Published online Feb 27, 2022. doi: 10.4254/wjh.v14.i2.442
Peer-review started: June 19, 2021
First decision: July 16, 2021
Revised: October 2, 2021
Accepted: February 10, 2022
Article in press: February 10, 2022
Published online: February 27, 2022
Processing time: 247 Days and 20.8 Hours
The surgical management of bile duct injuries (BDIs) after laparoscopic cholecystectomy (LC) is challenging and the optimal timing of surgery remains unclear. The primary aim of this study was to systematically evaluate the evidence behind the timing of BDI repair after LC in the literature.
To assess timing of surgical repair of BDI and postoperative complications.
The MEDLINE, EMBASE, and The Cochrane Library databases were systematically screened up to August 2021. Risk of bias was assessed via the Newcastle Ottawa scale. The primary outcomes of this review included the timing of BDI repair and postoperative complications.
A total of 439 abstracts were screened, and 24 studies were included with 15609 patients included in this review. Of the 5229 BDIs reported, 4934 (94%) were classified as major injury. Timing of bile duct repair was immediate (14%, n = 705), early (28%, n = 1367), delayed (28%, n = 1367), or late (26%, n = 1286). Standardization of definition for timing of repair was remarkably poor among studies. Definitions for immediate repair ranged from < 24 h to 6 wk after LC while early repair ranged from < 24 h to 12 wk. Likewise, delayed (> 24 h to > 12 wk after LC) and late repair (> 6 wk after LC) showed a broad overlap.
The lack of standardization among studies precludes any conclusive recommendation on optimal timing of BDI repair after LC. This finding indicates an urgent need for a standardized reporting system of BDI repair.
Core Tip: Bile duct injury after laparoscopic cholecystectomy is a relevant iatrogenic complication, which urgently needs attention. In this systematic review, we would like to focus on surgical repair and particularly on the timing of repair. This literature search reveals that the ideal timing of repair is reported remarkable poorly, indicating an urgent need for standardization to better direct treatment of this condition.
- Citation: Kambakamba P, Cremen S, Möckli B, Linecker M. Timing of surgical repair of bile duct injuries after laparoscopic cholecystectomy: A systematic review. World J Hepatol 2022; 14(2): 442-455
- URL: https://www.wjgnet.com/1948-5182/full/v14/i2/442.htm
- DOI: https://dx.doi.org/10.4254/wjh.v14.i2.442
Bile duct injury (BDI) remains the most serious and challenging adverse event after laparoscopic cholecystectomy (LC)[1-5]. If not recognized and treated properly, BDI may lead to severe morbidity and even death of the patient due to biliary peritonitis and sepsis[6-8].
The management of BDI requires multidisciplinary input, demanding close collaboration of surgeons, gastroenterologists, and interventional radiologists[9-13]. Endoscopic or interventional strategies may suffice in the treatment of minor BDI such as cystic stump leakage or partial laceration[14,15]. However, major BDI often requires surgical repair[10,16]. Due to the anatomical complexity of the biliary tree, surgical BDI repair requires a certain expertise in biliary reconstruction and therefore referral to a tertiary center with a division specialized in hepatobiliary (HPB) surgery is strongly recommended[17-21].
Alongside the extent of injury and surgical experience of those managing BDI, it has been suggested that timing of BDI repair may be a significant prognostic factor for clinical outcomes[10,20-24]. To date, the timing of BDI repair is controversial, with discussions in the literature failing to reach clear recommendations. Whereas several groups claim superiority of early BDI repair[25,26], other publications report beneficial outcome measures if BDI repair was delayed[27-29]. Inconsistent methods of reporting and a plethora of distinct definitions for time intervals create difficulties in comparing study outcomes and draw conclusions on the best timing of BDI repair[29,30].
Therefore, the aim of this systematic review was first to investigate the existing literature on outcome after BDI repair according to timing of repair and second to analyze the standardization concerning definitions of timing of BDI repair among studies.
A systemic electronic search for studies published until August 2021 was preformed, which screened different databases such as Medline, EMBASE, and Cochrane. The search strategy was designed to screen for publications reporting timing of BDI repair and outcome according to timing. Related key phrases and MESH subject headings were combined. The initial search was completed by an objective librarian (Supplementary Table 1).
All studies reporting BDI repair after LC, including information on timing and postoperative outcome, were included. Abstracts, reviews, case reports, letters to the editor, and articles only available in non-English language were excluded from analysis. Additionally, studies not reporting postoperative outcome according to timing of BDI repair were excluded.
The following data was extracted: Study period, number of patients, age, number of BDI, classification of BDI, presence of concomitant vascular injury, timing and type of BDI repair, and postoperative outcome after BDI repair. The primary outcome of this study was the definition of timing of BDI repair. Postoperative complications were considered as the secondary outcome.
Two independent reviewers (Kambakamba P and Linecker M) screened all articles and checked the extracted data for accuracy. The Newcastle-Ottawa scale was used to assess included papers for risk of bias[31,32].
Variables are described as the median and interquartile range (IQR), unless specified differently. The Mann-Whitney U Test or the one-way ANOVA tests was used.
Due to the fact that point estimates from most of the studies (e.g., odds ratios or risk ratios for binary outcomes, or mean difference for quantitative outcomes including 95% confidence interval) were missed, a statistical analysis by pooling the data according to the meta-analysis methods could not be performed. Significance was set at P = 0.05 and statistical trend was defined as P ≤ 0.1. Statistical analyses were performed with the software package SPSS 22 (SPSS Inc., Chicago, Ill) and Graph Pad Prism Software Version 6.0.
