Published online Apr 16, 2019. doi: 10.4253/wjge.v11.i4.292
Peer-review started: January 31, 2019
First decision: March 11, 2019
Revised: March 14, 2019
Accepted: March 26, 2019
Article in press: March 26, 2019
Published online: April 16, 2019
Processing time: 78 Days and 11.1 Hours
Esophageal varices are a result of progressive liver disease and portal hypertension. Treatment can be performed with band ligation versus non-selective beta blockers depending on the size of varices, ability to tolerate medications and history of variceal bleeding. Band ligation is an effective intervention with rare but serious complications including bleeding, ulcers and rarely obstruction. Few cases of esophageal obstruction and necrosis caused by banding have been reported, each with varied management from conservative treatment to band removal.
An 89 years old woman with a past medical history of nonalcoholic steatohepatitis cirrhosis presented to the hospital with an inability to swallow one day after screening esophagogastroduodenoscopy where band ligation of esophageal varices was performed for primary prophylaxis. The patient was not able to tolerate her oral secretions. Initial blood work revealed a Model of End Organ Liver Disease score of 7. She was treated with sublingual nitroglycerin for esophageal spasm, a known complication after esophageal banding. When she failed to improve, esophagogastroduodenoscopy was performed and revealed the mucosa surrounding the banded varix was necrosed and blocking the lumen of the esophagus. The band was purposefully dislodged, revealing distal ulceration and stricturing. Within 72 h after band removal, she was tolerating an oral diet. Endoscopy performed 2 wk later revealed an intrinsic stenosis, measuring 8 mm in diameter by 1 cm in length, which was dilated.
Esophageal obstruction is a complication of variceal banding that should be considered in patients with inability to tolerate oral diet after banding.
Core tip: Complete esophageal obstruction and necrosis is a rare complication of esophageal variceal banding. Patients typically present with dysphagia and inability to tolerate secretions shortly after banding. Diagnosis is made with a barium esophagram or upper endoscopy. Treatment consists of supportive care and total parental nutrition until recovery or removing the band endoscopically. Most patients recover but may require esophageal dilation afterwards.
- Citation: Sobotka LA, Ramsey ML, Wellner M, Kelly SG. Rare cause of dysphagia after esophageal variceal banding: A case report. World J Gastrointest Endosc 2019; 11(4): 292-297
- URL: https://www.wjgnet.com/1948-5190/full/v11/i4/292.htm
- DOI: https://dx.doi.org/10.4253/wjge.v11.i4.292
Esophageal and gastric varices are a result of progressive liver disease and portal hypertension. Screening and management of varices is a crucial part of the management in patient with end stage liver disease. Treatment can be performed with band ligation versus non-selective beta blockers depending on the size of varices, ability to tolerate medications and history of esophageal variceal bleeding. Variceal band ligation is a safe and effective intervention for varices with rare but serious complications including bleeding, ulcers and rarely obstruction[1-4].
We present a case of complete esophageal obstruction and necrosis as a result of esophageal variceal banding. The case report explores the differential diagnosis of dysphagia after band ligation, diagnosis of obstruction and reviews potential treatment options.
An 89 years old woman presented with an inability to swallow one day after band ligation of esophageal varices.
The patient experienced almost immediate regurgitation after any oral intake on the way home from endoscopy. Her initial esophagogastroduodenoscopy (EGD) was performed for surveillance of varices. She was found to have large, non-bleeding esophageal varices and type 1 gastroesophageal varices. Two bands were placed on the esophageal varices in the lower esophagus in an upward spiral motion for primary prophylaxis and varices were completely eradicated. She reported feeling well in recovery after the procedure and was discharged.
She has a past medical history of nonalcoholic steatohepatitis cirrhosis.
Upon arrival to the hospital the day after endoscopy, her vital signs were stable. The patient appeared uncomfortable and was not able to tolerate her oral secretions. Her physical exam was otherwise unremarkable with pertinent negatives including ascites, hepatic encephalopathy, hepatosplenomegaly, lower extremity edema or crepitus.
Initial blood work revealed a Model of End Organ Liver Disease score of 7. The rest of her blood work was unremarkable including a complete blood count, chemistry and liver function tests. She underwent a chest X-ray, which did not reveal any acute abnormalities.
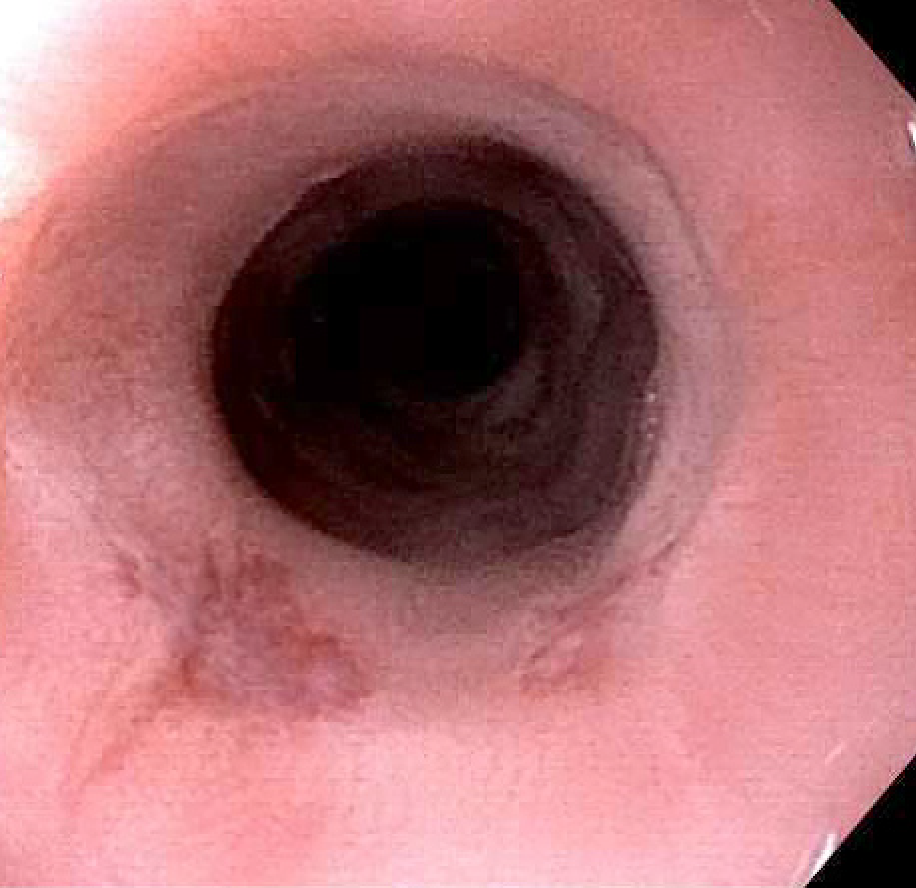
She was treated symptomatically with sublingual nitroglycerin for esophageal spasm, which is a known complication after esophageal banding and was the presumed issue here. She failed to improve with intravenous fluids and conservative management for several days and, therefore, underwent an EGD for further evaluation. Images from endoscopy five days after initial band placement are shown in Figure 1. Endoscopy revealed the mucosa surrounding the banded varix was now necrosed and blocking the lumen of the esophagus.
Complete esophageal obstruction and necrosis due to esophageal variceal band ligation.
The band was purposefully dislodged, revealing distal ulceration and stricturing which could not be transversed with an endoscope. She underwent a computed topography of the chest which did not reveal perforation. Surgery evaluated the patient and did not feel that an operation was warranted. Subsequent gastrograffin swallow study revealed passage of contrast into the stomach without extravasation (Figure 2). Within 72 h after the procedure, she was tolerating an oral diet and was discharged home.
She returned as an outpatient for an EGD two weeks after discharge. Endoscopy revealed intrinsic moderate stenosis 34 cm from the incisors. The stenosis was 8 mm in diameter by 1 cm in length and dilated with a through-the-scope balloon (Figures 3 and 4).
Band ligation is one of the most effective interventions for the prevention and treatment of esophageal variceal hemorrhage. When esophageal varices are banded, local venous occlusion and thrombosis leads to tissue necrosis at the site of the band. The band subsequently sloughs off within about 72 h of placement and a small ulceration is left at the place of the band[2]. Varices subsequently become smaller in diameter, reducing risk of life-threatening bleeding. Patient typically require multiple treatments in order to completely eradicate varices[5].
Variceal banding is an effective and well tolerated procedure; however, side effects including dysphagia, ulcer bleeding, pneumonia, and strictures have been reported[6,7]. The prevalence of these side effects, including dysphagia, have been reported in the literature; however rates have varied significantly from 0 to 75% of affected patients[8]. Dysphagia after variceal banding is more commonly due to dysmotility and esophageal spasms after banding. These symptoms tend to be transient and typically last about 24 to 48 h and most patients can successfully advance their diet[9]. Rarely dysphagia is a result of complete esophageal obstruction and necrosis. To our knowledge, there has only been 8 cases reports in the literature highlighting the diagnosis and management of this complication[10-18]. While the exact cause of obstruction and factors that predispose patients to developing this are unknown, some authors postulate that obstruction after banding may occur if a band is placed too close to mucosa that is already edematous or necrotic, which can be seen after previous banding[3].
Given the rarity of this complication, management has been based upon previous case reports in the literature and therefore has varied. Many patients were treated conservatively with no oral intake and received total parental nutrition until symptoms resolved. According to previous case reports, this has been a successful intervention and most patients began to show signs of improvement within a week[2,10-12]. Other case reports have highlighted removing the band endoscopically with mixed outcomes. Endoscopists have attempted band removal with biopsy forceps and rat tooth forceps. While many patients tolerated removal, were able to advance their diet and be discharged from the hospital faster, one patient suffered an intramural esophageal dissection and bleeding[16]. We opted to remove the band with biopsy forceps and this intervention was successful with no complications. Patient was able to safely advance her diet within 24 h. Our patient improved quickly once the band was removed from the obstructing varix, suggesting this could be an ideal intervention if the endoscopist is able to safely perform this maneuver.
In conclusion, complete esophageal obstruction and localized necrosis is an extremely rare complication of variceal banding. This should be considered in any patient that presents with an inability to tolerate an oral diet after band ligation of esophageal varices. Diagnosis of this complication is typically with a barium esophagram or repeat upper endoscopy. Treatment may consist of supportive care and nothing by mouth until symptoms resolve or with removing the band endoscopically.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lan C, Yuan JY S-Editor: Ji FF L-Editor: A E-Editor: Wu YXJ
| 1. | Garcia-Tsao G, Sanyal A, Grace ND, Care Y; Practice Guidelines Committee of the American Association for the Study of Liver Disease; Practice Parameters Committee of the American College of Gastroenterology. Prevention and Management of Gastroesophageal Varices and Variceal Hemorrhage in Cirrhosis. Hepatology. 2007;. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1229] [Cited by in RCA: 1209] [Article Influence: 67.2] [Reference Citation Analysis (0)] |
| 2. | Poza Cordon J, Froilan Torres C, Burgos García A, Gea Rodriguez F, Suárez de Parga JM. Endoscopic management of esophageal varices. World J Gastrointest Endosc. 2012;4:312-322. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 48] [Cited by in RCA: 53] [Article Influence: 4.1] [Reference Citation Analysis (2)] |
| 3. | Mansour M, Abdel-Aziz Y, Awadh H, Shah N, Ajmera A. Complete Esophageal Obstruction after Endoscopic Variceal Band Ligation in a Patient with a Sliding Hiatal Hernia. ACG Case Rep J. 2017;4:e8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Verma D, Pham C, Madan A. Complete esophageal obstruction: an ususual complication of esophageal variceal ligation. Endoscopy. 2009;41 Suppl 2:E200-E201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Villanueva C, Colomo A, Aracil C, Guarner C. Current endoscopic therapy of variceal bleeding. Best Pract Res Clin Gastroenterol. 2008;22:261-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 33] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 6. | Schmitz RJ, Sharma P, Badr AS, Qamar MT, Weston AP. Incidence and management of esophageal stricture formation, ulcer bleeding, perforation, and massive hematoma formation from sclerotherapy versus band ligation. Am J Gastroenterol. 2001;96:437-441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 54] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Al Traif I, Fachartz FS, Al Jumah A, Al Johani M, al-Omair A, al-Bakr F, al-Knawy B, el-Hafi A, Khan MH. Randomized trial of ligation versus combined ligation and sclerotherapy for bleeding esophageal varices. Gastrointest Endosc. 1999;50:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 49] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Goff JS, Reveille RM, Van Stiegmann G. Endoscopic sclerotherapy versus endoscopic variceal ligation: esophageal symptoms, complications, and motility. Am J Gastroenterol. 1988;83:1240-1244. [PubMed] |
| 9. | Kim HC, Song JH, Kim HE, Choi SC, Lyou JH, Kim TH, Shin BJ. Effects of endoscopic variceal ligation in lower esophageal motor function: a prospective study. Korean J Intern Med. 1995;10:120-124. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Nikoloff MA, Riley TR, Schreibman IR. Complete esophageal obstruction following endoscopic variceal ligation. Gastroenterol Hepatol (NY). 2011;7:557-559. [PubMed] |
| 11. | Elizondo-Rivera RL, González-González JA, Garcia-Compean D, Maldonado-Garza HJ. Complete esophageal obstruction after endoscopic variceal band ligation. Endoscopy. 2014;46 Suppl 1 UCTN:E457-E458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Dilshad A, Ahmad I, Niazi AK, Zubair M, Khalid U. Severe dysphagia after endoscopic variceal band ligation: a case report. Proceeding SZPGML. 2003;17:91-92. |
| 13. | Saltzman JR, Arora S. Complications of esophageal variceal band ligation. Gastrointest Endosc. 1993;39:185-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 32] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | de Melo SW. Complete esophageal occlusion after band ligation. Endoscopy. 2011;43 Suppl 2 UCTN:E259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Sarwar FC, Batul MB. Complete esophageal occlusion following esophageal variceal band ligation: an unusual complication; a case report. Visible Hum J Endosc. 2010;9 (1). |
| 16. | Chahal H, Ahmed A, Sexton C, Bhatia A. Complete esophageal obstruction following endoscopic variceal band ligation. J Community Hosp Intern Med Perspect. 2013;3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Kwiatt JT, Merchant P. Successful removal of an esophageal band causing complete esophageal obstruction after variceal ligation. Gastrointest Endosc. 2016;83:1030-1031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Kubovy J, Boswell TD, Vautier G, Arnold MM. Complete esophageal obstruction following endoscopic variceal ligation: a case report and literature review. Clin Exp Gastroenterol. 2018;11:165-168. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |