Published online Oct 15, 2009. doi: 10.4253/wjge.v1.i1.61
Revised: August 26, 2009
Accepted: September 2, 2009
Published online: October 15, 2009
AIM: To investigate the protective effect of subserosal injection of hyaluronic acid (HA) after endoscopic resection (ER) using ex vivo and in vivo studies.
METHODS: As the first examination, technical application of subserosal injection was tested 10 times using resected porcine stomachs. As the second examination, ER was applied to make six mucosal defects per stomach in three live minipigs and thermal damage was given on the proper muscle layer by using hemostatic forceps. Following the thermocoagulation, 1 mL of normal saline and HA, respectively, was injected targeting the subserosal layer in two mucosal defects each and the rest kept no injection as the control. The minipigs were recovered from the anesthesia and kept fasting until euthanasia which was carried out around 24 h after the procedures.
RESULTS: Ex vivo study revealed that complete and partial subserosal injection was possible two (20%) and four (40%) times, respectively. In vivo study revealed that no postoperative perforation occurred at any point of the thermocoagulation. Apparent retention of hyaluronic acid was identified at only two (33%) points where HA was injected.
CONCLUSION: This study failed to show preventative effects of subserosal injection of HA on postoperative perforation due to technical faults. However, this concept has a possibility to change strategy of ER with further technical innovation.
- Citation: Niimi K, Fujishiro M, Kodashima S, Ono S, Goto O, Yamamichi N, Koike K. Subserosal injection of hyaluronic acid may prevent perforation after endoscopic resection. World J Gastrointest Endosc 2009; 1(1): 61-64
- URL: https://www.wjgnet.com/1948-5190/full/v1/i1/61.htm
- DOI: https://dx.doi.org/10.4253/wjge.v1.i1.61
Owing to the remarkable development in therapeutic endoscopy, epithelial neoplasms in the gastrointestinal (GI) tract those fulfill the node-negative criteria of each organ have been endoscopically resected, especially in Japan[1,2]. Endoscopic mucosal resection (EMR), that is inject, cut technique or inject, suck, cut technique, is a conventional method applied for a small and non-ulcerative neoplasms and endoscopic submucosal dissection (ESD), that is inject, mucosal incision, submucosal cut technique with electrosurgical knife, is a relatively novel method applied for a large or ulcerative neoplasms[3]. When the target becomes more complex, complications accompanying these techniques frequently occurred.
Most commonly-encountered complications are bleeding and perforation and these complications are divided into intraoperative and postoperative ones. Bleeding can be managed by thermocoagulation or endoscopic clipping and, even if the attempts fail, blood transfusion can rescue disturbed patient’s condition in almost all cases as a final consideration in both of intraoperative and postoperative occasions. In terms of perforation, it is now considered that the intraoperative perforation can be successfully managed without surgical rescue when endoscopic closure of the perforation is completed[4-6]. However, postoperative perforation still needs surgical rescue because gut contents are poured out into the abdominal cavity at the time of notification and endoscopic procedures to close the perforation is quite risky with deteriorated conditions of the patients. Although the reason for postoperative perforation is still an open question, one of the major reasons may be excessive thermal injury to the remnant gut wall (the proper muscle layer) at the site of mucosal resection during the operation, which results in necrotic perforation.
Hyaluronic acid is a thick substance with high viscosity that is widely found in connective tissues. The current approved indications for its use in clinical practice in many countries, including Japan, Europe and the United States, are for intra-articular injections for osteoarthritis, as well as in eye surgery[7]. In Japan, it is also approved for submucosal injection material to lift the lesion from the proper muscle layer during endoscopic resection[8,9]. From the viscous nature of hyaluronic acid, we hypothesized that subserosal injection through the proper muscle layer after endoscopic resection might prevent from postoperative perforation. So we conducted this animal study to investigate whether our hypothesis was acceptable or not.
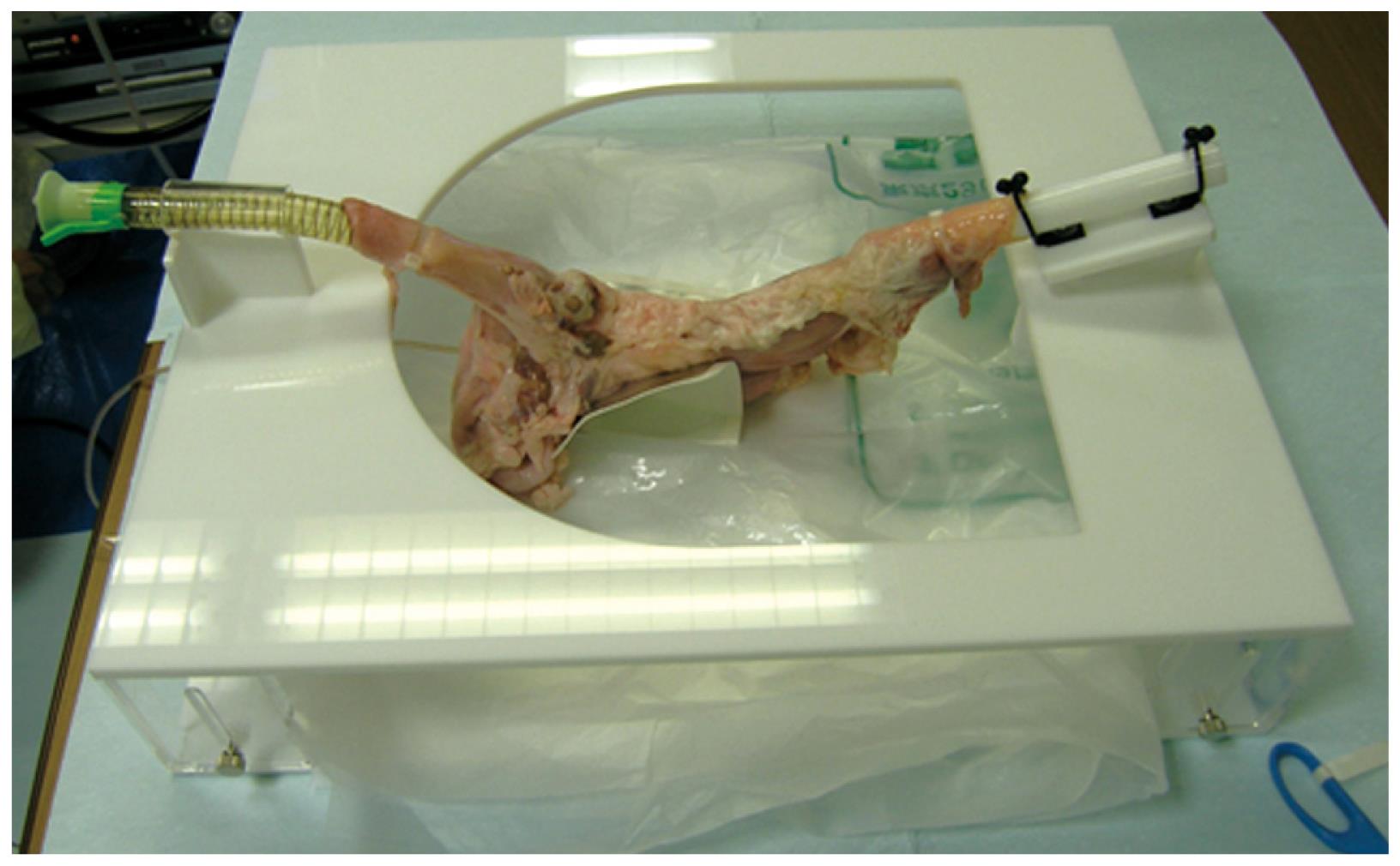
As the first examination, two resected porcine stomachs within a few hours after euthanasia was obtained from a butcher to validate the technical application of the injection needle in the subserosal layer after endoscopic resection. The resected stomachs were set on a training system for endoscopic procedure (Figure 1) after washing the residue and mucus on the mucosal surface by normal saline. A slim upper gastrointestinal endoscope (XQ230, Olympus, Tokyo, Japan) was inserted in the stomach and a standard ESD technique[10] by using a flex knife (KD-630L, Olympus) as an electrosurgical knife and normal saline as submucosal injection fluid was performed to make ten mucosal defects in total, about 3 cm in diameter, in different locations of the gastric bodies. Through the exposed proper muscle layer, 1 mL of 0.4% hyaluronic acid preparation (Mucoup, Johnson & Johnson Co., Tokyo, Japan) (HA) was injected targeting the subserosal layer by 23-gauge disposable injection needle (NM-200L-0423, Olympus) and the technical availability of subserosal injection was investigated.
For the second examination, three living minipigs (Sus scrofa; Miniature Swine) were used for an over-night survival study to elucidate the preventive effect of subserosal injection of hyaluronic acid for postoperative perforation. On the first day, endoscopic procedures were performed for the minipigs under general anesthesia after overnight fasting. An endoscope with two instrumental channels (GIF-2TQ240, Olympus) was used for the following entire examination. The stomachs were sufficiently inflated with air after the residue and mucus were washed out with tap water which was splashed from the instrumental channel.
After these preparations, endoscopic mucosal resection (EMR) was applied to make six mucosal defects per stomach with a standard EMR technique by using normal saline injection and an electrocautery snare. The electrosurgical unit used was VIO 300D (ERBE Elektromedizin, Tübingen, Germany), which employed a special coagulation current, soft coagulation current. After more than 30 min of the EMR procedure when the normal saline injected for EMR in the submucosal layer was absorbed into surrounding tissues, thermal damage was given on the proper muscle layer by using hemostatic forceps (Coagrasper, Olympus) at the settings of soft coagulation mode, effect 5, 50 watts for 10 s. The muscular damage imitated thermal damage for treatment of non-bleeding and bleeding vessels on the proper muscle layer during and immediately after endoscopic resection[11].
Following the thermocoagulation, 1 mL of normal saline and HA, respectively, was injected targeting the subserosal layer through the proper muscle layer by using the injection needle in two mucosal defects each to elucidate protective effects of postoperative perforation. The rest kept no injection as the control. The minipigs were recovered from the anesthesia and kept fasting until euthanasia which was carried out around 24 h after the procedures.
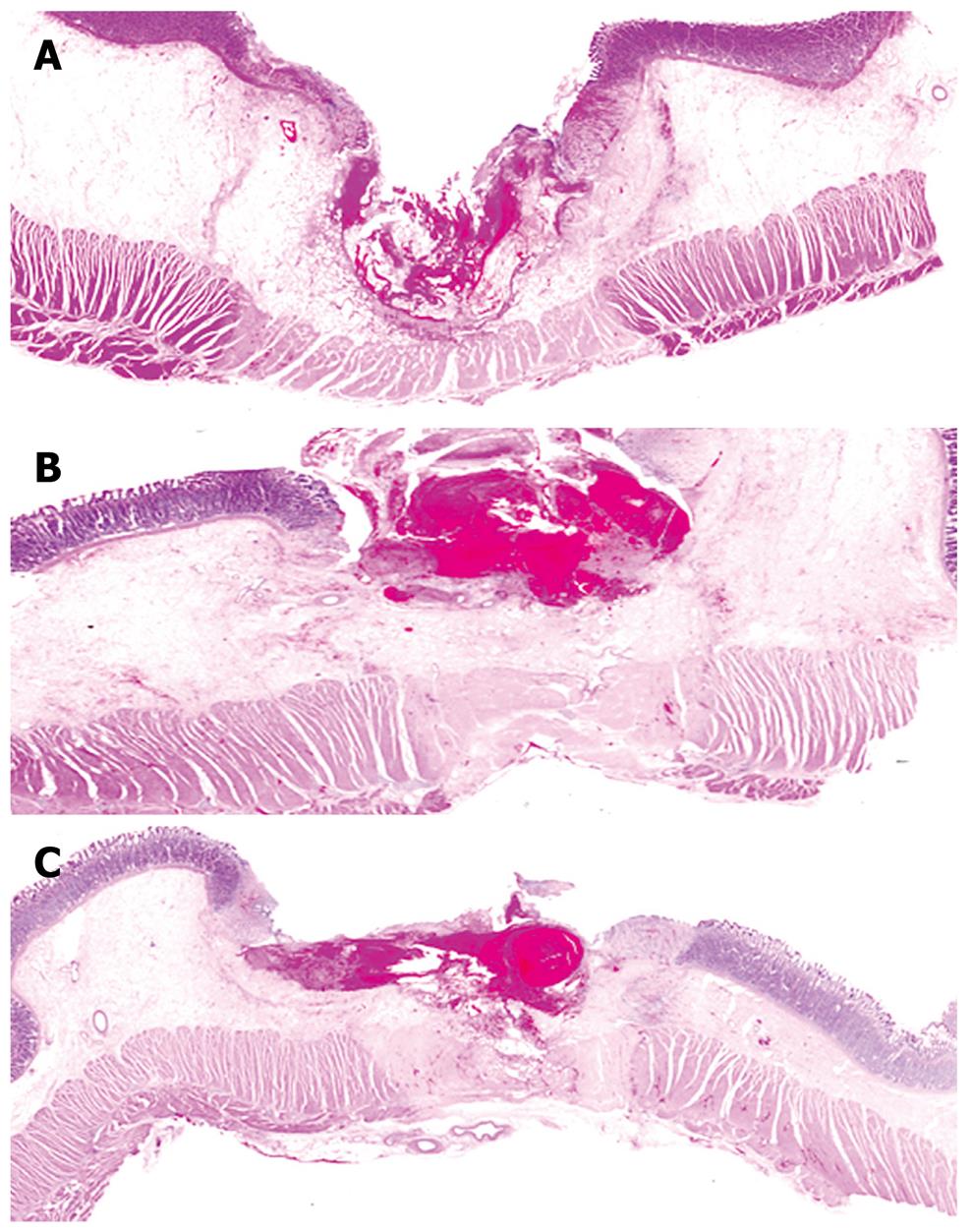
The retrieved stomachs were cut on the points of coagulation and fixed with formalin and embedded in paraffin. A histological section was made from each block, stained with hematoxylin and eosin, and examined tissue damage microscopically.
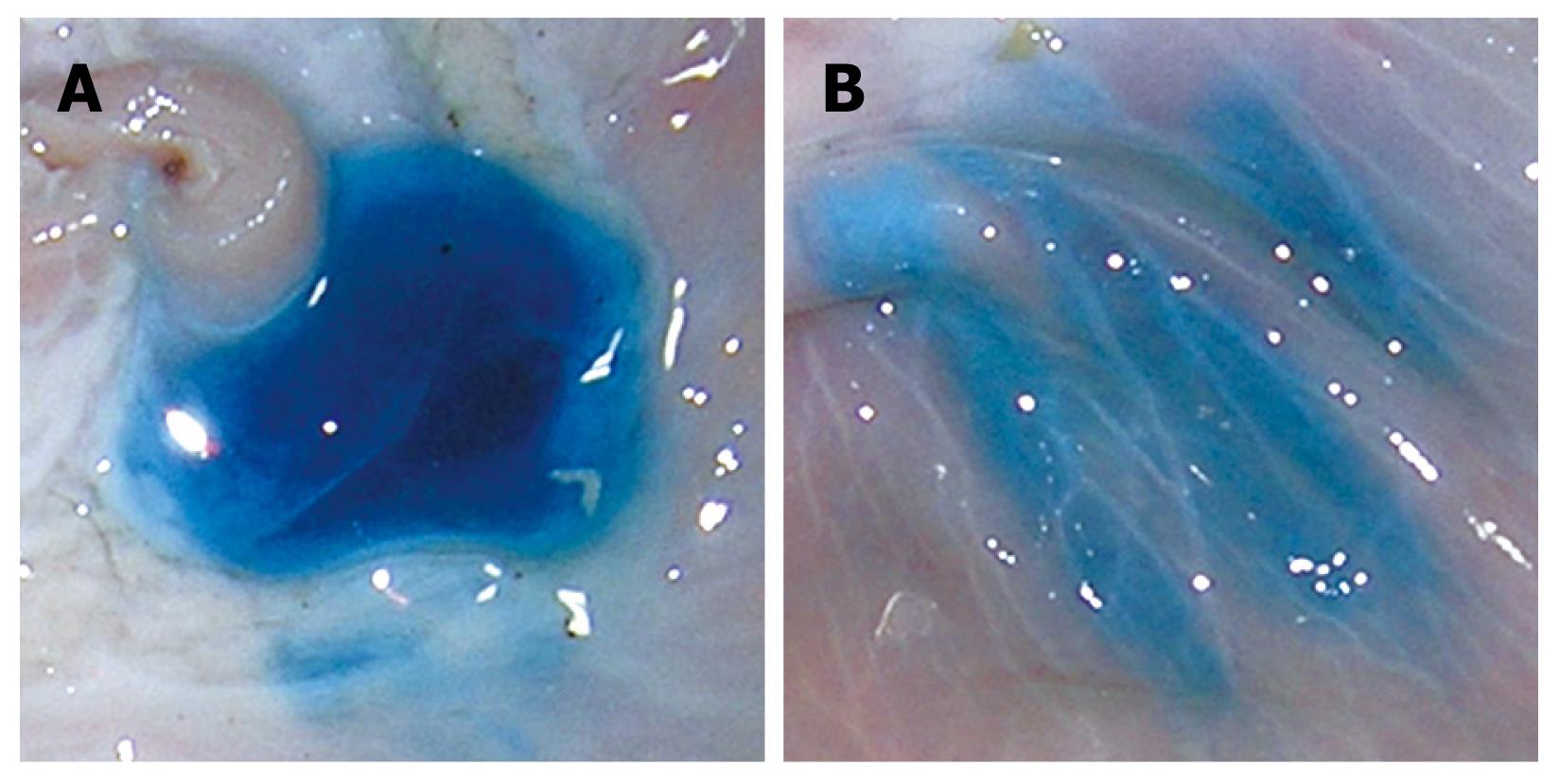
Ex vivo study by using the resected stomachs revealed that precise placement of HA in the subserosal layer was possible twice among ten trials. The rest was partial subserosal retention with intra-muscular and submucosal retention four times, intra-muscular and submucosal retention without subserosal retention twice, and no retention due to needle placement outside the wall twice (Figure 2).
In vivo study of the minipigs revealed that transmural tissue damage due to thermocoagulation was observed in 50% (3/6), 50% (3/6), and 50% (3/6) of the points where saline, HA, and nothing were injected, respectively. However, no postoperative perforation occurred at any point of the thermocoagulation. In terms of possible protective effects of postoperative perforation by subserosal injection, apparent identification of the subserosal layer, which was expected to be retaining of injected material, was observed at only two points where HA was injected (Table 1). The representative histological sections of each group were shown in Figure 3.
| Perforation, % | Extent of muscular damage | Identification of subserosa (%) | ||||
| 0 | < 50% | > 50% | 100% | |||
| Normal saline (n = 6) | 0 | 1 | 1 | 1 | 3 | 0 |
| Hyaluronic acid (n = 6) | 0 | 1 | 1 | 1 | 3 | 33 |
| Non-injection (n = 6) | 0 | 1 | 1 | 1 | 3 | 0 |
This study did not reveal the usefulness of subserosal injection through the proper muscle layer after endoscopic resection to prevent from postoperative perforation. The biggest fault of our pilot study may be an estimate that appropriate placement of hyaluronic acid in the subserosal layer were surely possible by using a commonly-used injection needle. However, in the ex vivo study, only 20% (2/10) and 40% (4/10) of injection, completely and partially, respectively, succeeded in subserosal placement of hyaluronic acid. When the placement was not validated, it was natural not to obtain reliable results from the in vivo study. So we have realized that technical innovation to put hyaluronic acid in the subserosal layer precisely is firstly necessary to advance our study.
Another fault may be the duration for survival after application of thermocoagulation. We considered that duration of 24 h were enough to lead to postoperative perforation. However, as shown in this study, no postoperative perforation was observed, although transmural damage was observed in 50% (9/18) of thermocoagulation. So longer duration, such as 2 d or more after thermocoagulation may be necessary to result in postoperative perforation even in case of transmural damage. Because the same application of thermocoagulation was impossible in the in vivo setting, it was acceptable to result that only half of the application had transmural damage. The disadvantage may be overcome when more cases were tested.
Although there were these faults in our pilot study, we believe that this study is meaningful in terms of a new foothold to cope with the rare but serious complication, postoperative perforation. When the protective effect on tissue destruction is elucidated by precise placement of hyaluronic acid into subserosal layer, there are several breakthroughs in addition to preventative effects on postoperative perforation in the field of endoscopic resection as follows: First, little possibility of postoperative perforation even in the small intestine which has the thinnest wall in the GI tract may result in intensive treatments of bleeding or non-bleeding visible vessels on the mucosal defect during and after mucosal resection. This should lead to a less frequency of postoperative bleeding[12]. Closure of the mucosal defect after endoscopic resection may be unnecessary for the fear of postoperative perforation, although preventative effect on postoperative bleeding should be considered as another possible indication. Second, the targets for endoscopic resection may be technically extended into non-lifting lesions which stick on the proper muscle layer without fear of transmural thermal injury, because detachment of these lesions just on the proper muscle layer or at the level of internal muscle layer is necessary. Third, retention of the substance into the subserosal layer may lead to not only protective effect of tissue destruction, but also acceleration of healing process, although there is no supportive data so far. Mixture of several promising molecules such as growth factors may be useful for healing of the injured site.
In summary, this study failed to show preventative effects of subserosal injection of hyaluronic acid on postoperative perforation. The main reason is technical difficulty in precise placement of hyaluronic acid into the subserosal layer. However, technical innovation in the near future enables to place it precisely, which has a possibility to change strategy of endoscopic resection in the GI tract.
Endoscopic resection of gastrointestinal tumors can replace surgical organ resection to some extent. Due to the technical limitation, however, some serious complications concerning endoscopic resection may occur.
One of rare but serious complications of endoscopic resection is post-operative perforation. The possible cause is transmural tissue damage due to thermocoagulation and there is no knowledge to prevent it so far.
This study shows the first attempt to make subserosal injection of hyaluronic acid and its preventative effect on postoperative perforation.
Although technical refinement should be necessary, the concept to make subserosal injection is promising.
Endoscopic mucosal resection: Endoscopic resection by the following sequences: marking, submucosal injection, snaring, and cut. Endoscopic submucosal dissection: Endoscopic resection by the following sequences: marking, submucosal injection, mucosal incision, and submucosal dissection. Hyaluronic acid: Non-antigenic thick substance for human with high viscosity that is widely found in human connective tissues.
There is novelty and innovation in the research field and this study may change the strategy of endoscopic resection in the gastrointestinal tract with further efforts.
Peer reviewer: Simon K Lo, MD, Division of Gastroenterology, Cedars-Sinai Medical Center, Los Angeles, CA 90048, United States
S- Editor Zhang HN L- Editor Negro F E- Editor Ma WH
| 1. | Kakushima N, Fujishiro M. Endoscopic submucosal dissection for gastrointestinal neoplasms. World J Gastroenterol. 2008;14:2962-2967. [Cited in This Article: ] |
| 2. | Fujishiro M. Perspective on the practical indications of endoscopic submucosal dissection of gastrointestinal neoplasms. World J Gastroenterol. 2008;14:4289-4295. [Cited in This Article: ] |
| 3. | Kantsevoy SV, Adler DG, Conway JD, Diehl DL, Farraye FA, Kwon R, Mamula P, Rodriguez S, Shah RJ, Wong Kee Song LM. Endoscopic mucosal resection and endoscopic submucosal dissection. Gastrointest Endosc. 2008;68:11-18. [Cited in This Article: ] |
| 4. | Taku K, Sano Y, Fu KI, Saito Y, Matsuda T, Uraoka T, Yoshino T, Yamaguchi Y, Fujita M, Hattori S. Iatrogenic perforation associated with therapeutic colonoscopy: a multicenter study in Japan. J Gastroenterol Hepatol. 2007;22:1409-1414. [Cited in This Article: ] |
| 5. | Fujishiro M, Yahagi N, Kakushima N, Kodashima S, Muraki Y, Ono S, Kobayashi K, Hashimoto T, Yamamichi N, Tateishi A. Successful nonsurgical management of perforation complicating endoscopic submucosal dissection of gastrointestinal epithelial neoplasms. Endoscopy. 2006;38:1001-1006. [Cited in This Article: ] |
| 6. | Minami S, Gotoda T, Ono H, Oda I, Hamanaka H. Complete endoscopic closure of gastric perforation induced by endoscopic resection of early gastric cancer using endoclips can prevent surgery (with video). Gastrointest Endosc. 2006;63:596-601. [Cited in This Article: ] |
| 7. | Fujishiro M, Yahagi N, Kashimura K, Mizushima Y, Oka M, Enomoto S, Kakushima N, Kobayashi K, Hashimoto T, Iguchi M. Comparison of various submucosal injection solutions for maintaining mucosal elevation during endoscopic mucosal resection. Endoscopy. 2004;36:579-583. [Cited in This Article: ] |
| 8. | Yamamoto H, Yahagi N, Oyama T, Gotoda T, Doi T, Hirasaki S, Shimoda T, Sugano K, Tajiri H, Takekoshi T. Usefulness and safety of 0.4% sodium hyaluronate solution as a submucosal fluid "cushion" in endoscopic resection for gastric neoplasms: a prospective multicenter trial. Gastrointest Endosc. 2008;67:830-839. [Cited in This Article: ] |
| 9. | Hirasaki S, Kozu T, Yamamoto H, Sano Y, Yahagi N, Oyama T, Shimoda T, Sugano K, Tajiri H, Takekoshi T. Usefulness and safety of 0.4% sodium hyaluronate solution as a submucosal fluid "cushion" for endoscopic resection of colorectal mucosal neoplasms: a prospective multi-center open-label trial. BMC Gastroenterol. 2009;9:1. [Cited in This Article: ] |
| 10. | Kodashima S, Fujishiro M, Yahagi N, Kakushima N, Ichinose M, Omata M. Endoscopic submucosal dissection for gastric neoplasia: experience with the flex-knife. Acta Gastroenterol Belg. 2006;69:224-229. [Cited in This Article: ] |
| 11. | Fujishiro M, Yahagi N, Kakushima N, Kodashima S, Muraki Y, Tateishi A, Omata M. Management of bleeding concerning endoscopic submucosal dissection with the flex knife for stomach neoplasm. Dig Endosc. 2006;18:S119-S122. [Cited in This Article: ] |