Published online Nov 16, 2020. doi: 10.4253/wjge.v12.i11.459
Peer-review started: June 18, 2020
First decision: September 11, 2020
Revised: September 26, 2020
Accepted: October 26, 2020
Article in press: October 26, 2020
Published online: November 16, 2020
Processing time: 150 Days and 13.9 Hours
Retrograde single balloon enteroscopy (SBE) is a minimally invasive procedure which is less frequently performed compared with antegrade SBE. There are few studies on the retrograde through–the-scope enteroscopy (TTSE), a novel technique for evaluation of the small bowel.
To compare the clinical utility and safety of retrograde TTSE with retrograde SBE.
Clinical data and complications of retrograde TTSE (2014-2018) and retrograde SBE (2011-2018) performed in a community hospital were reviewed and presented as mean ± SD or frequency (%) and compared using proper statistical tests. Technical success was defined as insertion of the enteroscope > 20 cm beyond ileocecal valve.
Data obtained from 54 retrograde SBE in 49 patients and 27 retrograde TTSE in 26 patients were studied. The most common indication for retrograde enteroscopy was iron deficiency anemia (41 patients) followed by gastrointestinal bleeding (37 patients), and chronic diarrhea (7 patients). The duration of retrograde SBE procedure (91.9 ± 34.2 min) was significantly longer compared with retrograde TTSE (70.5 ± 30.7 min) (P = 0.04). Technical success was comparable in TTSE [23/27 (85.2%)] and SBE [41/54 (75.9%) (P = 0.33)]. The mean depth of insertion beyond the ileocecal valve in retrograde SBE (92.5 ± 70.0 cm) tended to be longer compared with retrograde TTSE (64.6 ± 49.0 cm) (P = 0.08). No complication was observed in this study.
Both retrograde TTSE and retrograde SBE are feasible and safe. Retrograde TTSE takes a shorter time and has a comparable technical success with SBE. TTSE has a lower capacity of small bowel insertion.
Core Tip: Retrograde single balloon enteroscopy (SBE) and retrograde through–the-scope enteroscopy (TTSE) are minimally invasive procedures with limited data available about their value in the management of small intestinal pathologies. This study compared the clinical utility and safety of retrograde TTSE with retrograde SBE and found them to be feasible and safe with a shorter procedure time for retrograde TTSE and a comparable technical success with SBE.
- Citation: Jia Y, Michael M, Bashashati M, Elhanafi S, Dodoo C, Dwivedi AK, Carrion AF, Othman MO, Zuckerman MJ. Evaluation of the diagnostic and therapeutic utility of retrograde through-the-scope balloon enteroscopy and single-balloon enteroscopy. World J Gastrointest Endosc 2020; 12(11): 459-468
- URL: https://www.wjgnet.com/1948-5190/full/v12/i11/459.htm
- DOI: https://dx.doi.org/10.4253/wjge.v12.i11.459
The small bowel used to be inaccessible and out of reach by gastrointestinal endoscopists because of its depth, length and complex loops. For many decades, the only available diagnostic and therapeutic interventions for evaluation and management of small bowel disorders were radiographic imaging, laparotomy and intraoperative enteroscopy[1-3]. Video capsule endoscopy (VCE) revolutionized the evaluation of small bowel disorders due to its non-invasive nature and higher diagnostic yield compared with conventional imaging modalities, but remains a purely diagnostic modality without any interventional capability[4,5]. While current guidelines suggest VCE to be the first-line endoluminal intervention for suspected small bowel disorders[6], deep enteroscopy may be considered as the initial diagnostic procedure in select patients with a high level of suspicion of small-bowel angioectasias or in patients with surgically altered anatomy[7,8].
Balloon-assisted enteroscopy provides a minimally invasive diagnostic and therapeutic approach to the small bowel allowing real-time endoscopic assessment, tissue sampling and therapeutic interventions extending beyond the diagnostic capabilities of capsule endoscopy and radiographic imaging[9,10]. Single-balloon enteroscopy (SBE) is now available in many centers; however, the availability of double balloon enteroscopy and spiral enteroscopy is limited[11].
Diagnostic and therapeutic enteroscopy has two major routes, antegrade and retrograde enteroscopy. The technically easier route, antegrade SBE, is usually performed first for small bowel disorders of uncertain location. Retrograde SBE is more difficult and less commonly performed than antegrade, but can approach average insertion depths proximal to the ileocecal valve from 73 to 199 cm[11-13].
A new enteroscopy device has been designed to allow deep enteroscopy with a novel through–the-scope balloon [NaviAid (SMART Medical Systems Ltd, Ra'anana, Israel)][14,15]. This technique was introduced as a safe and effective way to perform deep enteroscopy by using a conventional colonoscope without the need for an enteroscope or an overtube. The ASGE guideline has not sufficiently elaborated on this newly introduced technique due to limited data regarding the use of this device for deep enteroscopy[16]. We conducted the current study to evaluate the clinical utility of retrograde TTSE and its impact on the diagnosis and management of small-bowel disorders and to compare both clinical and procedure characteristics of retrograde TTSE with retrograde SBE.
