Published online May 27, 2023. doi: 10.4254/wjh.v15.i5.641
Peer-review started: December 18, 2022
First decision: February 7, 2023
Revised: February 17, 2023
Accepted: April 6, 2023
Article in press: April 6, 2023
Published online: May 27, 2023
Processing time: 156 Days and 13.2 Hours
Non-alcoholic fatty liver disease (NAFLD) is a global problem. It may be caused by metabolic and hormonal disorders, including hypothyroidism. However, non-thyroid causes of NAFLD in people with hypothyroidism, including improper eating behavior and low physical activity, should be acknowledged. This study aimed to present the current literature on whether the development of NAFLD is related to hypothyroidism or a typical consequence of an unhealthy lifestyle in people with hypothyroidism. The results of previous studies do not allow for an unequivocal determination of the pathogenetic relationship between hypo
Core Tip: Non-alcoholic fatty liver disease affects 25% of the adult population worldwide; however, the causes of the disease remain unclear. This review answers the question of whether the development of non-alcoholic fatty liver disease is related to hypothyroidism or whether it is a typical consequence of an unhealthy lifestyle in people with hypothyroidism.
- Citation: Janota B, Szczepańska E, Adamek B, Janczewska E. Hypothyroidism and non-alcoholic fatty liver disease: A coincidence or a causal relationship? World J Hepatol 2023; 15(5): 641-648
- URL: https://www.wjgnet.com/1948-5182/full/v15/i5/641.htm
- DOI: https://dx.doi.org/10.4254/wjh.v15.i5.641
Global statistics indicate an increasing prevalence of non-alcoholic fatty liver disease (NAFLD) in society[1]. Currently, this disease affects approximately 25% of the adult population worldwide. It is often diagnosed in developed countries and is the second most common indication for liver transplantation[2].
The etiology of NAFLD is complex. NAFLD may be a result of excessive body weight, obesity, or carbohydrate and lipid metabolism disorders[3]. NAFLD is defined as a hepatic manifestation of metabolic syndrome[3,4]. The disorders mentioned are serious problems, which are related to improper eating habits and low physical activity, but may also have endocrine causes[5,6]. The most frequently described associations between NAFLD and endocrinopathies are polycystic ovary syndrome (PCOS) (PubMed: NAFLD PCOS - 93 publications in the last 5 years) and primary and secondary hypo
Considering the relationship between non-alcoholic fatty liver disease, lifestyle, and endocrine disorders, including thyroid dysfunction, it is important to determine whether the development of NAFLD is related to hypothyroidism as its result or a typical consequence of an improper lifestyle of people with hypothyroidism. This study presents considerations within this scope based on the current literature.
This literature review of the PubMed electronic database included 54 scientific articles over 5 years and 11 articles published between 2012 and 2016, including meta-analyses, cohort, and experimental studies. The following words were used to search for publications between October 2022 and February 2023: NAFLD and hypothyroidism = 86 publications, NAFLD and physical activity = 1009 publications, NAFLD and lifestyle = 1258 publications, NAFLD and Mediterranean diets = 172 publications, and lipid metabolism and thyroid = 693 publications. The last search was conducted in February 2023.
Hepatic lipid metabolism involves three substrate delivery mechanisms. The first is the absorption of fatty acids from chylomicrons formed during the absorption of lipids from food in the digestive system[14]. The second involves lipids stored in the adipocytes. Fatty acids supplied by food are stored as triglycerides in adipose tissue cells and in the liver. Triglyceride lipase affects the triglycerides in the adipose tissue, resulting in the release of fatty acids followed by their uptake by liver cells[14]. The third mechanism is de novo lipogenesis, in which hepatocytes absorb fatty acids due to the conversion of the consumed carbohydrates into fats[14].
Lipid metabolism in the liver can be classified into three transformations: oxidation of supplied fatty acids in the process of beta-oxidation, accumulation of fatty acids, or formation of protein complexes with fatty acid participation[14]. In NAFLD, fatty acid metabolism is disrupted. The accumulation of fatty compounds begins to increase, contrary to the synthesis and secretion of very-low-density lipoprotein (LDL) into the blood. De novo lipogenesis exceeds the efficiency of oxidation processes and the concentration of serum triglycerides of extrahepatic origin in the increases[14,15]. NAFLD is a progressive disease that begins with simple NAFLD, which may coexist with non-alcoholic steatohepatitis (NASH). NASH may be associated with fibrosis, leading to cirrhosis of the organ and the development of hepatocellular carcinoma[16].
Follicular thyroid cells produce and secrete thyroxine (T4) and triiodothyronine (T3) hormones. The control of their secretion depends on the concentrations of hormones of the hypothalamus (thyroliberin), and pituitary gland [tyrosine (TSH)]. The mechanism aimed at maintaining homeostasis is a negative feedback mechanism[17].
Thyroid hormones perform numerous functions, including metabolic control, maintenance of body temperature, regulation of hunger and satiety, and regulation of carbohydrate and lipid metabolism[18]. This is possible because of the localization of thyroid hormone receptors in the cells of many organs and tissues; for example, the liver (THR-beta), pancreas, adipose tissue (THR-alpha), and muscle tissue (THR-alpha)[18,19]. TSH receptors, which are located on thyroid cells, have also been located outside the thyroid gland in adipose tissue cells, hepatocytes, and ovaries[18,20].
Under the influence of thyroid hormones, the fat contained in adipocytes is broken down into free fatty acids, which are transported through the bloodstream to the hepatocytes by binding (1-L-fatty acid-binding protein and 36-CD36 fatty acid translocase) and transporting (fatty acid transport protein) proteins[19]. The function of these proteins is also regulated by thyroid hormones, which participate in de novo lipogenesis by enhancing gene expression, including the expression of Spot14[12,21]. Moreover, the activity of hepatic lipase, which breaks down fats into fatty acids, enabling their beta-oxidation, is dependent on the concentration of thyroid gland hormones[22].
Hypothyroidism is a disease in which the serum concentration of thyroid hormones is reduced[14,23]. This disease affects approximately 5% of the population[24]. Contributors of disease development include an insufficient supply of iodine, a component of thyroid hormones, or Hashimoto's disease. In the latter case, there is inflammatory lymphocytic infiltration and the production of antibodies against enzymes that enable the production of thyroid hormones, such as thyroid peroxidase and thyroglobulin[24]. Due to the formation of an insufficient amount of hormones, numerous disorders affecting the homeostasis of the body arise. The main common features of people with uncontrolled hypothyroidism are the occurrence of lipid disorders, increased blood cholesterol and triglyceride levels, and accumulation of fatty compounds in the liver[25,26]. Such disorders result from insufficient concentrations of thyroid hormones and excessive concentrations of TSH in the blood, which increase the production and secretion of T3 and T4 by the thyroid cells, according to the negative feedback effect. It should be noted that thyroxine supplementation significantly affects metabolism, causing an increase in the basic metabolic rate. This results in increased energy expenditure and, in the case of maintaining a negative caloric balance, may contribute to weight reduction[27].
In mouse models, elevated TSH levels in hypothyroidism have been observed to increase the expression of 3-hydroxy-3-methylglutaryl coenzyme A reductase in liver cells. This results in changes in cholesterol synthesis, which may lead to the accumulation of fatty compounds in the liver[28,29].
The regulation of lipid concentration in the body also occurs at a genetic level through transcription factors, including sterol regulatory element-binding protein (SREBP) and liver X receptor (LXR)[30,31]. LXR has also been detected in the liver, and is both a thyroid hormone receptor and a nuclear receptor. SREBP controls lipid synthesis, which is significantly influenced by thyroid hormone levels. The effect of the action of thyroid hormones on SREBP-2, an isoform of SREBP, is a decrease in the expression of the LDL receptor, which manifests as an increase in serum cholesterol levels. In cases of thyroid hormone deficiency, this situation is reversed[30].
In both overt and subclinical hypothyroidism, there is an increase in the concentration of angiopoietin-like proteins Angptl-3 and Angptl-8, which participate in lipid metabolism and inhibit the action of lipoprotein lipase. The weakened function of lipoprotein lipase can lead to fat accumulation in the liver and decrease LDL cholesterol breakdown. The results of studies on the occurrence of increased concentrations of Angplt3 and 8 are clear, and scientists suggest using these proteins in the detection of hypothyroidism, although high concentrations have also been observed in obesity and diabetes[32,33].
Fibroblast growth factor FGF-21, which is still under study, enhances the beta-oxidation of fatty acids in the liver (where it is produced) while slowing down the formation of triglycerides. In acute hypothyroidism caused by radioiodine treatment, there is an increase in FGF-21 concentration, which ultimately predisposes patients to hepatic steatosis by enhancing lipogenesis[34].
The control of hepatocyte autophagy is another function that involves thyroid hormones[35]. In autophagy within liver cells, NCoR1, a co-repressor of nuclear receptor 1 under typical conditions, is degraded. In hypothyroidism, beta-oxidation is reduced by affecting peroxisome proliferator-activated alpha receptor, resulting in an increase in de novo lipogenesis[36].
The influence of thyroid hormones on lipid metabolism and liver function is a topic widely described in the scientific literature, and control mechanisms include multilevel interactions at molecular and cellular levels[37]. These relationships are still being researched, proving the importance of the subject[38,39].
The relationship between NAFLD and hypothyroidism has been the subject of population studies in several countries. These results are sometimes contradictory, although most indicate the existence of a relationship[40]. In a cohort study involving 81166 German residents, a strong relationship between the diseases was found[41]. In contrast, no associations were found in a study involving 10116 Spanish residents, similar to the results of a retrospective study conducted among 18544 Korean residents[42,43]. Therefore, it is important to consider the non-thyroid causes of NAFLD in patients with hypothyroidism. Possible associations were studied by Mansour-Ghanaei et al[44], who examined 333 Iranian patients with diabetes, lipid disorders, obesity, and PCOS. Participants who had additional NAFLD were also diagnosed with hypothyroidism significantly more often; had significantly higher body mass index (BMI) values; smoked cigarettes more frequently; had considerably higher concentrations of total cholesterol, glucose, uric acid, and abnormal eating habits, which are important due to the unquestionable adverse effects on the body[44].
Due to the association between NAFLD and numerous metabolic disorders resulting from an improper lifestyle habits, metabolic dysfunction - associated fatty liver disease (MAFLD) has been distinguished as concurrent liver dysfunction and metabolic syndrome[45]. In turn, metabolic syndrome often accompanies hypothyroidism[46]. Biochemical and elastography screening tests are important for detecting the presence of metabolic disorders and MAFLD in people with hypothyroidism[47].
A significant risk factor for NAFLD is improper eating behavior, resulting in an excessive supply of energy in the diet, excessive consumption of monosaccharides (especially fructose), and saturated fats[38]. The diet of patients diagnosed with NAFLD should primarily limit the supply of monosaccharides because they intensify de novo lipogenesis[48]. Their consumption should also be limited because of the prevalence of insulin resistance in people with NAFLD, which is also observed in people with hypothyroidism[49]. Thyroid hormones affect glucose metabolism in the liver by activating glucose transporter 2, resulting in the release of glucose into the bloodstream[50]. The above mechanism is disrupted by thyroid hormone deficiency[50]. Insulin resistance, an imbalance in the proportion of serum insulin and glucose concentrations, activates SREBP-1c, resulting in the intensification of de novo lipogenesis, leading to fatty liver[51]. The Mediterranean diet, rich in vegetables, polyunsaturated fatty acids, and vitamin E, may be the recommended nutritional model for both hypothyroidism and NAFLD because of its proven anti-inflammatory effect and low glycemic index, which are important in the case of insulin resistance[52-56].
Excessive body weight caused by an increased amount of adipose tissue is an abnormality that may contribute to the development of obesity - a serious disease in which metabolic disorders (including lipid disorders) are associated with endocrine disorders and have a negative impact on all areas of a patient's life[55,56]. Scientists have emphasized that excessive body weight and obesity predict a worse course of NAFLD[57,58]. Obesity is also associated with hypothyroidism, as proven in a cohort study of 9,011 Chinese residents. In addition, researchers proved that obesity in younger men was an independent risk factor for hypothyroidism, while in older men, metabolic disorders were a significant factor in its pathogenesis[56]. There is equivocal evidence of a high correlation between BMI and TSH concentration[59,60]. Such conclusions were reached by Amin et al[59], who examined the effect of weight reduction on thyroid function and NAFLD in obese Egyptian adolescents during an intervention. It has been calculated that for an increase in TSH of 10 mIU/L, the BMI increases by 5.28 kg/m2[59]. Decreased body weight, TSH concentration, and percentage of people with fatty liver have been observed after lifestyle modifications, including altered physical activity and eating habits among adolescents[59]. Du et al[60] who studied the effect of thyroid hormones on central obesity, showed a positive correlation between the central obesity index (waist-hip Ratio, WHR), level of TSH, and BMI. The results of this study indicate the association between thyroid hormones and body weight and body fat distribution, which is due to the hypometabolic state caused by a thyroid hormone deficiency[60]. Researchers have suggested that hepatic steatosis may have a negative impact on thyroid function rather than hypothyroidism, which has a negative impact on liver function[61].
According to studies on the impact of lifestyle on the development of NAFLD[62]. The positive effect of physical activity is manifested by body weight reduction and increased insulin sensitivity in cells[55,63]. Additionally, physical activity prevents muscle mass reduction, which is a risk factor for NAFLD[60]. Increasing the level of physical activity is also recommended for people without excessive body weight but with NAFLD, in whom the researchers believed the cause of the disease to be an elevated TSH concentration[63,64]. Moreover, in a Chinese population study, which included 5,154 people, hypothyroidism was significantly more common in people who did not undertake physical activity than in euthyroid people[65].
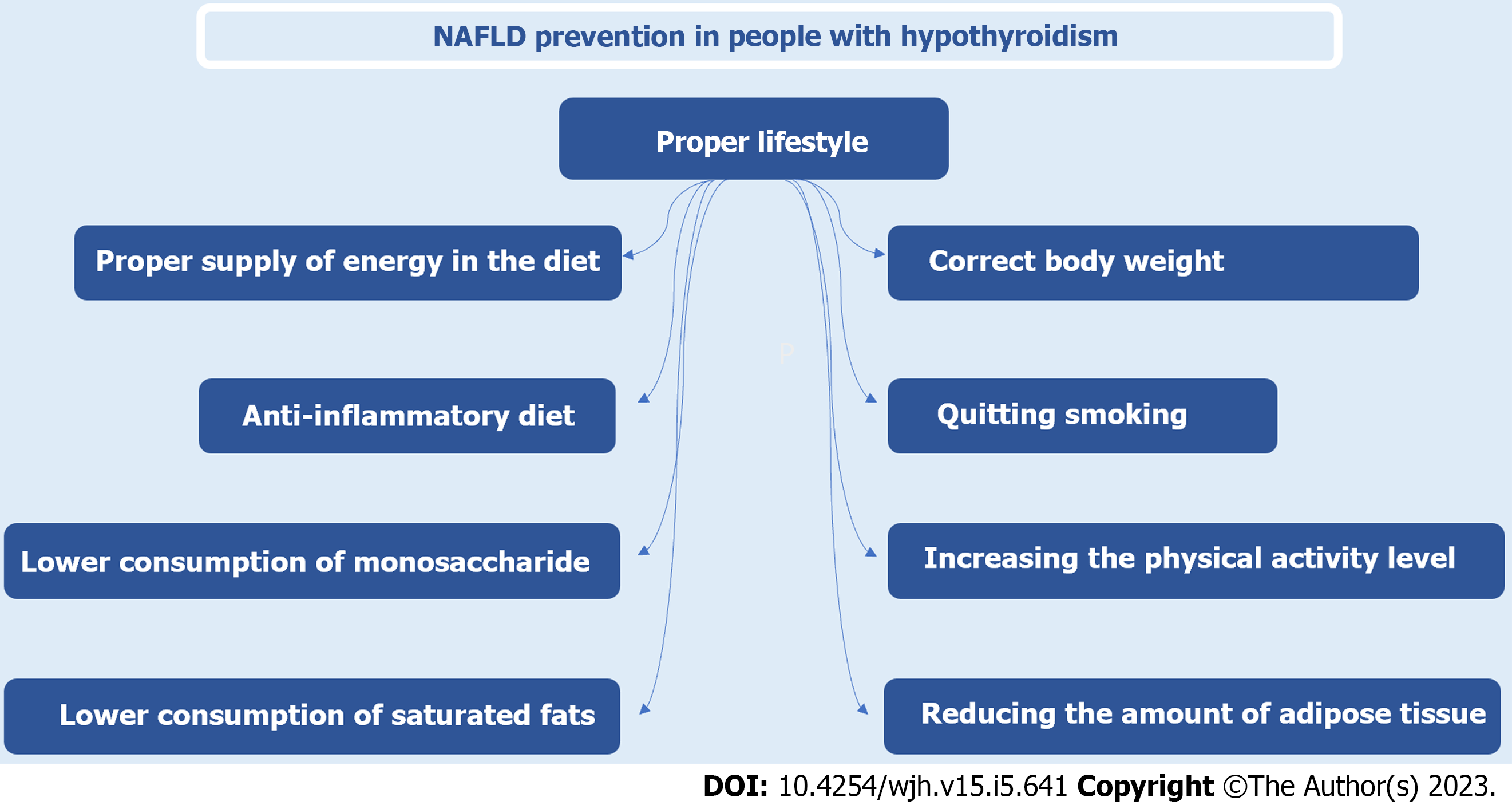
A summary of the above information about importance of proper lifestyle in people with hypothyroidism is presented in Figure 1.
Hypothyroidism and NAFLD coexist, although their interdependence is not a cause-and-effect relationship.
The pathomechanism of excessive fat accumulation in the liver is complex, and its important non-thyroid-initiating factors are as follows: (1) Providing too many calories in relation to requirements; (2) consuming excessive amounts of monosaccharides and saturated fats; (3) being overweight; and (4) keeping a low physical activity level.
The results of the previous studies do not allow for an unequivocal determination of the pathogenetic relationship between hypothyroidism and NAFLD.
Further research is necessary to answer the questions posed in the title. Among the patients with coexisting NAFLD and hypothyroidism, environmental factors and those dependent on human choice are more important.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Endocrinology and metabolism
Country/Territory of origin: Poland
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Jamali R, Iran; Shalaby MN, Egypt S-Editor: Wang JL L-Editor: A P-Editor: Cai YX
| 1. | Lazarus JV, Mark HE, Anstee QM, Arab JP, Batterham RL, Castera L, Cortez-Pinto H, Crespo J, Cusi K, Dirac MA, Francque S, George J, Hagström H, Huang TT, Ismail MH, Kautz A, Sarin SK, Loomba R, Miller V, Newsome PN, Ninburg M, Ocama P, Ratziu V, Rinella M, Romero D, Romero-Gómez M, Schattenberg JM, Tsochatzis EA, Valenti L, Wong VW, Yilmaz Y, Younossi ZM, Zelber-Sagi S; NAFLD Consensus Consortium. Advancing the global public health agenda for NAFLD: a consensus statement. Nat Rev Gastroenterol Hepatol. 2022;19:60-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 469] [Cited by in RCA: 455] [Article Influence: 151.7] [Reference Citation Analysis (0)] |
| 2. | Tokushige K, Ikejima K, Ono M, Eguchi Y, Kamada Y, Itoh Y, Akuta N, Yoneda M, Iwasa M, Otsuka M, Tamaki N, Kogiso T, Miwa H, Chayama K, Enomoto N, Shimosegawa T, Takehara T, Koike K. Evidence-based clinical practice guidelines for nonalcoholic fatty liver disease/nonalcoholic steatohepatitis 2020. J Gastroenterol. 2021;56:951-963. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 183] [Cited by in RCA: 178] [Article Influence: 44.5] [Reference Citation Analysis (0)] |
| 3. | Dietrich CG, Rau M, Geier A. Screening for nonalcoholic fatty liver disease-when, who and how? World J Gastroenterol. 2021;27:5803-5821. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 10] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (2)] |
| 4. | Kasper P, Martin A, Lang S, Kütting F, Goeser T, Demir M, Steffen HM. NAFLD and cardiovascular diseases: a clinical review. Clin Res Cardiol. 2021;110:921-937. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 103] [Cited by in RCA: 385] [Article Influence: 77.0] [Reference Citation Analysis (1)] |
| 5. | Saklayen MG. The Global Epidemic of the Metabolic Syndrome. Curr Hypertens Rep. 2018;20:12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1964] [Cited by in RCA: 2420] [Article Influence: 345.7] [Reference Citation Analysis (0)] |
| 6. | Lonardo A, Mantovani A, Lugari S, Targher G. NAFLD in Some Common Endocrine Diseases: Prevalence, Pathophysiology, and Principles of Diagnosis and Management. Int J Mol Sci. 2019;20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 85] [Cited by in RCA: 86] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 7. | Gariani K, Jornayvaz FR. Pathophysiology of NASH in endocrine diseases. Endocr Connect. 2021;10:R52-R65. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 55] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 8. | Tanase DM, Gosav EM, Neculae E, Costea CF, Ciocoiu M, Hurjui LL, Tarniceriu CC, Floria M. Hypothyroidism-Induced Nonalcoholic Fatty Liver Disease (HIN): Mechanisms and Emerging Therapeutic Options. Int J Mol Sci. 2020;21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 42] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 9. | Bikeyeva V, Abdullah A, Radivojevic A, Abu Jad AA, Ravanavena A, Ravindra C, Igweonu-Nwakile EO, Ali S, Paul S, Yakkali S, Teresa Selvin S, Thomas S, Hamid P. Nonalcoholic Fatty Liver Disease and Hypothyroidism: What You Need to Know. Cureus. 2022;14:e28052. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (1)] |
| 10. | Von-Hafe M, Borges-Canha M, Vale C, Leite AR, Sérgio Neves J, Carvalho D, Leite-Moreira A. Nonalcoholic Fatty Liver Disease and Endocrine Axes-A Scoping Review. Metabolites. 2022;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 11. | Yang EJ, Choi BS, Yang YJ. Risk of Nonalcoholic Fatty Liver Disease Is Associated with Urinary Phthalate Metabolites Levels in Adults with Subclinical Hypothyroidism: Korean National Environmental Health Survey (KoNEHS) 2012-2014. Int J Environ Res Public Health. 2022;19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 12. | Lugari S, Mantovani A, Nascimbeni F, Lonardo A. Hypothyroidism and nonalcoholic fatty liver disease - a chance association? Horm Mol Biol Clin Investig. 2018;41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 13. | Gor R, Siddiqui NA, Wijeratne Fernando R, Sreekantan Nair A, Illango J, Malik M, Hamid P. Unraveling the Role of Hypothyroidism in Non-alcoholic Fatty Liver Disease Pathogenesis: Correlations, Conflicts, and the Current Stand. Cureus. 2021;13:e14858. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Mato JM, Alonso C, Noureddin M, Lu SC. Biomarkers and subtypes of deranged lipid metabolism in non-alcoholic fatty liver disease. World J Gastroenterol. 2019;25:3009-3020. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 92] [Cited by in RCA: 142] [Article Influence: 23.7] [Reference Citation Analysis (4)] |
| 15. | Ipsen DH, Lykkesfeldt J, Tveden-Nyborg P. Molecular mechanisms of hepatic lipid accumulation in non-alcoholic fatty liver disease. Cell Mol Life Sci. 2018;75:3313-3327. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 795] [Cited by in RCA: 980] [Article Influence: 140.0] [Reference Citation Analysis (1)] |
| 16. | Nabrdalik K, Pokrzywnicka P, Nabrdalik-Leśniak D, Gumprecht J, Kwiendacz H. Amelioration of liver enzyme abnormalities and improvement in glucose control with pioglitazone in a patient with diabetes mellitus type 2 and nonalcoholic fatty liver disease. Clin Diabetol. 2016;5:199-202. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 17. | Wang JJ, Zhuang ZH, Shao CL, Yu CQ, Wang WY, Zhang K, Meng XB, Gao J, Tian J, Zheng JL, Huang T, Tang YD. Assessment of causal association between thyroid function and lipid metabolism: a Mendelian randomization study. Chin Med J (Engl). 2021;134:1064-1069. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 18. | Walczak K, Sieminska L. Obesity and Thyroid Axis. Int J Environ Res Public Health. 2021;18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 87] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 19. | Sinha RA, Singh BK, Yen PM. Direct effects of thyroid hormones on hepatic lipid metabolism. Nat Rev Endocrinol. 2018;14:259-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 463] [Cited by in RCA: 418] [Article Influence: 59.7] [Reference Citation Analysis (0)] |
| 20. | Martínez-Escudé A, Pera G, Costa-Garrido A, Rodríguez L, Arteaga I, Expósito-Martínez C, Torán-Monserrat P, Caballería L. TSH Levels as an Independent Risk Factor for NAFLD and Liver Fibrosis in the General Population. J Clin Med. 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 21. | Rudolph MC, Wellberg EA, Lewis AS, Terrell KL, Merz AL, Maluf NK, Serkova NJ, Anderson SM. Thyroid hormone responsive protein Spot14 enhances catalysis of fatty acid synthase in lactating mammary epithelium. J Lipid Res. 2014;55:1052-1065. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 36] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 22. | Brenta G, Berg G, Miksztowicz V, Lopez G, Lucero D, Faingold C, Murakami M, Machima T, Nakajima K, Schreier L. Atherogenic Lipoproteins in Subclinical Hypothyroidism and Their Relationship with Hepatic Lipase Activity: Response to Replacement Treatment with Levothyroxine. Thyroid. 2016;26:365-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 23. | Wilson SA, Stem LA, Bruehlman RD. Hypothyroidism: Diagnosis and Treatment. Am Fam Physician. 2021;103:605-613. [PubMed] |
| 24. | Chiovato L, Magri F, Carlé A. Hypothyroidism in Context: Where We've Been and Where We're Going. Adv Ther. 2019;36:47-58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 198] [Article Influence: 33.0] [Reference Citation Analysis (0)] |
| 25. | Liu H, Peng D. Update on dyslipidemia in hypothyroidism: the mechanism of dyslipidemia in hypothyroidism. Endocr Connect. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 39] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 26. | Yan F, Wang Q, Lu M, Chen W, Song Y, Jing F, Guan Y, Wang L, Lin Y, Bo T, Zhang J, Wang T, Xin W, Yu C, Guan Q, Zhou X, Gao L, Xu C, Zhao J. Thyrotropin increases hepatic triglyceride content through upregulation of SREBP-1c activity. J Hepatol. 2014;61:1358-1364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 111] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 27. | Johannsen DL, Galgani JE, Johannsen NM, Zhang Z, Covington JD, Ravussin E. Effect of short-term thyroxine administration on energy metabolism and mitochondrial efficiency in humans. PLoS One. 2012;7:e40837. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 38] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 28. | Zhang X, Song Y, Feng M, Zhou X, Lu Y, Gao L, Yu C, Jiang X, Zhao J. Thyroid-stimulating hormone decreases HMG-CoA reductase phosphorylation via AMP-activated protein kinase in the liver. J Lipid Res. 2015;56:963-971. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 78] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 29. | Kerr TA, Davidson NO. Cholesterol and nonalcoholic fatty liver disease: renewed focus on an old villain. Hepatology. 2012;56:1995-1998. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 49] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 30. | Moslehi A, Hamidi-Zad Z. Role of SREBPs in Liver Diseases: A Mini-review. J Clin Transl Hepatol. 2018;6:332-338. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 95] [Cited by in RCA: 123] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 31. | Miao Y, Warner M, Gustafsson JK. Liver X receptor β: new player in the regulatory network of thyroid hormone and 'browning' of white fat. Adipocyte. 2016;5:238-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 32. | Yang L, Yin R, Wang Z, Wang X, Zhang Y, Zhao D. Circulating Angptl3 and Angptl8 Are Increased in Patients with Hypothyroidism. Biomed Res Int. 2019;2019:3814687. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 33. | Abu-Farha M, Al-Khairi I, Cherian P, Chandy B, Sriraman D, Alhubail A, Al-Refaei F, AlTerki A, Abubaker J. Increased ANGPTL3, 4 and ANGPTL8/betatrophin expression levels in obesity and T2D. Lipids Health Dis. 2016;15:181. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 77] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 34. | Szczepańska E, Glinicki P, Zgliczyński W, Słowińska-Srzednicka J, Jastrzębska H, Gietka-Czernel M. FGF21 Is Released During Increased Lipogenesis State Following Rapid-Onset Radioiodine-Induced Hypothyroidism. Front Endocrinol (Lausanne). 2022;13:900034. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 35. | Sinha RA, Yen PM. Thyroid hormone-mediated autophagy and mitochondrial turnover in NAFLD. Cell Biosci. 2016;6:46. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 57] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 36. | Byrnes K, Blessinger S, Bailey NT, Scaife R, Liu G, Khambu B. Therapeutic regulation of autophagy in hepatic metabolism. Acta Pharm Sin B. 2022;12:33-49. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 85] [Article Influence: 28.3] [Reference Citation Analysis (0)] |
| 37. | Mavromati M, Jornayvaz FR. Hypothyroidism-Associated Dyslipidemia: Potential Molecular Mechanisms Leading to NAFLD. Int J Mol Sci. 2021;22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 65] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 38. | Duarte SMB, Stefano JT, Vanni DS, Carrilho FJ, Oliveira CPMS. IMPACT OF CURRENT DIET AT THE RISK OF NON-ALCOHOLIC FATTY LIVER DISEASE (NAFLD). Arq Gastroenterol. 2019;56:431-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 39. | Liao CJ, Huang PS, Chien HT, Lin TK, Yeh CT, Lin KH. Effects of Thyroid Hormones on Lipid Metabolism Pathologies in Non-Alcoholic Fatty Liver Disease. Biomedicines. 2022;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 40. | He W, An X, Li L, Shao X, Li Q, Yao Q, Zhang JA. Relationship between Hypothyroidism and Non-Alcoholic Fatty Liver Disease: A Systematic Review and Meta-analysis. Front Endocrinol (Lausanne). 2017;8:335. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 71] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 41. | Loosen SH, Demir M, Kostev K, Luedde T, Roderburg C. Incidences of hypothyroidism and autoimmune thyroiditis are increased in patients with nonalcoholic fatty liver disease. Eur J Gastroenterol Hepatol. 2021;33:e1008-e1012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 42. | Martínez Escudé A, Pera G, Arteaga I, Expósito C, Rodríguez L, Torán P, Caballeria L. Relationship between hypothyroidism and non-alcoholic fatty liver disease in the Spanish population. Med Clin (Barc). 2020;154:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 43. | Lee KW, Bang KB, Rhee EJ, Kwon HJ, Lee MY, Cho YK. Impact of hypothyroidism on the development of non-alcoholic fatty liver disease: A 4-year retrospective cohort study. Clin Mol Hepatol. 2015;21:372-378. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 52] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 44. | Mansour-Ghanaei F, Joukar F, Mobaraki SN, Mavaddati S, Hassanipour S, Sepehrimanesh M. Prevalence of non-alcoholic fatty liver disease in patients with diabetes mellitus, hyperlipidemia, obesity and polycystic ovary syndrome: A cross-sectional study in north of Iran. Diabetes Metab Syndr. 2019;13:1591-1596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 45. | Haufe S, Hupa-Breier KL, Bayerle P, Boeck HT, Rolff S, Sundermeier T, Kerling A, Eigendorf J, Kück M, Hanke AA, Ensslen R, Nachbar L, Lauenstein D, Böthig D, Hilfiker-Kleiner D, Stiesch M, Terkamp C, Wedemeyer H, Haverich A, Tegtbur U. Telemonitoring-Supported Exercise Training in Employees With Metabolic Syndrome Improves Liver Inflammation and Fibrosis. Clin Transl Gastroenterol. 2021;12:e00371. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 46. | Teixeira PFDS, Dos Santos PB, Pazos-Moura CC. The role of thyroid hormone in metabolism and metabolic syndrome. Ther Adv Endocrinol Metab. 2020;11:2042018820917869. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 98] [Cited by in RCA: 110] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 47. | Pujia R, Mazza E, Montalcini T, Arturi F, Brunetti A, Aversa A, Romeo S, Perticone M, Sciacqua A, Pujia A. Liver Stiffness in Obese Hypothyroid Patients Taking Levothyroxine. Medicina (Kaunas). 2022;58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 48. | Chen J, Huang Y, Xie H, Bai H, Lin G, Dong Y, Shi D, Wang J, Zhang Q, Zhang Y, Sun J. Impact of a low-carbohydrate and high-fiber diet on nonalcoholic fatty liver disease. Asia Pac J Clin Nutr. 2020;29:483-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 49. | Kizivat T, Maric I, Mudri D, Curcic IB, Primorac D, Smolic M. Hypothyroidism and Nonalcoholic Fatty Liver Disease: Pathophysiological Associations and Therapeutic Implications. J Clin Transl Hepatol. 2020;8:347-353. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 50. | Srivastava S, Mathur G, Chauhan G, Kapoor P, Bhaskar P, Jain G, Chopra M. Impact of Thyroid Dysfunction on Insulin Resistance: A Study from a Tertiary Care Center in India. J Assoc Physicians India. 2021;69:49-53. [PubMed] |
| 51. | Worm N. Beyond Body Weight-Loss: Dietary Strategies Targeting Intrahepatic Fat in NAFLD. Nutrients. 2020;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 45] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 52. | Anania C, Perla FM, Olivero F, Pacifico L, Chiesa C. Mediterranean diet and nonalcoholic fatty liver disease. World J Gastroenterol. 2018;24:2083-2094. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 156] [Cited by in RCA: 174] [Article Influence: 24.9] [Reference Citation Analysis (0)] |
| 53. | Bellastella G, Scappaticcio L, Caiazzo F, Tomasuolo M, Carotenuto R, Caputo M, Arena S, Caruso P, Maiorino MI, Esposito K. Mediterranean Diet and Thyroid: An Interesting Alliance. Nutrients. 2022;14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 27] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 54. | Semmler G, Datz C, Reiberger T, Trauner M. Diet and exercise in NAFLD/NASH: Beyond the obvious. Liver Int. 2021;41:2249-2268. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 112] [Article Influence: 28.0] [Reference Citation Analysis (0)] |
| 55. | Lin X, Li H. Obesity: Epidemiology, Pathophysiology, and Therapeutics. Front Endocrinol (Lausanne). 2021;12:706978. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 121] [Cited by in RCA: 595] [Article Influence: 148.8] [Reference Citation Analysis (0)] |
| 56. | Wang Y, Lin H, Li Q, Guan L, Zhao M, Zhong F, Liu J, Yuan Z, Guo H, Song Y, Gao L, Zhao J. Association between different obesity phenotypes and hypothyroidism: a study based on a longitudinal health management cohort. Endocrine. 2021;72:688-698. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 57. | Lu FB, Hu ED, Xu LM, Chen L, Wu JL, Li H, Chen DZ, Chen YP. The relationship between obesity and the severity of non-alcoholic fatty liver disease: systematic review and meta-analysis. Expert Rev Gastroenterol Hepatol. 2018;12:491-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 99] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 58. | Polyzos SA, Kountouras J, Mantzoros CS. Obesity and nonalcoholic fatty liver disease: From pathophysiology to therapeutics. Metabolism. 2019;92:82-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 453] [Cited by in RCA: 809] [Article Influence: 134.8] [Reference Citation Analysis (0)] |
| 59. | Amin MK, Ali AI, Elsayed H. Impact of Weight Reduction on Thyroid Function and Nonalcoholic Fatty Liver among Egyptian Adolescents with Obesity. Int J Endocrinol. 2022;2022:7738328. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 60. | Du FM, Kuang HY, Duan BH, Liu DN, Yu XY. Effects of thyroid hormone and depression on common components of central obesity. J Int Med Res. 2019;47:3040-3049. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 61. | Sharma R. Nonalcoholic Fatty Liver Disease and Subclinical Hypothyroidism in Obese Children. Indian J Pediatr. 2021;88:425-426. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (1)] |
| 62. | Caro-Sabido EA, Larrosa-Haro A. Efficacy of dietary intervention and physical activity in children and adolescents with nonalcoholic fatty liver disease associated with obesity: A scoping review. Rev Gastroenterol Mex (Engl Ed). 2019;84:185-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 63. | van der Windt DJ, Sud V, Zhang H, Tsung A, Huang H. The Effects of Physical Exercise on Fatty Liver Disease. Gene Expr. 2018;18:89-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 186] [Article Influence: 26.6] [Reference Citation Analysis (0)] |
| 64. | Ahadi M, Molooghi K, Masoudifar N, Namdar AB, Vossoughinia H, Farzanehfar M. A review of non-alcoholic fatty liver disease in non-obese and lean individuals. J Gastroenterol Hepatol. 2021;36:1497-1507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 59] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 65. | Huang Y, Cai L, Zheng Y, Pan J, Li L, Zong L, Lin W, Liang J, Huang H, Wen J, Chen G. Association between lifestyle and thyroid dysfunction: a cross-sectional epidemiologic study in the She ethnic minority group of Fujian Province in China. BMC Endocr Disord. 2019;19:83. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |