Published online May 27, 2022. doi: 10.4254/wjh.v14.i5.1038
Peer-review started: December 22, 2021
First decision: February 15, 2022
Revised: April 24, 2022
Accepted: April 24, 2022
Article in press: April 24, 2022
Published online: May 27, 2022
Processing time: 152 Days and 12.9 Hours
Transjugular intrahepatic portosystemic shunt (TIPS) is a method used to decrease portal hypertension. Biliary stricture is the rarest of the complications associated with this procedure with only 12 cases previously reported in the literature. None of these cases have documented the resolution of biliary stenosis induced by a stent graft. The only curative solutions reported are liver trans
This is the first reported case of biliary obstruction secondary to TIPS placement in a transplanted liver. In our patient, a portosystemic shunt was created to treat severe veno-occlusive liver graft disease manifesting itself primarily by fluid retention. A cholestatic liver lesion and cholangitis with abscesses developed due to a stent graft-induced stricture in the dorsal segment of the right hepatic duct and the stricture diminished following percutaneous drainage. Endoscopic drainage was performed after unsuccessful removal of the percutaneous catheter resulting in a bilio-cutaneous fistula. Although the liver graft now functions well, the stricture remains refractory even after 44 mo of treatment.
Biliary strictures caused by TIPS in both transplanted and native livers seem refractory to endoscopic treatment.
Core Tip: Biliary stricture is the most unusual complication of transjugular intrahepatic portosystemic shunt (TIPS) implantation yet to be reported in liver transplant recipients. In our patient, TIPS was successfully used to treat the rare liver graft disease, sinusoidal obstruction syndrome. Cholangitis with abscess formation caused by a TIPS-induced stricture of the right hepatic duct was successfully treated by percutaneous and subsequent endoscopic drainage and resulted in preserved liver graft function. However, the stenosis persisted even after long-term endoscopic treatment. The outcome of our case is comparable to those reported in a native liver where no case was resolved using only biliary drainage.
- Citation: Macinga P, Gogova D, Raupach J, Jarosova J, Janousek L, Honsova E, Taimr P, Spicak J, Novotny J, Peregrin J, Hucl T. Biliary obstruction following transjugular intrahepatic portosystemic shunt placement in a patient after liver transplantation: A case report. World J Hepatol 2022; 14(5): 1038-1046
- URL: https://www.wjgnet.com/1948-5182/full/v14/i5/1038.htm
- DOI: https://dx.doi.org/10.4254/wjh.v14.i5.1038
Transjugular intrahepatic portosystemic shunt (TIPS) is a procedure in which an artificial portosystemic shunt is applied to decrease portal hypertension. The most common indications are refractory ascites and uncontrolled variceal bleeding which often serves as a bridge to liver transplantation. Common complications of TIPS include encephalopathy, cardiac failure, occlusion and infection. Serious biliary complications are rare and occur in less than 1% of cases[1].
TIPS insertion can create a tract between the shunt and non-vascular structures, typically resulting in a biliary-TIPS fistula. This fistula can cause haemobilia and jaundice and is associated with acute and chronic TIPS occlusion[2]. Such complications have been significantly reduced with the use of covered stent grafts. Biliary stenosis secondary to TIPS placement is extremely rare with only 12 cases documented (7 case reports and 1 case series) (Table 1). Interestingly, a single-center retrospective study found TIPS-related segmental intrahepatic cholestasis in 4 of 135 intervened patients (2.9%)[3]. However, this observation has yet to be confirmed by further studies.
