Published online Feb 27, 2024. doi: 10.4254/wjh.v16.i2.229
Peer-review started: October 5, 2023
First decision: October 28, 2023
Revised: November 18, 2023
Accepted: December 14, 2023
Article in press: December 14, 2023
Published online: February 27, 2024
Processing time: 145 Days and 10.5 Hours
Echinococcosis is prevalent in 9 provinces in Western and Northern China. An epidemiological survey of echinococcosis in 2012 and 2016 showed cases of echinococcosis in Yunnan Province.
To understand the spatial distribution and epidemiological characteristics of echinococcosis in Yunnan for the prevention and control of echinococcosis and to reduce the risk of infection in Yunnan Province.
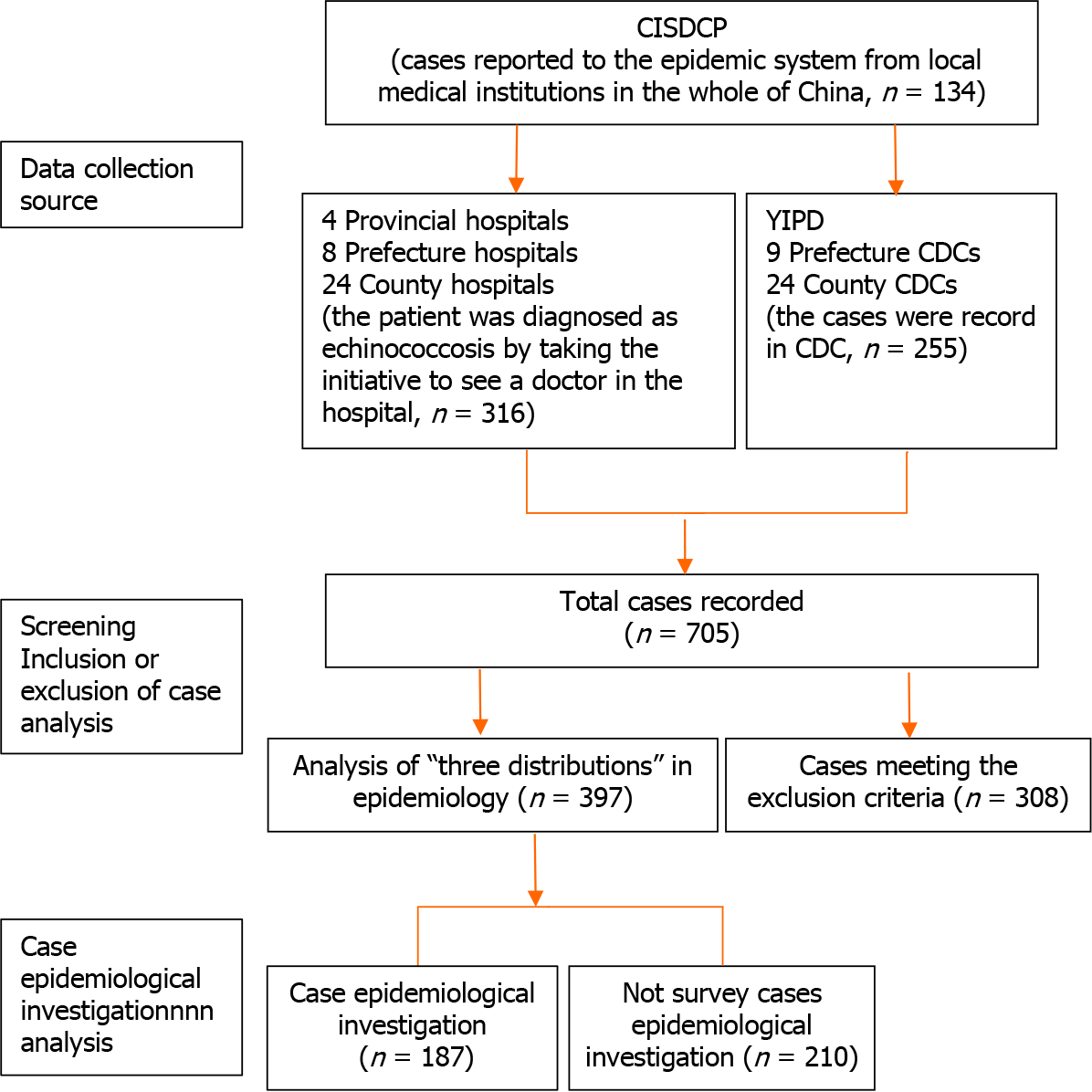
Based on the China Information System for Disease Control and Prevention (CISDCP), echinococcosis cases reported from 36 hospitals and 34 Centers for Disease Control were investigated and epidemiologically analyzed from 2021 to 2022. The exclusion criteria included suspected cases, same case only counted once and cases not from Yunnan. A total of 705 cases were investigated, of which 397 cases were suitable for statistical analysis. In these 397 cases, epidemiological investigation was tracked in 187 cases. All data were inputted using double entry in the Excel database, with error correction by double-entry comparison. The data on echinococcosis cases in Yunnan Province were analyzed by ArcGIS 10.1 software to generate a density map of echinococcosis distribution. All statistical analyses were conducted using SPSS 17.0, including the chi-square test, linear regression test and logistic univariate and multivariate regression analyses.
A total of 397 cases were found in 89 counties in Yunnan Province. The number of cases in the top three prefectures were Dali (38.1%), Diqing (10.1%), and Kunming (8.3%), and the top five counties were Jianchuan (9.1%), Shangri La (8.3%), Eryuan (7. 6%), Heqing (6.9%), and Dali Districts (5.0%). There were significant differences between the different areas. The case reporting rate by CISDCP (33.8%) was low; the first case was reported by CISDCP in 2002, and the highest number of cases was 50 (2017). Confirmed and clinical cases accounted for 62.5% and 37.5%, respectively. However, 90.9% of the cases of hydatid disease were reported by the hospital system, and only 9.1% of the cases of hydatid disease were found in the community through active screening. The difference between the two methods of case detection was statistically significant. Most of the cases of echinococcosis were found in farmers/herdsmen (75.1%) and students (9.1%). In addition, Han (43.6%) and Bai (26.2%) had a higher incidence of infection than other nationalities, and the liver (87.7%) and lung (6.8%) were the most common sites of cyst formation. Among the analyzed cases, 187 were epidemiologically analyzed and the clinical symptoms were not obvious in the early stage in 47.1% of cases. The results of logistic regression analysis showed that the age group, education level, presence of dogs in the family (either previously or currently), and handwashing (occasionally or not) were factors related to echinococcosis infection. 55.6% of cases were in endemic areas, and 44.4% of cases were in non-endemic areas. Among 83 cases in non-endemic areas, only 4 cases had been to endemic areas and had a history of living, working, travelling, or hunting in echinococcosis epidemic areas.
