Published online Aug 27, 2025. doi: 10.4254/wjh.v17.i8.110413
Revised: June 19, 2025
Accepted: July 22, 2025
Published online: August 27, 2025
Processing time: 82 Days and 18.9 Hours
A complete replacement left hepatic artery (LHA) solely originating from the left gastric artery (LGA), with no supply from the hepatic artery proper, is exce
A 62-year-old man underwent laparoscopic radical gastrectomy with D2 Lymphadenectomy for gastric cancer. During dissection of the hepatogastric ligament, an unexpected vascular anatomy was encountered: The LHA originated exclusively from the LGA, with no conventional branch from the hepatic artery proper. Recognizing this variant artery was essential for left liver perfusion, the LGA was ligated proximally near its celiac origin while meticulously preserving blood flow through the anomalous LHA. The gastrectomy and reconstruction were completed without complication. Postoperative recovery was smooth, with serial liver function tests remaining normal, confirming preserved hepatic arterial supply.
Preoperative mapping detected a critical aberrant left hepatic artery; its preservation prevented liver ischemia, ensured safety.
Core Tip: This case report underscores the critical importance of preoperatively clarifying hepatic vascular variations for surgical management. Preoperative imaging allows for confirmation of the specific type of variation and facilitates the development of personalized implementation strategies. These strategies ensure both radical tumor eradication and effective preservation of liver function. This approach provides a new perspective for managing such rare vascular anomalies. Complete details are available in the published article.
- Citation: Gao XX, Xu XX, Chen P, He TX, Du CZ, Zhou Q, Zhou GF, Guo XW, Peng JR, Li HT. Rare complete replacement-type left hepatic artery originating from the left gastric artery: A case report. World J Hepatol 2025; 17(8): 110413
- URL: https://www.wjgnet.com/1948-5182/full/v17/i8/110413.htm
- DOI: https://dx.doi.org/10.4254/wjh.v17.i8.110413
Hepatic arterial variations are critical anatomical considerations in surgical procedures. Preoperative vascular reconstruction to identify variant anatomy allows for personalized surgical planning, ensuring both oncological radicality and preservation of hepatic function. This article reports and analyzes a rare case of a complete replacement-type left hepatic artery (LHA) originating from the left gastric artery (LGA).
A 62-year-old male presented with a 6-month history of dysphagia after eating.
The patient initially ignored mild symptoms, but progressive worsening led to evaluation on March 3, 2025, at Linze County People’s Hospital. Esophagogastroduodenoscopy (EGD) revealed: (1) Cardia/gastric fundus carcinoma; and (2) Chronic atrophic gastritis. Biopsy confirmed gastric adenocarcinoma. No significant weight loss or other symptoms were reported.
No history of hepatitis, tuberculosis, hypertension, diabetes, coronary artery disease, or prior surgeries. No drug allergies or substance abuse.
Resided locally with no exposure to endemic regions. No smoking or alcohol use.
Soft abdomen without distension, venous engorgement, or palpable masses. Mild epigastric tenderness without rebound. Normal bowel sounds; negative Murphy’s sign and shifting dullness.
Liver function shows no abnormality.
EGD: Esophageal gastric mucosal heterotopia; cardia/fundal carcinoma; gastric angle ulcer; active C2 atrophic gastritis.
Pathology: Moderately differentiated adenocarcinoma (fundus); chronic gastritis with intestinal metaplasia (gastric angle).