| Ref. | Indication for TIPS placement | Interval between TIPS placement and biliary complications | Clinical presentation | Imaging finding | Treatment | Outcome | Long-term follow-up |
| Peynircioglu et al[12] | OH, in HCV cirrhosis | 3 mo | Jaundice, acute cholangitis | RHD stenosis by TIPS | PTC, impassable stricture, external biliary drainage | Decrease in bilirubin; sepsis due to infectious colitis, colon perforation, death | - |
| Duller et al [13] | OH in cirrhosis (aetiology not reported) | 4 mo | Jaundice | RHD stenosis by TIPS, fistula, biloma | TIPS replacement with a polytetrafluoroethylene-covered Wallstent, biloma drainage | Regression of biloma; SSC | OLTx |
| Paterno et al[14] | OH, in HCV cirrhosis | Immediate | Jaundice | Malposition of TIPS in CBD, obstruction of LHD and RHD at confluence | OLTx with HJA | Uneventful recovery | |
| Karlas et al[15] | RA in ALC | 18 mo (TIPS placement); 10 mo (TIPS extension) | Jaundice | Branch of RHD compression by TIPS extension | None, non-compliant patient | - | OLTx KI for continuous alcohol abuse |
| Korrapati et al[1] | RA in BCS | Immediate | Cholestatic liver lesion | LHD stenosis by TIPS | ERCP with biliary stent placement | Regression of cholestasis, persistent stenosis with stent replacement at 2 mo | Not reported |
| Meng et al[16] | OH, in cirrhosis (aetiology not reported) | 5 d | Jaundice | RHD stenosis by TIPS | PTC, impassable stricture, external biliary drainage | Normalisation of bilirubin | External drainage in situ for 2 yr, one episode of mild cholangitis |
| OH, in cirrhosis due to schistosomiasis | 10 d | Jaundice | RHD stenosis by TIPS | PTC, impassable stricture, external biliary drainage | Normalisation of bilirubin | Enrolled on WL for OLTx | |
| Bucher et al[3] | RA + HRS in ALC | 72 mo | Asymptomatic | Compression of segmental bile duct (SVII) by TIPS | None | - | Resolution of imaging finding after 2 yr; death due to metastatic HCC |
| RA in ALC | 83 mo | Asymptomatic | Compression of segmental bile duct (SVII) by TIPS, cystic congestion of the intrahepatic bile ducts (SVII) | None | - | Stable on F-U | |
| RA + HRS in ALC | 17 mo | Jaundice | Compression of segmental bile duct (SV) by TIPS | Failed ERCP (stricture not achieved); PTC KI for ascites; ATB prophylaxis | Lost to F-U (continuous alcohol abuse) | - | |
| RA in BCS | 0.4 mo | Cholestatic liver lesion | Stenosis of segmental bile duct (SI) by TIPS; liver abscess (SI) | Percutaneous drainage of abscess, failed ERCP (impassable stricture) | Normalisation of liver enzymes | “Unremarkable” | |
| Zhang et al[17] | Recurrent colonic variceal bleeding due to CTPV | 3 d | Jaundice | CBD stenosis by TIPS | Percutaneous and endoscopic drainage | Refractory stenosis, recurrent cholangitis; magnetassisted endoscopic biliaryduodenal anastomosis after 33 mo due to TIPS | |
This report documents the very first case of a TIPS-related bile duct stricture in a liver graft.
Dyspnoea in a patient early after liver transplantation.
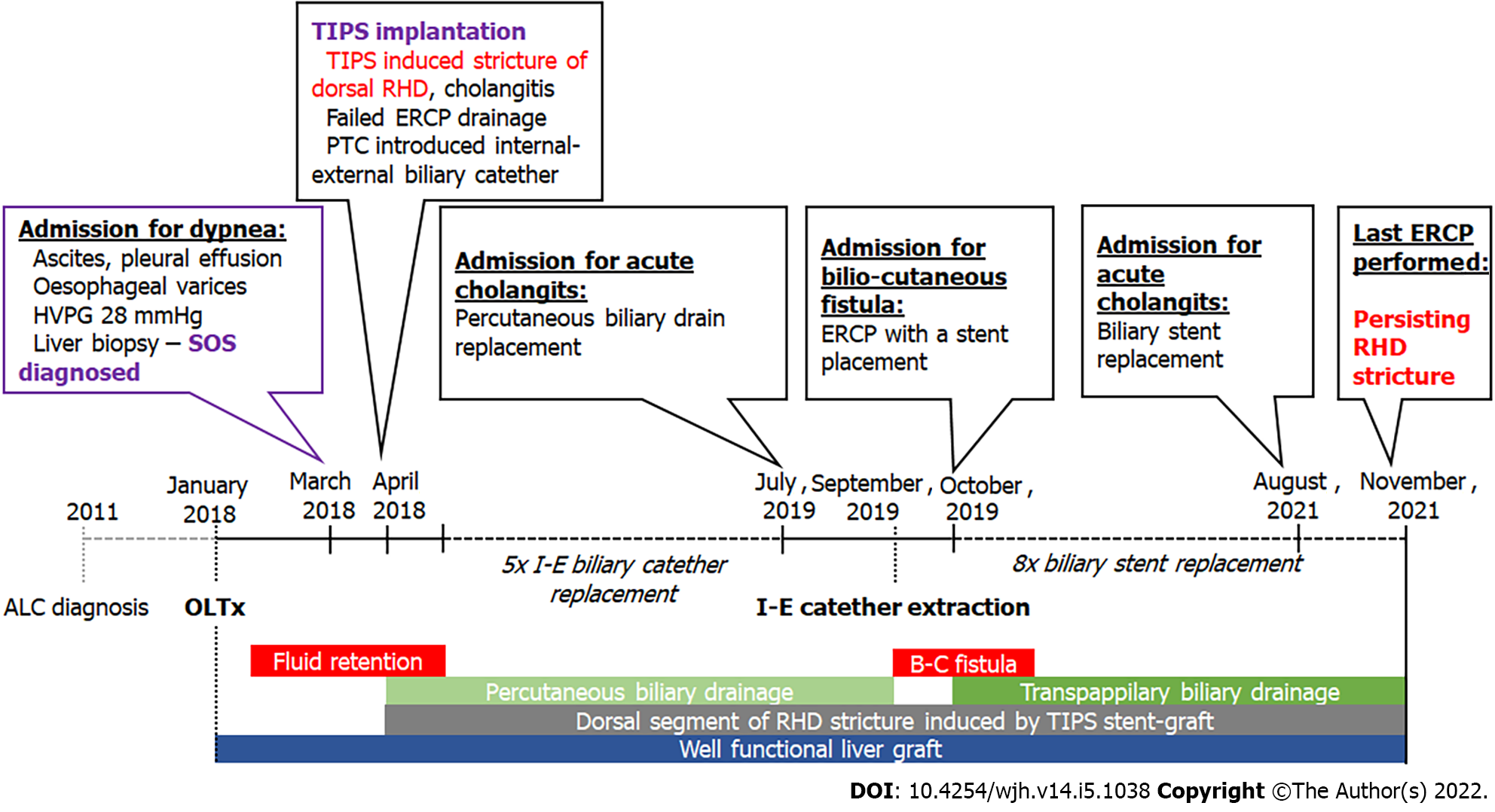
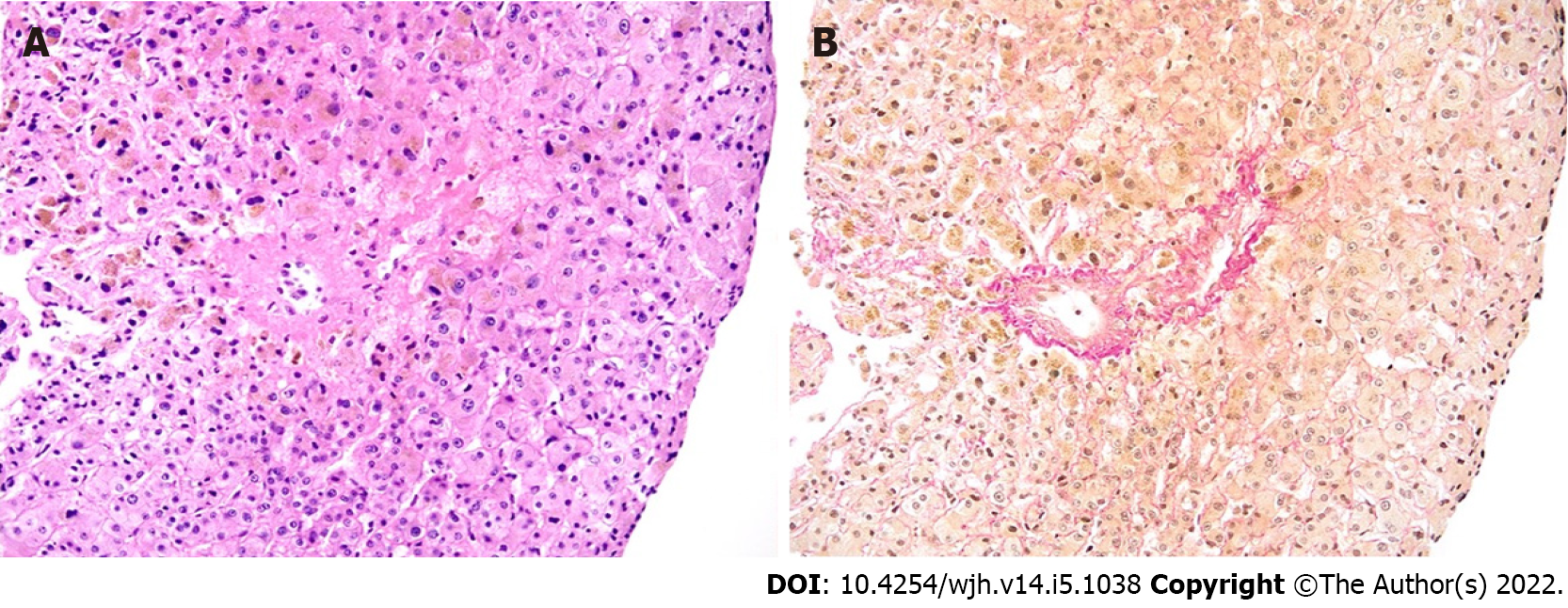
A 40-year-old Caucasian male underwent orthotopic liver transplantation for alcoholic liver cirrhosis (see Figure 1 for timeline). He received a full graft from an ABO-compatible 74-year-old cadaveric donor. Cold ischemia time was 3 h 21 min. The transplantation was performed using piggyback technique with side-to-side caval anastomosis (Belghiti Technique) and standard end-to-end hilar anastomoses. The duration of the procedure was 2 h 52 min. The postoperative course was uneventful. The immunosuppressive regimen consisted of tacrolimus, mycophenolate mofetil and corticosteroids. A month later, the patient presented with symptomatic ascites, large right-sided pleural effusion and normal liver function. Upper endoscopy revealed esophageal varices and the consequent catheterization of the hepatic veins showed a portosystemic gradient of 28 mmHg. Liver biopsy revealed microvascular damage corresponding to sinusoidal obstruction syndrome (SOS) (Figure 2). The patient was subsequently indicated for placement of a TIPS stent graft. This procedure was successfully performed and reduced the portosystemic gradient to 11 mmHg (Figure 3). Immediately after placement of the shunt, a rise in cholestatic enzyme levels was observed.
In the pre-transplant period, the patient was diagnosed with alcoholic liver cirrhosis but displayed no other significant comorbidities. He suffered from several severe episodes of hepatic encephalopathy (including coma) and was also treated for hepatorenal syndrome. At the time of transplantation, he had a MELD score of 27 and his Child-Pugh class was C (14 points).
The patient had a history of alcohol addiction but had been abstaining from alcohol for 2 years before liver transplantation. He had smoked 20 cigarettes a day for 20 years prior to quitting 18 mo prior to the present illness. His family history was unremarkable.
Upon initial examination, the patient was sarcopenic, pale, anicteric and dyspneic at rest with an oxygen saturation of 88%. He had tachycardia at 102 pulses per minute but blood pressure was within normal values. Breath sounds were inaudible on the right side and percussion in the right chest was dull. The patient exhibited large ascites and a palpable liver but no lower-limb oedema. No remarkable abdominal wall collateral vessels were noted on physical examination. After TIPS placement, we observed a significant regression in physical signs of both ascites and pleural effusion.
Upon admission, bilirubin and liver enzymes were within normal limits (total bilirubin 0.86 mg/dL, AST 18.67 U/L, ALT 26.51 U/L, ALP 96.58 U/L and GGT 62.99 U/L). Total serum protein was 46.5 g/L and the albumin level was 23.7 g/L. After shunt placement, we observed an elevated ALP (292.74 U/L) and GGT (435.51 U/L), but levels of bilirubin, AST and ALT remained at normal values.
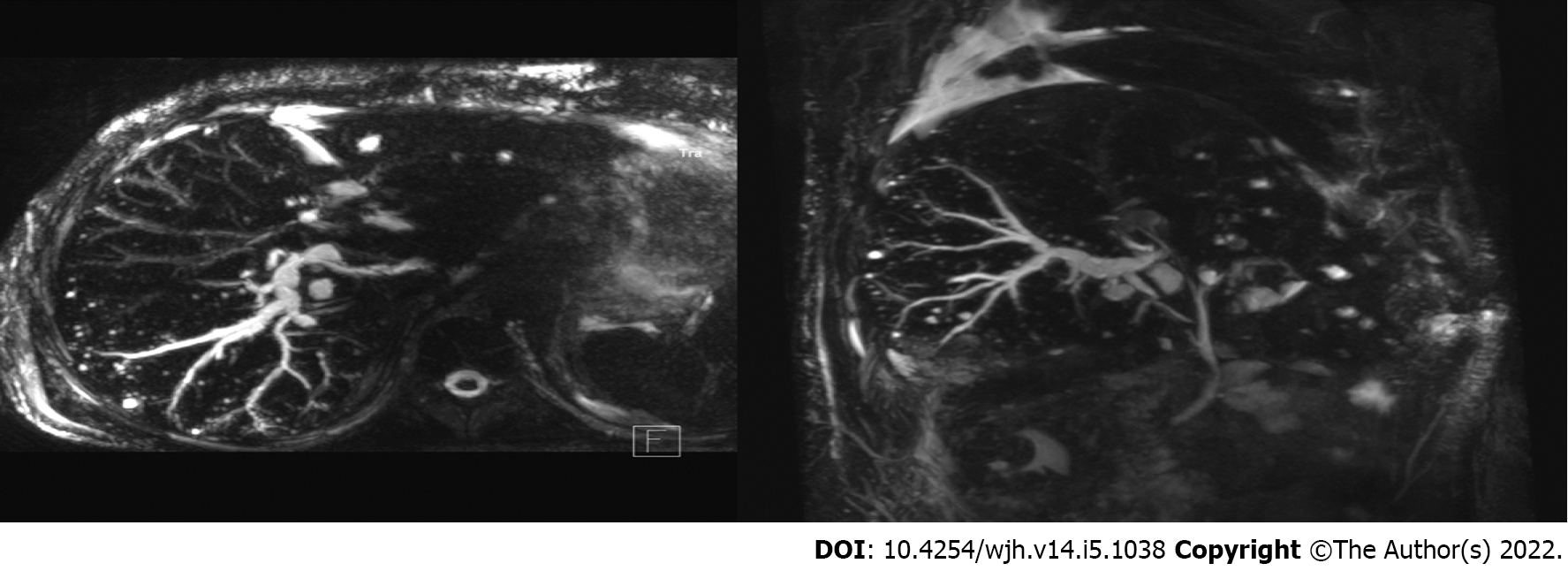
The initial abdominal ultrasound showed marked hepatomegaly (20.5 cm in the craniocaudal length) and massive ascites. After TIPS placement, liver ultrasound revealed a patent shunt with appropriate blood flow. Subsequent magnetic resonance analysis revealed tight stenosis of the right dorsal hepatic duct caused by the compression of the previously placed stent graft with prestenotic tract dilation and multiple small abscesses (Figure 4).
The patient was diagnosed with cholangitis and abscess formation due to biliary stenosis secondary to TIPS.
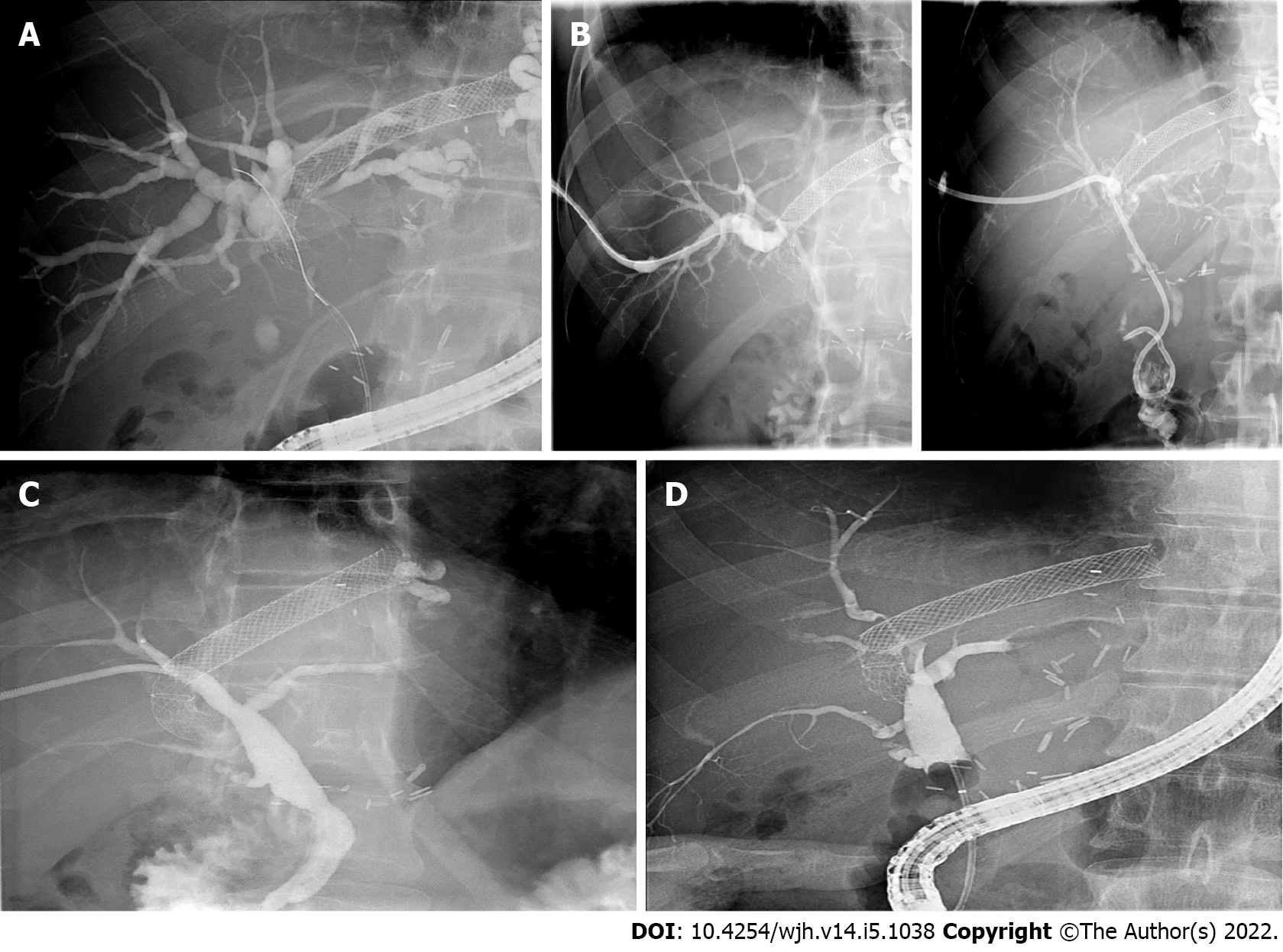
Intravenous antibiotics were administered. Endoscopic cholangiography confirmed our previous magnetic resonance finding. However, an attempt at biliary stent placement proved unsuccessful (Figure 5A). Following failed endoscopic drainage, an internal-external catheter was placed percutaneously (Figure 5B).
Percutaneous intervention led to a prompt reduction in cholestasis and the disappearance of hepatic abscesses. As a result, the patient was discharged. During follow-up, ascites and pleural effusion resolved completely. After 17 mo involving five replacements of the percutaneous drain, we observed a significant regression in biliary stenosis allowing for drainage extraction (Figure 5C). Shortly afterwards, however, the patient presented with a biliary leak due to opening of the cutaneous channel. Endoscopic cholangiography revealed persistent biliary stenosis. Endoscopic stent placement resulted in the resolution of the biliary fistula. Over the next 26 mo, the patient underwent eight ERCPs with repeated balloon dilations and stent replacements. Stricture location and anatomy do not allow for metal stent implantation and the stenosis has thus far proved refractory to treatment (Figure 5D). To date, the patient has suffered from two episodes of acute cholangitis and the liver graft has remained functional.
Biliary complications are common in liver transplant recipients occurring in approximately 30% of patients[4]. Among the most common are anastomotic (AnS) and non-anastomotic strictures (nAnS), with incidence of 6%–12% and 0.5%–10%, respectively[5]. Anastomotic strictures account for up to 80% of all stenotic complications and respond excellently to endoscopic treatment, especially those that occur early (< 3 mo after OLTx)[4]. AnS require the placement of repetitive multiple plastic stents or self-expandable metal stents to achieve sufficient radial tension. Recurrence of the stricture after treatment is uncommon, representing less than 20% of cases[6]. In contrast to AnS, endoscopic treatment of nAnS is difficult and often unsuccessful, resulting in compromised graft survival[7]. We know of no other reported case of non-anastomotic stricture in a transplanted liver due to TIPS placement.
Hepatic sinusoidal obstruction syndrome (SOS; previously known as veno-occlusive disease) is a rare endothelial disorder that occurs particularly after exposure to drugs or toxins. Obstruction of the terminal hepatic venules and sinusoids is typical following hematopoietic cell transplantation and as a consequence of myeloablative preparation (in up to 15% of patients)[8]. SOS is also infrequently observed in liver transplant recipients (with an approximate prevalence of 2%)[9], presumably as an immune-mediated condition related to rejection episodes or azathioprine therapy. SOS is also associated with inferior graft and patient survival[9,10]. The typical clinical manifestation of the disease is a triad of hepatomegaly, fluid retention and jaundice; treatment usually relies on fortification of immunosuppression. A few other pharmacological agents can be used for SOS therapy, but evidence of their efficacy in solid organ transplant recipients is limited. It has been documented that in the case of severe disease refractory to medical treatment, TIPS placement prior to re-transplantation is a justifiable therapy in patients after liver transplant; however, very few cases have been reported in the literature[11].
In our case, veno-occlusive disease manifesting in hepatomegaly and portal hypertension was successfully treated by TIPS intervention. Cholestatic injury developed as a consequence of biliary stenosis induced by the TIPS stent graft. The tight stenosis initially only allowed for percutaneous drainage, which was then converted to internal biliary stents after an unsuccessful attempt at removal. To date, even after a total follow-up time of 44 mo, endoscopic treatment has failed to resolve the stenosis. The patient remains dependent on repeated stent exchange due to refractory and persistent right hepatic duct stenosis.
Our observations are consistent with the outcomes of previously reported cases. Biliary stenosis due to TIPS has been reported in twelve patients thus far. In ten of these (83%) cases, patients were symptomatic and required treatment. Seven patients were indicated for biliary drainage: ERCP was attempted in three patients and percutaneous therapy in four patients. ERCP as a first-line treatment was technically successful only in one of the three patients, failing in the remaining two. One patient was contraindicated for percutaneous drainage due to ascites, but ERCP subsequently failed and the patient was lost to follow-up. In the other patient, laboratory findings normalized solely due to percutaneous drainage of a hepatic abscess proximal to the stricture. Surprisingly, however, the long-term outcome of this patient was designated “unremarkable” in spite of the stenosis having not been resolved. A primary percutaneous approach was successful in all of the remaining four cases. However, in three of these cases, only external drainage due to an impassable stricture was possible, with the fourth patient later converted to internal drainage. Altogether, successful stenting of TIPS-induced stenosis has been reported in only two published cases, both having either unknown or unfavorable long-term outcomes. While in the first patient only a very short 2-mo follow-up was reported, in the second patient the stricture remained refractory even after almost 3 years of percutaneous and subsequent endoscopic drainage.
The above observations may be attributable to characteristic differences between TIPS-induced stenosis and other etiologies. In TIPS-induced stenosis, ducts narrow due to external compression of the metal stent graft. In these instances, radial force cannot be completely reverted by balloon dilation or implantation of plastic stents or drains, as with, for example, fibrotic stenosis. Resolution of symptomatic TIPS-induced biliary strictures was only achieved in four of the ten patients: three by liver transplantation and one by magnet-assisted endoscopic biliary-duodenal anastomosis. Of the remaining six patients, one died from colon perforation, two were lost to follow-up due to continuous abuse of alcohol, one patient remained on internal biliary drainage and another on external biliary drainage. In the last patient, the stricture became unexpectedly asymptomatic after percutaneous drainage of a liver abscess induced by stenosis.
We present here a peculiar case of a liver transplant recipient with a unique non-anastomotic biliary stricture caused by a TIPS stent graft implanted as a treatment for a very rare post-transplant complication, hepatic sinusoidal obstruction syndrome. To our knowledge, this extraordinary case is the first to document biliary complication due to TIPS placement in a transplanted liver. In our patient, cholestatic liver injury was reverted by successful biliary drainage, resulting in preserved graft function. To date, even after a long follow-up period, the stenosis remains refractory to endoscopic treatment, with the patient dependent on repeated stent replacements. These results correspond with outcomes from previously published rare cases of TIPS-induced biliary strictures in native livers, in which complete resolution was only achieved as a result of liver transplantation or advanced endoscopic techniques.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Czech Republic
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Kitamura K, Japan; Sintusek P, Thailand S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Ma YJ
| 1. | Korrapati P, Bidari K, Komanduri S. Biliary Obstruction After Transjugular Intrahepatic Portosystemic Shunt Placement in a Patient With Budd-Chiari Syndrome. ACG Case Rep J. 2015;2:101-103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Saxon RR, Mendel-Hartvig J, Corless CL, Rabkin J, Uchida BT, Nishimine K, Keller FS. Bile duct injury as a major cause of stenosis and occlusion in transjugular intrahepatic portosystemic shunts: comparative histopathologic analysis in humans and swine. J Vasc Interv Radiol. 1996;7:487-497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 102] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 3. | Bucher JN, Hollenbach M, Strocka S, Gaebelein G, Moche M, Kaiser T, Bartels M, Hoffmeister A. Segmental intrahepatic cholestasis as a technical complication of the transjugular intrahepatic porto-systemic shunt. World J Gastroenterol. 2019;25:6430-6439. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 4. | Roos FJM, Poley JW, Polak WG, Metselaar HJ. Biliary complications after liver transplantation; recent developments in etiology, diagnosis and endoscopic treatment. Best Pract Res Clin Gastroenterol. 2017;31:227-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 40] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 5. | Lisotti A, Fusaroli P, Caletti G. Role of endoscopy in the conservative management of biliary complications after deceased donor liver transplantation. World J Hepatol. 2015;7:2927-2932. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Alazmi WM, Fogel EL, Watkins JL, McHenry L, Tector JA, Fridell J, Mosler P, Sherman S, Lehman GA. Recurrence rate of anastomotic biliary strictures in patients who have had previous successful endoscopic therapy for anastomotic narrowing after orthotopic liver transplantation. Endoscopy. 2006;38:571-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 77] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 7. | Verdonk RC, Buis CI, van der Jagt EJ, Gouw AS, Limburg AJ, Slooff MJ, Kleibeuker JH, Porte RJ, Haagsma EB. Nonanastomotic biliary strictures after liver transplantation, part 2: Management, outcome, and risk factors for disease progression. Liver Transpl. 2007;13:725-732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 116] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 8. | Coppell JA, Richardson PG, Soiffer R, Martin PL, Kernan NA, Chen A, Guinan E, Vogelsang G, Krishnan A, Giralt S, Revta C, Carreau NA, Iacobelli M, Carreras E, Ruutu T, Barbui T, Antin JH, Niederwieser D. Hepatic veno-occlusive disease following stem cell transplantation: incidence, clinical course, and outcome. Biol Blood Marrow Transplant. 2010;16:157-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 385] [Cited by in RCA: 428] [Article Influence: 26.8] [Reference Citation Analysis (0)] |
| 9. | Sebagh M, Azoulay D, Roche B, Hoti E, Karam V, Teicher E, Bonhomme-Faivre L, Saliba F, Duclos-Vallée JC, Samuel D. Significance of isolated hepatic veno-occlusive disease/sinusoidal obstruction syndrome after liver transplantation. Liver Transpl. 2011;17:798-808. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Sebagh M, Debette M, Samuel D, Emile JF, Falissard B, Cailliez V, Shouval D, Bismuth H, Reynès M. "Silent" presentation of veno-occlusive disease after liver transplantation as part of the process of cellular rejection with endothelial predilection. Hepatology. 1999;30:1144-1150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 72] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 11. | Campos-Varela I, Castells L, Dopazo C, Pérez-Lafuente M, Allende H, Len O, Llopart L, Vargas V, Charco R. Transjugular intrahepatic portosystemic shunt for the treatment of sinusoidal obstruction syndrome in a liver transplant recipient and review of the literature. Liver Transpl. 2012;18:201-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 12. | Peynircioglu B, Cho KJ, Cwikiel W. Portal hypertension and obstructive jaundice after hepatic interventions: report of two unusual complications. J Vasc Interv Radiol. 2007;18:567-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Duller D, Kniepeiss D, Lackner C, Portugaller RH, Jakoby E, Schaffellner S, Stiegler P, Kahn J, Mueller H, Roller R, Tscheliessnigg KH, Iberer F. Biliary obstruction as a complication of transjugular intrahepatic portosystemic shunt. Liver Transpl. 2009;15:556-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 14. | Paterno F, Khan A, Cavaness K, Asolati M, Campsen J, McKenna GJ, Onaca N, Ruiz R, Trotter J, Klintmalm GB. Malpositioned transjugular intrahepatic portosystemic shunt in the common hepatic duct leading to biliary obstruction and liver transplantation. Liver Transpl. 2011;17:344-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 15. | Karlas T, Hoffmeister A, Fuchs J, Tröltzsch M, Keim V. Bile duct obstruction after transjugular intrahepatic portosystemic shunt implantation. Endoscopy. 2013;45 Suppl 2 UCTN:E47-E48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Meng J, Yang S, Ding W, He C, Wu X. Biliary Obstruction following Transjugular Intrahepatic Portosystemic Shunt Creation in Patients with Variceal Bleeding. J Vasc Interv Radiol. 2016;27:558-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (1)] |
| 17. | Zhang L, Wei B, Wu H, Hu B. Intractable biliary obstruction after TIPS creation treated by magnet-assisted endoscopic biliary-duodenal anastomosis. Surg Endosc. 2021;35:467-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (3)] |