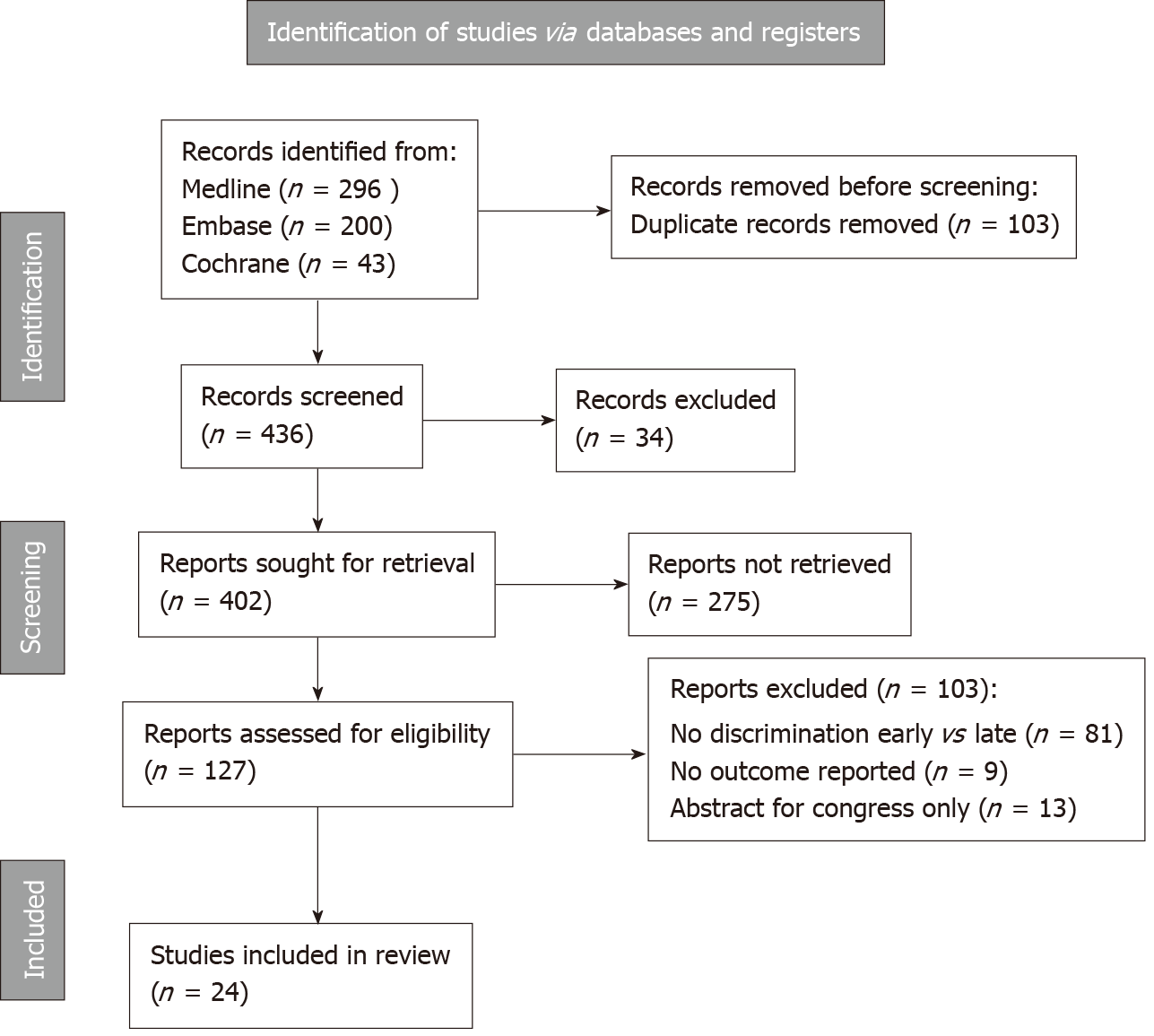
From all the databases searched, 539 studies were identified through screening of Medline (n = 296), EMBASE (n = 200), and Cochrane (n = 43, Figure 1). After excluding duplicates, a total of 539 studies remained for abstract reviewing. Of these, 275 studies were excluded because of reporting of interventional management of BDI only (i.e., endoscopy), or representing review articles or case series < 10 patients. Finally, after critical reading of 127 articles, 24 studies were considered for the final analysis (Figure 1)[18,20,25-28,33-51].
All 24 studies were assessed for the criteria selection (case definition, representativeness of cases, selection of controls, and definition of controls), comparability (age and sex, and other factors), and exposure (ascertainment of exposure, follow-up, and adequacy of follow-up; Supplementary Figure 1).
A total of 24 studies met the inclusion criteria and reported sufficient information on timing of surgical BDI repair and postoperative outcome after BDI repair. Overall, 15609 patients undergoing cholecystectomy were enrolled. Out of 5229 described injuries of the bile duct, 94% (n = 4934) were classified as major BDI with the need for surgical repair (Table 1).
| Ref. | Study period | Study population (n) | Major BDI (n) |
| de Reuver et al[20], 2007 | 1991- 2005 | 500 | 151 (30) |
| Mushtaq et al[35], 2020 | 1974- 2004 | 5000 | 11 (100) |
| Goykhman et al[28], 2008 | 2002- 2007 | 29 | 29 (100) |
| Silva et al[34], 2008 | - | 22 | 22 (100) |
| Stewart et al[18], 2009 | - | 307 | 307(100) |
| Sahajpal et al[42], 2010 | 1992-2007 | 69 | 69 (100) |
| Huang et al[25], 2011 | 1984- 2009 | 282 | 41 (15) |
| Perera et al[26], 2011 | 1991- 2007 | 200 | 157 (79) |
| Barauskas et al[41], 2012 | 2000- 2007 | 4438 | 23 (53) |
| Iannelli et al[27], 2013 | - | 640 | 543 (85) |
| Lubikowski et al[38], 2012 | 2002- 2011 | 300 (TPL) | 5 (100, TPL) |
| Parrilla et al[37], 2014 | 1987- 2010 | 27 | 27 (100, TPL) |
| Stilling et al[44], 2015 | 1995-2010 | 139 | 139 (100) |
| Arora et al[46], 2015 | 2000- 2010 | 10 | 10 (100) |
| Perini et al[36], 2015 | 2000 – 2011 | 148 | 9 (16, LR) |
| Sulpice et al[33], 2014 | 1992- 2010 | 60 | 38 (63) |
| Felekouras et al[40], 2015 | 1991- 2011 | 67 | 67 (100) |
| Kirks et al[45], 2016 | 2008- 2005 | 61 | 61 (100) |
| Dominguez-Rosado et al[43], 2016 | 1989- 2014 | 699 | 614 (88) |
| E-AHPBA[47], 2019 | 2000-2016 | 913 | 913 (100) |
| Battal et al[48], 2019 | 2012-2017 | 13 | 13 (100) |
| Sweigert et al[49], 2021 | 2006-2015 | 1168 | 1168 (100) |
| El Nakeeb et al[50], 2021 | 2015-2020 | 412 | 412 (100) |
| Anand et al[51], 2021 | 2013- 2020 | 105 | 105 (100) |
| Total | 15.609 | 4934 |
Three different classifications were used to characterize the type of major BDI: The Strasberg classification, the Bismuth classification, and the Stewart Way System. Fifteen studies, accounting for 49% (n = 2440)[26,33,34,36-43,45-47,49,50] of BDIs, used the Strasberg classification system, three studies, including 8% (n = 395)[43,47,51] of BDIs, used the Bismuth classification, and one study, reporting 6% (n = 307)[18] of BDIs, used the Stewart Way System (Table 2). Five studies, including 36% (n = 17924)[25,27,28,35,49] of patients, did not identify which classification system was used. Of note, one study including 12 patients used both the Bismuth and the Strasberg classification[39]. Concomitant vascular injury was reported in 4% (n = 222)[28,33,34,36,37,43-45,47] of included patients.