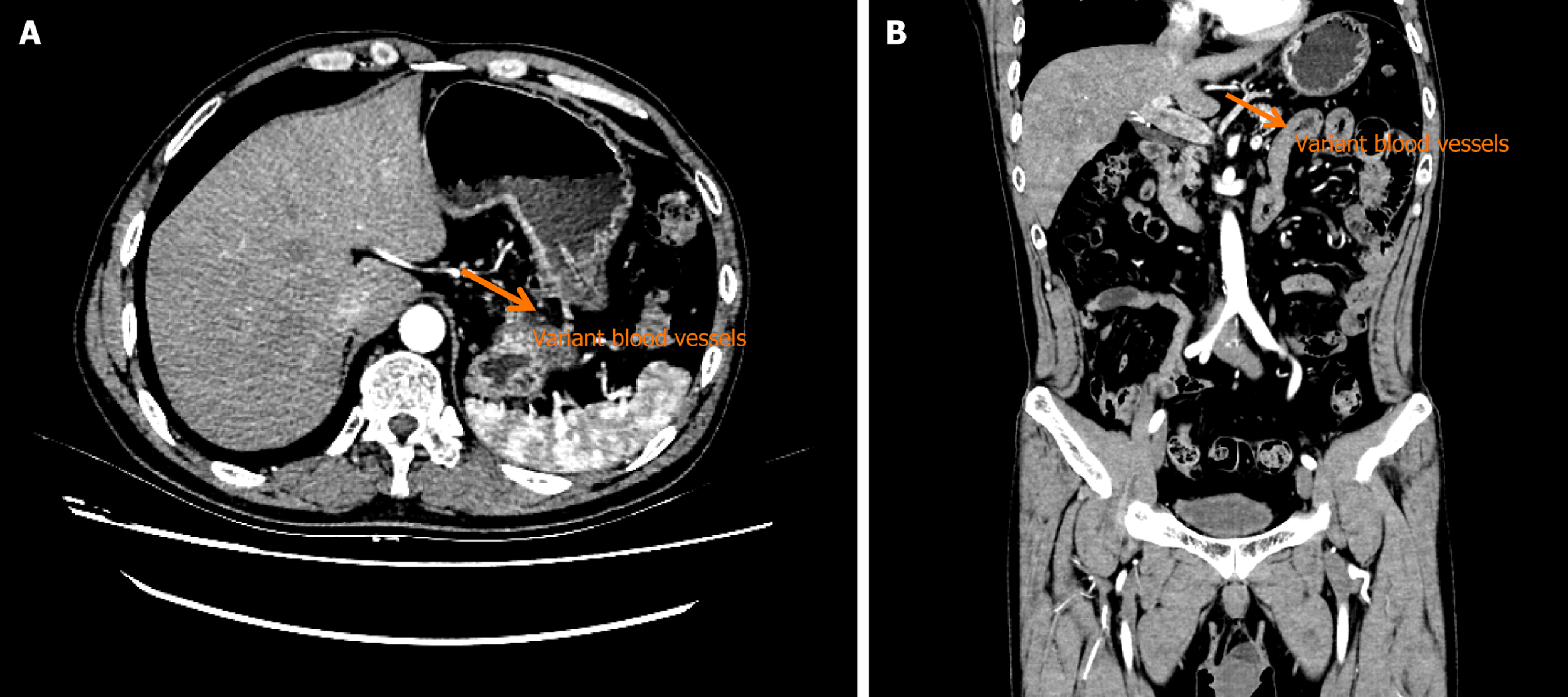
Abdominal contrast-enhanced computed tomography (CT): Irregular thickening of the cardia/fundal wall with heterogeneously enhancing soft tissue. A 1.2 cm × 1.1 cm lymph node in the hepatogastric space. The LHA arose from the mid-segment of the LGA, coursing through the hepatogastric ligament into the left portal vein (Figures 1 and 2).
Gastric adenocarcinoma.