Cases of echinococcosis were reported throughout the entire Yunnan province, with the majority distributed in Western Yunnan, suggesting that echinococcosis control should be strengthened in this area. We suggest that an epidemiological investigation should be carried out in the future, based on the clues from newly discovered cases in hospitals or from the CISDCP. The newly discovered cases in the hospital provided clues to comprehensively determine the location of cases and where epidemic spot investigation should be conducted.
Core Tip: Seventy medical institutions, including 36 hospitals, 34 Centers for Disease Control (CDCs), and China Information System for Disease Control and Prevention, were surveyed from 2021 to 2022. The 36 hospitals included 4 provincial hospitals (the First and Second-People’s Hospital of Yunnan, and the First and Second Affiliated Hospitals of Kunming Medical University), 8 prefectural hospitals, and 24 county hospitals. The 34 CDCs included the Yunnan Institute of Parasitic Diseases, 9 prefectural CDCs, and 24 county CDCs. Information on echinococcosis cases from the ultrasound department, hepatobiliary surgery department, and case archives in the hospitals was retrospectively surveyed and recorded. The registration and management information on echinococcosis was consulted through the CDCs. The collected information on cases was organized and summarized before being entered into the database. Patient-privacy data were not included.
- Citation: Zi JR, Xiao D, Peng J, Wu FW, Li JX, Yan XL, Wang ZQ, Cai X, Xu Q, Li BF, Yang YM. Epidemiological survey of cystic echinococcosis in southwest China: From the Qinghai-Tibet plateau to the area of Yunnan. World J Hepatol 2024; 16(2): 229-240
- URL: https://www.wjgnet.com/1948-5182/full/v16/i2/229.htm
- DOI: https://dx.doi.org/10.4254/wjh.v16.i2.229
Cystic echinococcus (CE) is a zoonotic parasitic disease caused by the larval stage of the parasite Echinococcus granulosus (E. granulosus), it parasitizes humans or animals and is distributed globally[1-4]. Two main types of echinococcosis are observed in humans: CE and alveolar echinococcosis (AE). People in epidemic areas commonly become poor or return to poverty due to echinococcosis, which is a major burden on communities in endemic areas of China and poses an important public health problem[5-8]. China has the highest prevalence of echinococcosis in the world. According to the prevalence of echinococcosis in the population and the infection rate of echinococcosis in dogs, the endemic counties were divided into the following 4 categories: Class I counties: The prevalence rate of humans ≥ 1%, or the infection rate of dogs ≥ 5%; class II counties: 0.1% ≤ the human prevalence rate < 1%, or 1% ≤ the canine infection rate < 5%; class III counties: 0 <the prevalence rate of people < 0.1%, or 0 < dog infection rate < 1%; class IV counties: There have been reports of local cases of echinococcosis in the past, but no local cases have been found in 3 years, and other counties are non-endemic areas. There were 368 counties identified as endemic echinococcosis counties in China, the case detection rate was 0.51%. The prevalence was estimated to be 0.28% in the whole endemic area, and the number of patients was estimated to be 166098 with a distribution in 9 provinces/autonomous regions in Western and Northern China, including Xinjiang, Yunnan and Qinghai province[9,10]. Human echinococcosis was first reported in 1978 in Yunnan province. Liu et al[11] screened surgical patient data from the First and Second Affiliated Hospitals of Kunming Medical University and showed that there were 24 cases of hydatid disease in Yunnan Province from 1981 to 2001, with most cases distributed in Northwest Yunnan[12]. An epidemiological survey of echinococcosis in Yunnan Province in 2012 and 2016 showed that the detection rate of echinococcosis in the population was 0.06%, all of which had CE. This survey indicates that Yunnan Province is a low prevalence area of CE, mainly distributed in the northwest of 25° north latitude, including 24 counties of the 9 prefectures such as Diqing and Dali[13]. Understanding the epidemiological status, regional distribution, and epidemic characteristics of echinococcosis will assist with the provision of better control strategies and measures for echinococcosis in Yunnan Province. To fill these knowledge gaps, we aim to describe the demographic characteristics of people with echinococcosis in Yunnan Province, to map the prevalence of CE at high spatial resolution, and to assess the impact of risk factors.
Seventy medical institutions, including 36 hospitals, 34 Centers for Disease Control (CDCs), and the China Information System for Disease Control and Prevention (CISDCP), were surveyed from 2021 to 2022. The 36 hospitals included 4 provincial hospitals (the First and Second-People’s Hospital of Yunnan, and the First and Second Affiliated Hospitals of Kunming Medical University), 8 prefectural hospitals, and 24 county hospitals. The 34 CDCs included the Yunnan Institute of Parasitic Diseases, 9 prefectural CDCs, and 24 county CDCs. Information on echinococcosis cases from the ultrasound department, hepatobiliary surgery department, and case archives in the hospitals was retrospectively surveyed and recorded. The registration and management information on echinococcosis was consulted through the CDCs. The collected information on cases was organized and summarized before being entered into the database. Patient-privacy data were not included.
Diagnosed cases were defined as confirmed, clinical, and suspected according to the “Diagnostic Criteria for Echinococcosis” (WS257-2006). Suspected cases were defined as those who had visited an echinococcosis epidemic area and presented with clinical characteristics and space-occupying lesions; clinical cases were defined as those with characteristic imaging of echinococcosis (by ultrasonography, computed tomography scan, magnetic resonance imaging, chest-X ray, bronchoscopy, or radiology) and with blood samples positive for anti-echinococcus antibodies (diagnosed by enzyme-linked immunosorbent assay, indirect hemagglutination antibody test, or indirect fluorescent antibody test); and confirmed cases were defined as those with an echinococcosis cyst wall, protoscolices, or ascocyst found on pathological and etiological examination[14]. The information collected from these cases was used to set up the database. The included cases were confirmed and clinical cases from Yunnan. The exclusion of cases included suspected cases, cases with duplicate diagnoses, and when the same case of echinococcosis was only counted once. Additionally, cases that were not from Yunnan were also excluded.
Among the 397 cases, the complete epidemiological investigation was tracked in 187 cases and included epidemiologically related information such as past medical history, living history, exposure history, etc., to determine the epidemic characteristics of CE in Yunnan Province, and identify the source of the infection, in order to provide a scientific basis for CE prevention and control decisions. The 210 cases that could not be contacted or did not cooperate in the investigation were not included in the epidemiological investigation.
The survey included questions pertaining to basic information, clinical symptoms, epidemiological history, and personal behavior. Basic case information included name, sex, age group, ethnic group, occupation, education level, case category, parasite site, and network reports. The clinical symptoms included abdominal pain, cough, headache, and seizures. The questions relating to epidemiological history were as follows: “Have you travelled, worked, or stayed in echinococcosis endemic areas? (YTWSEA)”; “When did you visit the epidemic areas?”; “When you stayed in the echinococcosis epidemic area, did you contact or touch dogs?” and “Have you eaten half cooked or raw food?”. The questions relating to personal behavior were as follows: “Do you, or have you ever had dogs in your family? (YHDIYF)”; “Did your family use cow dung to burn? (YUCDB)”; “Do you wash your hands before preparing meals or eating? (YWHPME)” and “Have you drunk wild water? (HYDWW)”.
Therefore, we used negative binomial regression to analyze the factors influencing the prevalence of CE from the Qinghai-Tibet Plateau to Yunnan Province. The number of CE cases was set as the dependent variable.
Both univariate analysis and multiple collinearity tests were performed. The sex, age groups, ethnic group, occupation, education level, YTWSEA, YHDIYF, YUCDB, YWHPME and HYDWW, which may affect the development of echinococcosis, and these 10 factors were the independent variables. Spearman correlation analysis was used for preliminary exploration of the relationship between the prevalence of CE and the variables. Logistic single factor analysis showed the associations with echinococcosis, which were included in the multivariate analysis.
All data were inputted using double entry in the Excel database with error correction by double-entry comparison. All cases meeting the inclusion criteria were used for statistical analysis, but suspected cases were not used in the analysis of disease factors. All statistical analyses were conducted using SPSS 17.0 (IBM, New York, United States), and mapping was performed using ArcGIS 10.1 (ESRI, RedLands, United States). The data are expressed as frequency and percentage, and the comparison of rates between groups was tested using the chi-square test, linear regression tests and logistic regression analysis were performed. The significance level was set at P < 0.05.
A total of 705 cases from 70 survey sites, including hospitals, CDCs and CISDCP, were recorded in the previously mentioned electronic database (Figure 1). A total of 397 cases found in 89 counties in Yunnan Province met the inclusion criteria, of which only 187 cases were subjected to individual epidemiological investigation. According to diagnostic criteria, the confirmed and clinical cases accounted for 62.4% (248/397) and 37.5% (149/397), respectively. Moreover, CE accounted for 99.8% (396/397) and AE accounted for 0.3% (1/397) of the total cases. According to the infection site, hepatic echinococcosis accounted for 87.7% (348/397), lung echinococcosis accounted for 6.8% (27/397), renal echinococcosis accounted for 1.3% (5/397), abdominal echinococcosis accounted for 1.0% (4/397), splenic echinococcosis accounted for 0.5% (2/397), cerebral echinococcosis accounted for 0.50% (2/397), and other sites accounted for 2.3% (9/397). The difference between the parasitic sites was statistically significant (χ2 = 1051.170, P < 0.05). Furthermore, there were significantly more hospital diagnosed cases (90.93%, 361/397) than investigation detected cases (9.1%, 36/397) (χ2 = 298.870, P < 0.05). The incidence rates were 0.002, 0.01, 0.01, 0.03, 0.03, 0.04, 0.04, 0.04, 0.07, 0.06, 0.07, 0.1, 0.08, 0.09, 0.08 and 0.06 per 100000 from 2006 to 2021, respectively. The incidence rate of this disease has been maintained at a low level.
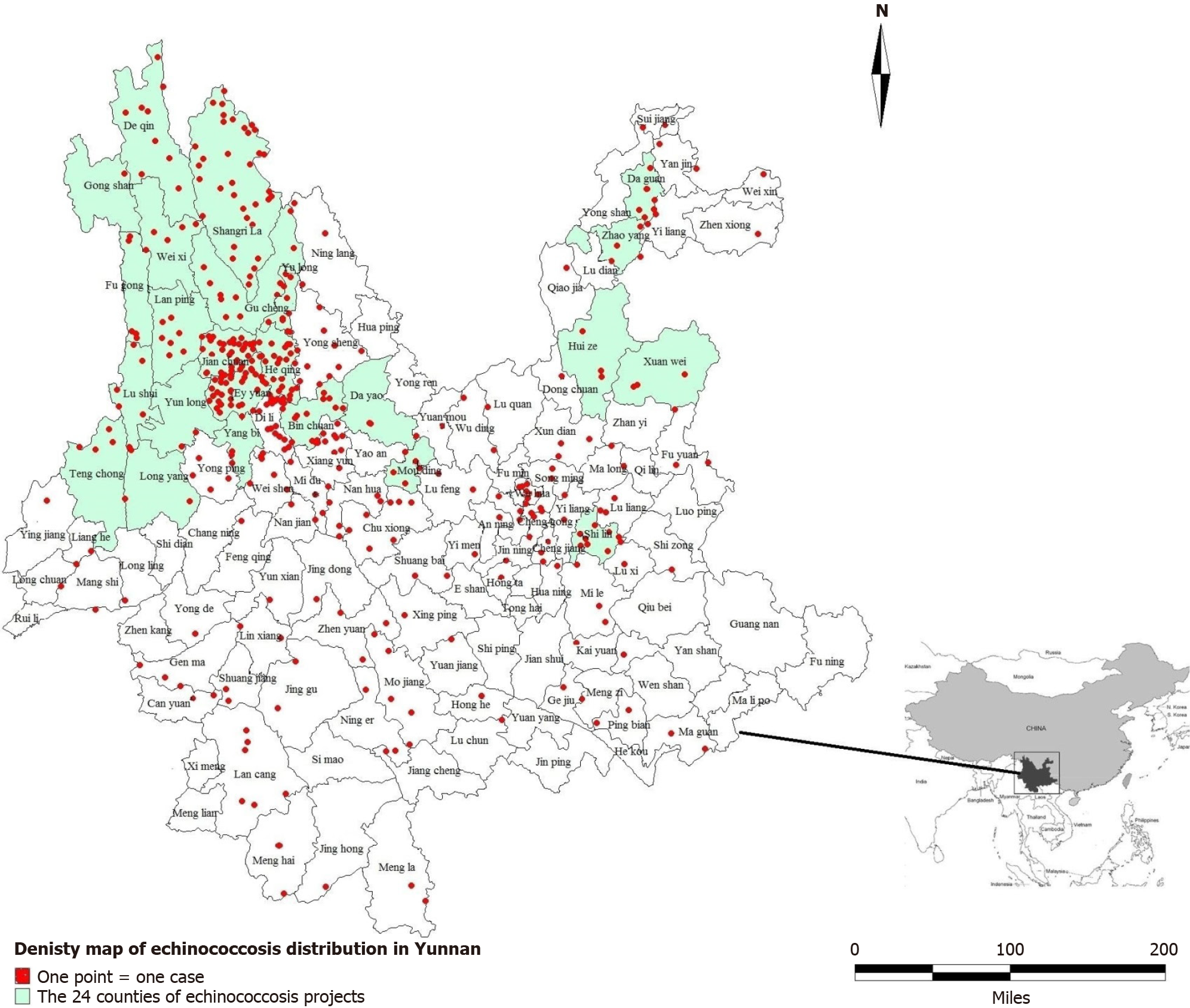
The data relating to the echinococcosis epidemic in Yunnan Province were used to generate a density map of echinococcosis distribution using ArcGIS 10.1 software (Figure 2). Echinococcosis was found in 89 of the 129 counties in the province, accounting for 68.99% of all counties. The density map showed that echinococcosis was mainly distributed in nine prefectures (cities) of Northwest Yunnan, including Diqing, Dali, Nujiang, Lijiang, Chuxiong, Baoshan, Zhaotong, and Kunming, while sporadic cases were found in other prefectures.
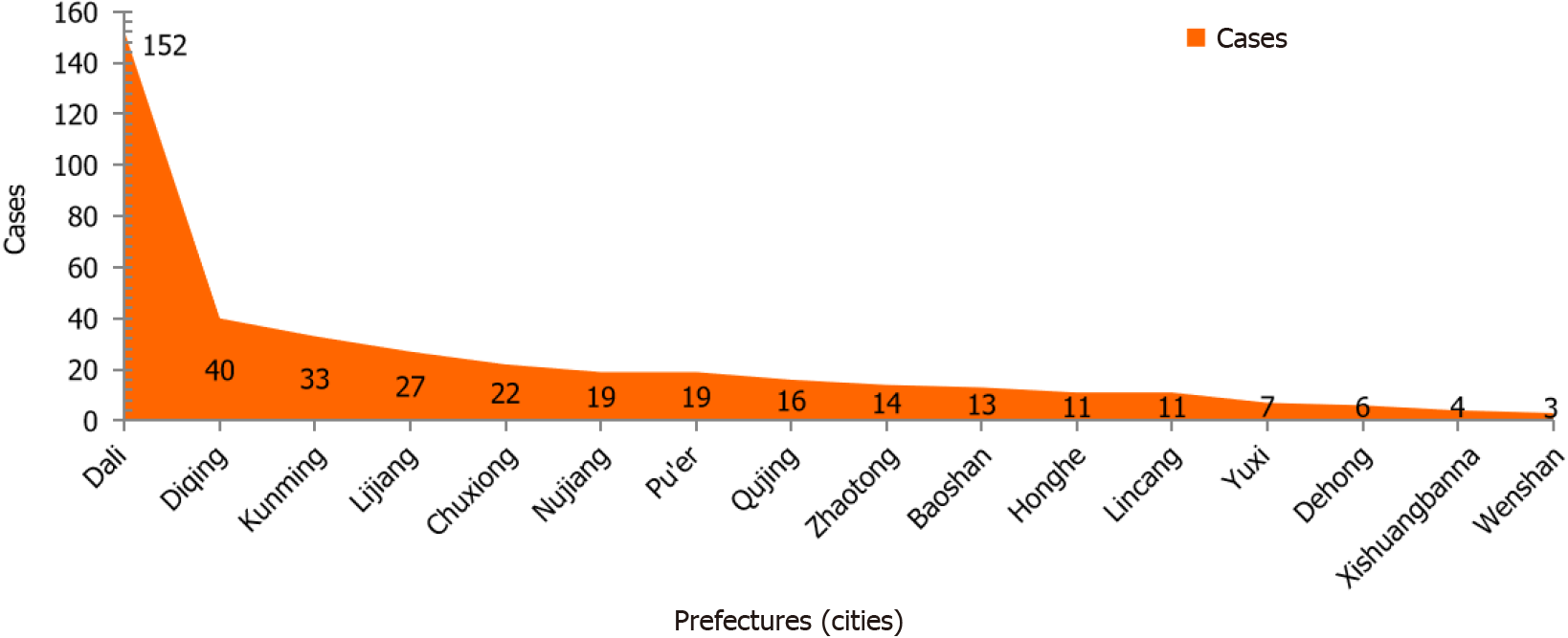
Cases of echinococcosis were found in 16 prefectures of the province (Figure 3), with the highest number of cases in Dali (38.3%, 152/397), followed by Diqing (10.1%, 40/397), while the lowest number of cases was in Wenshan (0.8%, 3/397). There were significant differences between the different areas (χ2 = 810.303, P< 0.05). By county, there were 3 counties with more than 30 cases, namely, Jianchuan County (9.1%, 36/397), Shangri-La city (8.3%, 33/397), and Eryuan County (7.7%, 30/397). Two counties had 20-29 cases, namely, Heqing County (6.6%, 26/397) and Dali City (5.0%, 20/397), while 2 counties had 10-19 cases, including Binchuan County (3.3%, 13/397) and Yongsheng County (2.5%, 10/397). The number of cases in the other 82 counties was < 10.
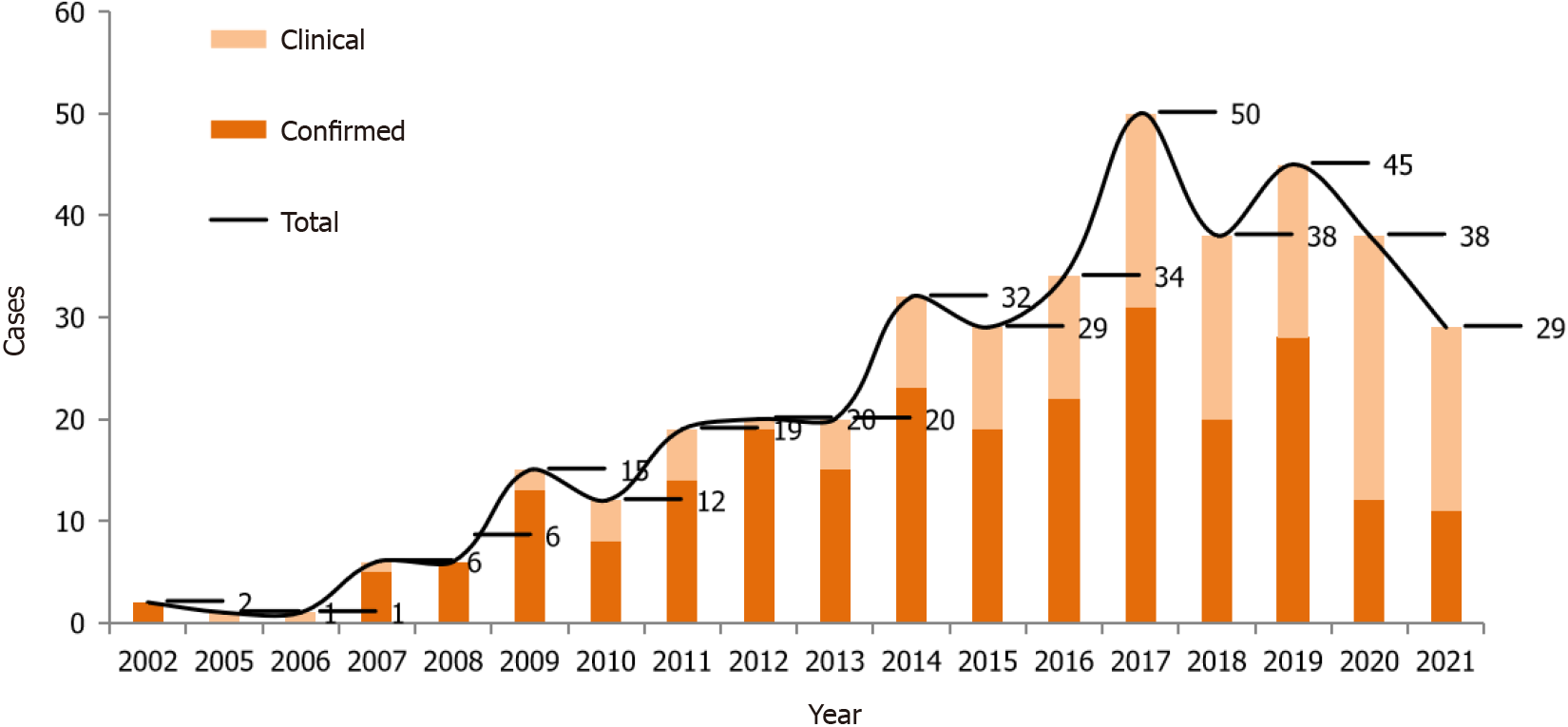
A total of 397 cases were found in Yunnan Province from 2002 to 2021 (Figure 4), of which the case reporting rate of CISDCP (33.8%, 134/397) was low; the first case was reported by CISDCP in 2002, and the highest number of reported cases was 50 (2017). With implementation of the echinococcosis prevention and control project in Yunnan Province, governments at all levels have increased efforts to conduct population echinococcosis screening, and the number of cases has increased annually.
The constituent echinococcosis ratios of male and female were 46.60% and 53.4%, respectively, and there was no significant difference between them (χ2 = 3.673, P > 0.05). Among all age groups, most cases were 40-49 years old, accounting for 18.4%, and there was a significant difference among different ages (χ2 = 118.105, P < 0.05). Most cases were Han (43.6%) and Bai (26.2%), with a significant difference among nationalities (χ2 = 667.763, P < 0.05). Among the occupation groups, echinococcosis was more common in farmers/herdsmen (75.1%) and students (9.1%), with a significant difference among occupations (χ2 =1645.711, P < 0.05) (Table 1).
| Features | Number of cases | Constituent ratio (%) |
| Sex | ||
| Male | 185 | 46.6 |
| Female | 212 | 53.4 |
| Age (yr) | ||
| 1-9 | 15 | 3.8 |
| 10-19 | 29 | 7.3 |
| 20-29 | 43 | 10.8 |
| 30-39 | 69 | 17.4 |
| 40-49 | 73 | 18.4 |
| 50-59 | 66 | 16.6 |
| 60-69 | 58 | 14.6 |
| 70-79 | 37 | 9.3 |
| ≥ 80 | 7 | 1.8 |
| Ethnicity | ||
| Han | 173 | 43.6 |
| Bai | 104 | 26.2 |
| Tibetan | 36 | 9.1 |
| Yi | 31 | 7.8 |
| Lisu | 11 | 2.8 |
| Naxi | 10 | 2.5 |
| Dai | 6 | 1.5 |
| Hani | 6 | 1.5 |
| Others | 20 | 5.0 |
| Occupation | ||
| Farmers and herders | 298 | 75.1 |
| Students | 36 | 9.1 |
| Cadre | 28 | 7.1 |
| Businessmen/individual | 10 | 2.5 |
| Children | 10 | 2.5 |
| Retired personnel | 5 | 1.3 |
| Guides | 4 | 1.0 |
| Others | 6 | 1.5 |
A total of 187 cases were epidemiologically investigated, including clinical symptoms, epidemiological history, and personal behavior of the cases. Investigation into clinical symptoms included the presence or absence of abdominal pain, cough, headache, and seizures. Symptoms were not obvious in the early stage in 47.1% (88/187). 31.6% (59/187) of cases had abdominal pain, 60.4% (113/187) of cases had no pain, and 8.0% (15/187) of cases were unclear. The cases with cough accounted for 11.8% (22/187), those with no cough accounted for 78.6% (147/187), and 9.63% (18/187) of cases were unclear. Cases with headache, none, and unclear accounted for 17.1% (32/187), 73.3% (137/187), and 9.6% (18/187), respectively. With regard to epilepsy, 1.6% (3/187) had epilepsy, 89.8% (168/187) did not, and 8.6% (16/187) were unknown. The results of the survey on the epidemiological history of cases showed that 13.9% (26/187) of cases had stayed, worked, travelled, or hunted in echinococcosis endemic areas, 78.6% (147/187) of cases had not been to endemic areas, and 7.5% (14/187) of cases did not know whether they had been to endemic areas. In terms of personal behavior, 74.9% (140/187) of cases stated that their household currently or previously had a dog, 20.9% (39/187) of cases did not have a dog, and 4.3% (8/187) had never had a dog. Among the cases, those who drank wild raw water, did not drink wild water, and those who could not remember whether they had drunk wild water accounted for 66.8% (125/187), 14.4% (28/187), and 18.2% (34/187), respectively. Among all cases, the proportions of frequent hand washing, occasional hand washing, and no hand washing before meals were 22.3% (42/187), 53.5% (100/187), and 24.1% (45/187), respectively.