| Ref. | BDI (n) | Classification | Bismuth classification | Strasberg classification | Vascular injury | ||||||||||||
| I | II | III | IV | V | A | B | C | D | E1 | E2 | E3 | E4 | E5 | ||||
| de Reuver et al[20] | 151 | Bismuth | 37 | 37 | 37 | - | - | - | - | - | - | - | - | - | - | - | - |
| Mushtaq et al[35] | 11 | None | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Goykhman et al[28] | 29 | None | - | - | - | - | - | - | - | - | - | - | - | - | - | 5 | |
| Silva et al[34] | 22 | Strasberg | - | - | - | - | - | - | 1 | - | 1 | 1 | 7 | 7 | 3 | 2 | 2 |
| Stewart et al[18] | 307 | Stewart | 16 | 72 | 187 | 32 | - | - | - | ||||||||
| Sahajpal et al[42] | 69 | Strasberg | 1 | - | - | 2 | 22 | 16 | 22 | 4 | 2 | - | |||||
| Huang et al[25] | 41 | None | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Perera et al[26] | 157 | Strasberg | - | - | - | - | - | 19 | 2 | 9 | 26 | 20 | 65 | 37 | 19 | 3 | - |
| Barauskas et al[41] | 23 | Strasberg | - | - | - | - | - | (4) | - | - | (17) | 1 | 21 | - | 1 | - | - |
| Iannelli et al[27] | 543 | None | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Lubikowski et al[38] | 5 | Strasberg | - | - | - | - | - | 1 | 2 | - | - | - | 1 | 1 | - | - | - |
| Parrilla et al[37] | 27 | Strasberg | - | - | - | - | - | - | - | - | - | - | 4 | 11 | 12 | - | 7 |
| Stilling et al[44] | 139 | Bismuth | 49 | 49 | 35 | 26 | |||||||||||
| Arora et al[46] | 10 | Strasberg | - | 1 | 3 | 5 | 1 | 0 | |||||||||
| Perini et al[36] | 9 | Strasberg | - | - | - | - | - | - | - | - | - | - | - | 2 | 7 | - | 9 |
| Sulpice et al[33] | 38 | Strasberg | - | - | - | - | 6 | 14 | 6 | 9 | 3 | 10 | |||||
| Felekouras et al[40] | 67 | Strasberg | 7 | - | 4 | 18 | 10 | 26 | 22 | 4 | 1 | - | |||||
| Kirks et al[45] | 61 | Strasberg | 2 | 1 | 7 | 4 | 10 | 16 | 11 | 6 | 1 | 12 | |||||
| Dominguez-Rosado et al[43] | 614 | Strasberg | 448 | 166 | 22 | ||||||||||||
| E-AHPBA[47] | 913 | Strasberg | 757 | 126 | |||||||||||||
| Battal et al[48] | 13 | Strasberg | 3 | 4 | 1 | 1 | |||||||||||
| Sweigert et al[49] | 1168 | None | |||||||||||||||
| El Nakeeb et al[50] | 412 | Strasberg | 59 | 234 | 80 | 33 | 6 | ||||||||||
| Anand et al[51] | 105 | Bismuth | 10 | 37 | 43 | 3 | |||||||||||
| TOTAL | 4934 | 112 | 195 | 267 | 67 | 0 | 34 | 6 | 20 | 71 | 134 | 1613 | 204 | 265 | 19 | 222 | |
Details on timing of surgical BDI repair were available in 98% (n = 4879) of analyzed major BDIs. Among all studies, the timing of repair was categorized as “immediate”, “early”, “delayed”, or “late“. In the literature, all four strategies were used in comparable frequencies: 14% (n = 705) of BDI repairs were classified as immediate and 28% (n = 1367) as early, whereas delayed and late repair represented 28% (n = 1364) and 26 % (n = 1286) of BDI repairs, respectively (Table 3).
| Ref. | Surgical repair (n) | Definition IR | IR (n) | Definition ER | ER (n) | Defintion DR | DR (n) | Definition LR | LR (n) | In favor of |
| de Reuver et al[20] | 151 | < 6 w | 15 (10) | - | - | > 6 w | 96 (64) | > 6 w (R) | 40 (27) | - |
| Mushtaq et al[35] | 11 | Initial surgery | 11 (100) | - | - | - | - | - | - | - |
| Goykhman et al[28] | 29 | Initial surgery | 14 (48) | - | - | 24-72 h | 5 (17) | > 8 w | 10 (35) | Delay |
| Silva et al[34] | 22 | Initial surgery | 22 (100) | - | - | - | - | |||
| Stewart et al[18] | 300 | Initial surgery | 163 (53) | 1-2 w | 61 (20) | 3-6 w | 33 (11) | > 6 w | 43 (14) | |
| Sahajpal et al[42] | 69 | ≤ 3 d | 13 (19) | 3d- 6w | 34 (49) | > 6 w | 22 (32) | Immidiate or delay | ||
| Huang et al[25] | 41 | - | - | < 14 d | 19 (46) | 14-24 w | 22 (54) | - | - | Early |
| Perera et al[26] | 112 | Initial surgery | 28 (18) | < 21 d | 43 (27) | > 21 d | 41 (26) | - | - | Early |
| Barauskas et al[41] | 23 | Initial surgery | 3 (13) | - | 7 (30) | - | 13 (57) | - | - | - |
| Iannelli et al[27] | 543 | Initial surgery | 194 (35) | < 45 d | 216 (39) | > 45 d | 133 (24) | - | - | Delay |
| Lubikowski et al[38] | 5 (TPL) | - | - | - | - | - | - | - | 5 (100) | - |
| Parrilla et al[37] | 27 (TPL) | - | - | - | - | - | - | - | 27 (100) | - |
| Stilling et al[44] | 139 | - | ||||||||
| Arora et al[46] | 10 | ≤ 3 d | 10 (100) | |||||||
| Perini et al[36] | 9 (LR) | - | - | - | - | - | - | - | 9 (100) | - |
| Sulpice et al[33] | 35 | < 3 d | 15 (43) | 3 d–6 w | 7 (20) | > 6 w | 4 (11) | > 24 mo | 9 (26) | - |
| Felekouras et al[40] | 67 | < 14 d | 34 (51) | 2-12 w | 11 (16) | > 12 w | 22 (33) | - | - | - |
| Kirks et al[45] | 61 | ≤ 2 d | 27 (44) | > 2 d | 34 (56) | Equal | ||||
| Dominguez-Rosado et al[43] | 614 | < 7 d | 61 (10) | 1-6 w | 152 (26) | > 6 w | 374 (63) | Early or late | ||
| E-AHPBA[47] | 913 | < 7 d | 339 (37) | 1-6 w | 261 (28.6) | 6 w-6 mo | 313 (34) | Equal | ||
| Battal et al[48] | 13 | < 3 d | 13 (100) | |||||||
| Sweigert et al[49] | 1168 | < 3 d | 569 (48) | 4 d-6 w | 439 (38) | > 6 w | 169 (15) | Early or late | ||
| El Nakeeb et al[50] | 412 | < 3 d | 156 (38) | 4-6 w | 75 (18) | > 6 w | 181 (44) | Early or delayed | ||
| Anand et al[51] | 105 | - | - | < 12 w | 21 (20) | - | - | > 12 w | 84 (80) | NS |
| TOTAL | 4879 | 705 (14) | 1367 (28) | 1364 (28) | 1286 (26) |
The most common type of surgery was biliodigestive reconstruction with a hepaticojejunostomy (median, 95%, IQR: 88%-100%; Table 4). Additionally, the late BDI repair group included nine (0.2%) cases of hepatic resections and 32 (0.6%) patients who were treated by liver transplantation.
| Timing of repair | Immediate n = 705 | Early n = 1378 | Delayed n = 1364 | Late n = 1286 | P | |
| Type of surgery | ||||||
| HJS | 89 (72-100) | 77 (75-91) | 100 (96-100) | 95 (91-100) | 0.132 | |
| End-to-end | 32 (19-57) | 21 (13-47) | 3 (2-10) | - | 0.265 | |
| Complications | 34 (21-41) | 21 (20-29) | 25 (16-36) | 28 (19-38) | 0.789 | |
| Bile leak | 21 (12-36) | 7 (5-12) | 12 (0-24) | 5 (5-14) | 0.653 | |
| Wound infection | 23 (12-35) | - | 10 (7- 28) | 9 (7-12) | 0.456 | |
| Liver dysfunction | 8 (5-11) | - | - | - | - | |
| Cholangitis | 11 (10-31) | 11 (7-25) | 13 (8- 59) | 10 (4-18) | 0.684 | |
| Jaundice | 9 (4-14) | - | - | - | - | |
| Redo HJS | 33 (3-43) | 8 (3-31) | 20 (10-31) | 3 (1-8) | 0.642 | |
| Intervention | 16 (14- 17) | 5 (2-12) | 24 (23- 25) | - | 0.035 | |
| Stricture | 17 (13-41) | 29 (14-39) | 25 (15- 62) | 13 (11- 19) | 0.821 | |
| Time to stricture | 11 (4-29) | 50 (12-89) | 14 (14-30) | - | 0.642 | |
| Mortality | 1 (0-5) | 2 (0-1) | 3 (1-5) | 0 | 0.832 | |
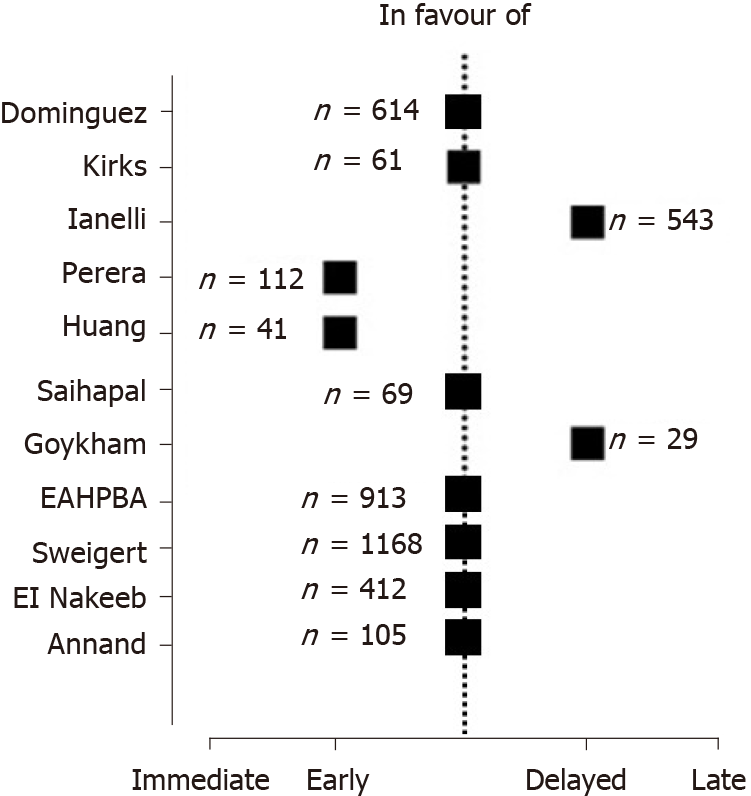
Thirteen studies, including 94% (n = 4643) of BDI repairs, defined postoperative outcome according to various timing groups of BDI repair, which included immediate vs early vs delayed in four studies (n = 745); immediate vs delayed vs late in four (n = 661); immediate vs early vs delayed vs late in three (n = 335); early vs delayed in three (n = 335); early vs delay vs late in three (n = 2695); and early vs late in one (n = 105) (Table 3). Overall, 11 studies (n = 4006) proposed a recommendation for timing of BDI repair. Two manuscripts were in favor of delayed (n = 572, 12%)[27,28], while two other groups (n = 153, 3%)[25, 26] recommended early repair of BDI (Figure 2). The other eight studies (n = 3281, 66%) postulating a recommendation for timing found equal results for early or delayed BDI repair[42,43,45].
Median overall morbidity after bile duct repair was 28% (IQR: 19-38) and did not vary significantly between the different timings of BDI repair (P = 0.789; Table 4). Further, mortality was low and was not different among groups (P = 0.832). A detailed list of reported complications can be found in Table 5.
| Timing of repair | ≤ 14 d (n = 1757) | > 14 d (n = 2031) | P |
| Type of surgery | |||
| HJS | 100 (73-100) | 100 (68-100) | 0.842 |
| End-to-end | 0 (0-27) | 0 (0-5) | 0.352 |
| Complications | 33 (21-41) | 22 (18-25) | 0.085 |
| Bile leak | 11 (5-21) | 6 (0-12) | 0.453 |
| Wound infection | 5 (0-14) | 9 (6-18) | 0.593 |
| Abnormal liver function | 11 (0-21) | 10 | - |
| Cholangitis | 11 (10-35) | 9 (9-10) | 0.348 |
| Jaundice | 13 (5-21) | - | - |
| Redo HJS | 23 (4-42) | 0 | - |
| Intervention | 16 (14-18) | 17 | - |
| Stricture | 18 (12-43) | 13 (5-23) | 0.352 |
| Time to stricture (mo) | 17 (10-62) | 3 | - |
| Mortality | 2 (0-3) | 4 (3-5) | 0.203 |
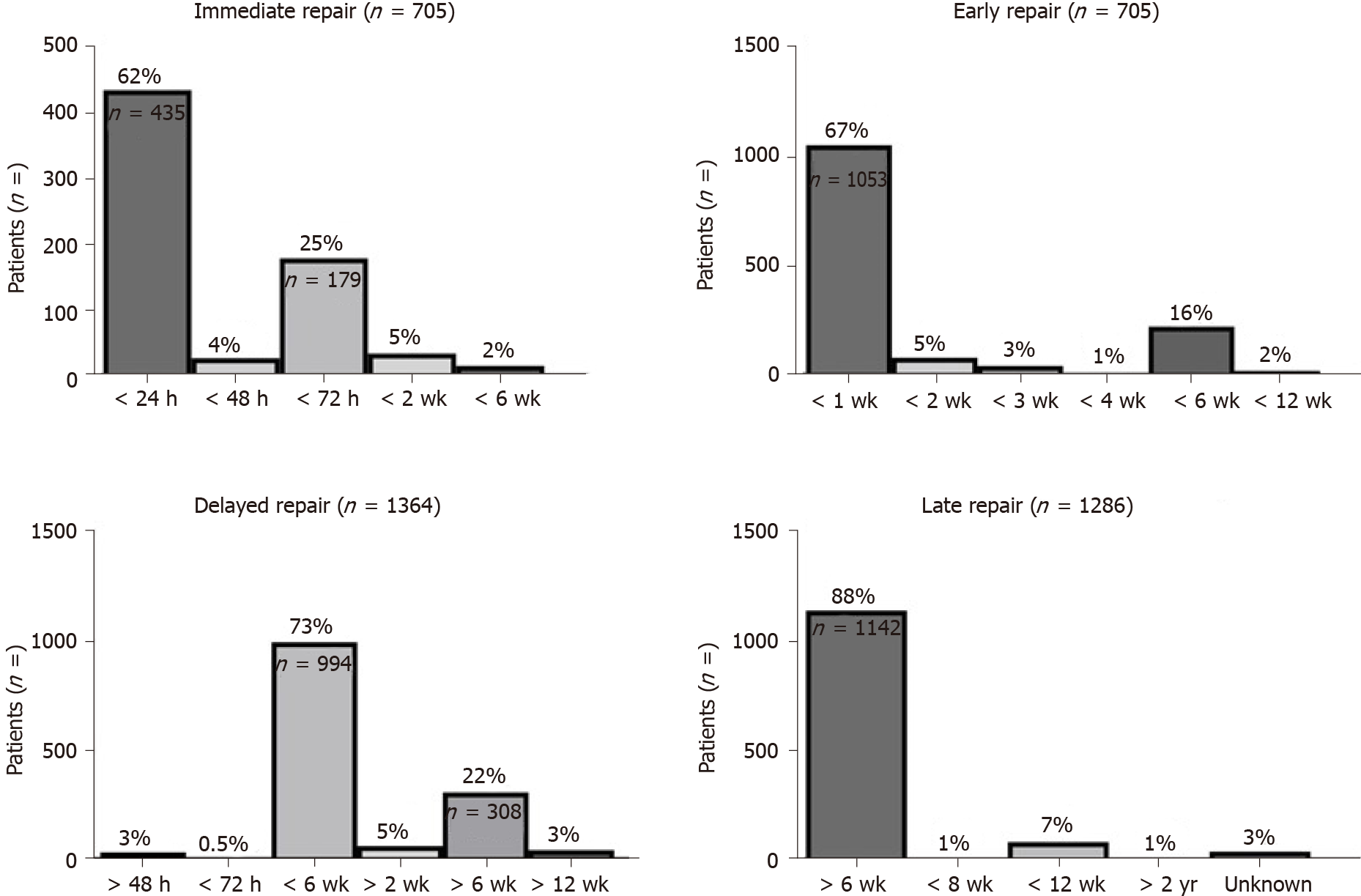
Among 14 studies, we found 14 different definitions of immediate repair (n = 705; Figure 3), ranging from a surgical repair during initial LC (n = 435/705, 62%) to BDI repair within 2 d (n = 27/705, 4%), 3 d (n = 179/705, 7%), 2 wk (n = 34/705, 5%), or within 6 wk (n = 15/705, 2%) after cholecystectomy (Figure 3). Six various definitions for early BDI repair (n = 1367) were provided. Early repair was described as surgery within 1 wk (n = 1053/1367, 67%), 2 wk (n = 80/1367, 5%), 3 wk (n = 43/1367, 3%), 4 wk (n = 12/1367, 1%), 6 wk (n = 223/1367, 16%), or 12 wk (n = 32/1367, 2%). Similar, definitions of delayed (n = 1364) and late repair (n = 1286) suffered from inconsistent reporting and were described in six and three distinct ways, respectively. The term “delayed” ranged from after 2 d (n = 34/1364, 3%) to within 3 d (n = 5/1364, 0.5%) to within 6 wk (n = 994/1364, 73%), to a minimum delay after cholecystectomy of 2 wk (n = 22/1364, 5%), 6 wk (n = 308/1364, 22%), or 12 wk (n = 22/1364, 3%). Late BDI repairs (n = 1286) were defined as BDI repair 6 wk (n = 1142/1286, 88%), 8 wk (n = 10/1286, 1%), 12 wk (n = 84/1286, 7%), or 2 years (n = 9/1286, 1%) after LC. In 3% (n = 41/1286) of patients undergoing late repair, the time interval was not further specified at all.
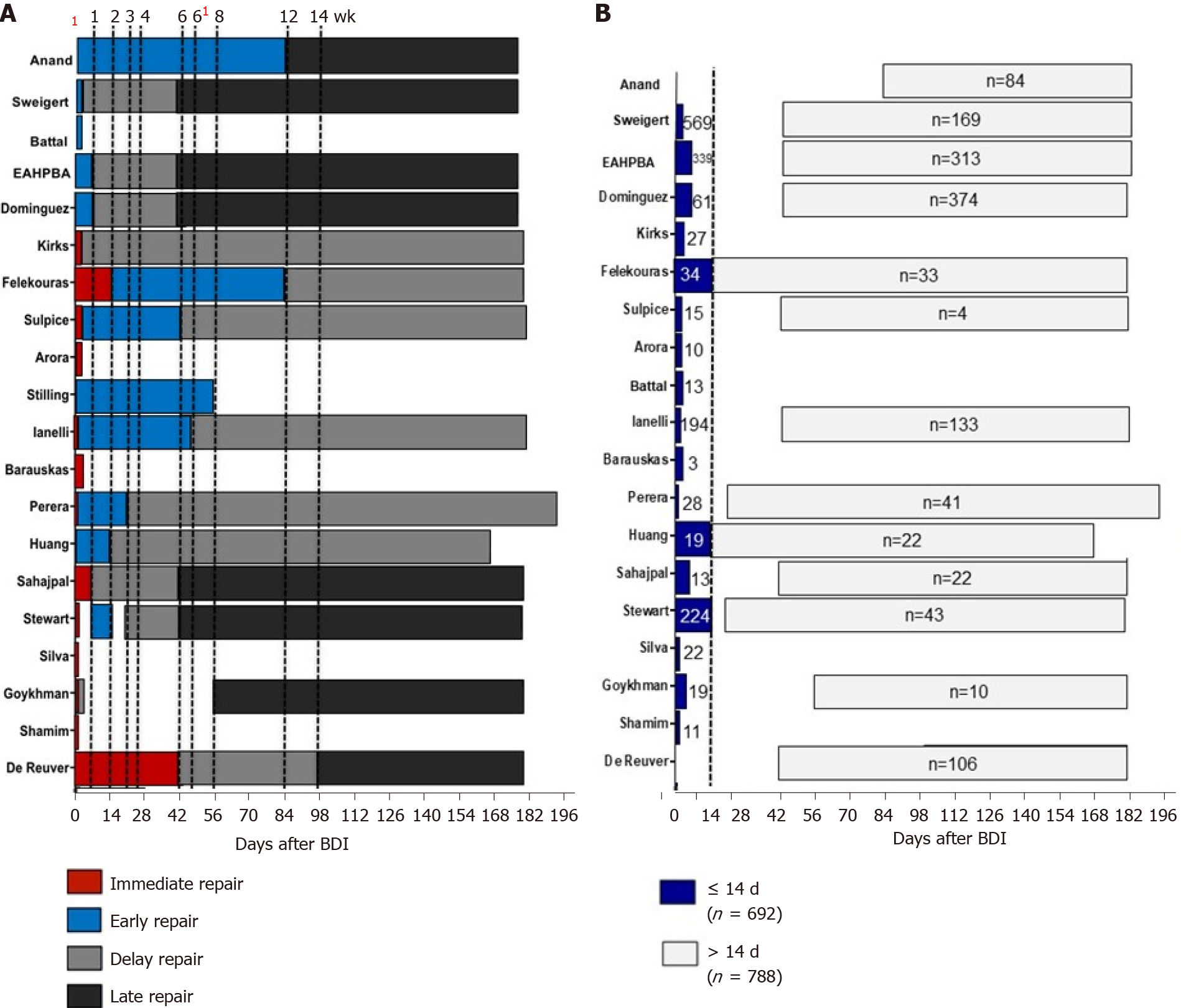
As described above, the standardization of timing of repair was remarkably poor among[8,29] studies. Based on the included literature, most commonly used definitions for immediate and early BDI repair were < 24 h and < 1 wk after (Figure 3). Both delayed and late repairs were equally described as BDI repair 6 wk after index surgery in the majority of reported cases (Figure 3). Overall, the lack of standardized reporting leads to a broad overlap of time intervals (Figure 4A), which precludes any conclusive comparison of different studies.
Nonetheless, the provided data allowed the formation of two groups without being confronted by an overlap. In an attempt to standardize the population according to timing of BDI repair, a cut off of 14 d was proposed (Figure 4B). This subgroup analysis revealed increased complications for a BDI repair within 14 d (n = 1757)[2,11,15,16,20,27,29,30,37,38,42,43,45-49] when compared to surgical repair after this interval (n = 2031)[18,20,25-28,33,40,42,43,47,49,51]. Nevertheless, this difference did not reach statistical significance, implicating that outcome is not dependent on timing of repair only. Therefore, based on the present literature, no recommendation can be given on whether early or delayed BDI repair should be preferred. Moreover, there are many inconsistencies in the reporting of timing intervals for BDI repair following LC in the identified literature.
The analysis of this systematical review revealed that standardization of definitions for timing of repair is remarkably poor among studies. This lack of standardized reporting precludes any conclusive recommendation on optimal timing of BDI repair after LC and claims for a uniform reporting system.
Despite single reports postulating reduced occurrence of BDI, it remains a major concern after LC[8,29]. The repair of major BDI requires exact preoperative characterization of lesions and sufficient expertise in HPB surgery[18,26]. As a result, there are numerous studies that investigate factors influencing outcome following biliary reconstruction for BDI[11,18,29]. Both patient-associated factors, such as septic complications and complexity of BDI, and surgical technique are known prognostic factors for outcome of BDI repair[10,11,18]. Additionally, several authors attach great importance to the optimal timing of surgical BDI repair[23-25,27,29,40]. Whereas immediate repair requires early identification of the injury and potentially shortens patient’s cumulative hospital stay, delayed reconstruction may provide optimal planning and enable the eradication of intra-abdominal infection prior to surgery. Both strategies are equally supported and opposed by various groups and therefore a conclusive recommendation on timing of BDI repair remains unclear[25-28,42,43,45].
Inconsistent methods of reporting the timing of BDI is a major reason for these continued inconsistencies in recommendations[30]. Substantial variability in presentation of data makes comparison of results difficult and precludes a synoptic statement. In line with our findings, a recent study by the group of Strasberg highlighted the weaknesses of irregular formats of observational studies in the field of BDI repair[30]. Likewise, our systematic review found a multitude of definitions for timing of BDI repair in the literature, resulting in a broad overlap of time intervals among studies. As a result, BDI repair may be considered as “early” in one study, whereas the same time interval may be classified as “delayed” or even “late” in another paper. This lack of standardized definition for BDI timing repair means that a conclusion on superiority of either one of the strategies cannot be reached. Hence, two studies included in this review proposed the early[25,26], while another two recommended the delayed[27,28] approach as treatment of choice. This goes in line with the findings of two recent meta-analyses that BDI repair should be undertaken either early or in a delayed fashion after 6 wk, whereas the time frame between 2-6 wk seems to be associated with increased morbidity[23,24].
In order to overcome this inconsistency in reporting of timing, the population was divided into two subgroups based on BDI repair within 14 d and after 14 d. Admittedly, the subgroup analysis failed to reveal a significant difference for outcome. This result emphasizes that outcomes after BDI repair are influenced by multiple variables and not just by timing of repair. Likewise, a multivariate analysis including 307 major BDIs concluded that timing of BDI repair plays a subordinate prognostic role for outcome[18]. In contrast, sepsis control, accurate characterization of the BDI, and surgical experience seem to be the major factors influencing the postoperative course.
Many of the studies included in this review were retrospective, which accounts for a major limitation of this systematic review. The retrospective study design does not allow conclusions on patients’ condition prior to surgery and the reason for surgeon’s choice for one strategy or the other. Surgeons’ decision was likely driven by extent of BDI, concomitant vascular injury, and inflammatory status than by standardized protocols. Subsequently, a retrospective comparison of early and delayed BDI repair group leads to clustering of two fundamentally heterogeneous populations. Nevertheless, the low incidence and the unpredictable course of BDI complicate the design of a prospective randomized control trial.
Likewise, the value of the attempt to standardize the groups according to a BDI repair within 14 d or more than 14 d is diminished by the above-mentioned limitations in data reporting. Still, this allowed a more precise pooling of patients undergoing BDI. In line with other publications, timing alone did not predict outcome in this subgroup analysis. Nevertheless, caution should be taken in interpreting these results based on the quality of provided data and heterogeneity of populations.
In this context, original raw data of the included studies was not available and all analyses were based on provided medians. Therefore, the analysis was limited by data quality, which precluded pooling the data according to the methods of a meta-analysis. However, this study has certain strengths, including the systematical character with providing a comprehensive review of studies declaring outcome according to timing of bile duct repair.
In conclusion, based on clinical practice, it is assumable that immediate BDI repair is reasonable if detected intraoperatively and sepsis control should be guaranteed before delayed BDI repair. Nevertheless, only standardized reporting can help to answer the ongoing debate of influence of timing on outcome and provide solid fundament for a recommendation. Therefore, based on the findings of this review, a consensus in the field of timing of BDI repair is urgently needed.
Bile duct injuries (BDIs) are an important topic for the practicing hepatobiliary (HPB) surgeon. While it is widely agreed that most major BDIs after laparoscopic cholecystectomy (LC) should undergo surgical repair, the timing of repair is still controversially discussed in the literature.
Our research motivation was: (1) To bring clarity into the terms "immediate", "early", "delayed", and "late" repair; and (2) to assess postoperative complications.
The objective of this study was to assess timing of bile duct repair after BDI and postoperative complications.
A systematic review of the literature was performed using the databases MEDLINE, EMBASE, and The Cochrane Library. These databases were systematically screened up to August 2021. Bias assessment was performed using the Newcastle Ottawa scale.
A total of 439 abstracts were screened, and 24 studies were included with 15609 patients included in this review. Of the 5229 BDIs reported, 4934 (94%) were classified as major injury. Timing of bile duct repair was immediate (14%, n = 705), early (28%, n = 1367), delayed (28%, n = 1367), or late (26%, n = 1286). Standardization of definition for timing of repair was remarkably poor among studies.
The lack of standardization among studies precludes any conclusive recommendation on optimal timing of BDI repair after LC. This finding indicates an urgent need for a standardized reporting system of BDI repair.