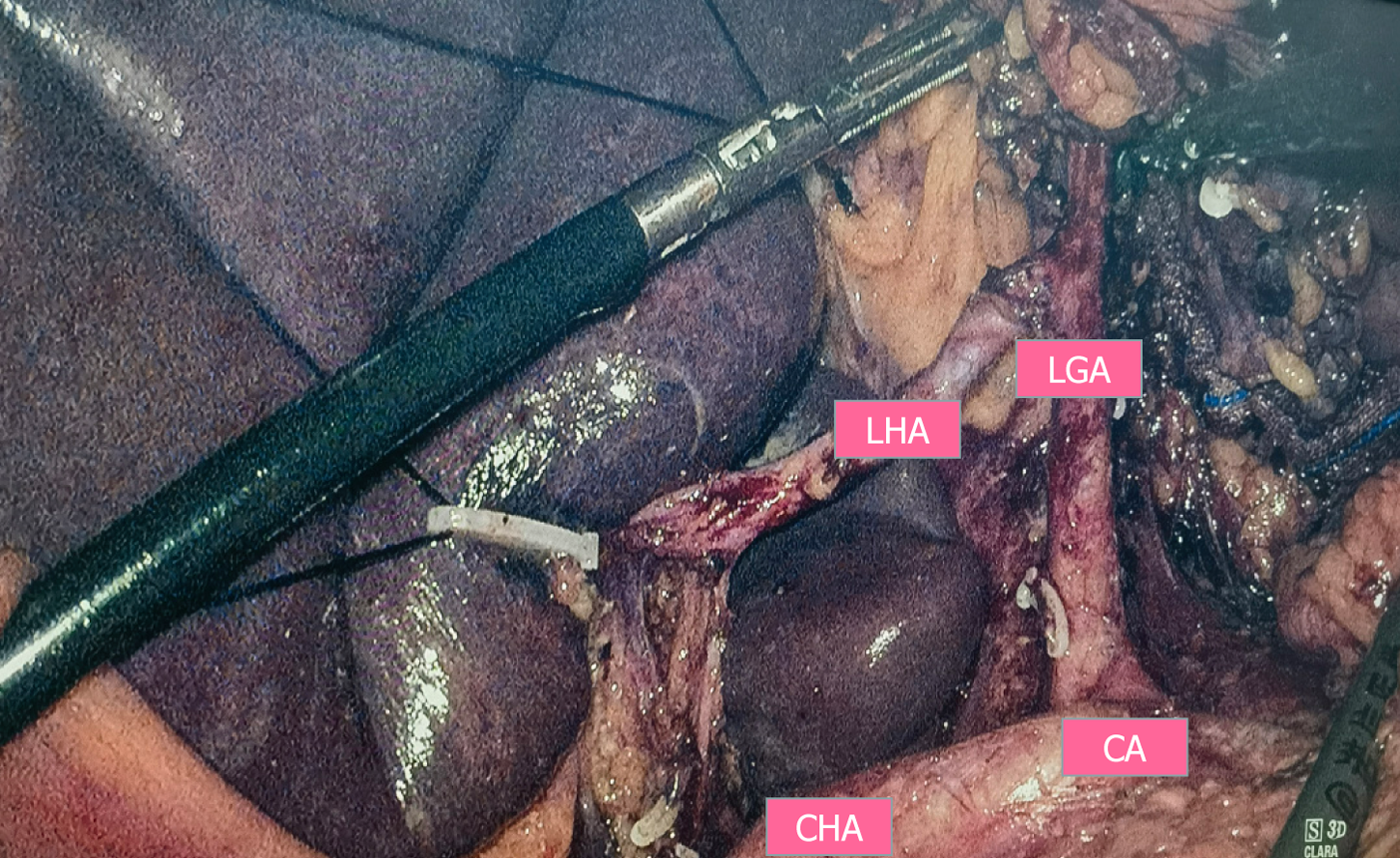
Intraoperative dissection confirmed the LHA originating from the LGA (Figure 3). The LGA was ligated proximally, preserving the variant LHA. Postoperative recovery was uncomplicated.
No hepatic dysfunction or recurrence observed during 5-year follow-up.
The liver is a common anatomical site in intraoperative surgery, and knowledge of the hepatic artery system and its vascular variants in particular, is crucial to avoid intraoperative injuries. Although most of the vascular variations have been documented in the literature and book descriptions, extremely rare cases can mostly be encountered only in clinical practice. Therefore, surgeons should document these vascular variants and analyze them in conjunction with preoperative examinations when appropriate, when dealing with hepatic vasculature, which can provide more detailed preoperative planning for patients[1].
