Published online May 16, 2019. doi: 10.4253/wjge.v11.i5.365
Peer-review started: March 8, 2019
First decision: April 13, 2019
Revised: April 30, 2019
Accepted: May 10, 2019
Article in press: May 11, 2019
Published online: May 16, 2019
Processing time: 72 Days and 21.6 Hours
The migration rate of fully covered self-expandable metal stents (FCSEMSs) has been reported to be between 14% to 37%. Anchoring of FCSEMSs using a double-pigtail plastic stent (DPS) may decrease migration.
To compare stent migration rates between patients who received FCSEMS alone and those who received both an FCSEMS and anchoring DPS.
We conducted a retrospective analysis of endoscopy reporting system and medical records of 1366 patients who underwent endoscopic retrograde cholangiopancreatography (ERCP) with FCSEMS placement at the University of Kentucky health care. Between July 2015 and April 2017, 203 patients with FCSEMS insertion for the treatment of malignant biliary stricture, benign biliary stricture, post-sphincterotomy bleeding, bile leak, and cholangitis drainage were identified. The review and analysis were conducted through our endoscopy reporting system (ProVation® MD) and medical records. Categorical data were analyzed using Chi-Square and Fischer exact test and continuous data using non-parametric tests. A regression analysis was performed to identify factors independently associated with increased risk of stent migration. We determined an FCSEMS migration endoscopically if the stent was no longer visible in the major papilla.
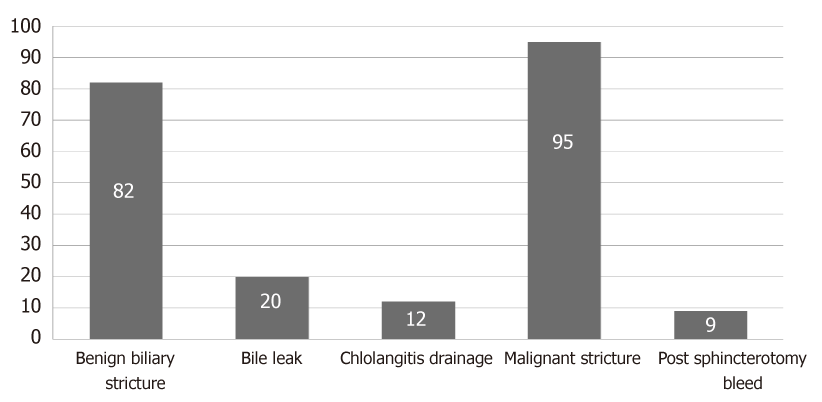
1366 patients had undergone ERCP by three advanced endoscopists over 21-mo period; among these, 203 patients had FCSEMSs placed. 65 patients had FCSEMSs with DPS, and 138 had FCSEMSs alone. 65 patients had FCSEMSs with DPS, and 138 had FCSEMSs alone. 95 patients had a malignant stricture, 82 patients had a benign stricture, 12 patients had bile leak, 12 patients had cholangitis, and nine patients had post-sphincterotomy bleeding. The migration rate in patients with anchored FCSEMSs with DPS was 6%, and those without anchoring DPS was 10% (P = 0.35). Overall, migration was reported in 18 patients with FCSEMSs placement out of 203 patients with an overall migration rate of 9.7%. There was no significant association between anchoring the FCSEMSs with DPS and the risk of stent migration. Only patients with the previous sphincterotomy and begin biliary stricture were found to have a statistically significant difference in the migration rate between patients who had FCSEMS with DPS and FCSEMS alone (P = 0.01).
The risk of migration of biliary FCSEMS was 9.7 %. Anchoring an FCSEMS with DPS does not decrease the risk of stent migration.
