Published online Jan 27, 2022. doi: 10.4254/wjh.v14.i1.158
Peer-review started: March 27, 2021
First decision: June 7, 2021
Revised: June 17, 2021
Accepted: December 22, 2021
Article in press: December 22, 2021
Published online: January 27, 2022
Processing time: 299 Days and 10.8 Hours
Recently, a single letter change has taken the world by storm. A group of experts have developed a consensus to upgrade the term non-alcoholic fatty liver disease (NAFLD) to metabolic associated fatty liver disease (MAFLD), suggesting that MAFLD would more accurately reflect not only the disease pathogenesis but would also help in patient stratification for management with NAFLD. However, the difference of opinion exists, which has made the NAFLD vs MAFLD debate the current talk of the town. This review will focus on the plausibility and implications of redefining NAFLD as MAFLD.
Core Tip: A group of experts have recently developed a consensus towards redefining non-alcoholic fatty liver disease (NAFLD) as metabolic associated fatty liver disease (MAFLD), suggestive of a more accurate differential diagnosis and signifying the exact disease pathogenesis to achieve higher patient stratification and delivery of better care to patients with NAFLD while avoiding stigmatization due to the presence of the word ‘alcohol’, particularly in regions where alcohol consumption is a taboo for cultural and religious reasons. However, differences in experts' opinions considering the implications of redefining NAFLD as MAFLD still hold strong. Therefore, this review article focuses on the plausibleness and implications of redefining NAFLD as MAFLD.
- Citation: Devi J, Raees A, Butt AS. Redefining non-alcoholic fatty liver disease to metabolic associated fatty liver disease: Is this plausible? World J Hepatol 2022; 14(1): 158-167
- URL: https://www.wjgnet.com/1948-5182/full/v14/i1/158.htm
- DOI: https://dx.doi.org/10.4254/wjh.v14.i1.158
The world has seen steady progress in the awareness of non-alcoholic fatty liver disease (NAFLD) owing to its rising prevalence, yet there has been no worthwhile advancement in treatment and management and or breakthrough in the therapeutic field. A great part of this shortcoming has always been linked to the inadequacy of the term NAFLD, as it fails to describe the underlying metabolic factors of the disorder, instead shedding undue light on the etiology which is in actual unrelated to the core pathology, i.e., alcohol. To overcome this problem, many scientists have joined hands and suggested an up-gradation in nomenclature. Hence, the term metabolic associated fatty liver disease (MAFLD) has been under a great uproar for the past couple of years.
NAFLD is a chronic disorder encompassing a spectrum of liver diseases characterized by excessive intrahepatic fat deposition, leading to hepatocyte ballooning injury in the absence of a known cause such as excessive alcohol consumption, viral hepatitis, medications, or a hereditary disorder[1]. It is further classified into NAFL when there is > 5% liver steatosis with no evidence of hepatocyte injury or fibrosis and non-alcoholic steatohepatitis (NASH) when there are > 5% liver steatosis and ballooning of hepatocytes with or without liver fibrosis. NASH may lead to complications such as cirrhosis and hepatocellular carcinoma, and increase liver-related mortality as fibrosis advances. Risk factors associated with fibrosis are old age, diabetes mellitus, obesity, hypertension, and degree of insulin resistance[2].
The nomenclature was introduced in 1980 by a pathologist, Jurgen Ludwig, who used the term NAFLD and NASH to describe the histological findings found in a series of 20 patients[3]. The introduction of the term was based on marked similarities between alcoholic steatohepatitis and NASH. Later, Kleiner et al[4] proposed the NAS score to evaluate changes in histological features individually to grade and stage the disease. A decade later, Bedossa et al[5] came up with an algorithm to diagnose NASH. However, none of these scores could predict future clinical outcomes in patients with NAFLD.
The prevalence of NAFLD is on the rise in the last three decades in the United States, reaching about 20%-30%, mirroring the steady increase in obesity globally[2,6]. It has become the second most common cause of liver transplantation in Western countries, which is quite alarming[7]. Despite the dangerously rising prevalence, awareness regarding the disease burden is still not up to the mark. This is also reflected by the lack of availability of a non-invasive diagnostic test. The only way to make a definitive diagnosis of NAFLD and assess its severity is a liver biopsy, which is invasive and costly, leading to delays in the final diagnosis[1]. Unfortunately, the therapeutic field has also not seen any breakthrough and to date, there is no FDA-approved pharmacotherapy available. The treatment solely relies on lifestyle modifications with regular exercise and dietary changes with weight loss being the goal of therapy[8]. This requires a good deal of cooperation on part of the patient with a large part of the therapeutic responsibility on the patient himself/herself, making the entire ordeal quite difficult since switching to and long-term sustenance of such a drastic lifestyle is quite arduous. Various agents have been used in addition to lifestyle modification, ranging from pioglitazone and vitamin E (antioxidant) to ursodeoxycholic acid, and while some drugs have been able to reduce liver fat content such as pinositol, vitamin E, and obeticholic acid, none of these had an impact on NASH or fibrosis; on the other hand, adverse effects and long-term safety from the use of these drugs have remained a major concern[9,10].
Inappropriate nomenclature of any disorder has an overall impact on its perception both by patients and physicians. It may lead to confusion and the development of mistrust between patients and their treating doctors, thus affecting overall outcomes. It is also difficult for patients to understand the magnitude of the problem when the disease terminology is based on a negative term. For instance, establishing a diagnosis of NAFLD requires exclusion of significant alcohol consumption while ironically, there is no accepted cut-off limit for significant alcohol consumption. On the other hand, less alcohol use may also be affiliated with hepatic steatosis and fibrosis progression in NAFLD patients. The current term does not provide any relevant information on what the condition is, rather it represents what it is not!
A significant concern lies in the stigmatization of the disease due to the presence of the word ‘alcohol’, particularly in regions where alcohol consumption is a taboo for cultural and religious reasons. It exerts a psychological strain on the patient to the existing clinical spectrum of the disease. In such cases, specific inquiries on intake of alcohol may be misinterpreted, adversely affecting the doctor-patient relationship. On the other hand, trivialization is a commonly faced problem with the current terminology as patients rely on quitting alcohol consumption solely to curb the disease progression and are reluctant for any other essentially needed lifestyle or behavioral modifications.
Advancements in the field to curb the existing dilemma are largely affected by the sub-optimal allocation of funding, resulting from a lack of awareness of disease severity and complications. It is expected that a change in nomenclature may be able to deal with the negative consequences, proving to be a catalyst to accelerate funding and health policy action.
Over the years, research has proven that NAFLD is an inadequate term to describe liver disease associated with metabolic dysfunction, as it fails to emphasize the most important and commonly noted etiology of metabolic dysfunction. To address these issues, researchers and societies have become inclined to the idea of changing the terminology. In 2005, Loria et al proposed to introduce positive criteria to define NAFLD[11]. Subsequently, in 2018, the European Liver Patient’s Association asked for a change in nomenclature owing to the limitations of existing terminology[12]. Eslam et al[13] in 2019 suggested updating the term and appealed to consider a more accurate term to define the disease.
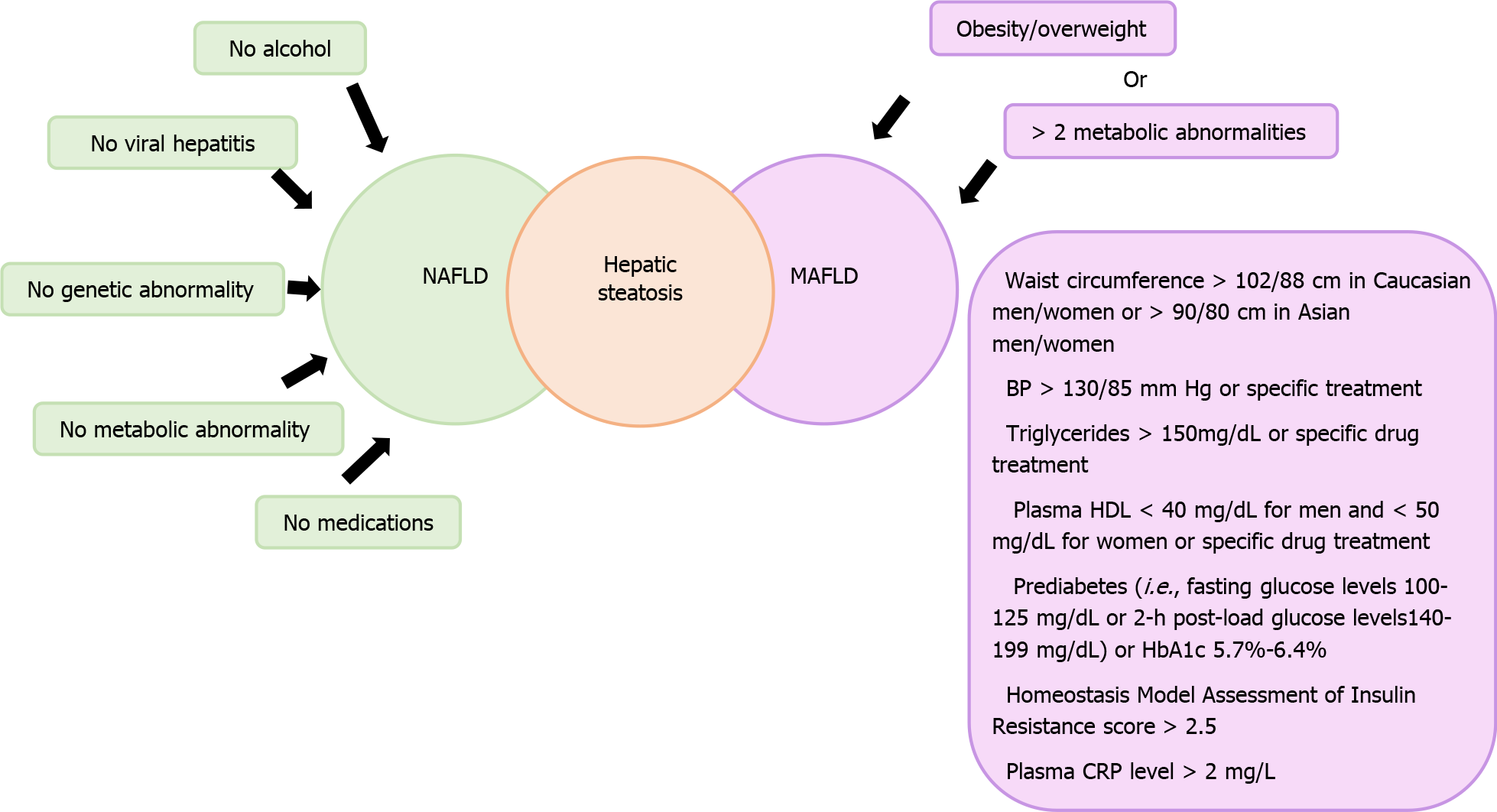
The basic reason calling for this substantial shift in terminology was to improve patient awareness and to overcome the challenges in management which seemed to be associated with the term NAFLD. After several modifications in search of the most appropriate terminology, the term MAFLD was coined, as it was most reflective of the most likely associations of the disease. The suggested criteria include the presence of hepatic steatosis radiologically or histologically in obese or overweight individuals. While in lean individuals who are found to have hepatic steatosis, evidence of two or more metabolic risk factors is mandatory as shown in Figure 1. Besides involving a large spectrum of diseases, the term MAFLD also acknowledges the presence of multiple overlapping causes and drivers of the disease, thus rendering it as a hepatic manifestation of a multi-system disease. A recent study illustrated that metabolic syndrome is a more deleterious cardiovascular risk factor than NAFLD, which could represent an epiphenomenon of the metabolic syndrome itself[14]. The change in terminology is not only expected to raise awareness at both patients’ and physicians’ levels but also gain attention from the funding agencies and other major stakeholders, eventually leading to an acceleration in advancement in the field of diagnosis and disease therapy.
Although the new term MAFLD is expected to deal with several issues posed by the term NALFD, it may have to face challenges of its own. While MAFLD is a flexible term and may encompass a variety of disorders, it is important to note that there is no fixed criterion to describe metabolic dysfunction and there remains some ambiguity regarding a complete definition. Also, genetic disorders associated with NAFLD may remain a separate entity as the term MAFLD fails to include that. Therefore, updating the term NAFLD to another umbrella term that does not adequately describe the underlying driving factors comprehensively, may become counterproductive, as this may need another upgrade following a few decades of advancements.
Because of the imprecision of the term NAFLD, crucial suggestions have been brought forward by Asian and European researchers to turn it to MAFLD, which can accurately capture the predisposing factor and diminish the exclusion criteria[15]. While upgrading the term may help in improving disease awareness, its impact on other aspects does not seem too promising. For scientific contention, scrutiny and reasoning lie in the evidence-based debate, and recognizing salient characteristics of evidence would be of great value[16,17]. The primary role of metabolic dysfunction makes a pivotal point in the pathophysiology of fatty liver disease[12,13]. Globally, this initiative has been endorsed by the Asian Pacific Association for the Study of the Liver and welcomed by many experts along with patients’ organizations[18-25]. On the other hand, a few scholars are skeptical about this change and advocate it as being overhasty[26].
Ever since its proposal, research studies have been carried out to compare the impact of the two terms on the feasibility of diagnosis and overall outcomes of the disease. The very first study by Lin et al[27] illustrated that the FIB-4 index and NAFLD fibrosis score were increased in MAFLD criteria and also proposed that the latter is more efficient in diagnosing high-risk patients. An analysis of the recent database (2017-2019) from Japan found that MAFLD was 20% more competent than NAFLD in the diagnosis of fibrosis[28]. Another study by Zheng et al[29] reflected that MAFLD diagnostic criteria were more pertinent even in resource-limited countries and was able to recognize more homogenous groups. Xu et al[30] validated the high diagnostic capability of the fatty liver index in MAFLD patients as a marker of hepatic steatosis, in particular where the use of ultrasound is narrowed. The MAFLD criteria were found more accurate than older NAFLD criteria when analyzing momentous hepatic fibrosis in the patients with cardiovascular disease[31,32], chronic kidney disease[33], and appraisal of genetic risk factors[34] in fatty liver disease. It also implies that MAFLD may coexist with other liver diseases, for instance, hepatitis B and C[15,35-37], HIV infection[38], Gaucher[39], and coeliac disease[40], hence making it more plausible than NAFLD. Table 1 shows all the studies comparing the two terms[41-44].
| No. | Ref. | Number of participants | Study type | Outcome measures | Result |
| 1 | Lin et al[27], 2020 | 13083 | Cross-sectional, cohort from the National Health and Nutrition Examination Surveys III database | Significant fibrosis | Liver enzymes and the non-invasive liver fibrosis scores were significantly higher in MAFLD compared to NAFLD group (P < 0.05) |
| 2 | Yamamura et al[28], 2020 | 765 | Cross-sectional Japanese cohort | Significant fibrosis | MAFLD (OR = 4.401; 95%CI: 2.144-10.629; P < 0.0001). NAFLD (OR = 1.721; 95%CI: 1.009-2.951; P = 0.0463) |
| 3 | Niriella et al[31], 2020 | 2985 | A prospective study with 7 years of follow-up | Cardiovascular event CVD (non-fatal + fatal) | Excluded by NAFLD definition but captured by MAFLD definition adjusted OR [8.5 (2.2-32.8)]. Excluded by MAFLD definition but captured by NAFLD definition Adjusted OR [2.0 (0.2-19.2)] |
| 4 | Mak et al[15], 2020 | 1134 | Cross-sectional chronic hepatitis B and fatty liver | Advanced fibrosis/ cirrhosis | Patients with CHB + MAFLD compared to patients with CHB + NAFLD outside the MAFLD criteria (22.6% vs 11.8%, P = 0.043) |
| 5 | Zheng et al[29], 2021 | 780 | Cohort,(Liver biopsy) | Diagnostic criteria easily applicable even in a resource-limited country | |
| 6 | Xu et al[30], 2020 | 35335 | Cohort | Fatty liver index as a marker of hepatic steatosis | AUROC of FLI for predicting HS was 0.856 (95%CI: 0.854–0.859) in malesand 0.909 (95%CI: 0.906-0.911) in females, which showed a good diagnostic ability |
| 7 | Liu et al[41], 2021 | 361 | Cross-sectional study, HIV and fatty liver disease | A positive correlation between LSM and CAP values was found in the MAFLD group | Prevalence of NAFLD (37.67%) and MAFLD (34.90%) (ALT) level (44.44% vs 16.17%, P < 0.001) and advanced fibrosis (19.05% vs 2.55%, P < 0.001) were significantly higher in the MAFLD group |
| 8 | Myers et al[42], 2021 | 920 | Population cohort study | The burden of NAFLD and MAFLD associated HCCs increased significantly, driving an increase in HCC incidence, particularly in women. | Proportion of NAFLD-HCC increased more in women (0% to 29%, P = 0.037) than in men (2% to 12%, P = 0.010) while the proportion of MAFLD increased from 21% to 68% in both sexes and 7% to 67% in women (P < 0.001) |
| 9 | Guerreiro et al[43], 2021 | 1233 | Retrospective cross-sectional study | Differences between NAFLD and MAFLD regarding cardiovascular events | MAFLD and NAFLD, CVR was intermediate/high (36.4 and 25.7%, P = 0.209) and CVD occurred in 20.1 and 12.8% (P = 0.137) of the cases, respectively |
| 10 | Ciardullo et al[44], 2021 | 1710 | A cross-sectional study of adults recruited in the 2017- 2018 National Health and Nutrition Examination Survey, a representative sample of the general United States population. | Significant fibrosis | The weighted prevalence of NAFLD and MAFLD were similar in the whole population at 37.1% (95% CI 34.0-40.4) and 39.1% (95% CI 36.3-42.1) respectively. |
Furthermore, the evolution of genome-wide association has led to the recognition of PNPLA3 and TM6SF2[45] genes that dictate the genetic linkage to pathophysiology and support the diagnostic approach of metabolic syndrome. As it is a genetically co-determined metabolic disorder, this terminology aids patients to comprehend the disease and perhaps boost compliance to lifestyle modification. New studies scrutinizing the involvement of the liver in the prognostication of COVID-19 integrated MAFLD criteria[46-48] identified a significant flaw in the MAFLD definition similar to that of NAFLD that is the paucity of knowledge about other relevant pathophysiological drivers except for metabolic risk factors, such as genetic components. Concerns are raised that the term MAFLD, shelters a group of large entities, which leads to increased sensitivity at the cost of low specificity. For instance, NAFLD could be misdiagnosed in metabolically healthy individuals unless we rule out alternative or additional reasons. Similar reasoning applies to lean patients having two or more metabolic risk factors[12,18]. This is why a few others suggested the term dysmetabolism-associated fatty liver disease because of its strong association with dysfunctional metabolism leading to NAFLD and its complications[49]. Lately, on the account of AASLD, Younossi et al[26] articulated that it is premature to rename the terminology due to various reasons; quoting one as, the term MAFLD may not be enough to clearly describe the genetic and environmental associations of the disease, making it yet another umbrella term requiring upgrading after a few decades once more information on the pathophysiology and natural history of the disorder is available. Inclusion of all significant stakeholders such as regulatory agencies and the patients’ organization is also mandatory in the movement of renaming the disease[26]. Mass screening would only be possible once all the scientific and patient care societies are on the same page.
NAFLD has set its foot in a world full of subspecialties via disseminating knowledge in different educational sessions; it yet lacks the channel of screening in the workup of their patients. To increase awareness and to overcome this roadblock, the liver community needs to engage genuinely with non-hepatologist to design a clinical approach based on the metabolic risk factors.
In contrast to viral hepatitis for which[50] the World Health Organization has developed a Global Health Sector Strategy to eliminate it by 2030, no such agendas are programmed to tackle the burden of NAFLD. Nonetheless, it seems to rise in the coming era and has a marked impact on economic and health losses, as it is the third leading cause of hepatocellular carcinoma and the second indication for liver transplantation in the West. To sum up, any terminology with the prefix ‘non’ may be considered a non-serious issue reducing its overall significance[51,52]. For the same purpose, there are ongoing efforts to eliminate the ‘non’ by renaming and reframing non-communicable diseases[53-55]. Within this frame of reference, an attempt should be made to instruct policymakers to allocate funding for research to cope with existing inequalities.
NAFLD like other non-communicable diseases, such as diabetes mellitus and obesity, is often referred to as contrition diseases, insinuating that this develops through personal behavioral choices which often lead to shame and accusation for individuals which hinder their desire to seek help. It is universally endorsed that an important part of treatment is a healthy diet and physically active lifestyle, thus essentially requiring the involvement of patients; however, many patients are not even aware of NAFLD as a disease entity[56,57]. Also, a survey conducted in the United States in 2015 indicated that no more than one-fourth of patients enrolled in the study were acquainted with the disease[58]. The National Health and Nutrition Examination Survey conducted from 2013 to 2016, showed that merely 3.5% of the population had awareness of the disease[59]. Similarly, ‘Continuum Clinical’ illustrated again that 6% of patients had the know-how of their disease. Various other studies likewise supported these results[60]. Primary care physicians also have insufficient sensitivity for establishing a diagnosis of NAFLD and how it should be assessed[61]. Another study depicted incidental diagnosis of NAFLD at the stage of cirrhosis[62]. Research in 2018 showed that despite expanding incidence, a massive number of patients remained underreported[63]. This lack of public health responses to NAFLD may be attributed to the baffled term alcohol in NAFLD which exerts hurdles in understanding and acceptance of the disease, thus damaging the disease response[64]. In many parts of the world, consumption of alcohol is prohibited due to social and religious norms with even more daunting concerns in children where its use is not well established. In such regions, the term imposes potential stigmatization of the disease. The European Liver Patients Association was not satisfied with the term NAFLD and put forward the thoughts to change the name. This NAFLD acronym also creates perplexity and hampers efficient communication that leads to negative repercussions on the physician-patient relationship. The “non” term in NAFLD also underestimates this deleterious health challenge which might be perceived as a trivial matter or as if, one is authorized to consume alcohol. Embracing the latest term MAFLD and related positive diagnostic criteria may resolve many issues regarding confusion, trivialization, and stigmatization related to the term NAFLD.
To curtail the serious outcomes associated with fatty liver disease, the previously faced challenges must be identified and tackled effectively. To begin with, owing to the heterogeneity of the disease and dynamic histopathology, no diagnostic biomarker is available as yet. This could be expedited by phenotypic classification for which Non-Invasive Biomarkers of Metabolic Liver Disease and Liver Investigation: Testing Marker Utility in Steatohepatitis work vigorously based on the validated biomarkers. Second, the lack of an FDA-approved drug for the management of the disease is already a huge hurdle, and a change in the disease terminology may hamper the ongoing drug trials. On the other hand, it was expected that the term MAFLD will aid in the refinement of clinical endpoints for future drug trials. However, for a change of the name, it demands vigilant speculation of societal and medical ramifications and real impact. In the long run, although the advancement is bound to be imperceptible, we must strike into the appropriate pathway to lay down the groundwork for accomplishing the long-term targets.
Nonetheless, being in the modern era, evidence-based medicine, an evolving science, advancement in technology, and personalized medicine will have a positive impact on healthcare. Due to the heterogeneity of the disease, there should be a multidisciplinary approach which not just involves hepatologists but also other specialties like endocrinologists and cardiologists. Notably, the conceptual framework of MAFLD lines up the liver disease with the latest comprehension of metabolic syndrome, obesity, and systemic biology. By doing this, we can adopt the heterogeneity and have many subtyping that can at length lead to a precision of medicine based on system narrative. From this viewpoint, the old term “cryptogenic cirrhosis” will be replaced by MAFLD-related cirrhosis. This name scales down the confusion not just on the etiologic spectrum, but also stigma and revamps physician-patient relationships.
What happens next when MAFLD gains ground? Then we would have to embrace the connection between metabolic disorder and low-grade inflammation, in particular adipose tissue inflammation which might unlock the door to new treatment strategies in the future. Hence, it is also essential to recognize that joint efforts of scientific societies, pharmaceutical industries, and patient associations have led to a marked acceleration in the development of medications currently under trial for NAFLD, which could all go in vain if the nomenclature is to change at this point. Hence, it may be wise to arrange a combined international conference of all the important stakeholders asking for their opinion regarding an upgrade in the nomenclature in addition to deciding an appropriate timing for it.
As it is a nascent idea, the journey can go at a snail’s pace as it needs affirmation by clinicians, patients, researchers, and industry worldwide. In addition, this calls for future studies and funding to be escalated to explore the consequences of change in terminology. Unless we all converge to bring a consensus regarding this as well as improving the overall disease outcomes, a mere change in terminology may still not be sufficient. Joint efforts are needed on everyone's part to increase disease awareness, reduce its global burden, and provide effective diagnostic and therapeutic modalities.
Provenance and peer review: Invited article; Externally peer-reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Pakistan
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Menichelli D, Treeprasertsuk S S-Editor: Liu M L-Editor: Wang TQ P-Editor: Liu M
| 1. | Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, Charlton M, Sanyal AJ; American Gastroenterological Association; American Association for the Study of Liver Diseases; American College of Gastroenterologyh. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology. Gastroenterology. 2012;142:1592-1609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1226] [Cited by in RCA: 1355] [Article Influence: 104.2] [Reference Citation Analysis (4)] |
| 2. | Younossi Z, Anstee QM, Marietti M, Hardy T, Henry L, Eslam M, George J, Bugianesi E. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018;15:11-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4054] [Cited by in RCA: 3772] [Article Influence: 538.9] [Reference Citation Analysis (2)] |
| 3. | . Younossi Z, Anstee QM, Marietti M, Hardy T, Henry L, Eslam M, George J, Bugianesi E. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018;15:11-20. |
| 4. | Kleiner DE, Brunt EM, Van Natta M, Behling C, Contos MJ, Cummings OW, Ferrell LD, Liu YC, Torbenson MS, Unalp-Arida A, Yeh M, McCullough AJ, Sanyal AJ; Nonalcoholic Steatohepatitis Clinical Research Network. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41:1313-1321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6807] [Cited by in RCA: 8212] [Article Influence: 410.6] [Reference Citation Analysis (5)] |
| 5. | Bedossa P; FLIP Pathology Consortium. Utility and appropriateness of the fatty liver inhibition of progression (FLIP) algorithm and steatosis, activity, and fibrosis (SAF) score in the evaluation of biopsies of nonalcoholic fatty liver disease. Hepatology. 2014;60:565-575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 396] [Cited by in RCA: 458] [Article Influence: 41.6] [Reference Citation Analysis (0)] |
| 6. | Younossi ZM. Non-alcoholic fatty liver disease - A global public health perspective. J Hepatol. 2019;70:531-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 943] [Cited by in RCA: 1453] [Article Influence: 242.2] [Reference Citation Analysis (1)] |
| 7. | Younossi ZM, Marchesini G, Pinto-Cortez H, Petta S. Epidemiology of Nonalcoholic Fatty Liver Disease and Nonalcoholic Steatohepatitis: Implications for Liver Transplantation. Transplantation. 2019;103:22-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 272] [Article Influence: 45.3] [Reference Citation Analysis (0)] |
| 8. | Romero-Gómez M, Zelber-Sagi S, Trenell M. Treatment of NAFLD with diet, physical activity and exercise. J Hepatol. 2017;67:829-846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 844] [Cited by in RCA: 921] [Article Influence: 115.1] [Reference Citation Analysis (0)] |
| 9. | Hossain N, Kanwar P, Mohanty SR. A Comprehensive Updated Review of Pharmaceutical and Nonpharmaceutical Treatment for NAFLD. Gastroenterol Res Pract. 2016;2016:7109270. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 10. | Pani A, Giossi R, Menichelli D, Fittipaldo VA, Agnelli F, Inglese E, Romandini A, Roncato R, Pintaudi B, Del Sole F, Scaglione F. Inositol and Non-Alcoholic Fatty Liver Disease: A Systematic Review on Deficiencies and Supplementation. Nutrients. 2020;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 11. | Loria P, Lonardo A, Carulli N. Should nonalcoholic fatty liver disease be renamed? Dig Dis. 2005;23:72-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 62] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 12. | Eslam M, Sanyal AJ, George J; International Consensus Panel. MAFLD: A Consensus-Driven Proposed Nomenclature for Metabolic Associated Fatty Liver Disease. Gastroenterology. 2020;158:1999-2014.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2367] [Cited by in RCA: 2196] [Article Influence: 439.2] [Reference Citation Analysis (1)] |
| 13. | Eslam M, Newsome PN, Sarin SK, Anstee QM, Targher G, Romero-Gomez M, Zelber-Sagi S, Wai-Sun Wong V, Dufour JF, Schattenberg JM, Kawaguchi T, Arrese M, Valenti L, Shiha G, Tiribelli C, Yki-Järvinen H, Fan JG, Grønbæk H, Yilmaz Y, Cortez-Pinto H, Oliveira CP, Bedossa P, Adams LA, Zheng MH, Fouad Y, Chan WK, Mendez-Sanchez N, Ahn SH, Castera L, Bugianesi E, Ratziu V, George J. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. J Hepatol. 2020;73:202-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2883] [Cited by in RCA: 2802] [Article Influence: 560.4] [Reference Citation Analysis (1)] |
| 14. | Pastori D, Sciacqua A, Marcucci R, Del Ben M, Baratta F, Violi F, Pignatelli P; ATHERO-AF study group. Non-alcoholic fatty liver disease (NAFLD), metabolic syndrome and cardiovascular events in atrial fibrillation. A prospective multicenter cohort study. Intern Emerg Med. 2021;16:2063-2068. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 15. | Mak LY, Yuen MF, Seto WK. Letter regarding "A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement". J Hepatol. 2020;73:1573-1574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 16. | Sehon SR, Stanley DE. A philosophical analysis of the evidence-based medicine debate. BMC Health Serv Res. 2003;3:14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 79] [Cited by in RCA: 66] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 17. | Upshur RE. Looking for rules in a world of exceptions: reflections on evidence-based practice. Perspect Biol Med. 2005;48:477-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 63] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 18. | Fouad Y, Waked I, Bollipo S, Gomaa A, Ajlouni Y, Attia D. What's in a name? Liver Int. 2020;40:1254-1261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 210] [Article Influence: 42.0] [Reference Citation Analysis (0)] |
| 19. | Kuchay MS, Misra A. From non-alcoholic fatty liver disease (NAFLD) to metabolic-associated fatty liver disease (MAFLD): A journey over 40 years. Diabetes Metab Syndr. 2020;14:695-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 20. | Zheng KI, Fan JG, Shi JP, Wong VW, Eslam M, George J, Zheng MH. From NAFLD to MAFLD: a "redefining" moment for fatty liver disease. Chin Med J (Engl). 2020;133:2271-2273. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 81] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 21. | Demirtas CO, Yilmaz Y. Metabolic-associated Fatty Liver Disease: Time to integrate ground-breaking new terminology to our clinical practice. Hepatology Forum. 2020;3: 79-81. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 22. | Tilg H, Effenberger M. From NAFLD to MAFLD: when pathophysiology succeeds. Nat Rev Gastroenterol Hepatol. 2020;17:387-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 176] [Article Influence: 35.2] [Reference Citation Analysis (0)] |
| 23. | The Lancet Gastroenterology Hepatology. Redefining non-alcoholic fatty liver disease: what's in a name? Lancet Gastroenterol Hepatol. 2020;5:419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 43] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 24. | Valenti L, Pelusi S. Redefining fatty liver disease classification in 2020. Liver Int. 2020;40:1016-1017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 41] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 25. | Eslam M, Sarin SK, Wong VW, Fan JG, Kawaguchi T, Ahn SH, Zheng MH, Shiha G, Yilmaz Y, Gani R, Alam S, Dan YY, Kao JH, Hamid S, Cua IH, Chan WK, Payawal D, Tan SS, Tanwandee T, Adams LA, Kumar M, Omata M, George J. The Asian Pacific Association for the Study of the Liver clinical practice guidelines for the diagnosis and management of metabolic associated fatty liver disease. Hepatol Int. 2020;14:889-919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 563] [Cited by in RCA: 551] [Article Influence: 110.2] [Reference Citation Analysis (0)] |
| 26. | Younossi ZM, Rinella ME, Sanyal AJ, Harrison SA, Brunt EM, Goodman Z, Cohen DE, Loomba R. From NAFLD to MAFLD: Implications of a Premature Change in Terminology. Hepatology. 2021;73:1194-1198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 290] [Article Influence: 72.5] [Reference Citation Analysis (0)] |
| 27. | Lin S, Huang J, Wang M, Kumar R, Liu Y, Liu S, Wu Y, Wang X, Zhu Y. Comparison of MAFLD and NAFLD diagnostic criteria in real world. Liver Int. 2020;40:2082-2089. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 424] [Cited by in RCA: 400] [Article Influence: 80.0] [Reference Citation Analysis (0)] |
| 28. | Yamamura S, Eslam M, Kawaguchi T, Tsutsumi T, Nakano D, Yoshinaga S, Takahashi H, Anzai K, George J, Torimura T. MAFLD identifies patients with significant hepatic fibrosis better than NAFLD. Liver Int. 2020;40:3018-3030. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 342] [Cited by in RCA: 313] [Article Influence: 62.6] [Reference Citation Analysis (0)] |
| 29. | Zheng KI, Sun DQ, Jin Y, Zhu PW, Zheng MH. Clinical utility of the MAFLD definition. J Hepatol. 2021;74:989-991. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 53] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 30. | Xu Z, Li H, Tian S, Wu J, Li X, Liu ZL, Li S, Chen YL, Xiao J, Wei JY, Liang XY, Ran L, Kong LQ. Blood biomarkers for the diagnosis of hepatic steatosis in metabolic dysfunction-associated fatty liver disease. J Hepatol. 2020;73:1264-1265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 31. | Niriella MA, Ediriweera DS, Kasturiratne A, De Silva ST, Dassanayaka AS, De Silva AP, Kato N, Pathmeswaran A, Wickramasinghe AR, de Silva HJ. Outcomes of NAFLD and MAFLD: Results from a community-based, prospective cohort study. PLoS One. 2021;16:e0245762. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 76] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 32. | Lee H, Lee YH, Kim SU, Kim HC. Metabolic Dysfunction-Associated Fatty Liver Disease and Incident Cardiovascular Disease Risk: A Nationwide Cohort Study. Clin Gastroenterol Hepatol. 2021;19:2138-2147.e10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 309] [Cited by in RCA: 312] [Article Influence: 78.0] [Reference Citation Analysis (0)] |
| 33. | Sun DQ, Jin Y, Wang TY, Zheng KI, Rios RS, Zhang HY, Targher G, Byrne CD, Yuan WJ, Zheng MH. MAFLD and risk of CKD. Metabolism. 2021;115:154433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 235] [Cited by in RCA: 222] [Article Influence: 55.5] [Reference Citation Analysis (0)] |
| 34. | Xia M, Zeng H, Wang S, Tang H, Gao X. Insights into contribution of genetic variants towards the susceptibility of MAFLD revealed by the NMR-based lipoprotein profiling. J Hepatol. 2021;74:974-977. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 34] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 35. | Ergenc I, Gokcen P, Adali G, Kani HT, Demirtas CO, Gunduz F, Celikel CA, Yilmaz Y. High incidence of hepatitis B core antibody positivity in metabolic-associated fatty liver disease-related cirrhosis. Hepatology Forum. 2021;2:20. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 36. | Fouad Y, Saad Z, Raheem EA, Moness H, Osman N, Abdelhameed W, et al Clinical Validity of the diagnostic criteria for metabolic-associated fatty liver disease: a real-world experience. 2020 Preprint. Available from: medRxiv. [DOI] [Full Text] |
| 37. | Gao F, Zheng KI, Wang XB, Yan HD, Sun QF, Pan KH, Wang TY, Chen YP, George J, Zheng MH. Metabolic associated fatty liver disease increases coronavirus disease 2019 disease severity in nondiabetic patients. J Gastroenterol Hepatol. 2021;36:204-207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 80] [Cited by in RCA: 85] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 38. | Jongraksak T, Sobhonslidsuk A, Jatchavala J, Warodomwichit D, Kaewduang P, Sungkanuparph S. Prevalence and predicting factors of metabolic-associated fatty liver disease diagnosed by transient elastography with controlled attenuation parameters in HIV-positive people. Int J STD AIDS. 2021;32:266-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 39. | Nascimbeni F, Lugari S, Cassinerio E, Motta I, Cavicchioli A, Dalla Salda A, Bursi S, Donatiello S, Spina V, Cappellini MD, Andreone P, Carubbi F. Liver steatosis is highly prevalent and is associated with metabolic risk factors and liver fibrosis in adult patients with type 1 Gaucher disease. Liver Int. 2020;40:3061-3070. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 40. | Rispo A, Imperatore N, Guarino M, Tortora R, Alisi A, Cossiga V, Testa A, Ricciolino S, Fiorentino A, Morisco F. Metabolic-associated fatty liver disease (MAFLD) in coeliac disease. Liver Int. 2021;41:788-798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 41. | Liu D, Shen Y, Zhang R, Xun J, Wang J, Liu L, Steinhart C, Chen J, Lu H. Prevalence and risk factors of metabolic associated fatty liver disease among people living with HIV in China. J Gastroenterol Hepatol. 2021;36:1670-1678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 42. | Myers S, Neyroud-Caspar I, Spahr L, Gkouvatsos K, Fournier E, Giostra E, Magini G, Frossard JL, Bascaron ME, Vernaz N, Zampaglione L, Negro F, Goossens N. NAFLD and MAFLD as emerging causes of HCC: A populational study. JHEP Rep. 2021;3:100231. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 71] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 43. | Guerreiro GTS, Longo L, Fonseca MA, de Souza VEG, Álvares-da-Silva MR. Does the risk of cardiovascular events differ between biopsy-proven NAFLD and MAFLD? Hepatol Int. 2021;15:380-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 50] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 44. | Ciardullo S, Perseghin G. Prevalence of NAFLD, MAFLD and associated advanced fibrosis in the contemporary United States population. Liver Int. 2021;41:1290-1293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 160] [Article Influence: 40.0] [Reference Citation Analysis (0)] |
| 45. | Park SL, Li Y, Sheng X, Hom V, Xia L, Zhao K, Pooler L, Setiawan VW, Lim U, Monroe KR, Wilkens LR, Kristal BS, Lampe JW, Hullar M, Shepherd J, Loo LLM, Ernst T, Franke AA, Tiirikainen M, Haiman CA, Stram DO, Le Marchand L, Cheng I. Genome-Wide Association Study of Liver Fat: The Multiethnic Cohort Adiposity Phenotype Study. Hepatol Commun. 2020;4:1112-1123. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 46. | Assante G, Williams R, Youngson NA. Is the increased risk for MAFLD patients to develop severe COVID-19 Linked to perturbation of the gut-liver axis? J Hepatol. 2021;74:487-488. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 47. | Zhou YJ, Zheng KI, Wang XB, Yan HD, Sun QF, Pan KH, Wang TY, Ma HL, Chen YP, George J, Zheng MH. Younger patients with MAFLD are at increased risk of severe COVID-19 illness: A multicenter preliminary analysis. J Hepatol. 2020;73:719-721. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 104] [Cited by in RCA: 106] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 48. | Zhou YJ, Zheng KI, Wang XB, Sun QF, Pan KH, Wang TY, Ma HL, Chen YP, George J, Zheng MH. Metabolic-associated fatty liver disease is associated with severity of COVID-19. Liver Int. 2020;40:2160-2163. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 81] [Cited by in RCA: 82] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 49. | Polyzos SA, Mantzoros CS. Making progress in nonalcoholic fatty liver disease (NAFLD) as we are transitioning from the era of NAFLD to dys-metabolism associated fatty liver disease (DAFLD). Metabolism. 2020;111S:154318. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 35] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 50. | Waheed Y. Transition from millennium development goals to sustainable development goals and hepatitis. Pathog Glob Health. 2015;109:353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 51. | Allen LN, Feigl AB. What's in a name? Lancet Glob Health. 2017;5:e129-e130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 35] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 52. | Sridhar D, Morrison JS, Piot P. Getting the politics right for the September 2011. UN high-level meeting on noncommunicable diseases; 2011 Sep 19-20, NewYork. United Nations, 2011. |
| 53. | Kozelka EE, Jenkins JH. Renaming non-communicable diseases. Lancet Glob Health. 2017;5:e655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 54. | Zou G, Decoster K, McPake B, Witter S. Renaming non-communicable diseases. Lancet Glob Health. 2017;5:e656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 55. | Lincoln P. Renaming non-communicable diseases. Lancet Glob Health. 2017;5:e654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 56. | Byrne CD, Targher G. EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease: is universal screening appropriate? Diabetologia. 2016;59:1141-1144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 77] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 57. | Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, Harrison SA, Brunt EM, Sanyal AJ. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67:328-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3544] [Cited by in RCA: 4929] [Article Influence: 704.1] [Reference Citation Analysis (9)] |
| 58. | Wieland AC, Mettler P, McDermott MT, Crane LA, Cicutto LC, Bambha KM. Low awareness of nonalcoholic fatty liver disease among patients at high metabolic risk. J Clin Gastroenterol. 2015;49:e6-e10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 59] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 59. | Singh A, Kumar A, Singh S, Dhaliwal AJS, Lopez R, Noureddin M, Naim A. Trends of Awareness of Non-Alcoholic Fatty Liver Disease, Alcoholic Liver Disease and Both Fatty Liver Diseases (BAFLD) Using National Health and Nutrition Examination Survey: 836. Am J Gastroenterol. 2018;113:S465. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 60. | Cook NS, Nagar SH, Jain A, Balp MM, Mayländer M, Weiss O, Chatterjee S. Understanding Patient Preferences and Unmet Needs in Non-alcoholic Steatohepatitis (NASH): Insights from a Qualitative Online Bulletin Board Study. Adv Ther. 2019;36:478-491. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 61. | Patel PJ, Banh X, Horsfall LU, Hayward KL, Hossain F, Johnson T, Stuart KA, Brown NN, Saad N, Clouston A, Irvine KM, Russell AW, Valery PC, Williams S, Powell EE. Underappreciation of non-alcoholic fatty liver disease by primary care clinicians: limited awareness of surrogate markers of fibrosis. Intern Med J. 2018;48:144-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 81] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 62. | Bertot LC, Jeffrey GP, Wallace M, MacQuillan G, Garas G, Ching HL, Adams LA. Nonalcoholic fatty liver disease-related cirrhosis is commonly unrecognized and associated with hepatocellular carcinoma. Hepatol Commun. 2017;1:53-60. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 66] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 63. | Alexander M, Loomis AK, Fairburn-Beech J, van der Lei J, Duarte-Salles T, Prieto-Alhambra D, Ansell D, Pasqua A, Lapi F, Rijnbeek P, Mosseveld M, Avillach P, Egger P, Kendrick S, Waterworth DM, Sattar N, Alazawi W. Real-world data reveal a diagnostic gap in non-alcoholic fatty liver disease. BMC Med. 2018;16:130. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 125] [Cited by in RCA: 198] [Article Influence: 28.3] [Reference Citation Analysis (0)] |
| 64. | Lazarus JV, Colombo M, Cortez-Pinto H, Huang TT, Miller V, Ninburg M, Schattenberg JM, Seim L, Wong VWS, Zelber-Sagi S. NAFLD - sounding the alarm on a silent epidemic. Nat Rev Gastroenterol Hepatol. 2020;17:377-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 107] [Article Influence: 21.4] [Reference Citation Analysis (0)] |