We collected data from consecutive adult patients (> 18 years old) who underwent retrograde balloon-assisted enteroscopy procedures at the University Medical Center in El Paso, a general hospital along the United States-Mexico border. The retrograde SBE studies were performed in the period from September 2011 to December 2018. The TTSE device was introduced after June 2014 and procedures were reviewed to December 2018. After June 2014, every other case was done with alternating retrograde enteroscopy methods depending on equipment availability. There were no preset criteria to prefer one technique over the other. This resulted in an approximately one to one allocation assignment. Double-balloon enteroscopy or the spiral-assisted enteroscopy system were not available at this institution. The study was approved by the Texas Tech University Health Sciences Center Institutional Review Board.
Patient demographics, clinical characteristics, endoscopy procedure data and complications were reviewed. The electronic medical record was used to obtain information about patient demographics and clinical characteristics, use of prior VCE and documented adverse effects, enteroscopy procedure data (routes, duration of procedures, depth of insertion for successful endoscopy cases, diagnostic yield, findings, and interventions) and complications. The indications for enteroscopy included iron deficiency anemia, overt gastrointestinal bleeding, abdominal pain, chronic diarrhea, familial adenomatous polyposis screening, and previous abnormal imaging. Depth of insertion was estimated on withdrawal by counting in 10 cm intervals as the endoscope was slowly withdrawn.
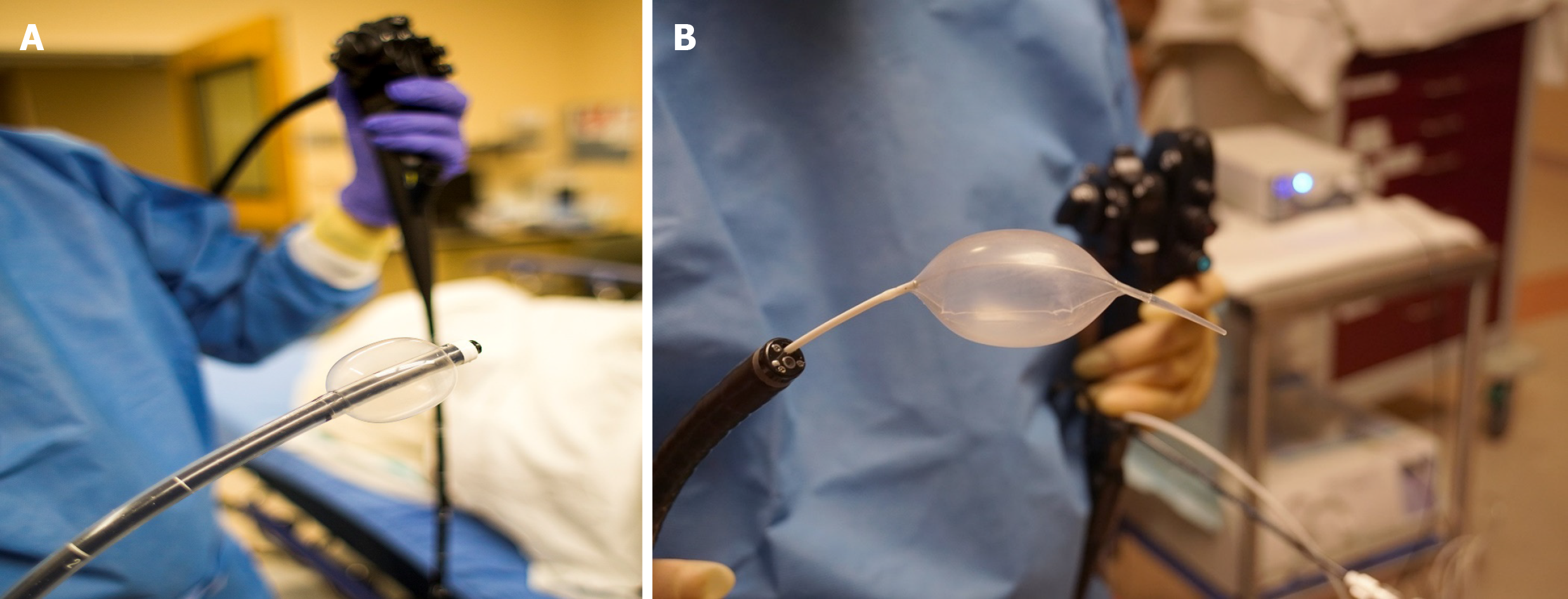
All enteroscopy procedures were performed by an experienced gastroenterologist (Zuckerman MJ). Single balloon enteroscopy was done with the Olympus SIF-Q180 enteroscope (Olympus, Melville, NY, United States) (Figure 1A), the balloon overtube system and the inflation/deflation external device. The through-the-scope (NaviAid) balloon system (SMART Medical Systems Ltd.) consisted of a single-use catheter-based inflatable balloon inserted through the instrument channel of a standard adult colonoscope (Olympus CF-180 or CF-190) (Figure 1B) and the external inflation/ deflation system[10]. Depth of insertion was estimated on withdrawal by counting 10 cm intervals as the endoscope was slowly withdrawn, similar to the technique previously described by Efthymiou et al[17] and utilized by Christian et al[18]. Technical success was defined as insertion of the endoscope greater than 20 cm beyond the ileocecal valve[18]. Procedure time was defined as the time from insertion to the time of complete withdrawal. All patients were monitored for complications. All patients were monitored for complications including uncontrolled bleeding (defined as need for blood transfusion), gastrointestinal perforation, infection, abdominal pain, fever, nausea and vomiting throughout the procedures and for 24 h afterward.