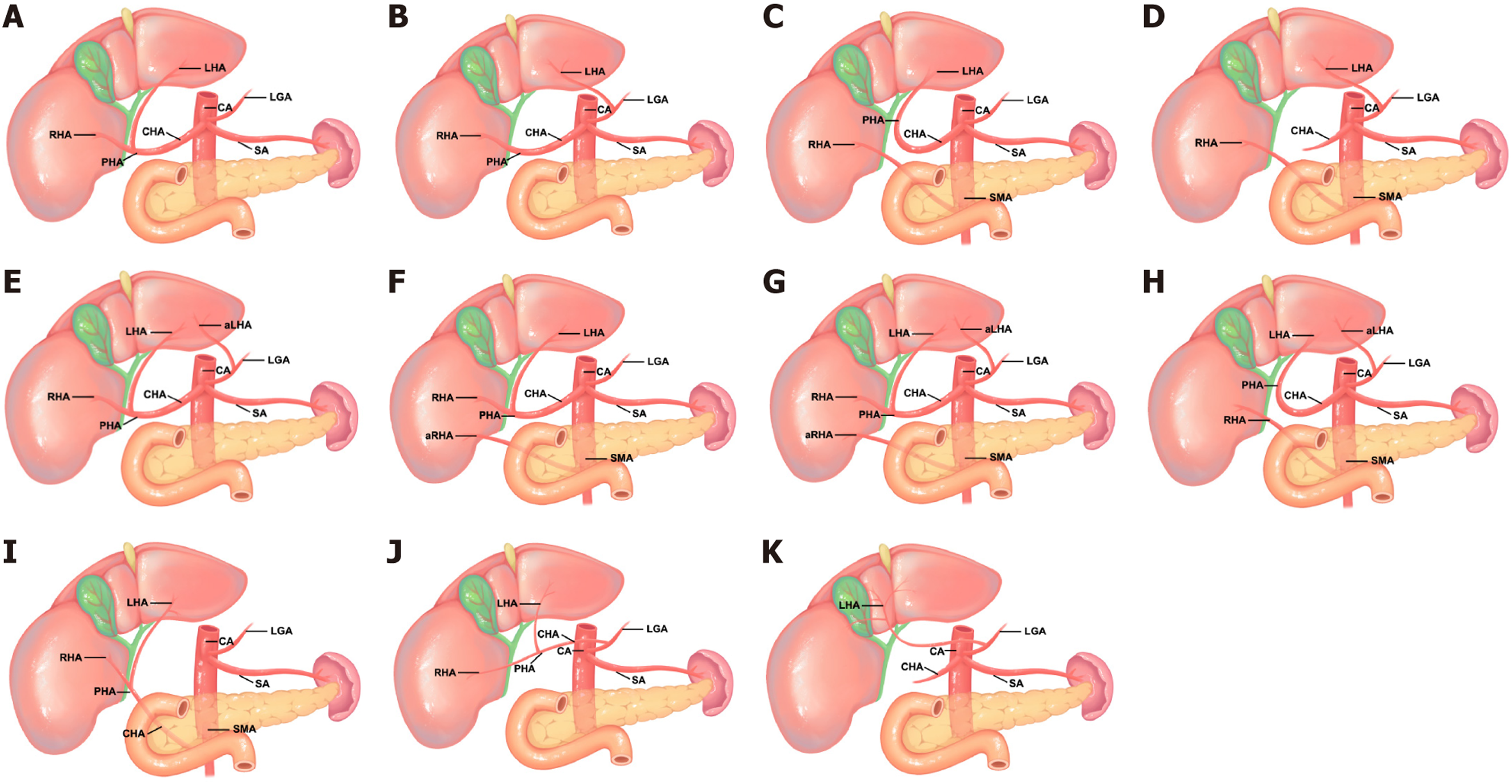
Knowledge of the distribution of the hepatic vascular system is essential for the surgeon and interventionalist, and its “standard” structure begins at the celiac trunk CT, which enters the splenic artery, the left gastric artery, and the common hepatic artery at the level of thoracic vertebrae 12. The common hepatic artery gives rise to three branches: The LHA, the proper hepatic artery, and the gastroduodenal artery. The proper hepatic artery bifurcates into the right and left hepatic arteries, which supply their respective lobes of the liver, whereas the right hepatic artery (RHA) supplies the gallbladder via the cystic artery[2]. The exact mechanism leading to the hepatic arterial vascular variant is currently unknown, with a high probability of originating from incomplete development of the ventral axis during embryonic development. The main cause is mostly considered to be incomplete development of the vasculature of the hepatic system and failure of vascular segregation, thus forcing the necessary circulation to come from non-normal origins[3,4]. Among the variants, the incidence of left hepatic artery originating from the LGA is 8%-12% (Michels type II), but complete substitution (no other hepatic artery branches) is rarer[5]. In contrast to the standard configuration of the hepatic circulation, most of the known variants of the hepatic vascular system to date have been categorized under Michels' classification system, which was established in 1955 and later expanded in 1966[5] (Table 1). Michels' original classification included 5 different types of variants, but subsequent studies have doubled it to at least 10 unique classifications[6] (Figure 3). Among these, the present patient belonged to Michels' classification type II and had no other hepatic artery branches, as shown in Figure 3K.
| Hepatic arterial anatomy | Michels’ class |
| Normal anatomy | Type I |
| LHA branching from LGA | Type II |
| RHA branching from SMA | Type III |
| LHA branching from LGA & RHA branching from SMA | Type IV |
| A LHA branching from LGA | Type V |
| A RHA branching from SMA | Type VI |
| A LHA branching from LGA and A RHA branching from SMA | Type VII |
| A LHA branching from LGA & RHA branching from SMA | Type VII |
| CHA branching from SMA | Type IX |
| CHA branching from LGA | Type X |
A LHA originating from the LGA is a critical anatomical variant. CT imaging currently excels in vascular visualization[7], and is routinely used for preoperative assessment, enabling the accurate and clear visualization of the anatomy of both the LHA and the RHA. Hepatic arterial variations in the porta hepatis increase the risk of impaired hepatic arterial blood supply. This may lead to unexpected bleeding or ischemia, as well as a higher incidence of biliary anastomotic leak, transient liver functional abnormalities, and potentially even liver failure[8]. Preoperative simulation facilitates individualized surgical planning[9], thereby minimizing complications through: Proactively dissecting the identified variant branch prior to surgery. Avoiding inadvertent transection of the LHA during the resection of the LGA[10].
This case describes a relatively rare hepatic circulatory system variant, predominantly a complete replacement type of left hepatic artery variant originating from the left gastric artery, demonstrating the significance of diagnosing and managing this rare vascular variant. In this article, a thorough diagnostic evaluation, including imaging analysis and intraoperative exploration, enabled accurate identification of the variant vessel, leading to successful radical surgical treatment. In addition, routine preoperative angiography, such as enhanced CT and CT angiography or arterial digital subtraction angiography, can usually identify variant hepatic arteries and their types, guiding intraoperative dissection. From another perspective, we can also observe the relationship between the variant hepatic vessels and the tumor, such as tumor invasion of an ectopic hepatic artery may affect the radical tumor resection and relate to the surgical decision. The variant hepatic artery may pass through the pancreas or even the tumor and cause postoperative hepatic insufficiency or even failure, especially in patients with obstructive jaundice.
The authors sincerely thank the patient for providing informed consent to publish this case report and accompanying medical images in an anonymized manner.
| 1. | Elsamaloty M, Schupp E, Ismail A, Borile C, Chun K, Sutton JM. A Rare Anatomic Variant of Double Replaced Hepatic Arteries: A Case Report and Brief Review of the Anomalous Hepatic Vasculature Literature. Am J Case Rep. 2021;22:e930990. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Abdelmaksoud MH, Louie JD, Kothary N, Hwang GL, Kuo WT, Hofmann LV, Hovsepian DM, Sze DY. Consolidation of hepatic arterial inflow by embolization of variant hepatic arteries in preparation for yttrium-90 radioembolization. J Vasc Interv Radiol. 2011;22:1364-1371.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Wang BG, Fröber R. Accessory extrahepatic arteries: Blood supply of a human liver by three arteries A case report with brief literature review. Ann Anat. 2009;191:477-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Gordon RD, Shaw BW Jr, Iwatsuki S, Todo S, Starzl TE. A simplified technique for revascularization of homografts of the liver with a variant right hepatic artery from the superior mesenteric artery. Surg Gynecol Obstet. 1985;160:474-476. [PubMed] |
| 5. | Michels NA. Newer anatomy of the liver and its variant blood supply and collateral circulation. Am J Surg. 1966;112:337-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 579] [Cited by in RCA: 560] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 6. | Covey AM, Brody LA, Maluccio MA, Getrajdman GI, Brown KT. Variant hepatic arterial anatomy revisited: digital subtraction angiography performed in 600 patients. Radiology. 2002;224:542-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 222] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 7. | Fang CH, Tao HS, Yang J, Fang ZS, Cai W, Liu J, Fan YF. Impact of three-dimensional reconstruction technique in the operation planning of centrally located hepatocellular carcinoma. J Am Coll Surg. 2015;220:28-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 72] [Article Influence: 6.5] [Reference Citation Analysis (1)] |
| 8. | Shukla PJ, Barreto SG, Kulkarni A, Nagarajan G, Fingerhut A. Vascular anomalies encountered during pancreatoduodenectomy: do they influence outcomes? Ann Surg Oncol. 2010;17:186-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 100] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 9. | Wu X, Kang J, Liu Y, Sun G, Shi Y, Niu J. A rare hepatic artery variant reporting and a new classification. Front Surg. 2022;9:1003350. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 10. | Huang CM, Chen RF, Chen QY, Wei J, Zheng CH, Li P, Xie JW, Wang JB, Lin JX, Lu J, Cao LL, Lin M. Application Value of a 6-Type Classification System for Common Hepatic Artery Absence During Laparoscopic Radical Resections for Gastric Cancer: A Large-Scale Single-Center Study. Medicine (Baltimore). 2015;94:e1280. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Coco D, Leanza S. Celiac Trunk and Hepatic Artery Variants in Pancreatic and Liver Resection Anatomy and Implications in Surgical Practice. Open Access Maced J Med Sci. 2019;7:2563-2568. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 12. | Imam A, Karatas C, Mecit N, Durur Karakaya A, Yildirimoglu T, Kalayoglu M, Kanmaz T. Anatomical variations of the hepatic artery: a closer view of rare unclassified variants. Folia Morphol (Warsz). 2022;81:359-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 13. | Swami A, Yadav T, Varshney VK, Sreesanth KS, Dixit SG. Hepatic Arterial Variations and Its Implication During Pancreatic Cancer Surgeries. J Gastrointest Cancer. 2021;52:462-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 14. | Choi TW, Chung JW, Kim HC, Lee M, Choi JW, Jae HJ, Hur S. Anatomic Variations of the Hepatic Artery in 5625 Patients. Radiol Cardiothorac Imaging. 2021;3:e210007. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 15. | Fonseca-Neto OCLD, Lima HCS, Rabelo P, Melo PSV, Amorim AG, Lacerda CM. ANATOMIC VARIATIONS OF HEPATIC ARTERY: A STUDY IN 479 LIVER TRANSPLANTATIONS. Arq Bras Cir Dig. 2017;30:35-37. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 16. | Yan Y, Wang B, Yuan W, Zhang J, Xiao J, Sha Y. A rare case with multiple arterial variations of the liver complicated laparoscopic pancreaticoduodenectomy. BMC Gastroenterol. 2022;22:331. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 17. | Vas D, Moreno Rojas J, Solà Garcia M. Replaced right hepatic artery arising from the distal renal artery, a new variation. Surg Radiol Anat. 2022;44:1339-1342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |