Published online Mar 16, 2018. doi: 10.4253/wjge.v10.i3.69
Peer-review started: July 16, 2017
First decision: January 15, 2018
Revised: January 20, 2018
Accepted: March 1, 2018
Article in press: March 1, 2018
Published online: March 16, 2018
Processing time: 63 Days and 22.8 Hours
We report a case of a 59-year-old woman who was diagnosed with gastric and small intestinal anisakiasis, which was successfully treated with endoscopic extraction and Gastrografin therapy. She was admitted to our hospital with epigastric pain and vomiting one day after eating raw fish. She exhibited tenderness in the epigastrium without obvious rebound tenderness or guarding. Computed tomography (CT) demonstrated segmental edema of the intestinal wall with proximal dilatation and a small number of ascites. Because enteric anisakiasis was suspected based on the patient’s history of recent raw fish consumption and abdominal CT, we performed gastroscopy and confirmed that nine Anisakis larvae were attached to the gastric mucosa. All of the Anisakis larvae were extracted via endoscopy, and the patient was diagnosed with gastric and enteric anisakiasis. Additionally, in the hospital, we performed ileography twice using Gastrografin, which led to shortened hospital stay. Based on the clinical results of this case, we suggest that Gastrografin therapy is a safe, convenient, and useful method to extract enteric Anisakis larvae.
Core tip: Enteric anisakiasis is difficult to diagnose due to a lack of definitive criteria, and there is currently no curative treatment. This case report describes two important clinical suggestions: (1) Abdominal computed tomography (CT) is useful for the diagnosis of enteric anisakiasis; and (2) Gastrografin administration is a safe, convenient, and useful therapy. In the case of intestinal anisakiasis, CT scan showed submucosal edema of the intestine with proximal dilatation and ascites. We performed ileography using Gastrografin to extract enteric Anisakis larvae after placing an ileus tube, which led to shortened hospital stay.
- Citation: Fujikawa H, Kuwai T, Yamaguchi T, Miura R, Sumida Y, Takasago T, Miyasako Y, Nishimura T, Iio S, Imagawa H, Yamaguchi A, Kouno H, Kohno H. Gastric and enteric anisakiasis successfully treated with Gastrografin therapy: A case report. World J Gastrointest Endosc 2018; 10(3): 69-73
- URL: https://www.wjgnet.com/1948-5190/full/v10/i3/69.htm
- DOI: https://dx.doi.org/10.4253/wjge.v10.i3.69
Anisakiasis is a human disease caused by the accidental ingestion of larval nematodes belonging to the Anisakidae family[1]. Anisakiasis usually occurs in the stomach, and can easily be diagnosed via gastroscopy and treated with endoscopic extraction. On the other hand, enteric anisakiasis is relatively rare. The clinical characteristics of enteric anisakiasis mainly consist of colicky or diffuse abdominal pain, nausea, vomiting, ascites, and peritonitis. In addition, because intestinal obstruction and ileus have been observed[2], patients are often misdiagnosed as having acute appendicitis or terminal ileitis[1]. However, enteric anisakiasis can generally be treated with conservative therapy such as analgesic drugs, because the larvae die within approximately one week in the human body. Thus, there is currently no curative treatment for enteric anisakiasis. This case report describes a patient with gastric and enteric anisakiasis who was successfully treated with endoscopic extraction and Gastrografin therapy.
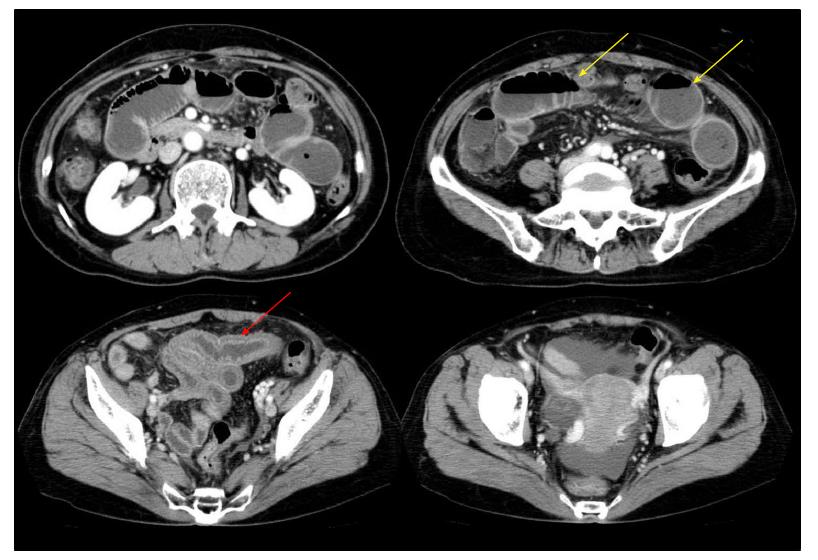
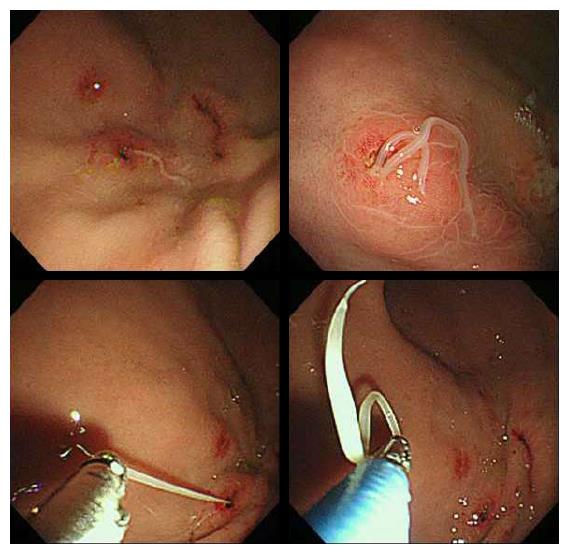
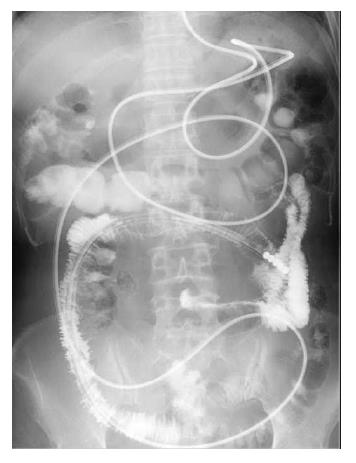
A 59-year-old Japanese woman was suffering from epigastric pain and vomiting since the evening and was brought to our hospital. She had eaten sliced raw horse mackerel and salmon at lunch. She was conscious, her blood pressure was 120/70 mmHg, her pulse was 75 beats/min, and her body temperature was 37.3 °C. Her medical history was significant for appendectomy. On physical examination, she exhibited tenderness in the epigastrium without obvious rebound tenderness or guarding. Her bowel sounds were slightly decreased. Laboratory examinations showed only increased C-reactive protein (19.7 mg/dL) and were otherwise unremarkable. Abdominal x-ray revealed a nonspecific gas pattern. Abdominal computed tomography (CT) demonstrated segmental edema of the intestinal wall with dilated bowel and a small number of ascites (Figure 1). Small intestinal anisakiasis was suspected based on the patient’s recent raw fish consumption and abdominal CT images; therefore, we performed gastroscopy to place an ileus tube. We confirmed that nine Anisakis larvae were attached to the gastric mucosa and performed direct endoscopic removal of all of the Anisakis larvae with a biopsy forceps (Figure 2). Therefore, she was diagnosed with gastric and enteric anisakiasis and we administered Gastrografin after placing an ileus tube. Ileography, using Gastrografin, on postoperative day 4 revealed that there was no small intestinal obstruction (Figure 3), and this was followed by clinical improvement. The patient was discharged 11 d after the procedure.
The course of this patient provides two important clinical suggestions: (1) Abdominal CT is useful for the diagnosis of enteric anisakiasis; and (2) Gastrografin administration therapy is a safe, convenient, and useful method to extract enteric Anisakis larvae.
First, abdominal CT is useful for the diagnosis of enteric anisakiasis. Anisakiasis commonly involves the stomach and rarely involves the intestine. According to Ishikura et al[3], gastric anisakiasis accounted for 95.6% of cases, enteric anisakiasis for 4.1% of cases, and other sites for 0.3% of cases However, as diagnosis via gastroscopy is relatively easy, the incidence of enteric anisakiasis is much lower due to a lack of definitive diagnosis criteria[4]. Consequently, it is considered that the true number of enteric anisakiasis cases is probably greater than has been reported[5]. For this type of infection, ultrasonography[5,6] and CT[7] have been useful for establishing a diagnosis. Intestinal anisakiasis shows marked submucosal edema of the intestine without showing complete intraluminal occlusion, ascites, or fluid collection in the distal segment of the constricted small intestine on CT[7]; these points were confirmed for this case.
Second, Gastrografin administration therapy is a safe, convenient, and useful method to extract enteric Anisakis larvae. In several reported cases, scattering Gastrografin over the lesion was useful for patients with gastric anisakiasis[8]; however, the effect on enteric anisakiasis is unclear. Regardless, it is known that Gastrografin therapy is effective for tapeworm infections such as Taenia saginata in the intestinal tract[9]. Gastrografin is a 76% solution of diatrizoate, a water-soluble contrast medium, and a three-iodine compound. It contains 66% meglumine salt solution and 10% sodium salt solution. It is a hypertonic solution with a specific gravity of 1.416-1.420, pH 6.0-7.7, iodine content of 370 mg/mL, and osmotic pressure of 1900 mOsmol/L[10]. Because of its high osmotic pressure, when Gastrografin is used for patients with upper gastrointestinal symptoms, diarrhea is often a result, and it seems that extraction of Anisakis larvae is the result of this purgative effect.
Since Anisakis larvae die over time, enteric anisakiasis is generally alleviated through conservative therapy. For example, Amano et al[11] suggested that retrieving Anisakis larvae through endoscopic extraction using double-balloon enteroscopy via the anal approach is useful for treating enteric anisakiasis. However, double-balloon enteroscopy still requires a high-level of expertise and is not routinely performed. Using an antiallergic drug such as Stronger Neo-Minophagen C and steroids is useful; however, it is just one of many conservative therapies and is not a radical treatment[12,13]. Kasuya et al[14] examined the killing effect of foods such as Perilla frutescens viridis Makino, Zingiber officinale, Wasabia japonica, Allium sativum, and ethanol to find the most effective form of prophylaxis, and confirmed that these foods were effective in stopping the motion of worms in vitro. However, these foods would need to be consumed in too high of a volume to be practical as an effective prophylaxis. Thus, of the available known treatment options, Gastrografin administration is the most convenient and useful therapy.
In conclusion, based on this case, abdominal CT is useful for the diagnosis of enteric anisakiasis, and Gastrografin administration therapy is useful for the extraction of enteric Anisakis larvae. Because most patients with intestinal anisakiasis cause intestinal obstruction and ileus, an ileus tube is indwelled. Our Gastrografin administration therapy is only two times of ileography using Gastrografin after placing an ileus tube, which is less in burdens on a patient. However more studies are necessary to confirm our results.
A 59-year-old Japanese woman who had eaten sliced raw horse mackerel and salmon at lunch presented with epigastric pain and vomiting since the evening.
Tenderness in the epigastrium without obvious rebound tenderness or guarding.
Acute abdomen including digestive disorders and gynecological disorders, acute coronary syndromes, urinary system diseases.
All labs were within normal limits, except for increased C-reactive protein (19.7 mg/dL).
Computed tomography (CT) scan demonstrated segmental edema of the intestinal wall with dilated bowel and a small number of ascites, and endoscopy revealed that nine Anisakis larvae were attached to the gastric mucosa.
Direct endoscopic removal of all of the Anisakis larvae in the stomach with a biopsy forceps and Gastrografin administration for enteric anisakiasis.
Abdominal CT is useful for the diagnosis of enteric anisakiasis and Gastrografin administration therapy is useful for the extraction of enteric Anisakis larvae.
The authors thank Naoko Matsumoto for assistance in collecting data and for office procedures.
CARE Checklist (2013) statement: The authors have read the CARE Checklist (2013), and the manuscript was prepared and revised according to the CARE Checklist (2013).
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Bueno-Lledo J, Song HJ S- Editor: Cui LJ L- Editor: A E- Editor: Li RF
| 1. | Sakanari JA, McKerrow JH. Anisakiasis. Clin Microbiol Rev. 1989;2:278-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 184] [Article Influence: 5.1] [Reference Citation Analysis (1)] |
| 2. | Yasunaga H, Horiguchi H, Kuwabara K, Hashimoto H, Matsuda S. Clinical features of bowel anisakiasis in Japan. Am J Trop Med Hyg. 2010;83:104-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 43] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 3. | Ishikura H, Kikuchi K, Nagasawa K, Ooiwa T, Takamiya H, Sato N, Sugane K. Anisakidae and anisakidosis. Prog Clin Parasitol. 1993;3:43-102. [PubMed] |
| 4. | Sasaki T, Fukumori D, Matsumoto H, Ohmori H, Yamamoto F. Small bowel obstruction caused by anisakiasis of the small intestine: report of a case. Surg Today. 2003;33:123-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Ido K, Yuasa H, Ide M, Kimura K, Toshimitsu K, Suzuki T. Sonographic diagnosis of small intestinal anisakiasis. J Clin Ultrasound. 1998;26:125-130. [PubMed] |
| 6. | Shirahama M, Koga T, Ishibashi H, Uchida S, Ohta Y, Shimoda Y. Intestinal anisakiasis: US in diagnosis. Radiology. 1992;185:789-793. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 46] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Shibata E, Ueda T, Akaike G, Saida Y. CT findings of gastric and intestinal anisakiasis. Abdom Imaging. 2014;39:257-261. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 8. | Kushigami M, Higashi F, Sumitani M, Kunishou N, Tamaki Y, Tamaki H, Tamaki M, Tamaki H, Kawai J, Itoh H. Usefulness of Gastrografin spray for endoscopic treatment of gastric anisakiasis. Gastroenterol Endosc. 1994;36:144-149. [DOI] [Full Text] |
| 9. | Waki K, Oi H, Takahashi S, Nakabayashi T, Kitani T. Successful treatment of Diphyllobothrium latum and Taenia saginata infection by intraduodenal ‘Gastrografin’ injection. Lancet. 1986;2:1124-1126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Oi H, Nakamura H, Nakabayashi T, Waki K. Method for ejecting cestodes: duodenal tube injection of gastrografin. AJR Am J Roentgenol. 1984;143:111-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Amano M, Fukumoto A, Yamao K, Imagawa H, Hashimoto Y, Iiboshi T, Onogawa S, Hirano N, Hanada K, Yonehara S. Successful treatment of enteric anisakiasis through endoscopic extraction using a double-balloon enteroscope. Gastroenterol Endosc. 2013;55:1643-1649. [DOI] [Full Text] |
| 12. | Yamamoto K, Kurihara T, Fukuo Y. A unique and simple treatment method for anisakiasis. Nihon Ika Daigaku Zasshi. 2012;8:179-180. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Ramos L, Alonso C, Guilarte M, Vilaseca J, Santos J, Malagelada JR. Anisakis simplex-induced small bowel obstruction after fish ingestion: preliminary evidence for response to parenteral corticosteroids. Clin Gastroenterol Hepatol. 2005;3:667-671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Kasuya S, Goto C, Ohtomo H. Studies on prophylaxis against anisakiasis--a screening of killing effects of extracts from foods on the larvae. Kansenshogaku Zasshi. 1988;62:1152-1156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |