Published online Sep 27, 2010. doi: 10.4254/wjh.v2.i9.354
Revised: August 14, 2010
Accepted: August 21, 2010
Published online: September 27, 2010
Although hepatic tuberculosis is not a rare disease entity, tubercular liver abscess (TLA) is extremely rare. It is usually associated with foci of infection either in the lung and/or gastrointestinal tract or with an immunocompromised state. An isolated or primary TLA with no evidence of tuberculosis elsewhere is even rarer. We report on a 28 year old man who developed an isolated tuberculous liver abscess not associated with lung involvement. Ultrasonography and computed tomography of the abdomen showed the abscess lesions in the liver but the diagnosis of tuberculosis was confirmed by histological examination of the wall of the abscess after surgical drainage. Although tuberculous liver abscess is very rare, it should be included in the differential diagnosis of abscess and unknown hepatic mass lesions.
- Citation: Hassani KIM, Ousadden A, Ankouz A, Mazaz K, Taleb KA. Isolated liver tuberculosis abscess in a patient without immunodeficiency: A case report. World J Hepatol 2010; 2(9): 354-357
- URL: https://www.wjgnet.com/1948-5182/full/v2/i9/354.htm
- DOI: https://dx.doi.org/10.4254/wjh.v2.i9.354
Isolated tubercular abscess of liver is a very rare form of extrapulmonary tuberculosis, even in countries where tuberculosis is an alarming public health problem. The diagnosis is usually difficult and is frequently confused with pyogenic or amoebic liver abscess.
The histological examination of the liver and the specific treatment with anti-tuberculous agents led to the final diagnosis of tuberculous liver abscess. In this report, we describe a rare case of tuberculous liver abscess with no evidence of infection in the lung or gastrointestinal tract in a patient without immunodeficiency.
We report on a case of 28 year old man who presented to the emergency department with non-radiating pain in the right hypochondrium and epigastrium associated with vomiting, intermittent fever with chills and rigors, anorexia and weight loss for 17 d. There was no previous history of tuberculosis (TB) or contact with any patient with TB. At the time of admission, the physical examination revealed a conscious man with a temperature of 39°C, dehydration and who looked very ill with a pulse rate of 98/min, blood pressure 100/75 mmHg and respiratory rate of 19/min. There was no jaundice or lymphadenopathy. Abdominal examination revealed a painful hepatomegaly, the liver span was 16 cm and there was no splenomegaly, ascites or any other palpable mass in his abdomen. Respiratory and cardiovascular system (CVS) examination revealed no abnormality.
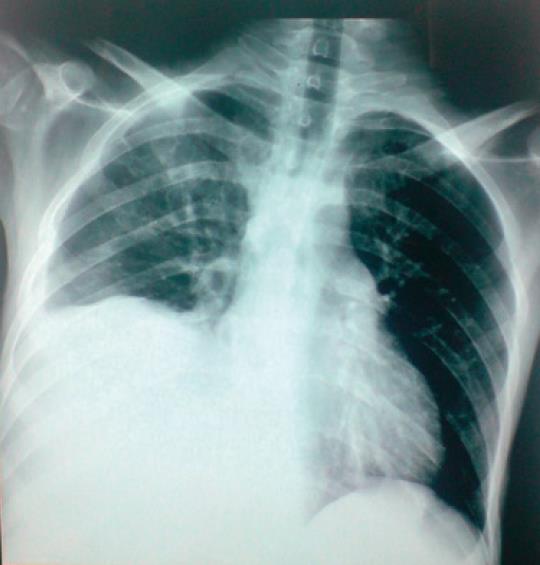
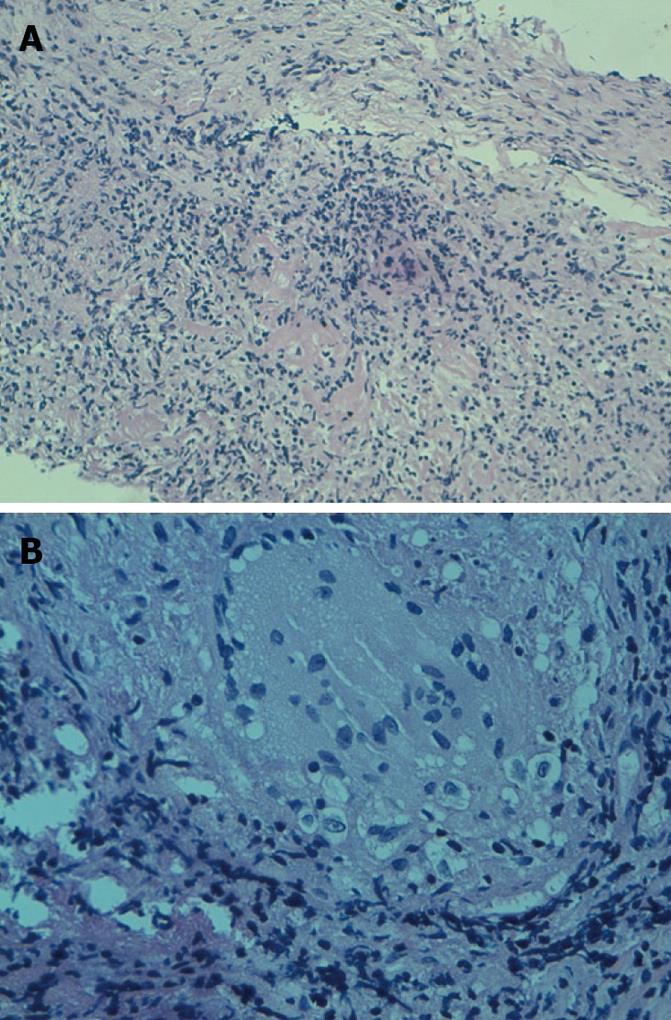
Laboratory data revealed hematocrit 26%; hemoglobin 9.6 g/dL; white blood cells 13 300/mm³ (78% neutrophils); blood urea 0.25g/; and creatinine level 10 mg/L. Liver enzymes showed a total bilirubin of 13mg/L with a direct component of 6 mg/L; SGOT and SGPT were 77 U/L and 96 U/L respectively (normal range for SGOT is 17-59 U/L and for SGPT is 21-72 U/L). The patient was non-reactive in HIV serology. Chest X-ray showed no lesion suggestive of TB but revealed a right-sided subdiaphragmatic pathology as the right hemi-diaphragm was raised and the costophrenic angle was blunted (Figure 1). Pleural biopsy was performed and histological examination showed no signs of TB. Ultrasonography (US) of the abdomen revealed ill-defined, heterogeneous hypo-echoic lesions reaching up to the liver surface with cystic areas in the right lobe of the liver suggestive of an abscess (Figure 2). Liver was enlarged with a span of 16.6 cm with no other focal lesion. No perihepatic effusion was seen. All other abdominal viscera appeared normal with no free fluid. A computerised tomographic (CT) scan of abdomen revealed a 14 cm/12 cm/7 cm multiseptate abscess in the right lobe of liver (Figure 3) for which a US guided aspiration of 250 cc of yellow colored pus was carried out. The aspiration material showed 10 200 leukocytes/L with 9200 neutrophils/L. Gram staining of the aspiration fluid and Ziehl-Neelsen staining for acid-fast bacteria were negative. Routine bacteriological cultures of the aspiration fluid were negative for bacterial infection and fungus. The patient was started on third generation cephalosporin and aminoglycoside with the provisional diagnosis of pyemic liver abscess. Despite this treatment, the patient’s symptoms worsened. A repeat CT scan of the abdomen showed a persistence of the right lobe liver abscess. In view of the patient’s condition and the refilling of the multiseptate abscess cavity, a decision to perform a laparotomy was taken. During the surgical exploration, a multiseptate intraparenchymal liver abscess was seen in the right lobe with no other positive abdominal findings. 750 cc of thick yellow colored pus was drained and after breaking of all of the loculi, a biopsy of the hull of the abscess was performed and the liver cavity was closed over a tube drain, the output of which in the initial period was about 250 cc and decreased after 5 d. The drain was removed one week post operatively. Histological examination of the biopsy showed Tuberculosis follicle with central caseous necrosis surrounded by lymphocytes, multi-nucleate giant cells and epithelioid macrophages (Figure 4). The polymerase chain reaction (PCR) of the specimen for Mycobacterium tuberculosis was not performed because it was not available in the hospital and because the culture in Löwenstein-Jensen medium using the specimen revealed Mycobacterium tuberculosis and confirmed the diagnosis of tuberculosis.
Four drugs for antitubercular therapy (Rifampicin, Isoniazid, Ethambutol and Pyrazinamide) were started. The patient had an uneventful postoperative therapy. At 4 wk follow up he was asymptomatic and the hepatomegaly had regressed. The repeat sonography of abdomen at 2 mo showed a complete resolution of the abscess cavity.
In extra pulmonary TB, hepatic tuberculosis has been regarded as a rare but not exceptional form of TB[1]. Tuberculous liver abscess (TLA), however, is extremely rare. Most of cases usually occur in association with miliary lung tuberculosis, mainly through hematogenous dissemination[2]. In our patient there was no evidence of any pulmonary or gastrointestinal tuberculosis. The first description of TLA was given by Bestowe in 1858[3]. The prevalence of TLA was just 0.34% in patients with hepatic tuberculosis, as shown in a study where the patient age ranged from 6 mo to 72 years with an average age of 39.2 years[4]. TLA is frequently confused with hepatoma, amoebic liver abscess and pyogenic liver abscess, as in the case of our patient. Because of the non-specific clinical presentation, the diagnosis of TLA is usually made at autopsy or occasionally after laparotomy has been performed[5]. The symptoms and signs of TLA are non-specific and include fever, vague abdominal pain, anorexia and weight loss[6]. Hepatomegaly is a common physical finding[7]. Jaundice is seldom encountered and may be caused by extra or intrahepatic obstruction[8]. No clear relationship exists between the degree of liver involvement and jaundice[9]. US and CT scan findings have a low specificity in TLA[10]. However, they are very helpful in delineating the site, the size and multiseptate nature of the abscess[11,12]. Their finding usually reflects different stages of disease varying from granulomatous tubercles with or without caseous necrosis to fibrosis and calcification in the healing stage[2]. Confirmation of the diagnosis depends on demonstration of acid-fast bacilli (AFB) in the aspirated pus, pus culture showing Mycobacterium Tuberculosis, positive ELISA and PCR for Mycobacterium Tuberculosis. AFB is most easily found in caseous necrotic material but even the absence of AFB should not detract from diagnosis, especially in a high TB prevalence country such as ours, as is evident from some other studies[1]. Recently, PCR assay was demonstrated to be useful in a diagnosis of hepatic tuberculosis[13,14]. Anti tubercular therapy alone or percutaneous aspiration along with antitubercular therapy are the preferred therapeutic options[5]. Quadruple therapy with antitubercular drugs is recommended for 1 year which was effectively advocated in our patient[7]. Gracey postulates that thick fibrous tissue around the abscesses and their large size may prevent antibiotics from reaching the target[15]. In some cases, TLA have been successfully treated by percutaneous drainage combined with transcatheter infusion of antitubercular drugs[6,16]. Surgery is reserved for cases in which percutaneous aspiration is not successful or not possible because of site and multiseptate nature of the abscess[17]. The diagnosis of LT is established by histological examination of the abscess wall which can show the characteristic aspect of a Tuberculosis follicle with central caseous necrosis surrounded by lymphocytes, multi-nucleate giant cells and epithelioid macrophages, as also seen in our patient. In our patient, the decision to operate was taken after CT scan because the percutaneous aspiration failed to drain the pus and the abscess was multiseptate and not accessible to percutaneous aspiration.
In conclusion, isolated hepatic tubercular liver abscess, although very rare, should always be considered in the differential diagnosis of multiloculated abscess and unknown hepatic mass lesions. Symptoms and radiological findings of the disease are commonly non-specific and the ultimate diagnosis depends upon the demonstration of AFB in pus, aspirate or biopsy specimen or the necrotic tissue. The prognosis with antitubercular treatment is good.
Peer reviewer: Nattiya Hirankarn, MD, Associated Professor, Immunology Unit, Department of Microbiology, Faculty of Medicine, Chulalongkorn University, Rama 4 road, Bangkok 10330, Thailand
S- Editor Zhang HN L- Editor Roemmele A E- Editor Liu N
| 1. | Bangaroo AK, Malhotra AS: Isolated hepatic tuberculosis. J Ind Assoc Paediatr Surg. 2005;10:105-107. |
| 2. | Hayashi M, Yamawaki I, Okajima K, Tomimatsu M, Ohkawa S. Tuberculous liver abscess not associated with lung involvement. Intern Med. 2004;43:521-523. |
| 4. | Essop AR, Segal I, Posen J, Noormohamed N. Tuberculous abscess of the liver. A case report. S Afr Med J. 1983;63:825-826. |
| 5. | Balsarkar D, Joshi MA. Isolated tuberculous hepatic abscess in a non-immunocompromised patient. J Postgrad Med. 2000;46:108-109. |
| 6. | Kubota H, Ageta M, Kubo H, Wada S, Nagamachi S, Yamanaka T. Tuberculous liver abscess treated by percutaneous infusion of antituberculous agents. Intern Med. 1994;33:351-356. |
| 7. | Baveja CP, Gumma CP, Chaudhary M, Jha H. Primary tubercular liver abscess in an immunocompetent adult: a case report. J Med Case Rep. 2009;3:78. |
| 8. | Desai CS, Joshi AG, Abraham P, Desai DC, Deshpande RB, Bhaduri A, Shah SR: Hepatic tuberculosis in absence of disseminated abdominal tuberculosis. Ann Hepatol. 2006;51:41-43. |
| 9. | Rab SM, Beg MZ. Tuberculous liver abscess. Brit J Clin Pract. 1977;31:157-158. |
| 10. | Polat KY, Aydinli B, Yilmaz O, Aslan S, Gursan N, Ozturk G, Onbas O: Intestinal tuberculosis and secondary liver abscess. Mount Sinai J Med. 2006;73:887-890. |
| 11. | Stevens A, Little JM. Isolated tuberculous hepatic abscess. Aust N Z J Surg. 1987;57:409-411. |
| 13. | Kawashima I, Fusegawa H, Obana M, Matsuoka Y. [A case of AIDS complicated with liver tuberculosis]. Kansenshogaku Zasshi. 2000;74:984-988. |
| 14. | Diaz ML, Herrera T, Lopez-Vidal Y, Calva JJ, Hernandez R, Palacios GR, Sada E. Polymerase chain reaction for the detection of Mycobacterium tuberculosis DNA in tissue and assessment of its utility in the diagnosis of hepatic granulomas. J Lab Clin Med. 1996;127:359-363. |
| 16. | Mustard RA, Mackenzie RL, Gray RG. Percutaneous drainage of a tuberculous liver abscess. Can J Surg. 1986;29:449-450. |
| 17. | Chaudhary A, Wakhlu A. Isolated Tubercular Liver Abscess In Pediatric Age Group. Int JTrop Med. 2005;2:2. |