Continuous variables were described using mean and standard deviation while categorical variables were described using frequencies and percentages. Baseline characteristics were compared between groups using either Student’s t-test or Wilcoxon sum rank test, for continuous data and Fisher’s exact test for categorical data. Furthermore, primary and secondary outcomes between groups were also compared using Student’s t-test or Wilcoxon rank sum test or Fisher’s exact test depending on the type and distribution of outcome. One way analysis of variance was used to compare the differences in the durations over the time periods while two way analysis of variance was used to compare the differences in the durations between two groups accounting for time period differences as well. Correlations were assessed using linear regression model.
A total of 81 retrograde enteroscopy procedures were performed in 75 patients during the study period. Overall, 54 retrograde SBE in 49 patients and 27 retrograde TTSE in 26 patients were performed. From 81 procedures, 74 was under general anesthesia, 6 under monitored anesthesia care and one under moderate sedation. There were no statistically significant differences in age, body mass index (BMI), gender, ethnicity, and history of abdominal surgery between the retrograde SBE and retrograde TTSE groups (Table 1). The main indications for both groups were iron deficiency anemia in 41 (50.6%), overt gastrointestinal bleeding in 37 (45.7%), abdominal pain in 17(21.0%), chronic diarrhea in 7 (8.6%), and FAP screening in 2 (2.5%). There were no differences in distribution of indications between two groups (Table 1). Thirty-nine patients and 19 patients underwent VCE before SBE and TTSE, respectively. The positive findings (35/39 and 17/19) were higher on VCE, but lower on both types of enteroscopy (15/54, 6/27) (Table 2). Other patients had abnormal imaging studies (CT abdomen, CT enterography, small bowel series) suggesting a distal small bowel lesion and would have gone straight to retrograde enteroscopy without VCE.
| Enteroscope device | ||||
| Entire cohort | Retrograde SBE1 | Retrograde TTSE2 | ||
| Number of patients | 75 | 49 | 26 | |
| Mean (standard deviation) | Mean (standard deviation) | Mean (standard deviation) | P value | |
| Age (yr)3 | 61.2 (17.6) | 62.6 (16.5) | 58.4 (19.6) | 0.33 |
| Body mass index3 | 29.0 (6.1) | 28.7 (6.3) | 29.6 (5.9) | 0.55 |
| Gender, n (%) | 0.63 | |||
| Female | 43 (57.3) | 27 (55.1) | 16 (61.5) | |
| Male | 32 (42.7) | 22 (44.9) | 10 (38.5) | |
| Ethnicity, n (%) | 0.91 | |||
| Hispanic | 27 (36.0) | 18 (36.7) | 9 (34.6) | |
| Other non-hispanic | 10 (13.3) | 7 (14.3) | 3 (11.5) | |
| White | 38 (50.7) | 24 (49.0) | 14 (53.9) | |
| Indication3 | 0.63 | |||
| Iron deficiency anemia, n (%) | 41 (50.6) | 28 (51.9) | 13 (48.2) | |
| Overt GI bleeding | 37 (45.7) | 23 (42.6) | 14 (51.9) | |
| Abdominal pain | 17 (21.1) | 7 (13.0) | 10 (37.0) | |
| Diarrhea | 7 (8.6) | 4 (7.4) | 3 (11.1) | |
| FAP screening | 2 (2.5) | 2 (3.7) | 0 (0) | |
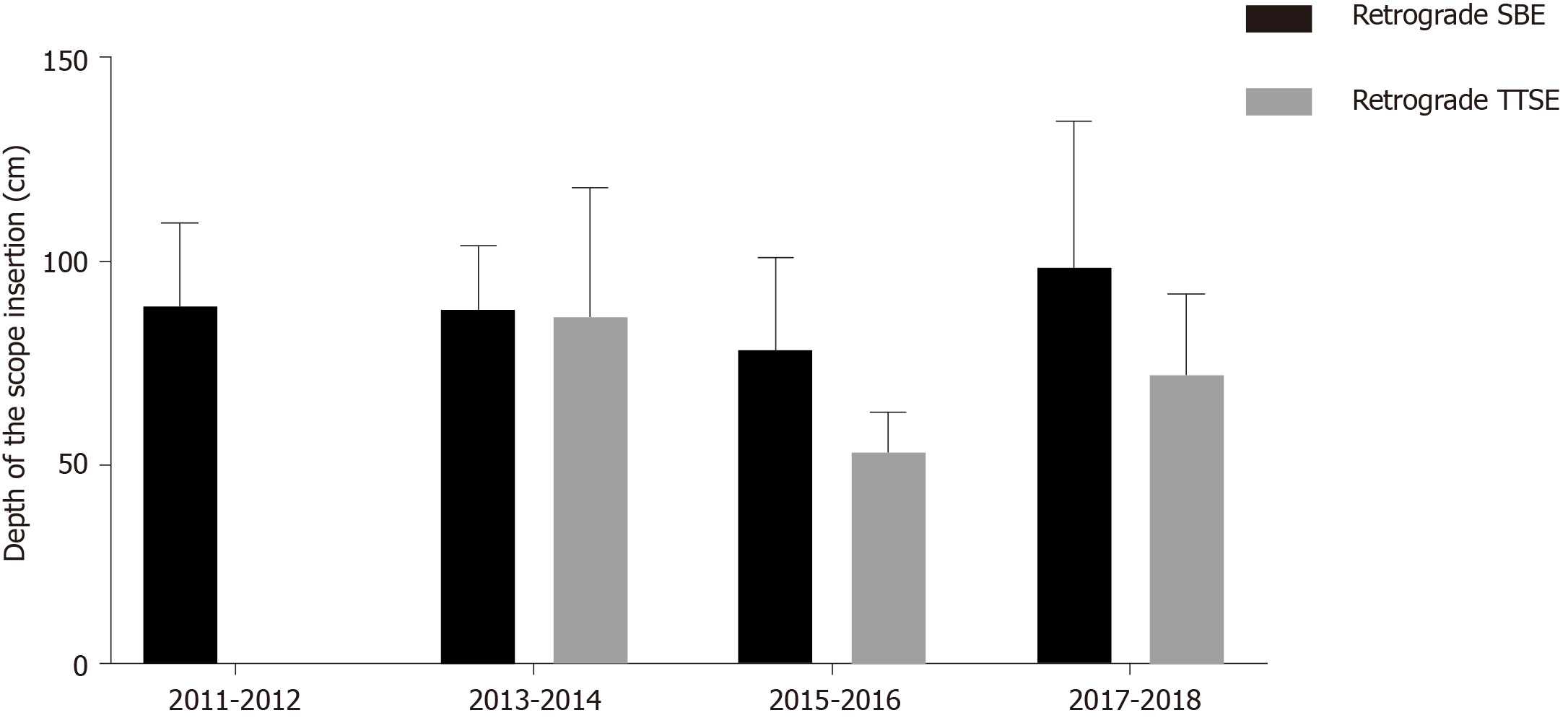
Retrograde enteroscopy was successful (> 20 cm beyond ileocecal valve) in 23/27 (85.2%) with TTS compared with 41/54 (75.9%) retrograde SBEs (P = 0.33). No specific trend was observed for the failure rate by time. Terminal ileal intubation was not achieved in 9/81 procedures [8 (14.8%) retrograde SBE and 1 (3.7%) TTSE]. The mean duration of procedures was longer in retrograde SBE (91.9 ± 34.2 min) compared with retrograde TTSE (70.5 ± 30.7 min) (P = 0.04). The mean depth of insertion beyond the ileocecal valve was not statistically different in retrograde SBE (92.5 ± 70.0 cm) compared with retrograde TTSE (64.6 ± 49.0 cm), but there was a trend for TTSE to have shorter depth of insertion (P = 0.08) (Table 3). There was no correlation between the depth of insertion and the duration of the procedure in retrograde SBE (linear regression R2 = 0.01; P = 0.56) and retrograde TTSE (linear regression R2 = 0.11; P = 0.23) groups. Analyzing the depth of endoscope insertion in successful procedures in consecutive time periods did not indicate any significant change from 2011 to 2018 (Figure 2).
| Enteroscope device | ||||
| Entire cohort | Retrograde SBE1 | Retrograde TTSE2 | ||
| Number of procedures | 81 | 54 | 27 | |
| Mean (SD) | Mean (SD) | Mean (SD) | P value3 | |
| Duration of procedure | 86.2 (34.2) | 91.9 (34.2) | 70.5 (30.7) | 0.04 |
| Depth of the scope insertion | 82.1 (64.1) | 92.5 (70.0) | 64.6 (49.0) | 0.08 |
| Successful procedure with diagnostic yield, n (%) | n = 64 | n = 41 | n = 23 | 0.39 |
| Normal | 43 (67.2) | 26 (63.4) | 17 (73.9) | |
| Positive finding | 21 (32.8) | 15 (36.6) | 6 (26.1) | |
| Intervention performed, n (%) | 0.38 | |||
| No | 65 (80.3) | 45 (83.3) | 20 (74.1) | |
| Yes | 16 (19.8) | 9 (16.7) | 7 (25.9) | |
| Failed (2011-2018), n (%) | 17 (21.0) | 13 (24.1) | 4 (14.8) | 0.33 |
| Terminal ileum not intubated | 9 (11.1) | 8 (14.8) | 1 (3.7) | |
| Insertion < 20 cm | 8 (9.9) | 5 (9.3) | 3 (11.1) | |
| Years | Failed/procedure | Failed/procedure | Failed/procedure | |
| 2011-2012 | 5/14 | 5/14 | - | |
| 2013-2014 | 4/27 | 4/22 | 0/5 | |
| 2015-2016 | 6/26 | 3/11 | 3/15 | |
| 2017-2018 | 2/14 | 1/7 | 1/7 | |
Positive findings were detected in 21 (32.8%) of all retrograde enteroscopies, including angioectasia in 8, erosion or ulcers in 7, foreign body in 3, polyps in 2, strictures in 2, mass/gastrointestinal stromal tumor in 1, congestion/nonspecific inflammation in 1, and blood in the lumen in 1. Intervention was performed in 16/81 (19.8%) procedures or 16/21 (76.2%) of procedures with findings. Some findings did not require intervention. Small intestinal sampling was performed in 4 patients. The hemostasis procedures consisted of argon plasma coagulation (APC) in 7, hemoclip in 1, both APC and hemoclip in 1. There were no complications, such as uncontrolled bleeding, gastrointestinal perforation, infection, abdominal pain, fever, nausea and vomiting, reported and all of the patients tolerated the procedure.
In this study, we evaluated and compared the clinical utility and procedure characteristics of retrograde SBE and retrograde TTSE. We found that both interventions were safe with comparable diagnostic yield. Our study had an overall positive findings of 21/81 procedures (25.9%). The major findings included angioectasia 27 (33.3%) and erosions or ulcers 18 (22.2%). Interventions were performed in 20 (24.7%) procedures with most of them being hemostasis procedures. Previous studies reported similar distributions with vascular lesions as the most common endoscopic findings. Our study had a lower diagnostic yield compared with others reporting 41%-65% and variable intervention rate for SBE ranging from 7%-54%[7,12-15]. The discrepancy between the higher yield on capsule endoscopy than on retrograde enteroscopy could be attributed to two factors. Not all procedures were successful and most importantly, retrograde enteroscopy depth of insertion may not have been sufficient to reach the abnormality seen on capsule endoscopy. Additionally, due to the time elapsed between capsule endoscopy and enteroscopy and the nature of some of the abnormalities seen, they may have no longer been present. Based on a new study, urgent enteroscopy might be associated with higher diagnostic and therapeutic yield with a lower small bowel rebleeding[19].
Small bowel enteroscopy is an effective diagnostic and therapeutic intervention for management of small bowel diseases, especially in patients with overt or occult gastrointestinal bleeding and chronic diarrhea[6,20]. DBE is a well-tolerated and safe procedure with a high diagnostic yield[9], but is somewhat laborious, requires a substantial operator learning curve, and requires relatively long procedure times[21-23]. On the other hand, SBE is a relatively newer procedure than DBE with shorter procedure time and comparable diagnostic yield, but with less probability to achieve total enteroscopy using both antegrade and retrograde routes. Retrograde SBE is technically more difficult compared with antegrade SBE[12,13]. Recently, a novel through–the-scope balloon system (NaviAid) was introduced as an enteroscopy device to allow deep enteroscopy insertion using standard colonoscopes[14,15,20]. Data on retrograde TTSE are very limited. According to a letter published in 2013, Rubin and Goeppinger[24] used the NaviAid balloon device in 6 patients for the diagnosis of ileal Crohn’s disease. In all patients, TTSE permitted retrograde intubation of extra 15 to 60 cm of the ileum, which clarified disease activity in all patients, without any reported adverse events. Subsequently, Kumbhari et al[14] published a letter indicating they had successfully performed retrograde enteroscopy using TTS in 24 patients, 3 for the diagnosis and management of suspected ileal Crohn's disease. Initial concerns about the use of this device included advancing the balloon in a blind fashion through potentially inflamed ileal mucosa; however, complications in this setting have not been reported[14]. In 2015, a multicenter study was published that included reporting retrograde TTSE in 33 cases with an average depth of insertion of 89 cm (range: 20-150 cm) beyond the ileocecal valve and overall diagnostic yield of 44% with no procedure-related adverse events. The average advancement time for the enteroscopy cases was 15.5 min in this study[15]. In this multicenter study[15], there were no adverse events reported, including no mucosal injury or perforation and it has been used in patients with small bowel diverticula. We did not encounter adverse events in our study with either modality, but there is a possibility that since the TTSE balloon is inflated without direct vision, there could be a problem when there is a stricture or diverticulum in the proximal segment, despite the soft flexible nature of the balloon catheter and controlled inflation-deflation system.
In a large retrospective study of 136 retrograde SBE procedures conducted with an overtube endoscope system, Christian found a mean depth of insertion of 68.3 cm and mean time to completion of 41.7 min[18]. In another study of 36 patients who underwent retrograde SBE using a single-balloon technique, median procedure time was 54 min, with a mean insertion depth of 68 cm beyond the ileocecal valve. The technical success rate was 86%. The diagnostic and therapeutic yields were 61% and 25%, respectively[25].
Several factors may affect the success rate of retrograde enteroscopy, procedure time, and depth of insertion, including endoscopist experience, patient anatomy, the severity of symptoms/complaints as well as patient setting (inpatient vs outpatient). Shorter procedure time which we observed in this study would increase technical feasibility and cost-effectiveness of retrograde TTSE. Previous studies report a range of retrograde SBE procedure time of 48-78 min and a range of depth of insertion from 73-199 cm[12,18,26,27]. Our overall failure rate of 21% is similar to the 10%-30% failure rate reported by others[18,26,27].
Depth of insertion in our study tended to be longer with SBE. This was assessed using the visualization estimation method on withdrawal described by Efthymiou et al[17] and utilized in the large study of retrograde SBE by Christian et al[18]. There is no agreed upon accurate method for measurement of insertion depth. Another method proposed is the fold-counting method on withdrawal, which May et al[27] found to correlate in their study with the visual estimate method. The first validated method for measuring insertion depth was the Erlangen method used with double-balloon enteroscopy by estimating the net advancement of the enteroscope at each cycle of overtube advancement, after training with the model. This technique may be more difficult to use in measuring the insertion depth in SBE than in double-balloon enteroscopy. However, depth of insertion always involves an estimate by the endoscopist[27]. Furthermore, we used the same technique developed for SBE to estimate depth of insertion using the TTSE system to provide consistency between results.
Our study had some limitations including nonrandomized design (patients were not randomized to be done with either TTSE or SBE), modest sample size, and lack of a gold standard for measurement of depth of insertion as discussed above. The post-study statistical power was 12% for the success rate and 10% for the diagnostic yield. Although the sample size was relatively modest in our study for success rate and diagnostic yield, the clinical difference in outcomes was within ± 10% indicating a comparable performance of two procedures for the success rate and diagnostic yield outcomes. This reflects that it is unlikely to observe significant differences in these outcomes even after substantially inflating the sample size for this study. The current sample size was sufficient to detect a statistically significant difference for the duration of procedures with 80% power at a 5% level of significance using an unpaired t-test. Other limitations of this study were the procedure which was performed by only one operator and the retrospective design. On the other hand, this is one of the few studies looking at efficacy and safety of retrograde TTSE and has the advantage of looking at this in the context of a center also doing retrograde SBE.
Both retrograde TTSE and SBE are feasible and safe. We demonstrate that the TTSE balloon system has comparable technical success and reduces enteroscopy time compared with SBE, but has a lower capacity of small bowel insertion. Larger prospective randomized studies are needed to further assess the diagnostic and therapeutic potential of the TTSE system and its role relative to other modalities available for evaluation of the small bowel.
A new device has been introduced and designed to allow deep enteroscopy with a through-the-scope balloon which can be used for the more difficult retrograde approach.
To compare safety, feasibility and outcomes of retrograde enteroscopy performed by the novel through- the-scope enteroscopy (TTSE) and traditional single balloon enteroscopy (SBE) techniques.
To describe how retrograde enteroscopy with the novel TTSE differs from the traditional SBE and to provide an in-depth overview of both techniques with detailed description of clinical findings, success rate and outcomes.
We performed a retrospective cohort study comparing clinical data and complications of retrograde TTSE and retrograde SBE in a community hospital. Technical success was considered as insertion of the enteroscope > 20 cm beyond the ileocecal valve.
Retrograde enteroscopy was safe and feasible using both systems. TTSE had comparable technical success, and reduced enteroscopy time compared with SBE, but with a lower capacity of small bowel insertion.
TTSE is a promising method for retrograde examination of the small bowel in adults.
Prospective multicenter studies to understand whether the findings of this study can be observed in other centers with different levels of experience and to compare the learning curve of TTSE vs SBE by different endoscopists.
The preliminary results of this project were partially presented as an abstract at World Congress of Gastroenterology at ACG2017 Meeting, Orlando, FL, United States in 2017.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: American Society for Gastrointestinal Endoscopy; American Gastroenterological Association; American Association for the Study of Liver Diseases; and American College of Gastroenterology.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Liu C, Shi H, Tsou YK S-Editor: Zhang L L-Editor: A P-Editor: Wang LL
| 1. | Jia Y, Majd M, Carrion A, Dodoo C, Dwivedi A, Othman MO, Zuckerman M. Evaluation of the Diagnostic and Therapeutic Utility of Retrograde Single-balloon Enteroscopy and Through-the-Scope Balloon Enteroscopy: A Single Center Experience: 1177. Am J Gastroenterol. 2017;112:S647. [DOI] [Full Text] |
| 2. | Aktas H, Mensink PB. Small bowel diagnostics: current place of small bowel endoscopy. Best Pract Res Clin Gastroenterol. 2012;26:209-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | Schulz HJ, Schmidt H. Intraoperative enteroscopy. Gastrointest Endosc Clin N Am. 2009;19:371-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Ell C, May A. Capsule status 2004: what is the outcome in bleeding? Endoscopy. 2004;36:1107-1108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Delvaux M, Fassler I, Gay G. Clinical usefulness of the endoscopic video capsule as the initial intestinal investigation in patients with obscure digestive bleeding: validation of a diagnostic strategy based on the patient outcome after 12 mo. Endoscopy. 2004;36:1067-1073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 136] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 6. | Gerson LB, Fidler JL, Cave DR, Leighton JA. ACG Clinical Guideline: Diagnosis and Management of Small Bowel Bleeding. Am J Gastroenterol. 2015;110:1265-87; quiz 1288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 368] [Cited by in RCA: 447] [Article Influence: 44.7] [Reference Citation Analysis (1)] |
| 7. | ASGE Standards of Practice Committee, Gurudu SR, Bruining DH, Acosta RD, Eloubeidi MA, Faulx AL, Khashab MA, Kothari S, Lightdale JR, Muthusamy VR, Yang J, DeWitt JM. The role of endoscopy in the management of suspected small-bowel bleeding. Gastrointest Endosc. 2017;85:22-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 110] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 8. | Rondonotti E, Spada C, Adler S, May A, Despott EJ, Koulaouzidis A, Panter S, Domagk D, Fernandez-Urien I, Rahmi G, Riccioni ME, van Hooft JE, Hassan C, Pennazio M. Small-bowel capsule endoscopy and device-assisted enteroscopy for diagnosis and treatment of small-bowel disorders: European Society of Gastrointestinal Endoscopy (ESGE) Technical Review. Endoscopy. 2018;50:423-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 333] [Cited by in RCA: 281] [Article Influence: 40.1] [Reference Citation Analysis (0)] |
| 9. | Heine GD, Hadithi M, Groenen MJ, Kuipers EJ, Jacobs MA, Mulder CJ. Double-balloon enteroscopy: indications, diagnostic yield, and complications in a series of 275 patients with suspected small-bowel disease. Endoscopy. 2006;38:42-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 295] [Cited by in RCA: 284] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 10. | Yamamoto H, Sekine Y, Sato Y, Higashizawa T, Miyata T, Iino S, Ido K, Sugano K. Total enteroscopy with a nonsurgical steerable double-balloon method. Gastrointest Endosc. 2001;53:216-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 896] [Cited by in RCA: 861] [Article Influence: 35.9] [Reference Citation Analysis (0)] |
| 11. | ASGE Technology Committee, Chauhan SS, Manfredi MA, Abu Dayyeh BK, Enestvedt BK, Fujii-Lau LL, Komanduri S, Konda V, Maple JT, Murad FM, Pannala R, Thosani NC, Banerjee S. Enteroscopy. Gastrointest Endosc. 2015;82:975-990. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 64] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 12. | Domagk D, Mensink P, Aktas H, Lenz P, Meister T, Luegering A, Ullerich H, Aabakken L, Heinecke A, Domschke W, Kuipers E, Bretthauer M. Single- vs. double-balloon enteroscopy in small-bowel diagnostics: a randomized multicenter trial. Endoscopy. 2011;43:472-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 130] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 13. | Ramchandani M, Reddy DN, Gupta R, Lakhtakia S, Tandan M, Rao GV, Darisetty S. Diagnostic yield and therapeutic impact of single-balloon enteroscopy: series of 106 cases. J Gastroenterol Hepatol. 2009;24:1631-1638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 92] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 14. | Kumbhari V, Saxena P, Khashab MA. A new through-the-scope balloon-assisted deep enteroscopy platform. Gastrointest Endosc. 2014;79:694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Ali R, Wild D, Shieh F, Diehl DL, Fischer M, Tamura W, Rubin DT, Kumbhari V, Okolo P, Storm A, Halpern Z, Neumann H, Khara HS, Pochapin MB, Gross SA. Deep enteroscopy with a conventional colonoscope: initial multicenter study by using a through-the-scope balloon catheter system. Gastrointest Endosc. 2015;82:855-860. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 16. | ASGE Standards of Practice Committee, Khashab MA, Pasha SF, Muthusamy VR, Acosta RD, Bruining DH, Chandrasekhara V, Chathadi KV, Eloubeidi MA, Fanelli RD, Faulx AL, Fonkalsrud L, Gurudu SR, Kelsey LR, Kothari S, Lightdale JR, Saltzman JR, Shaukat A, Wang A, Yang J, Cash BD, DeWitt JM. The role of deep enteroscopy in the management of small-bowel disorders. Gastrointest Endosc. 2015;82:600-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 47] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 17. | Efthymiou M, Desmond PV, Brown G, La Nauze R, Kaffes A, Chua TJ, Taylor AC. SINGLE-01: a randomized, controlled trial comparing the efficacy and depth of insertion of single- and double-balloon enteroscopy by using a novel method to determine insertion depth. Gastrointest Endosc. 2012;76:972-980. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 61] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 18. | Christian KE, Kapoor K, Goldberg EM. Performance characteristics of retrograde single-balloon endoscopy: A single center experience. World J Gastrointest Endosc. 2016;8:501-507. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 10] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Silva JC, Pinho R, Ponte A, Rodrigues A, Rodrigues J, Gomes AC, Afecto E, Carvalho J. Does urgent balloon-assisted enteroscopy impact rebleeding and short-term mortality in overt obscure gastrointestinal bleeding? Scand J Gastroenterol. 2020;55:1243-1247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 20. | Noujaim MG, Parish A, Raines D, Gross SA, Cave D, Vance I, Beyer D, Liu D, Hoffman B, Lawrence Z, Castillo G, Pavri T, Niedzwiecki D, Wild D. Use, Yield, and Risk of Device-assisted Enteroscopy in the United States: Results From a Large Retrospective Multicenter Cohort. J Clin Gastroenterol. 2020. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 21. | May A, Nachbar L, Pohl J, Ell C. Endoscopic interventions in the small bowel using double balloon enteroscopy: feasibility and limitations. Am J Gastroenterol. 2007;102:527-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 22. | Di Caro S, May A, Heine DG, Fini L, Landi B, Petruzziello L, Cellier C, Mulder CJ, Costamagna G, Ell C, Gasbarrini A; DBE-European Study Group. The European experience with double-balloon enteroscopy: indications, methodology, safety, and clinical impact. Gastrointest Endosc. 2005;62:545-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 153] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 23. | Pennazio M, Spada C, Eliakim R, Keuchel M, May A, Mulder CJ, Rondonotti E, Adler SN, Albert J, Baltes P, Barbaro F, Cellier C, Charton JP, Delvaux M, Despott EJ, Domagk D, Klein A, McAlindon M, Rosa B, Rowse G, Sanders DS, Saurin JC, Sidhu R, Dumonceau JM, Hassan C, Gralnek IM. Small-bowel capsule endoscopy and device-assisted enteroscopy for diagnosis and treatment of small-bowel disorders: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2015;47:352-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 482] [Cited by in RCA: 559] [Article Influence: 55.9] [Reference Citation Analysis (1)] |
| 24. | Rubin DT, Goeppinger SR. Initial experience of a through-the-scope balloon device for ileal intubation in Crohn's disease. Gastrointest Endosc. 2013;78:669-670. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 25. | Dufault DL, Brock AS. Cap-assisted retrograde single-balloon enteroscopy results in high terminal ileal intubation rate. Endosc Int Open. 2016;4:E202-E204. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 26. | Upchurch BR, Sanaka MR, Lopez AR, Vargo JJ. The clinical utility of single-balloon enteroscopy: a single-center experience of 172 procedures. Gastrointest Endosc. 2010;71:1218-1223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 63] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 27. | May A, Färber M, Aschmoneit I, Pohl J, Manner H, Lotterer E, Möschler O, Kunz J, Gossner L, Mönkemüller K, Ell C. Prospective multicenter trial comparing push-and-pull enteroscopy with the single- and double-balloon techniques in patients with small-bowel disorders. Am J Gastroenterol. 2010;105:575-581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 151] [Article Influence: 10.1] [Reference Citation Analysis (0)] |