Future perspectives include the establishment of a clear definition for the terms "immediate", "early", "delayed", and "late" repair. Only such a definition can make comparisons of study outcomes possible.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: IHPBA; E-AHPBA
Specialty type: Surgery
Country/Territory of origin: Germany
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hori T, Ozair A S-Editor: Liu M L-Editor: Wang TQ P-Editor: Liu M
| 1. | Strasberg SM. Error traps and vasculo-biliary injury in laparoscopic and open cholecystectomy. J Hepatobiliary Pancreat Surg. 2008;15:284-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 66] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 2. | Strasberg SM. Avoidance of biliary injury during LC. J Hepatobiliary Pancreat Surg. 2002;9:543-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 131] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 3. | Mercado MA, Domínguez I. Classification and management of bile duct injuries. World J Gastrointest Surg. 2011;3:43-48. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 56] [Cited by in RCA: 54] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 4. | Adamsen S, Hansen OH, Funch-Jensen P, Schulze S, Stage JG, Wara P. Bile duct injury during LC: a prospective nationwide series. J Am Coll Surg. 1997;184:571-578. [PubMed] |
| 5. | Hori T, Oike F, Furuyama H, Machimoto T, Kadokawa Y, Hata T, Kato S, Yasukawa D, Aisu Y, Sasaki M, Kimura Y, Takamatsu Y, Naito M, Nakauchi M, Tanaka T, Gunji D, Nakamura K, Sato K, Mizuno M, Iida T, Yagi S, Uemoto S, Yoshimura T. Protocol for LC: Is it rocket science? World J Gastroenterol. 2016;22:10287-10303. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 19] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (1)] |
| 6. | Flum DR, Cheadle A, Prela C, Dellinger EP, Chan L. Bile duct injury during cholecystectomy and survival in medicare beneficiaries. JAMA. 2003;290:2168-2173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 321] [Cited by in RCA: 316] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 7. | Nuzzo G, Giuliante F, Giovannini I, Ardito F, D'Acapito F, Vellone M, Murazio M, Capelli G. Bile duct injury during LC: results of an Italian national survey on 56 591 cholecystectomies. Arch Surg. 2005;140:986-992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 326] [Cited by in RCA: 262] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 8. | Archer SB, Brown DW, Smith CD, Branum GD, Hunter JG. Bile duct injury during LC: results of a national survey. Ann Surg. 2001;234:549-58; discussion 558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 242] [Cited by in RCA: 230] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 9. | Thompson CM, Saad NE, Quazi RR, Darcy MD, Picus DD, Menias CO. Management of iatrogenic bile duct injuries: role of the interventional radiologist. Radiographics. 2013;33:117-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 61] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 10. | Sicklick JK, Camp MS, Lillemoe KD, Melton GB, Yeo CJ, Campbell KA, Talamini MA, Pitt HA, Coleman J, Sauter PA, Cameron JL. Surgical management of bile duct injuries sustained during LC: perioperative results in 200 patients. Ann Surg. 2005;241:786-92; discussion 793. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 326] [Cited by in RCA: 294] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 11. | Pitt HA, Sherman S, Johnson MS, Hollenbeck AN, Lee J, Daum MR, Lillemoe KD, Lehman GA. Improved outcomes of bile duct injuries in the 21st century. Ann Surg. 2013;258:490-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 59] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 12. | de'Angelis N, Catena F, Memeo R, Coccolini F, Martínez-Pérez A, Romeo OM, De Simone B, Di Saverio S, Brustia R, Rhaiem R, Piardi T, Conticchio M, Marchegiani F, Beghdadi N, Abu-Zidan FM, Alikhanov R, Allard MA, Allievi N, Amaddeo G, Ansaloni L, Andersson R, Andolfi E, Azfar M, Bala M, Benkabbou A, Ben-Ishay O, Bianchi G, Biffl WL, Brunetti F, Carra MC, Casanova D, Celentano V, Ceresoli M, Chiara O, Cimbanassi S, Bini R, Coimbra R, Luigi de'Angelis G, Decembrino F, De Palma A, de Reuver PR, Domingo C, Cotsoglou C, Ferrero A, Fraga GP, Gaiani F, Gheza F, Gurrado A, Harrison E, Henriquez A, Hofmeyr S, Iadarola R, Kashuk JL, Kianmanesh R, Kirkpatrick AW, Kluger Y, Landi F, Langella S, Lapointe R, Le Roy B, Luciani A, Machado F, Maggi U, Maier RV, Mefire AC, Hiramatsu K, Ordoñez C, Patrizi F, Planells M, Peitzman AB, Pekolj J, Perdigao F, Pereira BM, Pessaux P, Pisano M, Puyana JC, Rizoli S, Portigliotti L, Romito R, Sakakushev B, Sanei B, Scatton O, Serradilla-Martin M, Schneck AS, Sissoko ML, Sobhani I, Ten Broek RP, Testini M, Valinas R, Veloudis G, Vitali GC, Weber D, Zorcolo L, Giuliante F, Gavriilidis P, Fuks D, Sommacale D. 2020 WSES guidelines for the detection and management of bile duct injury during cholecystectomy. World J Emerg Surg. 2021;16:30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 139] [Cited by in RCA: 106] [Article Influence: 26.5] [Reference Citation Analysis (0)] |
| 13. | Khadra H, Johnson H, Crowther J, McClaren P, Darden M, Parker G, Buell JF. Bile duct injury repairs: Progressive outcomes in a tertiary referral center. Surgery. 2019;166:698-702. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 14. | Davids PH, Rauws EA, Tytgat GN, Huibregtse K. Postoperative bile leakage: endoscopic management. Gut. 1992;33:1118-1122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 88] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 15. | Kim KH, Kim TN. Endoscopic management of bile leakage after cholecystectomy: a single-center experience for 12 years. Clin Endosc. 2014;47:248-253. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 36] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 16. | Rauws EA, Gouma DJ. Endoscopic and surgical management of bile duct injury after LC. Best Pract Res Clin Gastroenterol. 2004;18:829-846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 25] [Reference Citation Analysis (0)] |
| 17. | Davidoff AM, Pappas TN, Murray EA, Hilleren DJ, Johnson RD, Baker ME, Newman GE, Cotton PB, Meyers WC. Mechanisms of major biliary injury during LC. Ann Surg. 1992;215:196-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 368] [Cited by in RCA: 335] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 18. | Stewart L, Way LW. Laparoscopic bile duct injuries: timing of surgical repair does not influence success rate. A multivariate analysis of factors influencing surgical outcomes. HPB (Oxford). 2009;11:516-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 73] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 19. | Stewart L, Way LW. Bile duct injuries during LC. Factors that influence the results of treatment. Arch Surg. 1995;130:1123-1128; discussion 1129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 264] [Cited by in RCA: 224] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 20. | de Reuver PR, Grossmann I, Busch OR, Obertop H, van Gulik TM, Gouma DJ. Referral pattern and timing of repair are risk factors for complications after reconstructive surgery for bile duct injury. Ann Surg. 2007;245:763-770. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 107] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 21. | Mercado MA. Early versus late repair of bile duct injuries. Surg Endosc. 2006;20:1644-1647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 22. | Thomson BN, Parks RW, Madhavan KK, Wigmore SJ, Garden OJ. Early specialist repair of biliary injury. Br J Surg. 2006;93:216-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 73] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 23. | Wang X, Yu WL, Fu XH, Zhu B, Zhao T, Zhang YJ. Early Versus Delayed Surgical Repair and Referral for Patients With Bile Duct Injury: A Systematic Review and Meta-analysis. Ann Surg. 2020;271:449-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 24. | Schreuder AM, Nunez Vas BC, Booij KAC, van Dieren S, Besselink MG, Busch OR, van Gulik TM. Optimal timing for surgical reconstruction of bile duct injury: meta-analysis. BJS Open. 2020;4:776-786. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (1)] |
| 25. | Huang Q, Shao F, Qiu LJ, Wang C. Early vs. delayed repair of isolated segmental, sectoral and right hepatic bile duct injuries. Hepatogastroenterology. 2011;58:725-728. [PubMed] |
| 26. | Perera MT, Silva MA, Hegab B, Muralidharan V, Bramhall SR, Mayer AD, Buckels JA, Mirza DF. Specialist early and immediate repair of post-LC bile duct injuries is associated with an improved long-term outcome. Ann Surg. 2011;253:553-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 78] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 27. | Iannelli A, Paineau J, Hamy A, Schneck AS, Schaaf C, Gugenheim J. Primary versus delayed repair for bile duct injuries sustained during cholecystectomy: results of a survey of the Association Francaise de Chirurgie. HPB (Oxford). 2013;15:611-616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 49] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 28. | Goykhman Y, Kory I, Small R, Kessler A, Klausner JM, Nakache R, Ben-Haim M. Long-term outcome and risk factors of failure after bile duct injury repair. J Gastrointest Surg. 2008;12:1412-1417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 29. | Kapoor VK. Bile duct injury repair —— earlier is not better. Front Med. 2015;9:508-511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 30. | Cho JY, Jaeger AR, Sanford DE, Fields RC, Strasberg SM. Proposal for Standardized Tabular Reporting of Observational Surgical Studies Illustrated in a Study on Primary Repair of Bile Duct Injuries. J Am Coll Surg. 2015;221:678-688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 31. | Cook DA, Reed DA. Appraising the quality of medical education research methods: the Medical Education Research Study Quality Instrument and the Newcastle-Ottawa Scale-Education. Acad Med. 2015;90:1067-1076. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 361] [Cited by in RCA: 525] [Article Influence: 52.5] [Reference Citation Analysis (0)] |
| 32. | Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8858] [Cited by in RCA: 12669] [Article Influence: 844.6] [Reference Citation Analysis (0)] |
| 33. | Sulpice L, Garnier S, Rayar M, Meunier B, Boudjema K. Biliary cirrhosis and sepsis are two risk factors of failure after surgical repair of major bile duct injury post-laparoscopic cholecystectomy. Langenbecks Arch Surg. 2014;399:601-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 34. | Silva MA, Coldham C, Mayer AD, Bramhall SR, Buckels JA, Mirza DF. Specialist outreach service for on-table repair of iatrogenic bile duct injuries--a new kind of 'travelling surgeon'. Ann R Coll Surg Engl. 2008;90:243-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 46] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 35. | Mushtaq N, Resham S, Shamim S, Qureshi BM, Riaz Q, Bouffet E. Childhood Medulloblastoma. J Pak Med Assoc. 2020;70:2007-2016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 36. | Perini MV, Herman P, Montagnini AL, Jukemura J, Coelho FF, Kruger JA, Bacchella T, Cecconello I. Liver resection for the treatment of post-cholecystectomy biliary stricture with vascular injury. World J Gastroenterol. 2015;21:2102-2107. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 18] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 37. | Parrilla P, Robles R, Varo E, Jiménez C, Sánchez-Cabús S, Pareja E; Spanish Liver Transplantation Study Group. Liver transplantation for bile duct injury after open and laparoscopic cholecystectomy. Br J Surg. 2014;101:63-68. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 38. | Lubikowski J, Chmurowicz T, Post M, Jarosz K, Białek A, Milkiewicz P, Wójcicki M. Liver transplantation as an ultimate step in the management of iatrogenic bile duct injury complicated by secondary biliary cirrhosis. Ann Transplant. 2012;17:38-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 39. | Kohneh Shahri N, Lasnier C, Paineau J. [Bile duct injuries at laparoscopic cholecystectomy: early repair results]. Ann Chir. 2005;130:218-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 40. | Felekouras E, Petrou A, Neofytou K, Moris D, Dimitrokallis N, Bramis K, Griniatsos J, Pikoulis E, Diamantis T. Early or Delayed Intervention for Bile Duct Injuries following laparoscopic cholecystectomy? Gastroenterol Res Pract. 2015;2015:104235. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 41. | Barauskas G, Paškauskas S, Dambrauskas Z, Gulbinas A, Pundzius J. Referral pattern, management, and long-term results of laparoscopic bile duct injuries: a case series of 44 patients. Medicina (Kaunas). 2012;48:138-144. [PubMed] |
| 42. | Sahajpal AK, Chow SC, Dixon E, Greig PD, Gallinger S, Wei AC. Bile duct injuries associated with laparoscopic cholecystectomy: Timing of repair and long-term outcomes. Arch Surg. 2010;145:757-763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 52] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 43. | Dominguez-Rosado I, Sanford DE, Liu J, Hawkins WG, Mercado MA. Timing of Surgical Repair After Bile Duct Injury Impacts Postoperative Complications but Not Anastomotic Patency. Ann Surg. 2016;264:544-553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 61] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 44. | Stilling NM, Fristrup C, Wettergren A, Ugianskis A, Nygaard J, Holte K, Bardram L, Sall M, Mortensen MB. Long-term outcome after early repair of iatrogenic bile duct injury. A national Danish multicentre study. HPB (Oxford). 2015;17:394-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 52] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 45. | Kirks RC, Barnes TE, Lorimer PD, Cochran A, Siddiqui I, Martinie JB, Baker EH, Iannitti DA, Vrochides D. Comparing early and delayed repair of common bile duct injury to identify clinical drivers of outcome and morbidity. HPB (Oxford). 2016;18:718-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 46. | Arora A, Nag HH, Yadav A, Agarwal S, Javed A, Agarwal AK. Prompt Repair of Post Cholecystectomy Bile Duct Transection Recognized Intraoperatively and Referred Early: Experience from a Tertiary Care Teaching Unit. Indian J Surg. 2015;77:99-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 47. | A European-African HepatoPancreatoBiliary Association (E-AHPBA) Research Collaborative Study management group. Other members of the European-African HepatoPancreatoBiliary Association Research Collaborative. Post cholecystectomy bile duct injury: early, intermediate or late repair with hepaticojejunostomy - an E-AHPBA multi-center study. HPB (Oxford). 2019;21:1641-1647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (1)] |
| 48. | Battal M, Yazici P, Bostanci O, Karatepe O. Early Surgical Repair of Bile Duct Injuries following laparoscopic cholecystectomy: The Sooner the Better. Surg J (N Y). 2019;5:e154-e158. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 49. | Sweigert PJ, Eguia E, Nelson MH, Bunn C, Kulshrestha S, Luchette FA, Baker MS. Biliary Enteric Reconstruction After Biliary Injury: Delayed Repair Is More Costly Than Early Repair. J Surg Res. 2021;257:349-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 50. | El Nakeeb A, Sultan A, Ezzat H, Attia M, Abd ElWahab M, Kayed T, Hassanen A, AlMalki A, Alqarni A, Mohammed MM. Impact of referral pattern and timing of repair on surgical outcome after reconstruction of post-cholecystectomy bile duct injury: A multicenter study. Hepatobiliary Pancreat Dis Int. 2021;20:53-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (1)] |
| 51. | Anand U, Kumar R, Priyadarshi RN, Kumar M, Ahmed N, John AG, Parasar K, Kumar B. Analysis of outcomes of biliary reconstruction after post-cholecystectomy bile duct injuries. ANZ J Surg. 2021;91:1542-1548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |