Copyright
©The Author(s) 2015.
World J Gastrointest Endosc. Sep 25, 2015; 7(13): 1107-1113
Published online Sep 25, 2015. doi: 10.4253/wjge.v7.i13.1107
Published online Sep 25, 2015. doi: 10.4253/wjge.v7.i13.1107
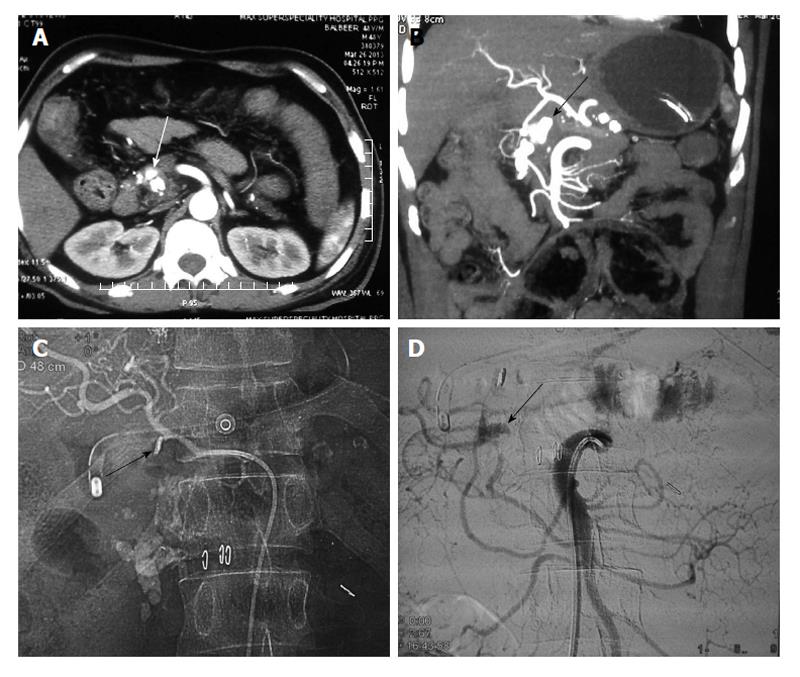
Figure 1 Chronic calcific pancreatitis with pseudoaneurysm of gastroduodenal artery (case 1).
A: Axial Contrast enhanced; B: Coronal MIP (3-D reformatted) CT images; C: Angiographic spot image; D: Superior mesenteric DSA image. There is a pseudoaneurysm (arrow, A and B) arising from the gastroduodenal artery, which is filling from pancreatic arcade (Inferior pancreatic branches from SMA, D), because of metallic clip placed surgically at the origin of gastroduodenal artery origin (arrow, C). CT: Computed tomography; MIP: Maximum intensity projection; DSA: Digital substraction angiography; SMA: Superior mesenteric artery.
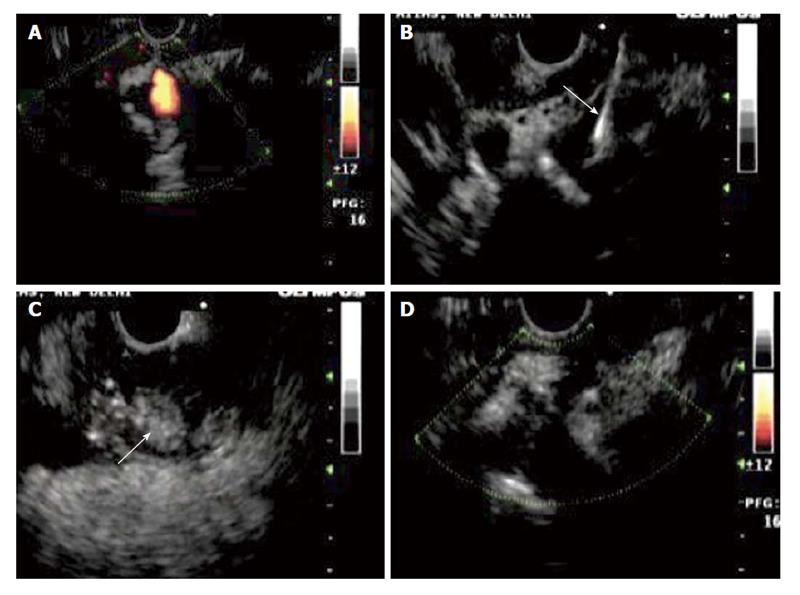
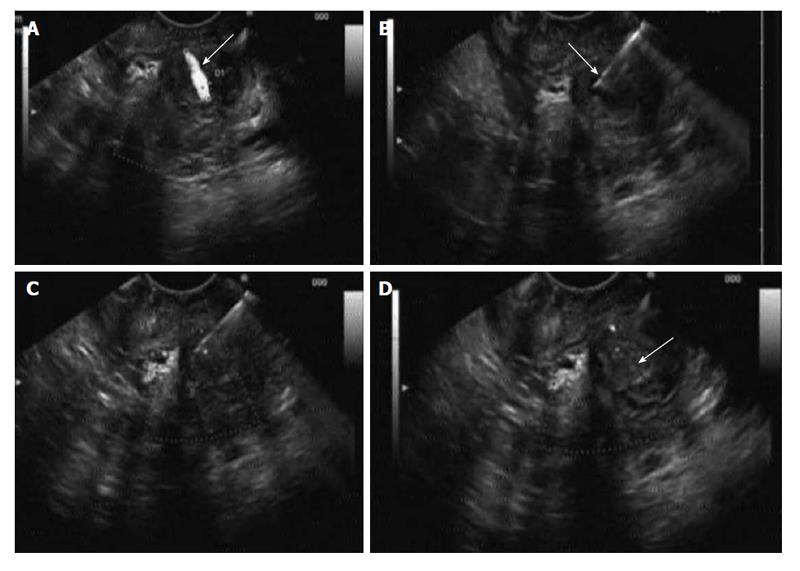
Figure 2 Endoscopic ultrasound guided thrombin instillation procedure (case 1).
A-D: Endoscopic ultrasound images. There is a pseudoaneurysm sac (A) filling from pancreatic arcade (shown in Figure 1) with EUS needle (arrow, B) in the center of pseudoaneurysm sac with formation of echogenic thrombus (arrow, C) within the pseudoaneurysm sac following thrombin injection; D: No flow is seen within the pseudoaneurysm sac suggesting successful obliteration of pseudoaneurysm sac. EUS: Endoscopic ultrasound.
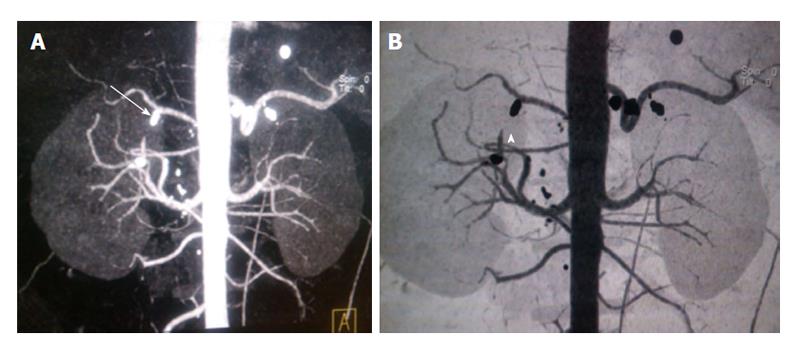
Figure 3 Follow up scan following thrombin injection procedure (case 1).
A and B: Coronal MIP (3-D reformatted) CT images. There is non-visualization of the pseudoaneurysm sac (arrowhead, B) with metallic clip (arrow, A) seen at the gastroduodenal artery stump due to previous laparoscopic surgical clipping. CT: Computed tomography; MIP: Maximum intensity projection.
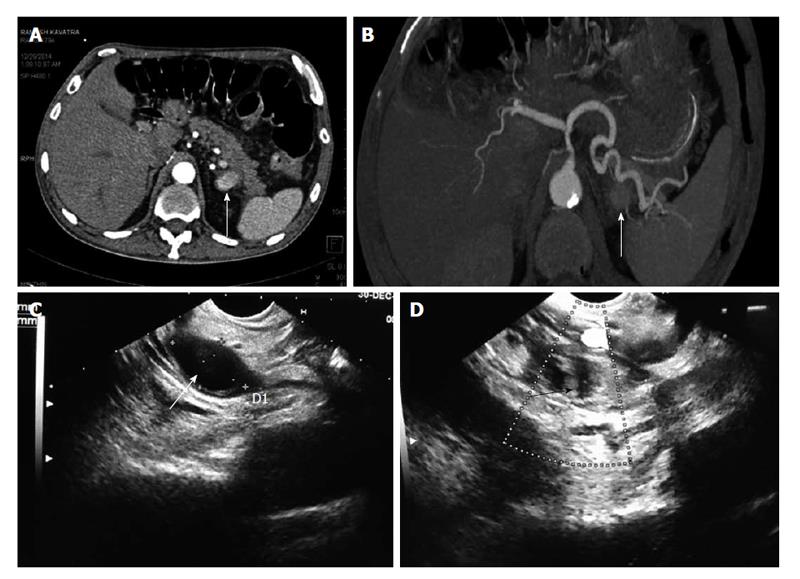
Figure 4 Pancreatitis related pseudoaneurysm (case 2).
A: Axial contrast enhanced CT; B: Coronal maximum intensity projection CT images; C and D: Digital substraction Images. In the background of pancreatitis there is a pseudoaneurysm in the distal body of the pancreas (arrow, A and B) which was not revealed on either left gastric artery (C) or splenic artery (D) angiograms. CT: Computed tomography.
Figure 5 Endoscopic ultrasound guided thrombin instillation procedure (case 2).
A-D: Endoscopic ultrasound images. There is a pseudoaneurysm sac (arrow, A) within pancreatic body region (A) with endoscopic ultrasound needle (arrow, B) inside the pseudoaneurysm sac, which was managed by instillation of thrombin (C) with subsequent thrombosis of the pseudoaneurysm sac as shown by echogenic pseudoaneurysm sac (arrow, D).
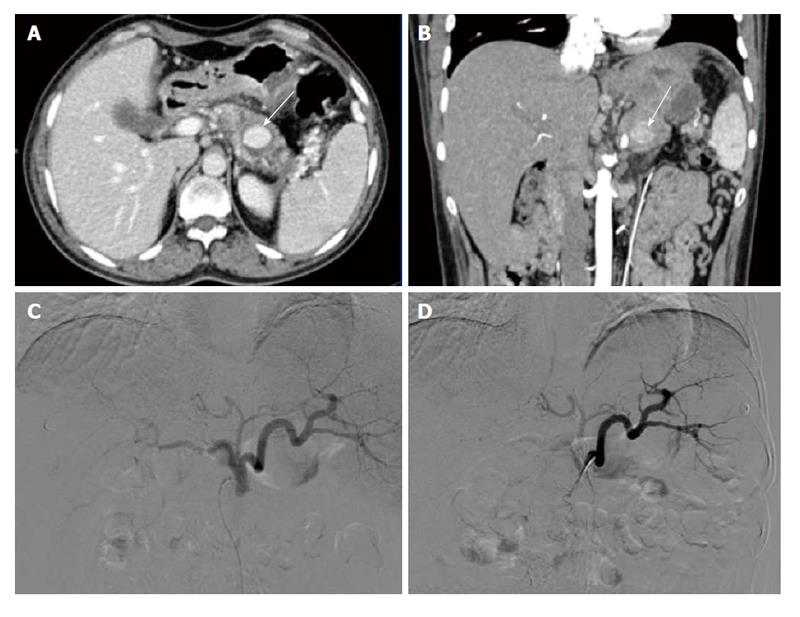
Figure 6 Chronic calcific pancreatitis with upper gastrointestinal bleed.
A: Axial contrast enhanced; B: Axial MIP (3-D reformatted) CT images; C and D: Endoscopic ultrasound images. There is a pseudoaneurysm sac (arrow, A) in relation to distal body of the pancreas, in close relation to the splenic artery (arrow, B) and confirmed by endoscopic ultrasound (arrow, C) and subsequently managed by instillation of thrombin under EUS guidance with complete thrombosis of the pseudoaneurysm was achieved as revealed by the transformation of the previously anechoic lesion to an echogenic sac (arrow, D). CT: Computed tomography; MIP: Maximum intensity projection; EUS: Endoscopic ultrasound.
- Citation: Gamanagatti S, Thingujam U, Garg P, Nongthombam S, Dash NR. Endoscopic ultrasound guided thrombin injection of angiographically occult pancreatitis associated visceral artery pseudoaneurysms: Case series. World J Gastrointest Endosc 2015; 7(13): 1107-1113
- URL: https://www.wjgnet.com/1948-5190/full/v7/i13/1107.htm
- DOI: https://dx.doi.org/10.4253/wjge.v7.i13.1107