Of the 187 cases, 26 had been to endemic areas and had a history of living, working, travelling, or hunting in epidemic areas of echinococcosis, 7.7% (2/26) of cases stayed perennially in an epidemic area, 15.4% (4/26) of cases visited an epidemic area 1 year previously, 3.9 (1/26) of cases visited an epidemic area 3 years previously, 7.7% (2/26) of cases visited an epidemic area 6 years previously, and 65.4% (17/26) of cases did not remember the time at which they visited an epidemic area. During their stay in an epidemic area of echinococcosis, 46.2% (12/26) of cases had contacted dogs, 11.5% (3/26) had not, and 43.3% (11/26) of cases were unclear. Moreover, 11.5% (3/26) of cases had eaten undercooked or raw food, 34.6% (9/26) of cases had not, and 53.9% (14/26) of cases did not remember. The cases that had drunk wild water, had not drunk wild water, and who were unclear as to whether they had drunk wild water accounted for 7.7 (2/26), 26.92% (7/26), and 65.4% (17/26), respectively. Of the 187 cases, 104 cases (55%) were in endemic areas and 83 cases (44.4%) were in non-endemic areas. Among 83 cases in non-endemic areas, 4 had been to endemic areas and had a history of living, working, travelling, or hunting in epidemic areas of echinococcosis. 79 cases lived in non-endemic areas.
Linear regression tests were performed on the following factors: Sex, age groups, ethnic group, occupation, education level, YTWSEA, YHDIYF, YUCDB, YWHPME and HYDWW, and the regression model showed statistical significance (F = 5.227, P < 0.05). The logistic analysis of the above 10 factors showed that the prevalence of human CE was positively correlated with age group, education level, YHDIYF and YWHPME (Table 2).
| Factors | Regression coefficient | Standard error | P value | Risk ratio (95%CI) |
| Sex | 0.627 | 0.402 | 0.119 | 1.872 (0.852-4.115) |
| Age group | 0.514 | 0.128 | 0.000 | 1.672 (1.301-2.149) |
| Ethnicity | 0.077 | 0.118 | 0.514 | 1.080 (0.857-1.361) |
| Occupation | -0.043 | 0.445 | 0.923 | 0.958 (0.400-2.292) |
| Education level | 0.637 | 0.281 | 0.023 | 1.891 (1.091-3.279) |
| YTWSEA | -0.008 | 0.081 | 0.926 | 0.992 (0.846-1.164) |
| YHDIYF | 1.040 | 0.228 | 0.000 | 2.830 (1.809-4.429) |
| YUCDB | -1.029 | 0.717 | 0.151 | 0.357 (0.088-1.457) |
| YWHPME | 0.630 | 0.269 | 0.019 | 1.877 (1.109-3.177) |
| HYDWW | -0.122 | 0.235 | 0.602 | 0.885 (0.559-1.402) |
Logistic analysis of single factors was conducted on 10 variables that may affect echinococcosis; these included sex, age, ethnicity, occupation, education level, YTWSEA, YHDIYF, YUCDB, YWHPME, and HYDWW. Among them, age, education level, YHDIYF, and YWHPME were significantly associated with echinococcosis (P < 0.05). Age as a risk factor was 1.672 (95%CI: 1.301-2.149) times greater than that of the other variables. Education level as a risk factor was 1.891 (95%CI: 1.091-3.279) times greater than that of the other variables, and the prevalence in the population with a low education level was higher than that in those with a high education level. YHDIYF as a risk factor was 2.830 (95%CI: 1.809-4.429) times greater than that of the other variables. YWHPME as a risk factor was 1.877 (95%CI: 1.109-3.177) times greater than that of the other variables (Table 2).
Logistic multiple factor analysis was conducted on age group, education level, YHDIYF and YWHPME which showed statistical significance in the single factor analysis. For age group, age from 20 to 29 years was 40.846 (95%CI: 3.855-432.769) times, 30 to 39 years was 40.846 (95%CI: 3.855-432.769) times, and 40 to 49 years was 8.302 (95%CI: 1.014-67.938) times that of the other variables. Where there was a dog in family, YHDIYF was 24.112 (95%CI: 2.347-247.666) times, and washing hands occasionally was 10.38 (95%CI: 3.464-31.101) times that of the other variables (Table 3).
| Factors | Regression coefficient | Standard error | P value | Risk ratio (95%CI) |
| Age group | ||||
| 1-9 | 19.167 | 0.000 | 2.11E+08 (2.11E + 08-2.11E + 08) | |
| 10-19 | 19.576 | 5647.366 | 0.997 | 3.18E + 08 (0-.b) |
| 20-29 | 3.534 | 1.298 | 0.006 | 34.26 (2.689-436.552) |
| 30-39 | 3.710 | 1.204 | 0.002 | 40.846 (3.855-432.769) |
| 40-49 | 2.116 | 1.073 | 0.048 | 8.302 (1.014-67.938) |
| 50-5 | 1.776 | 0.937 | 0.058 | 5.908 (0.941-37.081) |
| 60-69 | 0.976 | 0.892 | 0.274 | 2.654 (0.462-15.253) |
| 70-79 | 0.971 | 0.914 | 0.288 | 2.642 (0.441-15.834) |
| ≥ 80 | 0c | 0.000 | ||
| Education level | ||||
| Illiterate | 2.059 | 3.242 | 0.525 | 7.836 (0.014-4503.762) |
| Elementary school | 0.763 | 3.212 | 0.812 | 2.145 (0.004-1161.921) |
| Junior high school | 1.123 | 3.225 | 0.728 | 3.073 (0.006-1708.471) |
| High school | 2.636 | 3.676 | 0.473 | 13.953 (0.010-18788.338) |
| College and above | 0c | 0.00 | ||
| YHDIYF | ||||
| Yes | 3.183 | 1.188 | 0.007 | 24.112 (2.347-247.666) |
| No | -0.013 | 1.260 | 0.992 | 0.987 (0.084-11.661) |
| Previously | 2.066 | 1.247 | 0.098 | 7.894 (0.685-90.92) |
| Never | 0c | 0.000 | ||
| YWHPME | ||||
| Often | 1.176 | 0.636 | 0.064 | 3.241 (0.932-11.270) |
| Occasionally | 2.340 | 0.560 | 0.000 | 10.38 (3.464-31.101) |
| Not | 0c | 0.000 |
Echinococcosis is a chronic zoonotic parasitic disease caused by the larval stages of cestodes of the genus Echinococcus[3]. Four species of E. granulosus cause human infection, namely, CE, AE, polycystic echinococcosis (E. vogeli Rausch), and E. oligarthrus. Echinococcosis in humans presents predominantly as CE and AE types. E. vogeli Rausch and E. oligarthrus cause polycystic echinococcosis, but the incidence in humans is very rare[15]. Echinococcosis is globally distributed[4], and it is estimated that 91% of all AE cases worldwide occur in China[8]. Echinococcosis is endemic in China, mainly in the Western regions, including Inner Mongolia, Tibet, Gansu, Qinghai, Ningxia, and Xinjiang Production and Construction Corps, Sichuan, Yunnan, and Xi’an provinces[16,17].
The results of this survey demonstrated that sporadic cases of echinococcosis were reported throughout Yunnan Province, with a low prevalence, while most cases were distributed in 24 endemic counties in 9 prefectures, including Diqing and Dali in the Northwest. The prevalence of echinococcosis varied significantly in different areas. As there are many intermediate hosts suitable for echinococcus infection in Yunnan Province, the infection rate of animal hosts is high and there are natural foci with a potential risk of transmission and epidemics[13]. Yunnan Province closely neighbors Tibet and Sichuan provinces with a high prevalence of echinococcosis and is at risk of becoming an epidemic area[18-24]. According to the survey results, there was no significant difference in the constituent ratio of male and female; which may be related to the geographical characteristics of the combination of agricultural and pastoral areas, the mode of production in local residents, and their living habits in Yunnan. The first case of echinococcosis was reported by CISDCP in 2002, and screening has been strengthened since the implementation of the echinococcosis control project in 2012. As a result, the number of cases has increased annually, with the highest number of cases in 2017 (50), followed by 2019 (45) and then declined. The reduced number of cases in 2020 and 2021 was probably due to the coronavirus disease 2019 pandemic, and requires further investigation. According to the parasitic sites, hepatic (87.66%) and lung (6.80%) CE were the main types, which is in agreement with previous studies conducted in Yunnan[12,13]. The infection rate of pulmonary echinococcosis in Yunnan Province is as low as 6.8%. This may be related to geographical characteristics, echinococcosis species and ethnicity, which requires further research. Significantly more cases were diagnosed in hospital (90.93%) compared to those found by investigation (9.07%) (χ2 = 298.870, P < 0.05). This result shows that most cases were identified in hospital and few cases were found by active investigation or screening, likely due to the high cost of investigation and screening when the prevalence of echinococcosis in the population was reduced to a low level. Age group analysis showed that most cases were > 10 years old, with the highest proportion of cases aged 40-49 years. Logistic analysis showed that age was significantly associated with the prevalence of echinococcosis (P < 0.05). As echinococcosis is a chronic infectious disease with a long disease course, symptoms may occur more than 5 years after infection and patients may survive for many years after exposure. In line with this, the older age group may have been exposed to an environment contaminated by echinococcus eggs for an extended time, with the cumulative risk increasing with age[22]. Furthermore, most of the cases were Han (43.58%) and Bai (26.20%) nationalities. The constituent ratio of farmers/herdsmen (75.06%) and students (9.07%) was higher than that of other occupational groups, with significant differences among nationalities and occupations.
A total of 187 cases were investigated and basic information, including clinical symptoms, epidemiological history, and personal behavior, was collected. The survey results showed that the clinical symptoms in 47.1% of cases were not obvious in the early stage. Echinococcosis, is a chronic infectious disease with a long disease course, and the symptoms may occur 5-20 years after infection, leading to patients surviving for many years after exposure. The epidemiological history analysis showed that 78.61% of cases had not stayed, worked, travelled, or hunted in echinococcosis endemic areas, and that YTWSEA was not a risk factor for echinococcosis, indicating that there were local cases of infection in Yunnan Province. Regarding personal behavior, 74.87% (140/187) of households currently or previously had a dog. The proportions of occasional hand washing and no hand washing before meals were 53.48% and 24.06%, respectively, with the results of logistic analysis showing that the above two variables were factors influencing the prevalence of echinococcosis.
The prevalence of echinococcosis in Yunnan Province was low, and most of the cases were distributed in Northwest Yunnan. The prevention and control of echinococcosis should be strengthened in Diqing, Dali, and other areas in Northwest Yunnan. Based on the discovery of new cases, a case report is required by CISDCP within 24 h, and an epidemiological investigation of the individual cases should be conducted within 2 wk. According to the results, investigations should be conducted in the villages that are comprehensively judged as local infection sites within 2 mo. Together, this forms a comprehensive prevention and control strategy focused on the control of infectious sources, the prevention and control of intermediate hosts, and the combination of patient investigation, treatment, health education and publicity, and is referred to as the “1-2-2” prevention and control mode. Promoting changes in the behavior of the population, such as not raising dogs and washing hands frequently, through health education will serve to control endemic echinococcosis and reduce the medical burden on the population.
Ten cases of echinococcosis were in hospital in 1978, and surgical cases were 24 from 1981 to 2001 in Yunnan Province. An epidemiological survey of echinococcosis in 2012 and 2016 showed cases of echinococcosis in Yunnan Province. It is important to understand the spatial distribution and epidemiological characteristics of echinococcosis in Yunnan for the prevention and control of the disease.
To understand the species and sources of echinococcosis in Yunnan Province using a retrospective investigation and epidemiological analysis. Based on the local epidemic species of echinococcosis corresponding prevention and control measures can then be taken to effectively control the spread and prevalence of echinococcosis in Yunnan Province.
Cystic echinococcus is the main hydatid disease that has a medium prevalence. The aim of this study was to prevent and control echinococcosis and to reduce the risk of infection in Yunnan Province.
The cases were retrospectively epidemiologically investigated and analyzed in hospitals, Centers for Disease Control, and China Information System for Disease Control and Prevention.
A total of 397 cases were found in 89 counties in Yunnan Province, 55.6% of cases were in endemic areas, and 44.4% of cases were in non-endemic areas. The highest number of cases was 50 (2017). Confirmed and clinical cases accounted for 62.5% and 37.5%, respectively. However, 90.9% of the cases with hydatid disease were reported by the hospital system, and only 9.1% of the cases with hydatid disease were found in the community through active screening.
Cases of echinococcosis were reported throughout the entire Yunnan Province, with the majority distributed in Western Yunnan, suggesting that echinococcosis control should be strengthened in this area. Tracing hydatid disease cases, taking local infection cases as clues, and investigating local infection in villages were carried out, which effectively blocked the spread of hydatid disease.
Trace the source of cases, block the source of infection, and effectively control hydatid disease.
This survey was conducted by the Yunnan Institute of Parasitic Diseases and Tibet Centers for Disease Control and Prevention. We sincerely thank all the participants who were involved in this investigation, including the Centers for Disease Control (Institute/Station of Schistosomiasis Control) and related hospitals in Dali, Diqing, Kunming, Lijiang, Chuxiong, Nujiang, Zhaotong, Qujing, and Baoshan.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Amante MF, Argentina S-Editor: Qu XL L-Editor: Webster JR P-Editor: Yuan YY
| 1. | Xiao N, Yao JW, Ding W, Giraudoux P, Craig PS, Ito A. Priorities for research and control of cestode zoonoses in Asia. Infect Dis Poverty. 2013;2:16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 2. | Kirigia JM, Mburugu GN. The monetary value of human lives lost due to neglected tropical diseases in Africa. Infect Dis Poverty. 2017;6:165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 3. | McManus DP, Zhang W, Li J, Bartley PB. Echinococcosis. Lancet. 2003;362:1295-1304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 691] [Cited by in RCA: 717] [Article Influence: 32.6] [Reference Citation Analysis (0)] |
| 4. | Moro P, Schantz PM. Echinococcosis: a review. Int J Infect Dis. 2009;13:125-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 573] [Cited by in RCA: 678] [Article Influence: 42.4] [Reference Citation Analysis (0)] |
| 5. | Xue X, Wu WP. The factors of prevalent echinococcosis. Guoji Yixue Jishengchong Bing Zazhi. 2007;34:262-264. |
| 6. | Cadavid Restrepo AM, Yang YR, McManus DP, Gray DJ, Giraudoux P, Barnes TS, Williams GM, Soares Magalhães RJ, Hamm NA, Clements AC. The landscape epidemiology of echinococcoses. Infect Dis Poverty. 2016;5:13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 71] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 7. | Budke CM, Deplazes P, Torgerson PR. Global socioeconomic impact of cystic echinococcosis. Emerg Infect Dis. 2006;12:296-303. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 502] [Cited by in RCA: 591] [Article Influence: 31.1] [Reference Citation Analysis (0)] |
| 8. | Torgerson PR, Keller K, Magnotta M, Ragland N. The global burden of alveolar echinococcosis. PLoS Negl Trop Dis. 2010;4:e722. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 395] [Cited by in RCA: 364] [Article Influence: 24.3] [Reference Citation Analysis (0)] |
| 9. | Wu WP, Wang H, Wang Q, Zhou XN. A nationwide sampling survey on echinococcosis in China during 2012-2016. Chin J Parasitiol Parasit Dis. 2018;36:1-13. |
| 10. | Qi YF, Wu WP. Progress on Epidemiology of Eechinococcosis. Zhongguo Jishengchong Yu Jishengchongbing Zazhi. 2013;31:143-148. |
| 11. | Zhang BX, Zhang LL, Yang HM. Investigation of hydatid diseases in Yunnan province. Zhongguo Renshou Gonghuanbing Zazhi. 1997;13:66-67. |
| 12. | Pang YK. Analysis On Epidemic Status Of Echinococcosis In Yunnan Province. Zhonghua Jibing Kongzhi Zazhi. 2004;17:238-239. [DOI] [Full Text] |
| 13. | Yang YM, Wang LB, Wu FW, Yan XL, Ma XK, Du ZW. Survey of echinococcosis prevalence in area neighboring Tibet in Yunnan. Jibing Jiance. 2014;29:52-55. |
| 14. | Smego RA Jr, Bhatti S, Khaliq AA, Beg MA. Percutaneous aspiration-injection-reaspiration drainage plus albendazole or mebendazole for hepatic cystic echinococcosis: a meta-analysis. Clin Infect Dis. 2003;37:1073-1083. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 138] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 15. | Mandal S, Mandal MD. Human cystic echinococcosis: epidemiologic, zoonotic, clinical, diagnostic and therapeutic aspects. Asian Pac J Trop Med. 2012;5:253-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 112] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 16. | Zhang W, Zhang Z, Wu W, Shi B, Li J, Zhou X, Wen H, McManus DP. Epidemiology and control of echinococcosis in central Asia, with particular reference to the People's Republic of China. Acta Trop. 2015;141:235-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 153] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 17. | Wang Z, Wang X, Liu X. Echinococcosis in China, a review of the epidemiology of Echinococcus spp. Ecohealth. 2008;5:115-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 97] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 18. | Chai JJ. Echinococcosis control in China: challenges and research needs. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi. 2009;27:379-383. [PubMed] |
| 19. | Danzhen WJ, Xue CZ, Gongsang QZ, Ai JJ, Luo ZH, Danzeng QZ, Wei XG, Zheng CH. Analysis of echinococcosis prevalence in Nagqu Prefecture. Zhongguo Jishengchongxue Yu Jishengchongbing Zazhi. 2018;36:47-53. |
| 20. | Wang DM, He RF, Gongsang QZ, Xiao D, Suolang WJ, Xue L, Bianba ZM, Li JZ. Prevalence of echinococcosis in Nyingchi City. Zhongguo Jishengchongxue Yu Jishengchongbing Zazhi. 2018;36:75-79. |
| 21. | Gongsang QZ, Li B, Chen WQ, Song GA, Suolang WJ, Wang DM, Kangzhu YX, Li JZ. Pevalence of echinococcosis in Changdu City. Zhongguo Jishengchongxue Yu Jishengchongbing Zazhi. 2018;36:68-74. |
| 22. | Li B, Quzhen G, Xue CZ, Han S, Chen WQ, Yan XL, Li ZJ, Quick ML, Huang Y, Xiao N, Wang Y, Wang LY, Zuoga G, Ma BC, Wei XG, Zheng CJ, Wu WP, Zhou XN. Epidemiological survey of echinococcosis in Tibet Autonomous Region of China. Infect Dis Poverty. 2019;8:29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 42] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 23. | Sha L, Wang Q, Yang L, Yu WJ, He W, Zhang GJ, Huang Y. Analysis of Surveillance Results of Echinococcosis in Sichuan 2020. Yufang Yixue Qingbao Zazhi. 2021;37:1641-1647. |
| 24. | He W, Wang LY, Yu WJ, Zhang GJ, Zhong B, Liao S, Wang Q, Li RR, Yang L, Yao RX, Liu Y, Danba Z, Qin SC, Wang SA, Wang YX, Huang Y. Prevalence and spatial distribution patterns of human echinococcosis at the township level in Sichuan Province, China. Infect Dis Poverty. 2021;10:82. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |