Published online Feb 27, 2023. doi: 10.4254/wjh.v15.i2.274
Peer-review started: August 5, 2022
First decision: October 20, 2022
Revised: November 24, 2022
Accepted: January 18, 2023
Article in press: January 18, 2023
Published online: February 27, 2023
Processing time: 175 Days and 21.1 Hours
Non-alcoholic fatty liver disease is a global health care challenge and a leading indication of liver transplantation (LT). Hence, more patients with diabetes mel
To evaluate the impact of DM on short-term outcomes post-LT in patients over the age of 65.
We collected data of patients who underwent LT from January 2001 until Dece
Total of 148 patients who are 65 year or older underwent LT during the study period. The mean age is 68.5 ± 3.3 years and 67.6% were male. The median Model for End-stage Liver Disease score at time of transplantation was 22 (6-39), 39% of patients had hepatocellular carcinoma and 77.7% underwent living donor LT. The one-year survival was similar between DM patients and others, 91%. ACR occurred in 13.5% of patients (P = 0.902). The median ICU stay is 4.5-day P = 0.023. The rates of ICU and 90-d readmission were similar (P = 0.821) and (P = 0.194), respectively.
The short-term outcome of elderly diabetic patients undergoing LT is similar to others. The presence of DM in elderly LT candidates should not discourage physicians from transplant consideration in this cohort of patients.
Core Tip: Diabetes mellitus (DM) is very common in elderly patients who are candidates for liver transplant. In a single center experience, DM did not affect the short term outcome in elderly patients who underwent liver transplantation (LT). Hepatitis C virus and non-alcoholic steatohepatitis were the leading indications for LT. Majority of patients in this study had living liver donors.
- Citation: Alghamdi S, Alamro S, Alobaid D, Soliman E, Albenmousa A, Bzeizi KI, Alabbad S, Alqahtani SA, Broering D, Al-Hamoudi W. Diabetes mellitus is not associated with worse short term outcome in patients older than 65 years old post-liver transplantation. World J Hepatol 2023; 15(2): 274-281
- URL: https://www.wjgnet.com/1948-5182/full/v15/i2/274.htm
- DOI: https://dx.doi.org/10.4254/wjh.v15.i2.274
Non-alcoholic fatty liver disease (NAFLD) is increasingly becoming a global healthcare challenge with an estimated worldwide prevalence of 24%[1,2]. The leading causes behind the increase are obesity, diabetes mellitus (DM) and dyslipidemia[3]. In recent years, the term metabolic dysfunction-associated fatty liver disease has been put forward as a more inclusive name for NAFLD, however this has not been universally accepted as of yet. Similarly, NAFLD, previously considered a disease of exclusion, is widely accepted as a disease of inclusion and can co-exist with additional chronic liver diseases[3]. It is linked to insulin resistance and fat metabolism dysregulation[4], and it can progress to non-alcoholic steatohepatitis (NASH) and advanced cirrhosis in 25% of patients[5]. Therefore, after the advent of effective direct antiviral therapy for hepatitis C (HCV), NAFLD is now becoming a leading indication for liver transplantation (LT) worldwide[6] and expected to surpass other indications[5].
Currently, the prevalence of NAFLD in Saudi Arabia is 25%, one of the highest rates in the world[7]. Studies have shown a progressive rise in obesity and diabetes in Arab countries and Saudi Arabia[8]. It is not surprising, therefore, that an estimated 30% of the Saudi population could have NAFLD by 2030[7]. In addition, the median age of the population is also increasing[9]. Hence, an increasing number of LTs will be performed on older patients with DM or obesity.
More people above the age of 65 have become candidates for LT[10]. Studies demonstrate that age alone should not disqualify patients from LT if they have no other major contraindications. Functional status and comorbidities are particularly important considerations regarding transplantation in this cohort of patients. Older people often have multiple comorbidities, such as coronary artery disease and DM, that contribute to worse short- and long-term outcomes which vary across transplant centers[10]. Therefore, LT candidates undergo extensive cardiopulmonary evaluation prior to transplantation.
DM is associated with increased mortality among patients with liver cirrhosis[11]. Studies demonstrate that long-term outcomes after LT on both patient and graft survivals, particularly in older populations, are poor; while studies of short-term outcomes are limited[12]. The impact of diabetes on short-term outcomes such as intensive care unit (ICU) stay, length of hospital stay, and acute cellular rejection (ACR) is unknown with regard to Saudi Arabia. Knowledge of these outcomes can inform guidelines for recipient suitability, pre-operative assessment, and immediate post-operative management.
This study aims to evaluate the role of DM as an independent predictor of short-term outcomes in LT recipients aged 65 and over.
Using our electronic medical record system, we retrospectively collected data of patients who underwent LT from January 2001 until December 2019 at King Faisal Specialist Hospital & Research Center in Riyadh. We included all patients who were 65 years or older at the time of transplantation.
We collected basic demographic data (age, gender), body mass index (BMI), indication for transplantation, presence of co-morbidities (DM, hypertension, dyslipidemia, coronary heart disease), and outcomes. We assessed the impact of DM on short-term outcomes, one year, post-LT based on the following variables: Survival at one year; ACR rates; ICU and hospital length of stay (LOS); and readmissions. The diagnoses of DM, hypertension, dyslipidemia, and coronary artery disease were based on the international classification of diseases, 10th revision. ACR must have been biopsy proven with histological changes consistent with ACR.
The Institutional Research Board at King Faisal Specialist Hospital and Research Center approved the study. The consent was waived given the retrospective nature of the study.
Generally, listing patients for LT and ranking them on the waitlist at our center is based on the Model for End-stage Liver Disease (MELD)[13]. Patients were assigned to one of the following rankings: (1) Status 1A for acute liver failure; (2) The calculated MELD score; and (3) MELD exception for patients with hepatocellular carcinoma (HCC), hepatopulmonary syndrome, or portopulmonary hypertension. Patients with HCC were discussed in the tumor multidisciplinary board for locoregional therapy options while completing the workup or waiting for LT. The MELD score was assessed and updated regularly. All patients were seen in the outpatient clinics regularly and within three months prior to their LT.
The standard immunosuppression protocol in our institution includes calcineurin inhibitors and mycophenolate mofetil during the first 6-12 mo after transplantation and oral prednisone for the first 3 mo. The doses of immunosuppressive medications were adjusted according to their serum levels and were modified in patients with renal impairment. We aim to minimize immunosuppression post liver transplantation in patients with HCC.
We used SPSS software (version 21.0; SPSS, Inc., Chicago, IL, United States) for statistical analyses. Data are described in counts and percentages, medians and ranges, and means and standard deviations. Fisher exact or chi-square tests were used to compare categorical variables. Mann-Whitney and t tests were used for continuous nonparametric and parametric variables, respectively. Kaplan-Meier curves were used to estimate 1-year patient survival rates, and log-rank test was used to compare survival between the groups. A significance level of alpha = 0.05 was set.
A total of 148 patients aged 65 years or older underwent LT during the study period. Living donor LT was performed on the majority of the patients (115, 77.7%). The baseline characteristics are summarized in Table 1. Patients were predominantly male (100, 67.6%) with a mean age of 68.5 ± 3.3 years. The median MELD score was 22 (6–39) just prior to transplantation, and hepatocellular carcinoma was present in 58 (39.2%) of patients, with or without other liver diseases.
| Variables | All, n = 148 | DM, n = 98 | No DM, n = 50 | P value | |
| Age (years)1 | 68.5 ± 3.3 | 68.4 ± 3.1 | 68.5 ± 3.9 | 0.578 | |
| Gender (Male)2 | 100 (67.6%) | 69 (70.4%) | 31 (62.0%) | 0.301 | |
| Living Donor2 | 115 (77.7%) | 79 (80.6%) | 37 (74.0%) | 0.355 | |
| Cause of liver disease2 | HCV | 52 (35.1%) | 32 (32.7%) | 20 (40%) | 0.341 |
| HBV | 24 (16.2%) | 14 (14.3%) | 10 (20%) | ||
| NASH | 51 (34.5%) | 35 (35.7%) | 16 (32%) | ||
| Others | 21 (14.2%) | 17 (17.3%) | 4 (8%) | ||
| HCC2 | 58 (39.2%) | 40 (40.8%) | 18 (36.0%) | 0.570 | |
| MELD2 | 22 (6-39) | 22 (6-39) | 21 (8-35) | 0.833 | |
| BMI1 (kg/m2) | 26.7 ± 5.1 | 26.2 ± 4.6 | 28.6 ± 6.1 | 0.048a | |
| HTN2 | 52 (35.1%) | 42 (42.9%) | 10 (20.0%) | 0.006a | |
| Hyperlipidemia2 | 10 (6.8%) | 9 (9.2%) | 1 (2.0%) | 0.100 | |
| CAD2 | 4 (2.7%) | 3 (3.1%) | 1 (2.0%) | 0.692 | |
| CKD2 | 40 (26.4%) | 28 (28.6%) | 12 (24.0%) | 0.554 | |
| On insulin2 | 60 (41.2%) | 60 (60.2%) | 0 | ||
| On OHA2 | 46 (31.1%) | 46 (46.9%) | 0 | ||
| HbA1c1 | 5.9 ± 1.7 | 6.5 ± 1.7 | 4.6 ± 0.8 | 0.000a | |
| Length of stay (days)3 | 24 (2-275) | 23 (2-275) | 22 (4-149) | 0.717 |
Risk factors-namely hyperlipidemia, essential hypertension, cardiac ischemia, and renal impairment-were similar for both diabetic and non-diabetic patients (Table 1). Nondiabetic patients (non-DM) had a higher BMI (28.6 ± 6.1) than patients with diabetes (DM), P = 0.048. The main indication for LT was HCV (52, 35.1%) followed by NASH (51, 34.5%).
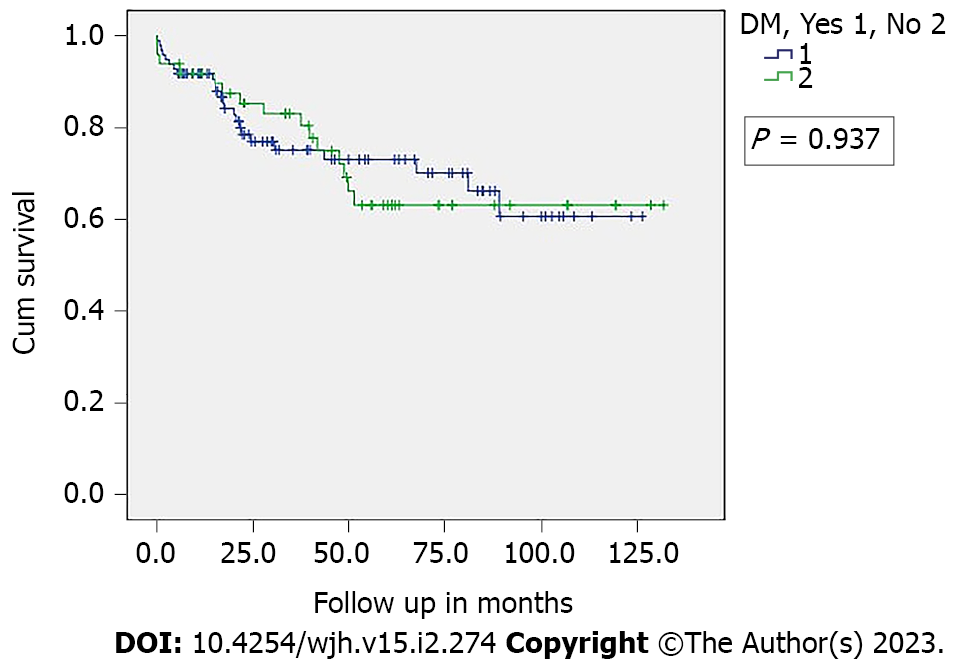
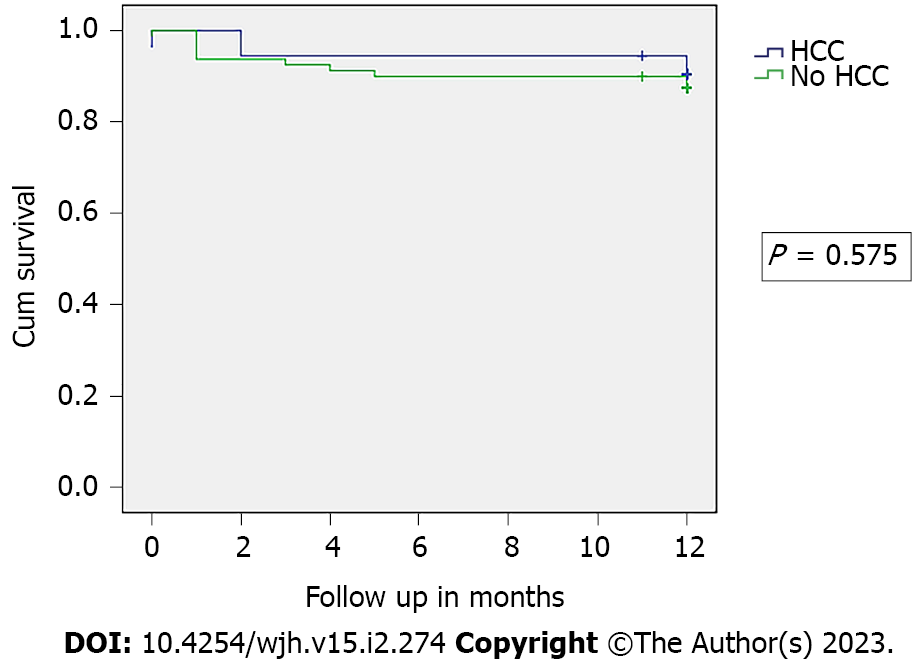
There was a similar median follow-up of 33.5 mo for both diabetic and non-diabetic groups, with a one-year survival rate of 89% (Figure 1). ACR arose in 20 (13.5%) of the total study population (DM = 13, 13.3% and non-DM = 7, 14%; P = 0.902). With regard to ICU readmission, the DM rate was 11 (11.2%) while non-DM was 5 (10%; P = 0.821). Although hospital LOS was comparable (DM = 23 d and non-DM = 22 d; P = 0.717), the median ICU stay was shorter in days for DM patients, DM = 4 (1-70) compared to non-DM = 5 (2-185), P = 0.023. The 90-d readmission rate was likewise largely similar (DM = 38.8% and non-DM = 28%; P = 0.194). The presence of HCC did not affect survival outcomes within the first year after transplantation (Figure 2).
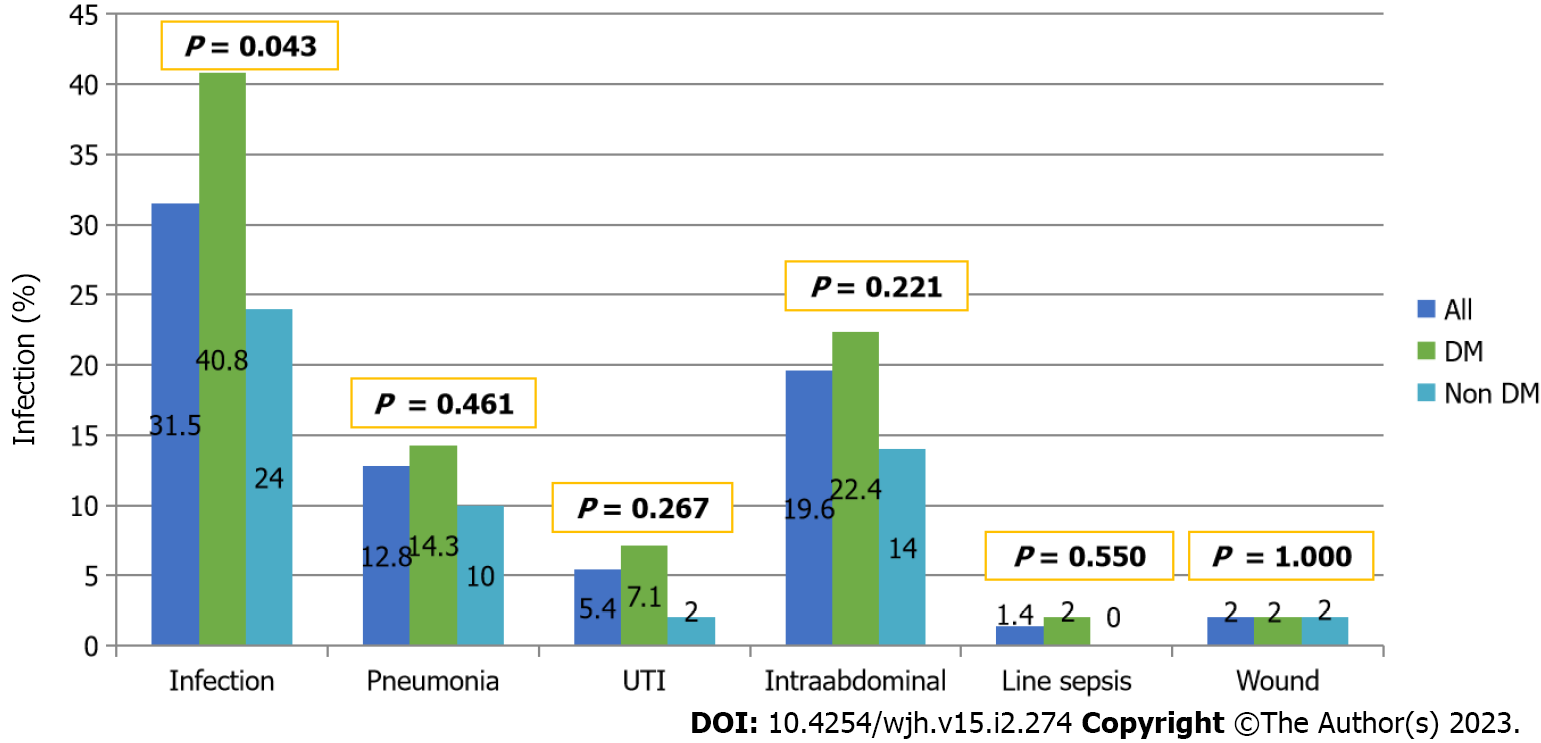
In the first-year post-transplantation, 31.5% of patients experienced at least one infectious event. DM patients had a higher rate of infections (40.8% vs 24%, P = 0.043). However, there has been no statistically significant difference regarding the site of infection (Figure 3). Intrabdominal infections are the most commonly seen infectious source 22.4% followed by pneumonia 14.3%.
Data from recent literature suggests that diabetics who are candidates for, or are in the post-operative context of, LT might have severe negative impact on the long-term outcome of these patients. Therefore, adequately controlling diabetes is crucial to increasing candidacy for LT and improving long-term outcomes[14]. The short-term outcome of diabetes among older patients undergoing LT is unknown. Furthermore, the data are extremely limited in this subgroup of patients who have undergone living donor LT. Our results showed an excellent one-year survival rate of 89%, which is comparable with the survival rate among highly performing LT centers[15,16]. We also found that the survival rate was similar between deceased-donor and living-donor LT patients in this cohort. The presence of DM before LT did not have a negative impact on short-term survival. Aravinthan et al[12] showed that neither pretransplant nor posttransplant DM affect the survival post-LT[12]. However, an association was found between chronic renal failure, major cardio-vascular diseases and pretransplant DM. In contrast to our study, they included younger patients as well, with a median age of 54. Other larger studies have shown that DM has a statistically significant negative effect on patient and graft survival[17].
Both patients with diabetes and those without experienced ACR at a similar rate. Several reports illustrated an increased risk of ACR and graft loss among patients with pretransplant DM. Most ACR occurs within the first year after transplantation. A study by Lieber et al[18] demonstrated an increased risk of ACR among patients with posttransplant DM[18], although a smaller study did not detect any effect of either pre-transplant DM or post-transplant DM on ACR[19]. In general, however, patients with pre-transplant DM experience worse graft survival rates[17,20]. As expected, more diabetic patients had infections in their first-year post transplantation. The infection specific site was similar between both groups. Despite increased infectious complications in the DM patients, the survival rate is similar as outlined above.
Both groups had similar ICU and hospital stays, and the rate of readmission was also similar. A large study of 3772 patients from the United Kingdom with a 20% prevalence of diabetes showed that DM did not have any effect on LOS[21]. However, a study of 12442 patients from the United States of America with a 24% prevalence of diabetes found that diabetic recipients perform worse with regard to LOS and readmissions[16]. The differences, though, are small and may not be clinically relevant. Rather, individual patient factors are more important. A study by Washburn et al[22] showed that MELD score and increasing age are independent predictors of hospital LOS. The overall median LOS was higher than what has been reported in the literature by other centers. This is primarily because of the nature of the health-care system in Saudi Arabia, which has few available acute rehabilitation centers and primary care physician networks. Therefore, patients remain in the hospital until they are fully mobile and independent before discharge.
Overall, the principle limiting factors of this study are its’ retrospectivity and the single-center experience. Nevertheless the data can be considered representative of our region since over half of LTs in Saudi Arabia are performed at our center[23]. Furthermore over the last decades, advances have been made in the medical management of LT patients resulting in improved early outcomes, though not significantly improved long-term survival[24]. Another potential limiting factor is the low number of deceased donors in our cohort. One last limitation for this study is that we did not use the random forest survival analysis, an analysis representing the rapid rise of artificial intelligence in medicine, which surpasses traditional statistical approaches in terms of accuracy and explainable utility.
The short-term outcome of elderly diabetic patients undergoing LT is similar to patients without diabetes. The presence of DM in elderly liver transplant candidates should not discourage physicians when considering patients for LT.
More patients older than 65 undergo liver transplantation (LT) nowadays. Significant number of those patients have diabetes mellitus (DM).
To address the impact of DM on short term outcome post liver transplant in patients older than 65. There is limited data in the literature particularly for patients undergoing living donor LT.
To determine the short term impact of DM in older patients post LT.
This is a retrospective study of previously collected data from a high volume single transplant center. We included all patients who are 65 years old or older at the time of transplantation and assessed important short term outcomes such as one year survival, intensive care unit length of stay and acute cellular rejection.
One-year survival was comparable between diabetic and nondiabetic elderly patients undergoing LT. Acute cellular rejection rates were comparable between diabetic and nondiabetic elderly patients undergoing LT. Intensive care unit, hospital length of stay, and readmissions were comparable between diabetic and nondiabetic elderly patients undergoing LT.
Diabetes was not found to affect the short-term outcomes in elderly patients undergoing LT.
The presence of DM in elderly liver transplant candidates should not discourage physicians when considering patients for LT.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Saudi Arabia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lee KS, South Korea; Naderi D, Iran S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
| 1. | Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5322] [Cited by in RCA: 7504] [Article Influence: 833.8] [Reference Citation Analysis (0)] |
| 2. | Asrani SK, Devarbhavi H, Eaton J, Kamath PS. Burden of liver diseases in the world. J Hepatol. 2019;70:151-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1382] [Cited by in RCA: 2279] [Article Influence: 379.8] [Reference Citation Analysis (0)] |
| 3. | Eslam M, Newsome PN, Sarin SK, Anstee QM, Targher G, Romero-Gomez M, Zelber-Sagi S, Wai-Sun Wong V, Dufour JF, Schattenberg JM, Kawaguchi T, Arrese M, Valenti L, Shiha G, Tiribelli C, Yki-Järvinen H, Fan JG, Grønbæk H, Yilmaz Y, Cortez-Pinto H, Oliveira CP, Bedossa P, Adams LA, Zheng MH, Fouad Y, Chan WK, Mendez-Sanchez N, Ahn SH, Castera L, Bugianesi E, Ratziu V, George J. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. J Hepatol. 2020;73:202-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2883] [Cited by in RCA: 2802] [Article Influence: 560.4] [Reference Citation Analysis (1)] |
| 4. | Neuschwander-Tetri BA. Non-alcoholic fatty liver disease. BMC Med. 2017;15:45. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 262] [Cited by in RCA: 325] [Article Influence: 40.6] [Reference Citation Analysis (0)] |
| 5. | Goh GB, McCullough AJ. Natural History of Nonalcoholic Fatty Liver Disease. Dig Dis Sci. 2016;61:1226-1233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 97] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 6. | Parrish NF, Feurer ID, Matsuoka LK, Rega SA, Perri R, Alexopoulos SP. The Changing Face of Liver Transplantation in the United States: The Effect of HCV Antiviral Eras on Transplantation Trends and Outcomes. Transplant Direct. 2019;5:e427. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 7. | Alswat K, Aljumah AA, Sanai FM, Abaalkhail F, Alghamdi M, Al Hamoudi WK, Al Khathlan A, Al Quraishi H, Al Rifai A, Al Zaabi M, Babatin MA, Estes C, Hashim A, Razavi H. Nonalcoholic fatty liver disease burden - Saudi Arabia and United Arab Emirates, 2017-2030. Saudi J Gastroenterol. 2018;24:211-219. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 87] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 8. | Alzaman N, Ali A. Obesity and diabetes mellitus in the Arab world. J Taibah University Medical Sciences. 2016;11:301-309. [RCA] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Plecher H. Saudi Arabia - median age of the population 1950-2050 [Internet]. Statista. 2020;. [DOI] [Full Text] |
| 10. | Durand F, Levitsky J, Cauchy F, Gilgenkrantz H, Soubrane O, Francoz C. Age and liver transplantation. J Hepatol. 2019;70:745-758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 211] [Article Influence: 35.2] [Reference Citation Analysis (0)] |
| 11. | Quintana JO, García-Compean D, González JA, Pérez JZ, González FJ, Espinosa LE, Hernández PL, Cabello ER, Villarreal ER, Rendón RF, Garza HM. The impact of diabetes mellitus in mortality of patients with compensated liver cirrhosis-a prospective study. Ann Hepatol. 2011;10:56-62. [PubMed] |
| 12. | Aravinthan AD, Fateen W, Doyle AC, Venkatachalapathy SV, Issachar A, Galvin Z, Sapisochin G, Cattral MS, Ghanekar A, McGilvray ID, Selzner M, Grant DR, Selzner N, Lilly LB, Renner EL, Bhat M. The Impact of Preexisting and Post-transplant Diabetes Mellitus on Outcomes Following Liver Transplantation. Transplantation. 2019;103:2523-2530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 13. | Kamath PS, Kim WR; Advanced Liver Disease Study Group. The model for end-stage liver disease (MELD). Hepatology. 2007;45:797-805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1075] [Cited by in RCA: 1223] [Article Influence: 67.9] [Reference Citation Analysis (0)] |
| 14. | Brodosi L, Petta S, Petroni ML, Marchesini G, Morelli MC. Management of Diabetes in Candidates for Liver Transplantation and in Transplant Recipients. Transplantation. 2022;106:462-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 15. | Aduen JF, Sujay B, Dickson RC, Heckman MG, Hewitt WR, Stapelfeldt WH, Steers JL, Harnois DM, Kramer DJ. Outcomes after liver transplant in patients aged 70 years or older compared with those younger than 60 years. Mayo Clin Proc. 2009;84:973-978. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 98] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 16. | Bhat V, Tazari M, Watt KD, Bhat M. New-Onset Diabetes and Preexisting Diabetes Are Associated With Comparable Reduction in Long-Term Survival After Liver Transplant: A Machine Learning Approach. Mayo Clin Proc. 2018;93:1794-1802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 45] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 17. | Hoehn RS, Singhal A, Wima K, Sutton JM, Paterno F, Steve Woodle E, Hohmann S, Abbott DE, Shah SA. Effect of pretransplant diabetes on short-term outcomes after liver transplantation: a national cohort study. Liver Int. 2015;35:1902-1909. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 40] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 18. | Lieber SR, Lee RA, Jiang Y, Reuter C, Watkins R, Szempruch K, Gerber DA, Desai CS, DeCherney GS, Barritt AS 4th. The impact of post-transplant diabetes mellitus on liver transplant outcomes. Clin Transplant. 2019;33:e13554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 19. | Dogan N, Hüsing-Kabar A, Schmidt HH, Cicinnati VR, Beckebaum S, Kabar I. Acute allograft rejection in liver transplant recipients: Incidence, risk factors, treatment success, and impact on graft failure. J Int Med Res. 2018;46:3979-3990. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 20. | Kuo HT, Lum E, Martin P, Bunnapradist S. Effect of diabetes and acute rejection on liver transplant outcomes: An analysis of the organ procurement and transplantation network/united network for organ sharing database. Liver Transpl. 2016;22:796-804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 21. | Tovikkai C, Charman SC, Praseedom RK, Gimson AE, van der Meulen J. Time spent in hospital after liver transplantation: Effects of primary liver disease and comorbidity. World J Transplant. 2016;6:743-750. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Washburn WK, Meo NA, Halff GA, Roberts JP, Feng S. Factors influencing liver transplant length of stay at two large-volume transplant centers. Liver Transpl. 2009;15:1570-1578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 48] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 23. | Rogiers X, Berrevoet F, Troisi R. Comments on Bonney et al. "Outcomes on right liver lobe transplantation: a match pair analysis" (Transpl. Int. 2008; 21: 1045-1051). Transpl Int. 2009;22:588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 24. | Rana A, Ackah RL, Webb GJ, Halazun KJ, Vierling JM, Liu H, Wu MF, Yoeli D, Kueht M, Mindikoglu AL, Sussman NL, Galván NT, Cotton RT, O'Mahony CA, Goss JA. No Gains in Long-term Survival After Liver Transplantation Over the Past Three Decades. Ann Surg. 2019;269:20-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 92] [Article Influence: 15.3] [Reference Citation Analysis (0)] |