Core tip: In this study, we conducted a retrospective analysis to evaluate the efficacy of 7-French (Fr) and 10-Fr double-pigtail plastic stent (DPS) within the fully covered self-expandable metal stent (FCSEMS) as an anti-migration technique. We compared the rate of stent migration between patients who received FCSEMS alone and those who received both an FCSEMS and anchoring DPS in a large patient population with both benign and malignant strictures as well as non-stricture etiologies. Our findings suggest that anchoring of FCSEMS with a 7-Fr or 10-Fr DPS does not decrease the risk of stent migration. Only benign biliary stricture and previous sphincterotomy were to have a significant association with stent migrations (P = 0.01). We did not find evidence to support the routine placement of anchoring DPS.
- Citation: Emhmed Ali S, Frandah WM, Su L, Fielding C, Mardini H. Should a fully covered self-expandable biliary metal stent be anchored with a double-pigtail plastic stent? A retrospective study. World J Gastrointest Endosc 2019; 11(5): 365-372
- URL: https://www.wjgnet.com/1948-5190/full/v11/i5/365.htm
- DOI: https://dx.doi.org/10.4253/wjge.v11.i5.365
Fully covered self-expandable metal stents (FCSEMSs) have been widely used as an effective biliary endoprosthesis in the setting of pancreaticobiliary conditions such as benign and malignant strictures, post-sphincterotomy bleeding, and occasionally bile leaks[1]. The primary advantages of covered stents are a lower rate of tumor ingrowth, longer patency, and their potential removability compared to uncovered stents. However, one concern about FCSEMSs is a higher migration rate than uncovered stents[2]. The migration rate of FCSEMSs in prospective studies for benign biliary strictures is 5%-37%[1]. In this study, we conducted a retrospective analysis to evaluate the efficacy of 7-French (Fr) and 10-Fr double-pigtail plastic stent (DPS) within the FCSEMS as an anti-migration technique. We compared the rate of stent migration between patients who received FCSEMS alone and those who received both an FCSEMS and anchoring DPS in a large patient population with both benign and malignant strictures as well as non-stricture etiologies.
Between July 2015 and April 2017, 1366 patients had undergone endoscopic retrograde cholangiopancreatography (ERCP) at our institution. Among these, 203 patients with FCSEMS placement with or without DPS were identified. The review and analysis were conducted through our endoscopy reporting system (ProVation® MD) and medical records. Patients included in the study had FCSEMS insertion for the treatment of malignant biliary stricture, benign biliary stricture, and non-stricture etiology such as post-sphincterotomy bleeding and bile leak.
After the Institutional Review Board and the Ethics Committee of our hospital approved the study protocol, data was extracted by reviewing patient charts, ERCP reports, and fluoroscopic images. Patients who only had uncovered stents or plastic stents placed were excluded. All endoscopic procedures were performed by three advanced endoscopists. Comprehensive data were collected through Microsoft Excel spreadsheet and included the following: stent type [WallflexTM (Boston Scientific) vs Viabil® (Gore Medical)], the diameter of double-pigtail PS (7-Fr vs 10-Fr), indications for FCSEMS placement including stricture type (malignant vs benign), and non-stricture etiologies such as post-sphincterotomy bleeding and bile leak.
Baseline patient characteristics were identified, such as previous cholecystectomy, biliary sphincterotomy, history of stent migration, choledocholithiasis, and diameter of the common bile duct (CBD). After stent placement and during the follow-up period, patients’ records were reviewed to verify the stent position. We defined FCSEMS migration endoscopically if the stent was no longer visible through the major papilla. It either migrates proximally (into the bile duct) or distally (out of the bile of duct). The anti-migration properties of FCSEMSs include higher radial force, anchoring flap, anchoring fins and flared ends have been designed to prevent the migration. Categorical data were analyzed using the Chi-Square test and Fisher Exact test and continuous data using non-parametric tests. A regression analysis was performed to identify factors independently associated with increased risk of stent migration. All analyses were completed in SAS 9.4 (SAS Institute Inc., Cary, NC, United States).
The primary endpoint of the study was to compare stent migration rates between patients who received FCSEMSs alone and those who received both an FCSEMS with an anchoring DPS. A secondary endpoint was the presence of complications related to stent migration.
1366 patients had undergone ERCP by three advanced endoscopists over 21-mo period; among these, 203 patients had FCSEMS placed with or without DPS (88 females and 115 males). 65 patients had FCSEMSs with DPS, and 138 had FCSEMSs alone (Table 1 and Table 2). 95 patients had a malignant stricture, 82 patients had a benign stricture, 12 patients had bile leak, 12 patients had cholangitis, and nine patients had post-sphincterotomy bleeding (Figure 1). For the patients with stent migration, 12 (66.7%) had a benign biliary stricture, and 6 (33.3%) did not have, while for the patients without stent migration, 70 (37.8%) had a benign biliary stricture and 115 (62.2%) did not have (P = 0.01). Also. For patients with stent migration, 12 (66.7%) had the previous sphincterotomy, and 6 (33.3%) did not have, while for the patients without stent migration, 71 (38.4%) had the previous sphincterotomy and 114 (61.6%) did not have (P = 0.01). The migration rate in patients with benign biliary stricture was 14.6% and for those with non-benign biliary stricture was 5%. Migration rate in patients with the previous sphincterotomy was 14.5%, and those without previous sphincterotomy was 5%. Therefore, the distribution of patients that had a benign biliary stricture and previous sphincterotomy were significantly different between patients with stent migration and patients with no stent migration. There was no significant association between any of the other tested variables including anchoring the FCSEMSs with DPS and the risk of stent migration. The migration rate in patients with anchored FCSEMSs with DPS was 6%, and those without anchoring DPS was 10% (P = 0.35). Overall, migration was reported in 18 patients with FCSEMS placement out of 203 patients with an overall migration rate of 9.7%.
| Characteristic | Determinant | Frequency count | Percent of total frequency |
| Gender | Female | 88 | 43.34 |
| Male | 115 | 56.65 | |
| Race | Black | 9 | 4.43 |
| White | 194 | 95.56 | |
| Age | Mean (62.97); Range (23.00-91.00) | ||
| Brand of FCSEMS | Viabil fully covered | 90 | 44.33 |
| Viabil fully covered with proximal fenestration | 63 | 31.03 | |
| WallFlex | 50 | 24.63 | |
| Cholangitis drainage | No | 191 | 94.08 |
| Yes | 12 | 5.91 | |
| Choledocholithiasis at time of stent placement | No | 188 | 92.61 |
| Yes | 15 | 7.38 | |
| History of cholecystectomy | No | 92 | 45.32 |
| Yes | 111 | 54.67 | |
| History of stent migration | No | 196 | 96.55 |
| Yes | 7 | 3.44 | |
| Length of FCSEMS (cm) | 4 | 30 | 14.77 |
| 6 | 106 | 52.21 | |
| 8 | 47 | 23.15 | |
| 10 | 20 | 9.85 | |
| Length of Stricture (mm) | Mean (19.21); Range (0.00-90.00) | ||
| CBD diameter (mm) | Mean (11.19); Range (3.00-35.00) | ||
| Malignant stricture | No | 108 | 53.20 |
| Yes | 95 | 46.79 | |
| Migration | No | 185 | 91.13 |
| Yes | 18 | 8.86 | |
| Post sphincterotomy bleed | No | 194 | 95.56 |
| Yes | 9 | 4.43 | |
| Previous sphincterotomy | No | 120 | 59.11 |
| Yes | 83 | 40.88 | |
| Sphincterotomy at time of stent deployment | No | 82 | 40.39 |
| Yes | 121 | 59.60 |
| Characteristic | Determinant | Migration (n = 18) | No migration (n = 185) | P-value |
| Gender | Female | 5 (27.8%) | 83 (44.9%) | 0.1626 |
| Male | 13 (72.2%) | 102 (55.1%) | - | |
| Age | mean ± SD (range) | 59.83 (12.38) - (34.00, 91.00) | 63.28 (15.23) - (23.00, 91.00) | 0.3539 |
| Race | Black | 2 (11.1%) | 7 (3.8%) | 0.1494 |
| White | 16 (88.9%) | 178 (96.2%) | - | |
| Post sphincterotomy bleed | No | 17 (94.4%) | 177 (95.7%) | 0.8086 |
| Yes | 1 (5.6%) | 8 (4.3%) | - | |
| Bile leak | No | 18 (100.0%) | 165 (89.2%) | 0.1418 |
| Yes | 0 (0.0%) | 20 (10.8%) | - | |
| Benign biliary stricture | No | 6 (33.3%) | 115 (62.2%) | 0.0173 |
| Yes | 12 (66.7%) | 70 (37.8%) | - | |
| Cholangitis drainage | No | 18 (100.0%) | 173 (93.5%) | 0.2653 |
| Yes | 0 (0.0%) | 12 (6.5%) | - | |
| Malignant stricture | No | 13 (72.2%) | 95 (51.4%) | 0.0902 |
| Yes | 5 (27.8%) | 90 (48.6%) | - | |
| Brand of FCSEMS | Viabil fully covered | 8 (44.4%) | 82 (44.3%) | 0.2294 |
| Viabil fully covered with proximal fenestration | 3 (16.7%) | 60 (32.4%) | - | |
| WallFlex | 7 (38.9%) | 43 (23.2%) | - | |
| Length of FCSEMS (cm) | 4 | 2 (11.1%) | 28 (15.1%) | 0.9376 |
| 6 | 9 (50.0%) | 97 (52.4%) | - | |
| 8 | 5 (27.8%) | 42 (22.7%) | - | |
| 10 | 2 (11.1%) | 18 (9.7%) | - | |
| Anchored FCSEMSs with DPS | No | 14 (77.8%) | 124 (67.0%) | 0.3507 |
| Yes | 4 (22.2%) | 61 (33.0%) | - | |
| Length of stricture (mm) | mean ± SD (range) | 14.67 (10.72) - (0.00, 40.00) | 19.65 (19.32) - (0.00, 90.00) | 0.0958 |
| CBD diameter (mm) | mean ± SD (range) | 11.61 (4.50) - (5.00,22.00) | 11.15 (4.70) - (3.00,35.00) | 0.6878 |
| History of cholecystectomy | No | 5 (27.8%) | 87 (47.0%) | 0.1173 |
| Yes | 13 (72.2%) | 98 (53.0%) | - | |
| Previous sphincterotomy | No | 6 (33.3%) | 114 (61.6%) | 0.0198 |
| Yes | 12 (66.7%) | 71 (38.4%) | - | |
| Sphincterotomy at time of stent deployment | No | 9 (50.0%) | 73 (39.5%) | 0.3843 |
| Yes | 9 (50.0%) | 112 (60.5%) | - | |
| History of stent migration | No | 17 (94.4%) | 179 (96.8%) | 0.6078 |
| Yes | 1 (5.6%) | 6 (3.2%) | - | |
| Choledocholithiasis at time of stent placement | No | 16 (88.9%) | 172 (93.0%) | 0.5272 |
| Yes | 2 (11.1%) | 13 (7.0%) | - |
FCSEMS has been associated with longer patency than uncovered stents in some studies even though they may have higher rates of migration[3-5]. To minimize the risk of migration, FCSEMSs have been designed with anti-migration mechanical properties, such as higher radial force, an anchoring flap, and specific stent flare structures[6-8]. Nevertheless, other modifications such as anchoring fins and flared ends have been designed to prevent the migration of FCSEMSs, even though; there are no randomized studies to evaluate their effectiveness[7,9].
In our study, the risk of migration of biliary FCSEMS seemed to be lower than previous studies at 9.7%. In contrast, migration rates have been reported to be up to 37.5% in the previous study[1]. To our knowledge, there are only two studies that have evaluated the efficacy of anchoring DPS to prevent migration of FCSEMS.
In a randomized controlled study, Park et al[10] described their experience of placing a 5-Fr DPS into FCSEMS in 17 patients out of 33 patients who received FCSEMS for benign biliary strictures. During the follow-up, the migration rate was significantly lower in the anchored group (FCSEMS + anchoring DPS) compared with a non-anchored group (FCSEMS alone): 1/16 (6.3%) vs 7/17 (41.2%) respectively, P = 0.024. However, in the study by Park et al[10], their sample size was underpowered to identify any significant clinical difference between the two groups and the study was terminated before the planned sample size was reached.
Recently, Katsinelos et al[11] investigated the efficacy of using a 10-Fr DPS to prevent migration in 10 patients with malignant biliary strictures and one patient with a suprapapillary benign biliary stenosis. These patients were prospectively enrolled. The median follow-up period was eight months, and no migration of FCSEMS was reported. Even though it was the first study to assess the use of anchoring a 10-Fr DPS inside an FCSEMS as anti-migration technique, it was limited by small sample size and lack of randomization.
Our study contains a much larger sample size than the studies described above. Also, we included patients with a variety of indications for FCSEMS placement, such as benign and malignant biliary stricture, post sphincterotomy bleed, cholangitis drainage, and bile leak. Our study was different from the above studies because 90% of DPS were 7-Fr and 10% were 10-Fr.
The complication rate from stent migration was very low in our study. Five patients developed obstructive jaundice due to stent migration, and only one patient developed stent-induced cholecystitis secondary to the occlusion of the cystic orifice by a proximally migrated stent in a patient with pancreatic cancer. Acute cholecystitis after placement of a biliary metallic stent has been reported in up to 13% and is likely associated with tumor involvement at the orifice of the cystic duct[12-14].
This study was limited by being retrospective and not being randomized. However, this is the first study to investigate the efficacy of a 7-Fr DPS inside an FCSEMS as an anti-migration technique and the first study to assess the migration rate of FCSEMS with or without anchoring DPS among those with non-stricture etiologies such post-sphincterotomy bleeding and bile leak.
In conclusion, our findings suggest that anchoring of FCSEMS with a 7-Fr or 10-Fr DPS does not decrease the risk of stent migration. Only benign biliary stricture and previous Sphincterotomy were to have a significant association with stent migrations (P = 0.01). We did not find evidence to support the routine placement of anchoring DPS. However, prospective randomized controlled studies are needed to evaluate the efficacy of an anchoring DPS within an FCSEMS as an anti-migration technique.
Fully covered self-expandable metal stents (FCSEMSs) have been widely used as an effective biliary endoprosthesis in the setting of pancreaticobiliary conditions such as benign and malignant strictures, post-sphincterotomy bleeding, and occasionally bile leaks. The primary advantages of covered stents are a lower rate of tumor ingrowth, longer patency, and their potential removability compared to uncovered stents. However, one concern about FCSEMSs is a higher migration rate than uncovered stents. In this study, we conducted a retrospective analysis to evaluate the efficacy of 7-French (Fr) and 10-Fr double-pigtail plastic stent (DPS) within the FCSEMS as an anti-migration technique. We compared the rate of stent migration between patients who received FCSEMS alone and those who received both an FCSEMS and anchoring DPS in a large patient population with both benign and malignant strictures as well as non-stricture etiologies. We did not find evidence to support the routine placement of anchoring DPS. We found that anchoring of FCSEMS with a 7-Fr or 10-Fr DPS does not decrease the risk of stent migration.
FCSEMSs have been commonly used as an effective biliary endoprosthesis in the setting of pancreaticobiliary conditions such as benign and malignant strictures. To minimize the risk of migration, FCSEMSs have been designed with different anti-migration mechanical properties. The use of DPS is still unclear as an anti-migration method. Prospective randomized controlled studies are needed to evaluate the efficacy of an anchoring DPS within an FCSEMS as an anti-migration technique.
The main objective of the study was to assess to the rate of stent migration between patients who received FCSEMS alone and those who received both an FCSEMS and anchoring DPS in both benign and malignant strictures as well as non-stricture etiologies. To our knowledge, there are only two small retrospective studies that have evaluated the efficacy of anchoring DPS to prevent migration of FCSEMS. So, more randomized controlled trials with a larger number of patients are needed.
A retrospective analysis of endoscopy reporting system and medical records of patients who underwent ERCP with FCSEMS placement was conducted. The review and analysis were conducted through our endoscopy reporting system (ProVation® MD) and medical records. Patients included in the study had FCSEMS insertion for the treatment of malignant biliary stricture, benign biliary stricture, and non-stricture etiology such as post-sphincterotomy bleeding and bile leak. Data included stent type [WallflexTM (Boston Scientific) vs Viabil® (Gore Medical)], the diameter of double-pigtail PS (7-Fr vs 10-Fr), and indications for FCSEMS placement. We defined FCSEMS migration endoscopically if the stent was no longer visible through the major papilla. It either migrates proximally (into the bile duct) or distally (out of the bile of duct).
There was no significant association between any of the other tested variables including anchoring the FCSEMSs with DPS and the risk of stent migration. The migration rate in patients with anchored FCSEMSs with DPS was 6%, and those without anchoring DPS was 10% (P = 0.35). Overall, migration was reported in 18 patients with FCSEMS placement out of 203 patients with an overall migration rate of 9.7%. The distribution of patients that had a benign biliary stricture and previous sphincterotomy were significantly different between patients with stent migration and patients with no stent migration.
In our study, the risk of migration of biliary FCSEMS was 9.7 %. Anchoring an FCSEMS with a 7-Fr or 10-Fr DPS does not decrease the risk of stent migration. Routine placement of anchoring stents is unnecessary. We believe that further randomized controlled trials with a larger number of patients might be helpful to ascertain if anchoring an FCSEMS with DPS is useful as an anti-migration technique.
Anchoring of FCSEMS with a 7-Fr or 10-Fr DPS does not decrease the risk of stent migration. Only benign biliary stricture and previous Sphincterotomy were to have a significant association with stent migrations. Needs more prospective large studies. More randomized controlled trials with a larger number of patients are needed.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Gurkan A, Fiori E, Goral V, Osawa S, Fogli L S-Editor: Dou Y L-Editor: A E-Editor: Xing YX
| 1. | Dumonceau JM, Tringali A, Blero D, Devière J, Laugiers R, Heresbach D, Costamagna G; European Society of Gastrointestinal Endoscopy. Biliary stenting: indications, choice of stents and results: European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline. Endoscopy. 2012;44:277-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 278] [Cited by in RCA: 290] [Article Influence: 22.3] [Reference Citation Analysis (0)] |
| 2. | Isayama H, Komatsu Y, Tsujino T, Sasahira N, Hirano K, Toda N, Nakai Y, Yamamoto N, Tada M, Yoshida H, Shiratori Y, Kawabe T, Omata M. A prospective randomised study of "covered" versus "uncovered" diamond stents for the management of distal malignant biliary obstruction. Gut. 2004;53:729-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 460] [Cited by in RCA: 459] [Article Influence: 21.9] [Reference Citation Analysis (0)] |
| 3. | Lee JH, Krishna SG, Singh A, Ladha HS, Slack RS, Ramireddy S, Raju GS, Davila M, Ross WA. Comparison of the utility of covered metal stents versus uncovered metal stents in the management of malignant biliary strictures in 749 patients. Gastrointest Endosc. 2013;78:312-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 86] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 4. | Kitano M, Yamashita Y, Tanaka K, Konishi H, Yazumi S, Nakai Y, Nishiyama O, Uehara H, Mitoro A, Sanuki T, Takaoka M, Koshitani T, Arisaka Y, Shiba M, Hoki N, Sato H, Sasaki Y, Sato M, Hasegawa K, Kawabata H, Okabe Y, Mukai H. Covered self-expandable metal stents with an anti-migration system improve patency duration without increased complications compared with uncovered stents for distal biliary obstruction caused by pancreatic carcinoma: a randomized multicenter trial. Am J Gastroenterol. 2013;108:1713-1722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 171] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 5. | Saleem A, Leggett CL, Murad MH, Baron TH. Meta-analysis of randomized trials comparing the patency of covered and uncovered self-expandable metal stents for palliation of distal malignant bile duct obstruction. Gastrointest Endosc. 2011;74:321-327.e1-3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 190] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 6. | Isayama H, Nakai Y, Toyokawa Y, Togawa O, Gon C, Ito Y, Yashima Y, Yagioka H, Kogure H, Sasaki T, Arizumi T, Matsubara S, Yamamoto N, Sasahira N, Hirano K, Tsujino T, Toda N, Tada M, Kawabe T, Omata M. Measurement of radial and axial forces of biliary self-expandable metallic stents. Gastrointest Endosc. 2009;70:37-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 172] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 7. | Park DH, Lee SS, Lee TH, Ryu CH, Kim HJ, Seo DW, Park SH, Lee SK, Kim MH, Kim SJ. Anchoring flap versus flared end, fully covered self-expandable metal stents to prevent migration in patients with benign biliary strictures: a multicenter, prospective, comparative pilot study (with videos). Gastrointest Endosc. 2011;73:64-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 120] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 8. | Isayama H, Kawakubo K, Nakai Y, Inoue K, Gon C, Matsubara S, Kogure H, Ito Y, Tsujino T, Mizuno S, Hamada T, Uchino R, Miyabayashi K, Yamamoto K, Sasaki T, Yamamoto N, Hirano K, Sasahira N, Tada M, Koike K. A novel, fully covered laser-cut nitinol stent with antimigration properties for nonresectable distal malignant biliary obstruction: a multicenter feasibility study. Gut Liver. 2013;7:725-730. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 9. | Moon SH, Kim MH, Park DH, Song TJ, Eum J, Lee SS, Seo DW, Lee SK. Modified fully covered self-expandable metal stents with antimigration features for benign pancreatic-duct strictures in advanced chronic pancreatitis, with a focus on the safety profile and reducing migration. Gastrointest Endosc. 2010;72:86-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 103] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 10. | Park JK, Moon JH, Choi HJ, Min SK, Lee TH, Cheon GJ, Cheon YK, Cho YD, Park SH, Kim SJ. Anchoring of a fully covered self-expandable metal stent with a 5F double-pigtail plastic stent to prevent migration in the management of benign biliary strictures. Am J Gastroenterol. 2011;106:1761-1765. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 11. | Katsinelos P, Lazaraki G, Gkagkalis S, Chatzimavroudis G, Anastasiadou K, Georgakis N, Giouleme O, Zavos C, Kountouras J. A fully covered self-expandable metal stent anchored by a 10-Fr double pigtail plastic stent: an effective anti-migration technique. Ann Gastroenterol. 2017;30:114-117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Kahaleh M, Tokar J, Conaway MR, Brock A, Le T, Adams RB, Yeaton P. Efficacy and complications of covered Wallstents in malignant distal biliary obstruction. Gastrointest Endosc. 2005;61:528-533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 51] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 13. | Isayama H, Kawabe T, Nakai Y, Tsujino T, Sasahira N, Yamamoto N, Arizumi T, Togawa O, Matsubara S, Ito Y, Sasaki T, Hirano K, Toda N, Komatsu Y, Tada M, Yoshida H, Omata M. Cholecystitis after metallic stent placement in patients with malignant distal biliary obstruction. Clin Gastroenterol Hepatol. 2006;4:1148-1153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 124] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 14. | Suk KT, Kim HS, Kim JW, Baik SK, Kwon SO, Kim HG, Lee DH, Yoo BM, Kim JH, Moon YS, Lee DK. Risk factors for cholecystitis after metal stent placement in malignant biliary obstruction. Gastrointest Endosc. 2006;64:522-529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 127] [Article Influence: 6.7] [Reference Citation Analysis (0)] |