct appeared to be free of neoplastic infiltration, thus we decided to perform an EUS-GBD using an Axios™ stent plus electrocautery enhanced delivery system. The gallbladder was best visualized from the duodenum and penetrated with EC-Axios by applying cautery. A 10 mm × 10 mm Axios™ stent (Figure 1 and Video 1) was placed under EUS guidance from the duodenal bulb through the stent wire meshes into the gallbladder.
The procedure was technically successful without short- and long-term adverse events (Figure 2) and with a dramatic decrease in bilirubin concentration (2.7 mg/dL) and progressive normalization of inflammatory indexes. The patient started to feed after 48 h and was discharged 1 wk later after full antibiotic treatment was completed. No other hospitalizations due to cholangitis or symptoms of the Axios™ stent occlusion/dysfunction were observed before the patient died due to her underlying disease 6 mo later.
ERCP is the gold standard to treat obstructive jaundice due to malignant distal biliary obstruction[6]. However, ERCP can fail or be impossible in cases of duodenal stenosis, no access to Vater’s papilla zone or altered postsurgical anatomy. In these cases, EUS-guided biliary drainage techniques, such as EUS-guided rendezvous, EUS-guided choledochoduodenostomy and EUS-guided hepaticogastrostomy are all recognized alternative modalities that have a better outcome than percutaneous drainage[7,8].
Recently, several studies demonstrated that EUS-GBD is useful to treat acute cholecystitis in patients unfit for surgery because of its similarity to percutaneous transhepatic gallbladder in terms of efficacy and safety[9]. Thus, when ERCP and EUS-biliary drainage cannot be performed for technical reasons, EUS-GBD may be a suitable alternative given that the gallbladder is a large organ with better accessibility by EUS from the gastric antrum or duodenal bulb[10].
The key factor to perform an effective EUS-GBD in this clinical scenario was lack of involvement of the cystic duct by the tumor. In our case, we performed EUS-GBD as a rescue procedure to treat severe acute cholangitis in a patient with advanced pancreatic neoplasia, in whom previous biliary and duodenal stenting were done. Before performing drainage, careful visualization of the pancreatic mass and lack of involvement of the cystic duct were done, followed by the drainage procedure that was technically and clinically successful as demonstrated by the rapid decrease of the patient’s inflammatory indexes, disappearance of the septic status and normalization of the bilirubin. The persistent clinical success was demonstrated by the absence of further episodes of jaundice or cholangitis.
In conclusion, our report showed that EUS-GBD could be a useful option to obtain an effective biliary drainage in patients in which conventional ERCP or EUS-guided choledocoduodenostomy could not be performed or were unsuccessful.
Manuscript source: Unsolicited manuscript
Corresponding Author’s Membership in Professional Societies: Società Italiana Di Gastroenterologia Ed Endoscopia Digestiva, No. 15757.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Ciaccio EJ, Luo HS S-Editor: Zhang H L-Editor: Filipodia P-Editor: Wang LL
| 1. | Iwashita T, Doi S, Yasuda I. Endoscopic ultrasound-guided biliary drainage: a review. Clin J Gastroenterol. 2014;7:94-102. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 92] [Cited by in RCA: 106] [Article Influence: 9.6] [Reference Citation Analysis (1)] |
| 2. | Sharaiha RZ, Khan MA, Kamal F, Tyberg A, Tombazzi CR, Ali B, Tombazzi C, Kahaleh M. Efficacy and safety of EUS-guided biliary drainage in comparison with percutaneous biliary drainage when ERCP fails: a systematic review and meta-analysis. Gastrointest Endosc. 2017;85:904-914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 224] [Cited by in RCA: 285] [Article Influence: 35.6] [Reference Citation Analysis (2)] |
| 3. | Itoi T, Binmoeller K, Itokawa F, Umeda J, Tanaka R. Endoscopic ultrasonography-guided cholecystogastrostomy using a lumen-apposing metal stent as an alternative to extrahepatic bile duct drainage in pancreatic cancer with duodenal invasion. Dig Endosc. 2013;25 Suppl 2:137-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 34] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 4. | Imai H, Kitano M, Omoto S, Kadosaka K, Kamata K, Miyata T, Yamao K, Sakamoto H, Harwani Y, Kudo M. EUS-guided gallbladder drainage for rescue treatment of malignant distal biliary obstruction after unsuccessful ERCP. Gastrointest Endosc. 2016;84:147-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 79] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 5. | Teoh AYB, Kitano M, Itoi T, Pérez-Miranda M, Ogura T, Chan SM, Serna-Higuera C, Omoto S, Torres-Yuste R, Tsuichiya T, Wong KT, Leung CH, Chiu PWY, Ng EKW, Lau JYW. Endosonography-guided gallbladder drainage versus percutaneous cholecystostomy in very high-risk surgical patients with acute cholecystitis: an international randomised multicentre controlled superiority trial (DRAC 1). Gut. 2020;69:1085-1091. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 191] [Article Influence: 38.2] [Reference Citation Analysis (2)] |
| 6. | Will U, Thieme A, Fueldner F, Gerlach R, Wanzar I, Meyer F. Treatment of biliary obstruction in selected patients by endoscopic ultrasonography (EUS)-guided transluminal biliary drainage. Endoscopy. 2007;39:292-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 107] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 7. | Burmester E, Niehaus J, Leineweber T, Huetteroth T. EUS-cholangio-drainage of the bile duct: report of 4 cases. Gastrointest Endosc. 2003;57:246-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 216] [Cited by in RCA: 196] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 8. | Anderloni A, Attili F, Sferrazza A, Rimbaș M, Costamagna G, Repici A, Larghi A. EUS-guided gallbladder drainage using a lumen-apposing self-expandable metal stent in patients with coagulopathy or anticoagulation therapy: a case series. Endosc Int Open. 2017;5:E1100-E1103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 9. | Maekawa S, Nomura R, Murase T, Ann Y, Oeholm M, Harada M. Endoscopic gallbladder stenting for acute cholecystitis: a retrospective study of 46 elderly patients aged 65 years or older. BMC Gastroenterol. 2013;13:65. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 66] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 10. | Chang JI, Dong E, Kwok KK. Endoscopic ultrasound-guided transmural gallbladder drainage in malignant obstruction using a novel lumen-apposing stent: a case series (with video). Endosc Int Open. 2019;7:E655-E661. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |