Published online Jul 27, 2021. doi: 10.4254/wjh.v13.i7.731
Peer-review started: February 11, 2021
First decision: May 3, 2021
Revised: May 14, 2021
Accepted: July 7, 2021
Article in press: July 7, 2021
Published online: July 27, 2021
Processing time: 161 Days and 13.4 Hours
Portal hypertension (PH), a common complication of liver cirrhosis, results in development of esophageal varices. When esophageal varices rupture, they cause significant upper gastrointestinal bleeding with mortality rates up to 20% despite state-of-the-art treatment. Thus, prophylactic measures are of utmost importance to improve outcomes of patients with PH. Several high-quality studies have demonstrated that non-selective beta blockers (NSBBs) or endoscopic band ligation (EBL) are effective for primary prophylaxis of variceal bleeding. In secondary prophylaxis, a combination of NSBB + EBL should be routinely used. Once esophageal varices develop and variceal bleeding occurs, standardized treatment algorithms should be followed to minimize bleeding-associated mortality. Special attention should be paid to avoidance of overtransfusion, early initiation of vasoconstrictive therapy, prophylactic antibiotics and early endoscopic therapy. Pre-emptive transjugular intrahepatic portosystemic shunt should be used in all Child C10-C13 patients experiencing variceal bleeding, and potentially in Child B patients with active bleeding at endoscopy. The use of carvedilol, safety of NSBBs in advanced cirrhosis (i.e. with refractory ascites) and assessment of hepatic venous pressure gradient response to NSBB is discussed. In the present review, we give an overview on the rationale behind the latest guidelines and summarize key papers that have led to significant advances in the field.
Core Tip: Variceal bleeding is a severe, and often deadly, complication of portal hypertension. Screening for varices, effective bleeding prophylaxis and standardized management of bleeding is critical to improve clinical outcomes. While carvedilol seems to be the treatment of choice for primary prophylaxis in compensated cirrhosis, the use of hepatic venous pressure gradient measurements and safety of non-selective betablockers in advanced cirrhosis with refractory ascites is controversial. The pre-emptive use of transjugular intrahepatic portosystemic shunt within 72 h after variceal bleeding prevents rebleeding and mortality in Child C10-C13 patients.
- Citation: Pfisterer N, Unger LW, Reiberger T. Clinical algorithms for the prevention of variceal bleeding and rebleeding in patients with liver cirrhosis. World J Hepatol 2021; 13(7): 731-746
- URL: https://www.wjgnet.com/1948-5182/full/v13/i7/731.htm
- DOI: https://dx.doi.org/10.4254/wjh.v13.i7.731
Chronic liver diseases cause recurrent liver damage and can result in the development of liver fibrosis and, ultimately, liver cirrhosis[1]. Fibrosis and cirrhosis lead to gradually increased intrahepatic vascular resistance, splanchnic vasodilatation and increased portal blood flow, which subsequently results in increased portal pressure and the development of collaterals[2]. To allow risk stratification, evidence-based guidelines have been developed to grade portal hypertension severity, and the term clinically significant portal hypertension (CSPH) has been defined to indicate a high risk of complications[3]. CSPH is defined as a hepatic venous pressure gradient (HVPG), an invasive surrogate parameter of portal venous pressure, of ≥ 10 mmHg[4]. This definition is based on studies demonstrating that esophageal varices (EV) develop above the 10 mmHg HVPG threshold, subsequently increasing the risk of bleeding[5]. In cross sectional studies, between 40%-60% of patients with liver cirrhosis show EV, highlighting the clinical importance of this condition[6,7]. Variceal bleeding is, next to liver failure, hepatocellular carcinoma, infections and the hepatorenal syndrome, one of the main causes of mortality in patients with CSPH and adequate diagnosis as well as treatment is of utmost importance, given that variceal bleeding episodes are still associated with a high mortality rate of up to 20%[8-12]. Thus, to avoid unnecessary fatal outcomes, variceal bleeding and re-bleeding must be prevented, ideally by (primary or secondary) prophylactic treatment of portal hypertension per se. Therefore, this review focusses on clinical algorithms and summarizes the available evidence on prevention and treatment of variceal bleeding.
In patients with cirrhosis but without EVs at baseline, the incidence of developing EV rises from 5% after one year to 28% after three years, independently of liver function or compensated/decompensated liver cirrhosis[13]. In a cross-sectional study of 494 patients of which 48% had decompensated liver cirrhosis, 38% of patients had EV at the time of screening[14]. Thus, EV are common in patients with advanced chronic liver disease, and it was shown that patients with EV suffer from significantly higher mortality rates and decompensating events than patients without[14]. Of note, however, bleeding risk is correlated with HVPG values, and patients with a HVPG of ≥ 12 mmHg are at significantly higher bleeding risk than patients with < 12 mmHg, despite the diagnostic CSPH cutoff value of 10 mmHg[15,16]. Although HVPG is considered the gold standard, measurement requires specific expertise and equipment, comes at relatively high cost and is invasive. Thus, it is not considered as standard of care and not available to most centers[17]. As an alternative, transient elastography (TE) has been established as a well-validated cheap, non-invasive tool to measure liver stiffness, as fibrosis/cirrhosis severity and portal pressure directly correlate[18,19]. TE allows to classify patients with liver cirrhosis, defined as a liver stiffness measurement value > 15 kPa and can be used as screening tool[3,20]. Efforts to establish clear cutoff values have been made[21], and evidence indicates that patients with TE values < 20 kPa and platelet count > 150 G/L are unlikely to have varices (< 5%)[22]. These values can be used to avoid screening gastroscopies for EV, and the next TE screening for EV can be postponed for another year[22]. Screening gastroscopy is, however, required in patients with diagnosed liver cirrhosis who do not meet these mentioned criteria[3,17,22] and allows to identify “high risk” varices, which are referred to as “varices needing treatment” (VNT) in recent guidelines[22]. VNT are varices of large size (> 5 mm diameter) or small varices (< 5 mm diameter) with red spot signs/red wale markings, as both of them are at high risk of bleeding[22]. When VNT are detected, treatment with non-selective betablockers (NSBB) or endoscopic band ligation (EBL) should be initiated for primary prophylaxis of variceal bleeding[3,17,22].
While evidence is clear on these VNTs, current guidelines are less validated whether endoscopic screening is indicated for small varices[23]. Augustin et al[24] found that following the current Baveno VI criteria spared more screening endoscopies with a minimal risk of missing VNT, but when guidelines are followed strictly, small varices would be missed in a significant number of patients. Thus, treatment decisions in these cases should be made on a case-to-case basis until further evidence is available.
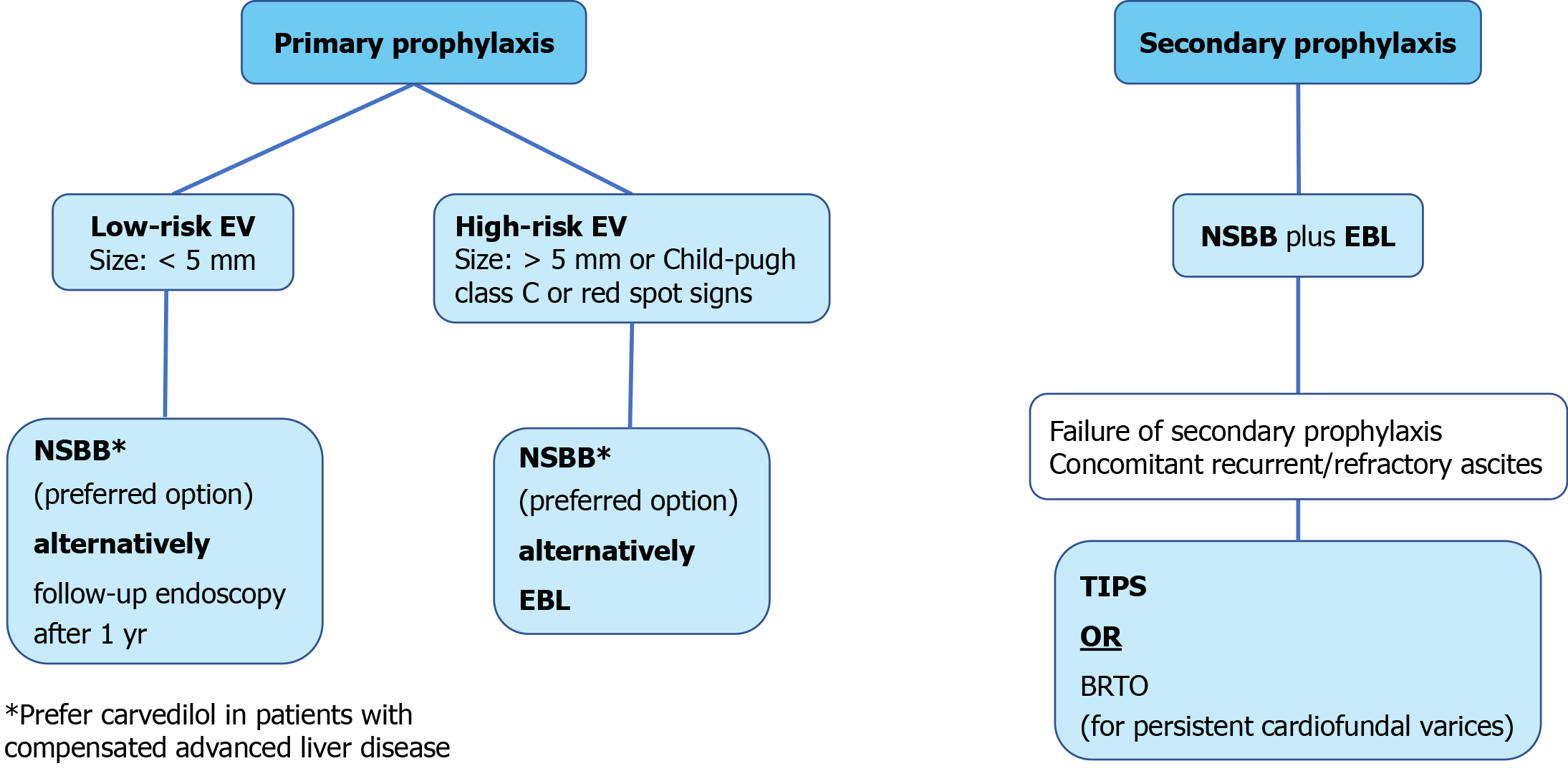
When patients with high risk EV are identified, treatment should aim to prevent variceal bleeding as primary prophylaxis. Current guidelines recommend either NSBB or EBL for prevention of first EV bleeding in patients with medium to large varices, while they do not specifically recommend treatment for small varices due to above mentioned lack of decisive studies[3,17].
While available evidence uniformly demonstrated that NSBB therapy effectively prevents first, as well as recurrent, EV bleeding and reduces mortality when EV are diagnosed[25,26], it is under debate whether NSBB should be prescribed without signs of EV. One large randomized multicenter study assigned patients with CSPH without EV to timolol or placebo and found that although HVPG was lower in timolol-treated patients, the subsequent development of EV or variceal bleeding rate did not differ between timolol or placebo treated patients[27]. Although the HVPG-response to NSBB differs in patients with or without CSPH, the results were relatively unexpected[27].
Little high-quality evidence is available regarding treatment of patients with small and low risk varices in primary prophylaxis[22,28]. It seems as if some trials were underpowered to see sufficient effects of NSBB on the incidence of first variceal bleeding in patients with small varices[23] while others demonstrated that NSBB effectively prevented the progression from small to large varices, especially in patients assigned to carvedilol[29,30]. The recently published PREDESCI trial showed that NSBB were associated with a decreased risk of decompensation [hazard ratio: 0.51 (95%CI: 0.26-0.97), P = 0.041] in patients with CSPH and low risk varices, potentially resulting in longer decompensation-free survival[31]. Taken together, the conflicting evidence led the authors of the current international guidelines to not recommend NSBB treatment for patients with no EV or for prevention of varix progression. However, some experts still recommend using NSBB in patients with cirrhosis as soon as CSPH is evident (e.g. by HVPG ≥ 10 mmHg or by any size of varices) to prevent clinical decompensation.
Prescribing NSBB for primary prophylaxis is less expensive, has no procedural risk, does not require repetition of esophageal gastroscopy after initiation of NSBB for prevention of variceal bleeding and saves time for gastroenterologists[3,17]. Therefore, NSBB are sometimes favorable compared to EBL, with dosing intensities summarized in Table 1. Beside the positive effect of NSBB on variceal bleeding (absolute risk reduction of up to -16%, NNT = 6), several studies have also demonstrated benefits that are likely mediated by their additional non-hemodynamic effects[32-35]. With regards to beta blocker selection, some trials showed a better or comparable efficacy in primary prophylaxis of carvedilol in comparison to other NSBBs, probably as carvedilol has additional anti-α-1-adrenergic activity and does therefore result in a more potent decrease of portal pressure[36-38]. Thus, carvedilol is recommended as first line therapy in some national guidelines[3,39-41]. However, carvedilol for the sole indication of portal hypertension should not be prescribed in doses above 12.5 mg per day, as higher doses (> 12.5 mg/d) do not lead to further reductions of portal pressure[36,37]. Importantly, carvedilol may be prescribed when NSBB have already failed, as our group could show that in 58% of patients who did not respond to propranolol, carvedilol still resulted in a significant HVPG response (defined as reduction of HVPG of more than 20% or reduction to a HVPG value < 12 mmHg)[36].
| Beta blocker | Initial dose | Goal | Treatment duration | Further guidance |
| Propranolol | 20–40 mg twice daily | Maximum dosage of 160 mg/day; Or until the resting heart rate of 55–60 beats/min; Maximum dosage of 80 mg/day in patients with ascites | Indefinite | Adapt every 2-3 d until optimal dose is reached; Discontinue during spontaneous bacterial peritonitis, hyponatremia (Na < 125 mmol/L) or acute kidney injury; Systolic blood pressure should not decrease below 90 mmHg; EGD for further variceal screening is not needed |
| Carvedilol | 6.25 mg once daily | Maximum dosage of 12.5 mg/day | Indefinite | Adapt dose after 3 d and increase to 6.25 mg twice daily; Discontinue during spontaneous bacterial peritonitis, hyponatremia (Na < 125mmol/L) or acute kidney injury; Systolic blood pressure should not decrease below 90 mmHg; EGD for further variceal screening is not needed; Potential switch from carvedilol to propranolol in case of new onset of ascites |
| Nadolol | 20-40 mg once daily | Maximum dosage of 160 mg/day; Or until the resting heart rate of 55–60 beats/min; Maximum dosage of 80 mg/day in patients with ascites | Indefinite | Adapt every 2-3 d until optimal dose is reached; Discontinue during spontaneous bacterial peritonitis, hyponatremia (Na < 125mmol/L) or acute kidney injury; Systolic blood pressure should not decrease below 90 mmHg; EGD for further variceal screening is not needed |
Despite the easy handling of NSBB or carvedilol, up to 15% of patients require a dose reduction or discontinuation due to common and severe side effects such as hypotension, shortness of breath and/or fatigue[42], and 15% to 25% of patients have absolute or relative contraindications for NSBB initiation[35,42]. In addition, there is a great abundance of studies comparing NSBB to EBL in primary prophylaxis, and there is no clear outcome benefit for one or the other. In a Cochrane analysis from 2012, patients who underwent EBL as primary prophylaxis showed reduced variceal bleeding rates compared to patients using NSBB alone, while bleeding did not impact on mortality[43]. Another meta-analysis demonstrated that there was no difference in bleeding rates when high-quality studies were assessed[44]. In contrast to these meta-analyses, one large multicenter study showed better efficacy of carvedilol for primary prophylaxis compared to EBL alone[41], and another meta-analysis of 32 randomized controlled trials and a total number of 3362 patients with large varices in primary prophylaxis found that NSBB monotherapy was associated with a decrease of all-cause mortality, decrease risk of first variceal bleeding and a better safety profile compare to patients treated with EBL[45]. Overall, bleeding rates in primary prophylaxis greatly vary between studies and no reproducible differences between the overall effectiveness, especially the overall- or bleeding-related mortality, could be established so far[46-49]. To address certain limitations of previous studies, another large rando
Due to vasodilating effects, sympathetic activation, increased left ventricle systolic function and, therefore, impairment of renal perfusion, several studies questioned the safety of NSBB and carvedilol in patients with decompensated cirrhosis[51-59]. This is in line with evidence that NSBBs were associated with higher mortality in patients with refractory ascites[51,60,61]. However, these findings were not uniformly confirmed and some studies report no impact on outcome[62-64]. As a result of this conflicting evidence, current guidelines suggest to monitor blood pressure, serum sodium levels and kidney function in patients with decompensated cirrhosis[3,17,22], but do not state that NSBB are contraindicated[17,22]. Nevertheless, high doses of NSBB (e.g. propranolol > 160 mg/day) should be avoided as they seem to be associ
Similar conflicting results were reported for NSBB use in patients with spontaneous bacterial peritonitis (SBP) and/or acute kidney injury[56]. In one retrospective study, NSBB use was associated with a higher risk for the development of a hepatorenal syndrome in patients with newly diagnosed SBP, resulting in impaired survival[59]. However, a more recent study suggests that NSBB maintenance during an SBP-episode is not associated with increased mortality as long as there is no severe arterial hypotension, highlighting the importance of the guideline’s recommendations to monitor blood pressure[66].
EBL has a very low procedural risk and is the most effective endoscopic choice for EV[3,17,22,67,68]. When EBL is chosen for primary prophylaxis, it should be repeated every two to four weeks until varices are completely eradicated (small “remnant” varices can be tolerated) and endoscopy should subsequently be repeated after six and twelve months[3]. If EV reappear, the treatment algorithm has to be restarted in the same intervals[3]. Compared to NSBB, EBL for primary prophylaxis has a lower overall rate of adverse events, but if adverse events occur they are more severe and life-threatening (e.g. EBL-related ulcer bleeding)[47,49,69]. Procedure related bleeding as a potential complication after EBL has been described to occur in 2%-6% of interventions[68,70-72]. In addition to potential esophageal injuries, EBL induces/ accelerates the development of gastric collaterals[73] as it does not affect the underlying cause of increased portal pressure and thus has no disease-modifying effects. In summary, however, both treatments, namely NSBB or EBL, are effective and physicians should choose individually which primary prophylaxis is used, based on patients’ concomitant risk factors and local availability. As a brief overview, we have summarized the recommended clinical algorithms in Figure 1.
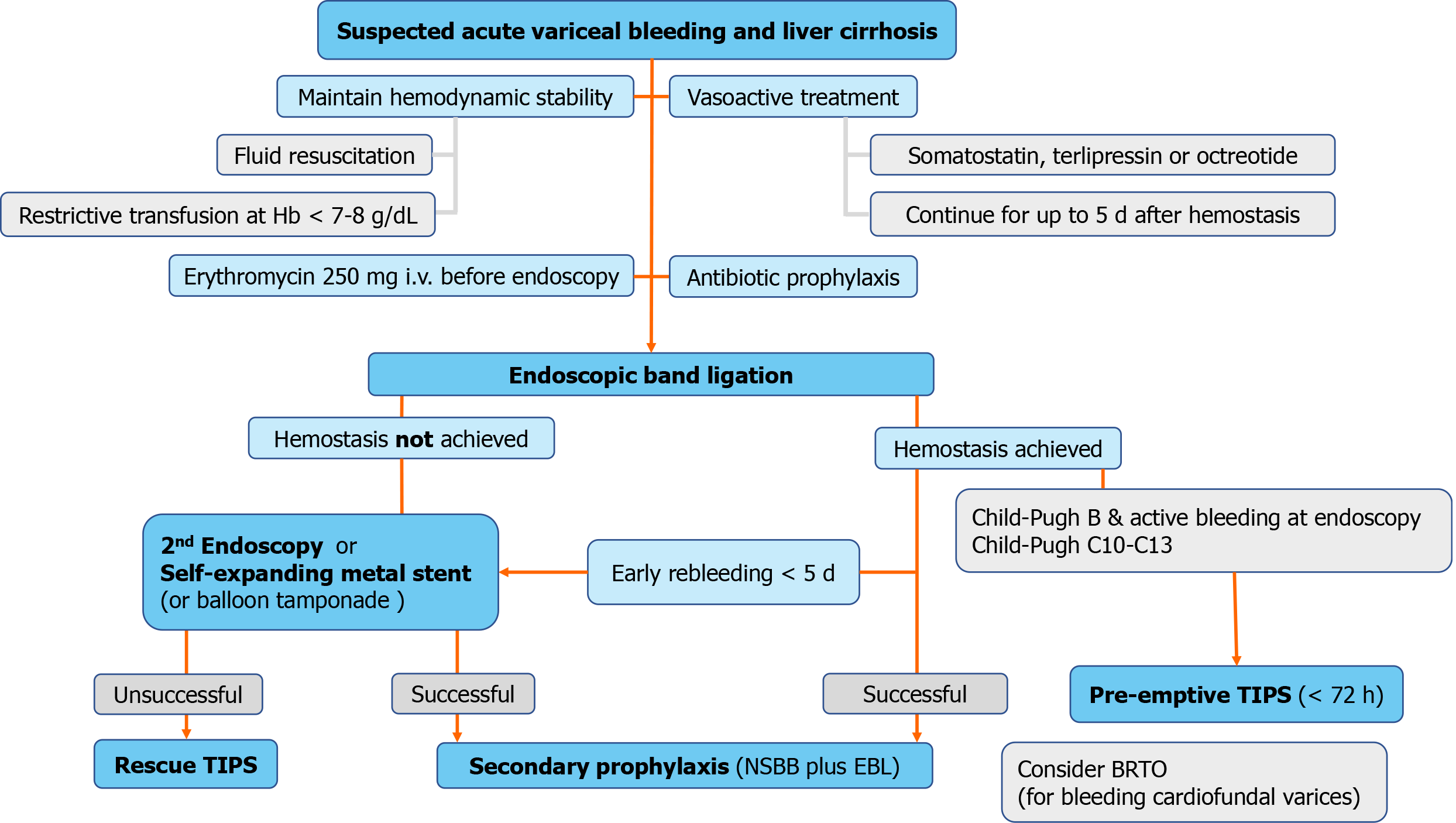
When EV are not detected in time, or if primary prophylaxis fails and acute variceal bleeding cannot be prevented, a determined and rapid treatment initiation as well as intensive care are required to optimize outcome. Despite improved mortality rates in the past decades, bleeding-related mortality remains as high as 15%-20%[9,10,12,74]. Patients presenting with acute variceal bleeding are classified as “decompensated cirrhosis”, irrespective of fibrosis severity[5,17]. Despite this classification, 5 year mortality rates are affected by the underlying fibrosis severity as complications such as ascites and/or hepatic encephalopathy also impact on overall survival[14]. Fluid resuscitation, pharmacological treatment and endoscopy/EBL are the three main pillars for acute variceal bleeding treatment (see Figure 2)[3,17,22].
Initial fluid resuscitation to counteract hemorrhagic shock is the first important step in patients with acute variceal bleeding, and packed red blood cell (PRBC) transfusions are indicated when hemoglobin levels are below 7 to 8 g/dL, as too liberal administration of PRBCs has been shown to impair outcome[3,75]. In the randomized controlled study by Villanueva et al[75], patients with “liberal” use of PRBC trans
In contrast to PRBCs, transfusion of platelets, the use of fresh frozen plasma or administration of recombinant factor VIIa to correct platelet count or international normalized ratio (INR), respectively, did not demonstrate a clear benefit and is therefore not recommended[3,17,22,76,77].
To counteract active bleeding, vasoactive drugs (vasopressin, terlipressin, somatostatin or octreotide, dosing regimens summarized in Table 2) have been shown to reduce portal pressure by reducing portal systemic collateral blood flow, portal blood flow and intravariceal pressure via systemic and splanchnic vasoconstriction[17,78,79]. Thus, they are recommended for use in patients with acute variceal bleeding, while none of the vasoactive treatments has been shown to be superior to the others in terms of bleeding control and impact on mortality[3,17,22,80,81]. Of note, however, terlipressin has been associated with hyponatremia, especially in patients with preserved liver function and sodium levels should therefore be monitored, although these systemic sodium alterations did not translate to any outcome difference[80].
| Regimen | Dosing | Duration of regimen | Further guidance |
| Somatostatin | Bolus of 500 μg, followed by 500 μg/h via continuous infusion (6 mg/50 mL, infusion rate of 4.2 mL/h) | 2-5 d | Bolus can be repeated in case of uncontrolled bleeding |
| Terlipressin | Bolus of 2mg every 4 h for the first 24-48 h, followed by giving bolus of 1mg every 4 h; Or continuous infusion 2 mg/d; maximum 12 mg/d | 2-5 d | Be caution in patients with coronary artery disease, peripheral arterial occlusive disease hyponatremia (< 125 mmol/L), cardiac arrhythmia and severe asthma or chronic occlusive pulmonary disease |
| Octreotide (somatostatin analogue) | Bolus of 50 μg, followed by 50 μg via continuous infusion | 2-5 d | Bolus can be repeated in case of uncontrolled bleeding |
In addition to fluid resuscitation and administration of vasoactive drugs, antibiotic treatment is indicated as patients with acute variceal bleeding suffer from a significant risk of infection[82]. Thus, intravenous broad spectrum antibiotics (e.g. ceftriaxone at a dose of 1g every 24 h with a duration for 7 d or less) should be administered before endoscopic therapy is initiated[3,17,22]. In addition, erythromycin should be admini
Finally, EBL is the gold standard of endoscopic treatment after hemodynamic stabilization and should ideally be performed within the first six to twelve hours of admission when EV bleeding is suspected or detected[3,17,22,84,85]. Performing endoscopists should be adequately trained, and EBL has been proven to be the best available treatment in terms of rebleeding, further development of esophageal strictures, and associated mortality[86].
Recently, however, data suggests that instead of vasoactive drugs and endoscopic therapy, preemptive implantation of a transjugular intrahepatic portosystemic shunt (TIPS) to lower portal pressure can be effective. An international multicenter observational study compared pre-emptive TIPS to endoscopy plus vasoactive drugs in patients with Child-Pugh C or Child Pugh B cirrhosis with active bleeding at the time of endoscopy[87]. The authors found that pre-emptive TIPS implantation, compared to standard of care with medication and endoscopic treatment, significantly reduced treatment failure and rebleeding in Child-Pugh C, and Child-Pugh B patients with active bleeding. This translated into a significantly lower mortality rate in Child-Pugh C patients, while mortality in Child-Pugh B patients with active bleeding were low in both, EBL/medication and TIPS, groups and did not improve by pre-emptive TIPS implantation[87]. Thus, pre-emptive TIPS implantation emerges as a valid option in patients with high risk of rebleeding, especially in Child-Pugh C patients.
These favorable results are in line with findings in patients with therapy refractory acute variceal bleeding in which rescue-TIPS implantation is the best choice when standard treatment fails[3,17,22]. Rescue-TIPS, e.g. TIPS implantation after EBL failure to control bleeding, achieves bleeding control in 90%-100% and results in very low rebleeding rates of approximately 15%[88]. However, despite the available encou
As these high complication rates are considered unacceptable in modern medicine, a self-expanding metal stent (SEMS), SX-ELLA Stent Danis, has been developed to improve procedure related complication rates. It can easily be deployed without endoscopic guidance and can be left in situ for up to seven days. Several studies showed successful bleeding control in 70%-100% of patients[99-101] with lower complication rates than balloon tamponade, although this did not improve mortality rates[102,103]. Current guidelines nevertheless recommend the use of SEMS because of its better safety profile[3,17,22].
On the basis of these poor outcome data, balloon tamponade and SEMS are usually only used as a bridging to further definitive therapy, such as TIPS implantation. Despite this large body of favorable evidence, however, we recently reported a lack of systematic use of TIPS implantation after SEMS in acute variceal bleeding[101]. This is in line with recently published real-life data from France which showed that approximately 1/3 of patients with variceal bleeding fulfilled the criteria for early TIPS, but only 7% underwent subsequent early TIPS implantation[90]. This knowledge gap on TIPS indication criteria was also evident in our recently published survey in which only 20% of the respondents could report TIPS criteria correctly[104]. Therefore, knowledge on early TIPS implantation must be improved among all specialists.
Furthermore, in case of additional cardiofundal variceal bleeding and/or ongoing variceal bleeding after TIPS implantation, balloon occluded retrograde transvenous variceal obliteration (BRTO) should be considered[3,105-107]. A recently published meta-analysis showed improved outcome in terms of rebleeding, mortality and hepatic encephalopathy in patients who also underwent BRTO as compared to patients who only underwent TIPS implantation[106].
Secondary prophylaxis is defined as the prevention of recurrent variceal bleeding. Patients who survive and recover from an episode of acute variceal bleeding are at high risk of rebleeding and death, which is 60% and 33% in the first year, respectively[17,108]. Older studies found that HVPG measurement at the time of the first bleeding episode can predict rebleeding risk, and a HVPG of ≥ 20 mmHg was associated with a significantly increased risk for rebleeding and death[109]. Despite several non-invasive scores (APRI, FIB-4, AST/ALT, King´s score) are available, their role as non-invasive predictors for the presence of esophageal varices in patients with cirrhosis is not established. Kraja et al[110] showed that the FIB-4 is a powerful predictor of EV (cut off value: 3.23; AUC: 0.66, 95%CI: 0.54-0.78) but a poor predictor for EV bleeding (AUC: 0.42, 95%CI: 0.28-0.56) and that all other non-invasive biomarkers were not useful. This is in line with several other available studies that showed great variation in accuracy in different populations and etiologies of liver cirrhosis[111-113]. Recently, Drolz et al[68] reported high bilirubin and larger size varices as risk factors for rebleeding within 30 d of prophylactic EBL, while reduced platelet counts, elevated INR, and decreased fibrinogen levels were associated with procedure-related bleeding in other studies[113-115]. Another study showed an adequate prediction value for predicting in-hospital rebleeding using Child-Turcotte-Pugh score (cut off > 7) and Clinical Rockall score (cut off > 2)[116], while the well-established MELD and MELD-Na scores showed good results for predicting in-hospital mortality[116]. Thus, non-invasive prognostic scoring systems cannot be recommended to predict risk for recurrent variceal bleeding but are useful tools to estimate overall mortality rates[116-118].
In terms of secondary prophylaxis to avoid rebleeding, monotherapy of NSBB or EBL are associated with higher mortality in secondary prophylaxis than combined NSBB + EBL therapy, which is in contrast to studies in the primary prophylaxis setting[35]. Thus, current guidelines recommend the combination of EBL + NSBBs[3,17,22,119,120], while the combined treatment of NSBB and low-dose isosorbide mononitrate, a combination used in the past, is no longer recommended due to high rates of adverse events[3,17,22].
With regard to NSBB choice, propranolol is recommended at a daily dosage of 80–160 mg/day in most guidelines, with a maximum dosing of 80 mg/day in patients with ascites[3]. Similar to primary prophylaxis, some guidelines also recommend carvedilol, while others do not (yet) recommend its general use[17,22]. Guidelines that do recommend carvedilol suggest to use it at a concentration of 6.25–12.5 mg/day and only in patients without ascites[3]. Finally, with regards to EBL for secondary prophylaxis, endoscopy and banding intervals are equal to the intervals in primary prophylaxis (complete eradication, re-endoscopy after 6 and 12 mo).
Similarly, when first-line therapy with EBL + NSBB to prevent rebleeding fails, TIPS implantation is the best choice for further treatment[3,17,22], as it decreases portal pressure and therefore targets the underlying cause of EV bleeding. Of note, however, no significant benefit on survival rates was found despite the better outcomes in terms of rebleeding rates[15,126,122]. In patients with gastric varices and contraindications for TIPS implantation such as spontaneous episodes of hepatic encephalopathy, BRTO can be considered as treatment option in selected patients, as it may even decrease portosystemic shunting through the collaterals that are scheduled for occlusion[3]. Furthermore, surgical shunts, devascularization, splenectomy or (partial) splenic embolization may be considered if first-line treatments fail[3].
The continuous efforts of hepatologists and gastroenterologists around the world, as well as initiatives of international collaborations to generate high-quality evidence has translated to improved survival in patients with EV bleeding in the last decades. Thus, we have summarized recent advances and highlighted the rationale for specific treatments now recommended by several national and international guidelines.
In primary prophylaxis, NSBB or EBL are equal in outcomes and are therefore both recommended as monotherapies to prevent a first variceal bleeding event[3,17,22]. However, carvedilol – due to its higher potency to lower portal pressure[36] resulting in higher proportions of HVPG responders – may be the treatment of choice for primary prophylaxis in compensated cirrhosis. No clear recommendation for the use of betablockers can be made for patients with small varices (even with additional risk factors), as their efficacy in this setting remains unclear. Importantly, due to non-hemodynamic effects of NSBBs on intestinal permeability[34], systemic inflammation[124] and considering the results of the recent PREDESCI trial[31] showing reduced risk of decompensation and mortality, NSBB may already be recommended for small varices.
To monitor NSBB treatment response, invasive HVPG measurement is still considered as gold standard, but other non-invasive surrogates to monitor NSBB response to prevent variceal bleeding such as ultrasound-based elastography or transient elastography assessment of the spleen are currently under consideration as HVPG measurement is not widely available[125,126].
When acute variceal bleeding occurs, standardized treatment algorithms recommend conservative transfusion strategies, early initiation of vasoactive drugs, prophylactic antibiotics, and EBL[3,17,22]. More recently, the pre-emptive use of TIPS implantation in selected high-risk patients with variceal bleeding has been demonstrated to not only decrease rebleeding rates but also mortality[3,17,22,127,128].
Due to logistic challenges with the “time-critical” use of pre-emptive TIPS implantation, specialist should be familiar with this concept and infrastructure and networks need to be developed in order to improve the outcomes of patients with variceal bleeding.
In secondary prophylaxis, the combination of NSBB and EBL has proven to be superior to either monotherapy[3,17,22].
In conclusion, NSBBs remain the cornerstone of medical therapy of portal hypertension and are still used for pharmacological bleeding prophylaxis. EBL may also be used for primary prophylaxis, but its main role is in effective control of acute variceal bleeding and variceal eradication in secondary prophylaxis. Standardized concepts and the infrastructure for the general use of pre-emptive TIPS in selected patients with high-risk variceal bleeding need to be developed. This review should have provided clinicians with valuable concepts for the management of PH, including variceal screening, primary bleeding prophylaxis, management of acute variceal bleeding and finally effective secondary prevention of variceal rebleeding.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Austria
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Zhao H S-Editor: Zhang H L-Editor: A P-Editor: Wang LL
| 1. | Trautwein C, Friedman SL, Schuppan D, Pinzani M. Hepatic fibrosis: Concept to treatment. J Hepatol. 2015;62:S15-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 439] [Cited by in RCA: 518] [Article Influence: 51.8] [Reference Citation Analysis (0)] |
| 2. | García-Pagán JC, Gracia-Sancho J, Bosch J. Functional aspects on the pathophysiology of portal hypertension in cirrhosis. J Hepatol. 2012;57:458-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 207] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 3. | Reiberger T, Püspök A, Schoder M, Baumann-Durchschein F, Bucsics T, Datz C, Dolak W, Ferlitsch A, Finkenstedt A, Graziadei I, Hametner S, Karnel F, Krones E, Maieron A, Mandorfer M, Peck-Radosavljevic M, Rainer F, Schwabl P, Stadlbauer V, Stauber R, Tilg H, Trauner M, Zoller H, Schöfl R, Fickert P. Austrian consensus guidelines on the management and treatment of portal hypertension (Billroth III). Wien Klin Wochenschr. 2017;129:135-158. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 82] [Cited by in RCA: 103] [Article Influence: 12.9] [Reference Citation Analysis (2)] |
| 4. | Iwakiri Y. Pathophysiology of portal hypertension. Clin Liver Dis. 2014;18:281-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 193] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 5. | Garcia-Tsao G, Bosch J. Management of varices and variceal hemorrhage in cirrhosis. N Engl J Med. 2010;362:823-832. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 639] [Cited by in RCA: 640] [Article Influence: 42.7] [Reference Citation Analysis (0)] |
| 6. | Garcia-Pagan JC, De Gottardi A, Bosch J. Review article: the modern management of portal hypertension--primary and secondary prophylaxis of variceal bleeding in cirrhotic patients. Aliment Pharmacol Ther. 2008;28:178-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 47] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | D'Amico G, Luca A. Natural history. Clinical-haemodynamic correlations. Prediction of the risk of bleeding. Baillieres Clin Gastroenterol. 1997;11:243-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 144] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 8. | Reverter E, Tandon P, Augustin S, Turon F, Casu S, Bastiampillai R, Keough A, Llop E, González A, Seijo S, Berzigotti A, Ma M, Genescà J, Bosch J, García-Pagán JC, Abraldes JG. A MELD-based model to determine risk of mortality among patients with acute variceal bleeding. Gastroenterology. 2014;146:412-419.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 268] [Article Influence: 24.4] [Reference Citation Analysis (0)] |
| 9. | Stokkeland K, Brandt L, Ekbom A, Hultcrantz R. Improved prognosis for patients hospitalized with esophageal varices in Sweden 1969-2002. Hepatology. 2006;43:500-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 85] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 10. | Jairath V, Rehal S, Logan R, Kahan B, Hearnshaw S, Stanworth S, Travis S, Murphy M, Palmer K, Burroughs A. Acute variceal haemorrhage in the United Kingdom: patient characteristics, management and outcomes in a nationwide audit. Dig Liver Dis. 2014;46:419-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 72] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 11. | D'Amico G, De Franchis R; Cooperative Study Group. Upper digestive bleeding in cirrhosis. Post-therapeutic outcome and prognostic indicators. Hepatology. 2003;38:599-612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 585] [Cited by in RCA: 597] [Article Influence: 27.1] [Reference Citation Analysis (0)] |
| 12. | Cerqueira RM, Andrade L, Correia MR, Fernandes CD, Manso MC. Risk factors for in-hospital mortality in cirrhotic patients with oesophageal variceal bleeding. Eur J Gastroenterol Hepatol. 2012;24:551-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 13. | Merli M, Nicolini G, Angeloni S, Rinaldi V, De Santis A, Merkel C, Attili AF, Riggio O. Incidence and natural history of small esophageal varices in cirrhotic patients. J Hepatol. 2003;38:266-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 349] [Cited by in RCA: 341] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 14. | D'Amico G, Pasta L, Morabito A, D'Amico M, Caltagirone M, Malizia G, Tinè F, Giannuoli G, Traina M, Vizzini G, Politi F, Luca A, Virdone R, Licata A, Pagliaro L. Competing risks and prognostic stages of cirrhosis: a 25-year inception cohort study of 494 patients. Aliment Pharmacol Ther. 2014;39:1180-1193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 304] [Cited by in RCA: 373] [Article Influence: 33.9] [Reference Citation Analysis (1)] |
| 15. | Bosch J, García-Pagán JC. Prevention of variceal rebleeding. Lancet. 2003;361:952-954. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 309] [Cited by in RCA: 288] [Article Influence: 13.1] [Reference Citation Analysis (2)] |
| 16. | Brunner F, Berzigotti A, Bosch J. Prevention and treatment of variceal haemorrhage in 2017. Liver Int. 2017;37 Suppl 1:104-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 48] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 17. | Garcia-Tsao G, Abraldes JG, Berzigotti A, Bosch J. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology. 2017;65:310-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1108] [Cited by in RCA: 1441] [Article Influence: 180.1] [Reference Citation Analysis (3)] |
| 18. | Kim MY, Cho MY, Baik SK, Park HJ, Jeon HK, Im CK, Won CS, Kim JW, Kim HS, Kwon SO, Eom MS, Cha SH, Kim YJ, Chang SJ, Lee SS. Histological subclassification of cirrhosis using the Laennec fibrosis scoring system correlates with clinical stage and grade of portal hypertension. J Hepatol. 2011;55:1004-1009. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 136] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 19. | Friedrich-Rust M, Ong MF, Martens S, Sarrazin C, Bojunga J, Zeuzem S, Herrmann E. Performance of transient elastography for the staging of liver fibrosis: a meta-analysis. Gastroenterology. 2008;134:960-974. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1046] [Cited by in RCA: 1077] [Article Influence: 63.4] [Reference Citation Analysis (1)] |
| 20. | Castera L, Pinzani M, Bosch J. Non invasive evaluation of portal hypertension using transient elastography. J Hepatol. 2012;56:696-703. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 236] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 21. | Paternostro R, Reiberger T, Bucsics T. Elastography-based screening for esophageal varices in patients with advanced chronic liver disease. World J Gastroenterol. 2019;25:308-329. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 45] [Cited by in RCA: 48] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 22. | de Franchis R; Baveno VI Faculty. Expanding consensus in portal hypertension: Report of the Baveno VI Consensus Workshop: Stratifying risk and individualizing care for portal hypertension. J Hepatol. 2015;63:743-752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2011] [Cited by in RCA: 2294] [Article Influence: 229.4] [Reference Citation Analysis (3)] |
| 23. | Reiberger T, Bucsics T, Paternostro R, Pfisterer N, Riedl F, Mandorfer M. Small Esophageal Varices in Patients with Cirrhosis-Should We Treat Them? Curr Hepatol Rep. 2018;17:301-315. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 24. | Augustin S, Pons M, Maurice JB, Bureau C, Stefanescu H, Ney M, Blasco H, Procopet B, Tsochatzis E, Westbrook RH, Bosch J, Berzigotti A, Abraldes JG, Genescà J. Expanding the Baveno VI criteria for the screening of varices in patients with compensated advanced chronic liver disease. Hepatology. 2017;66:1980-1988. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 224] [Cited by in RCA: 204] [Article Influence: 25.5] [Reference Citation Analysis (0)] |
| 25. | Poynard T, Calès P, Pasta L, Ideo G, Pascal JP, Pagliaro L, Lebrec D. Beta-adrenergic-antagonist drugs in the prevention of gastrointestinal bleeding in patients with cirrhosis and esophageal varices. An analysis of data and prognostic factors in 589 patients from four randomized clinical trials. Franco-Italian Multicenter Study Group. N Engl J Med. 1991;324:1532-1538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 376] [Cited by in RCA: 312] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 26. | Pagliaro L. Lebrec D, Poynard T, Hillon P, Benhamou J-P. Propranolol for prevention of recurrent gastrointestinal bleeding in patients with cirrhosis. A controlled study [N Engl J Med 1981;305:1371-1374]. J Hepatol. 2002;36:148-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 27. | Groszmann RJ, Garcia-Tsao G, Bosch J, Grace ND, Burroughs AK, Planas R, Escorsell A, Garcia-Pagan JC, Patch D, Matloff DS, Gao H, Makuch R; Portal Hypertension Collaborative Group. Beta-blockers to prevent gastroesophageal varices in patients with cirrhosis. N Engl J Med. 2005;353:2254-2261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 714] [Cited by in RCA: 653] [Article Influence: 32.7] [Reference Citation Analysis (1)] |
| 28. | Tripathi D, Stanley AJ, Hayes PC, Patch D, Millson C, Mehrzad H, Austin A, Ferguson JW, Olliff SP, Hudson M, Christie JM; Clinical Services and Standards Committee of the British Society of Gastroenterology. U.K. guidelines on the management of variceal haemorrhage in cirrhotic patients. Gut. 2015;64:1680-1704. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 454] [Cited by in RCA: 416] [Article Influence: 41.6] [Reference Citation Analysis (2)] |
| 29. | Bhardwaj A, Kedarisetty CK, Vashishtha C, Bhadoria AS, Jindal A, Kumar G, Choudhary A, Shasthry SM, Maiwall R, Kumar M, Bhatia V, Sarin SK. Carvedilol delays the progression of small oesophageal varices in patients with cirrhosis: a randomised placebo-controlled trial. Gut. 2017;66:1838-1843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 62] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 30. | Merkel C, Marin R, Angeli P, Zanella P, Felder M, Bernardinello E, Cavallarin G, Bolognesi M, Donada C, Bellini B, Torboli P, Gatta A; Gruppo Triveneto per l'Ipertensione Portale. A placebo-controlled clinical trial of nadolol in the prophylaxis of growth of small esophageal varices in cirrhosis. Gastroenterology. 2004;127:476-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 198] [Cited by in RCA: 167] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 31. | Villanueva C, Albillos A, Genescà J, Garcia-Pagan JC, Calleja JL, Aracil C, Bañares R, Morillas RM, Poca M, Peñas B, Augustin S, Abraldes JG, Alvarado E, Torres F, Bosch J. β blockers to prevent decompensation of cirrhosis in patients with clinically significant portal hypertension (PREDESCI): a randomised, double-blind, placebo-controlled, multicentre trial. Lancet. 2019;393:1597-1608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 248] [Cited by in RCA: 451] [Article Influence: 75.2] [Reference Citation Analysis (0)] |
| 32. | D'Amico G, Pagliaro L, Bosch J. Pharmacological treatment of portal hypertension: an evidence-based approach. Semin Liver Dis. 1999;19:475-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 600] [Cited by in RCA: 484] [Article Influence: 18.6] [Reference Citation Analysis (1)] |
| 33. | Krag A, Wiest R, Albillos A, Gluud LL. The window hypothesis: haemodynamic and non-haemodynamic effects of β-blockers improve survival of patients with cirrhosis during a window in the disease. Gut. 2012;61:967-969. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 158] [Article Influence: 12.2] [Reference Citation Analysis (1)] |
| 34. | Reiberger T, Ferlitsch A, Payer BA, Mandorfer M, Heinisch BB, Hayden H, Lammert F, Trauner M, Peck-Radosavljevic M, Vogelsang H; Vienna Hepatic Hemodynamic Lab. Non-selective betablocker therapy decreases intestinal permeability and serum levels of LBP and IL-6 in patients with cirrhosis. J Hepatol. 2013;58:911-921. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 255] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 35. | Pfisterer N, Dexheimer C, Fuchs EM, Bucsics T, Schwabl P, Mandorfer M, Gessl I, Sandrieser L, Baumann L, Riedl F, Scheiner B, Pachofszky T, Dolak W, Schrutka-Kölbl C, Ferlitsch A, Schöniger-Hekele M, Peck-Radosavljevic M, Trauner M, Madl C, Reiberger T. Betablockers do not increase efficacy of band ligation in primary prophylaxis but they improve survival in secondary prophylaxis of variceal bleeding. Aliment Pharmacol Ther. 2018;47:966-979. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 36. | Reiberger T, Ulbrich G, Ferlitsch A, Payer BA, Schwabl P, Pinter M, Heinisch BB, Trauner M, Kramer L, Peck-Radosavljevic M; Vienna Hepatic Hemodynamic Lab. Carvedilol for primary prophylaxis of variceal bleeding in cirrhotic patients with haemodynamic non-response to propranolol. Gut. 2013;62:1634-1641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 230] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 37. | Sinagra E, Perricone G, D'Amico M, Tinè F, D'Amico G. Systematic review with meta-analysis: the haemodynamic effects of carvedilol compared with propranolol for portal hypertension in cirrhosis. Aliment Pharmacol Ther. 2014;39:557-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 105] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 38. | Schwarzer R, Kivaranovic D, Paternostro R, Mandorfer M, Reiberger T, Trauner M, Peck-Radosavljevic M, Ferlitsch A. Carvedilol for reducing portal pressure in primary prophylaxis of variceal bleeding: a dose-response study. Aliment Pharmacol Ther. 2018;47:1162-1169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 39] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 39. | Bañares R, Moitinho E, Matilla A, García-Pagán JC, Lampreave JL, Piera C, Abraldes JG, De Diego A, Albillos A, Bosch J. Randomized comparison of long-term carvedilol and propranolol administration in the treatment of portal hypertension in cirrhosis. Hepatology. 2002;36:1367-1373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 75] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 40. | Hobolth L, Møller S, Grønbæk H, Roelsgaard K, Bendtsen F, Feldager Hansen E. Carvedilol or propranolol in portal hypertension? Scand J Gastroenterol. 2012;47:467-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 41. | Shah HA, Azam Z, Rauf J, Abid S, Hamid S, Jafri W, Khalid A, Ismail FW, Parkash O, Subhan A, Munir SM. Carvedilol vs. esophageal variceal band ligation in the primary prophylaxis of variceal hemorrhage: a multicentre randomized controlled trial. J Hepatol. 2014;60:757-764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 71] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 42. | Longacre AV, Imaeda A, Garcia-Tsao G, Fraenkel L. A pilot project examining the predicted preferences of patients and physicians in the primary prophylaxis of variceal hemorrhage. Hepatology. 2008;47:169-176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 53] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 43. | Gluud LL, Krag A. Banding ligation versus beta-blockers for primary prevention in oesophageal varices in adults. Cochrane Database Syst Rev. 2012;CD004544. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 73] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 44. | Li L, Yu C, Li Y. Endoscopic band ligation versus pharmacological therapy for variceal bleeding in cirrhosis: a meta-analysis. Can J Gastroenterol. 2011;25:147-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 48] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 45. | Sharma M, Singh S, Desai V, Shah VH, Kamath PS, Murad MH, Simonetto DA. Comparison of Therapies for Primary Prevention of Esophageal Variceal Bleeding: A Systematic Review and Network Meta-analysis. Hepatology. 2019;69:1657-1675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 71] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 46. | Funakoshi N, Duny Y, Valats JC, Ségalas-Largey F, Flori N, Bismuth M, Daurès JP, Blanc P. Meta-analysis: beta-blockers versus banding ligation for primary prophylaxis of esophageal variceal bleeding. Ann Hepatol. 2012;11:369-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 37] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 47. | Sarin SK, Wadhawan M, Agarwal SR, Tyagi P, Sharma BC. Endoscopic variceal ligation plus propranolol versus endoscopic variceal ligation alone in primary prophylaxis of variceal bleeding. Am J Gastroenterol. 2005;100:797-804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 107] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 48. | Bonilha DQ, Lenz L, Correia LM, Rodrigues RA, de Paulo GA, Ferrari AP, Della Libera E. Propranolol associated with endoscopic band ligation reduces recurrence of esophageal varices for primary prophylaxis of variceal bleeding: a randomized-controlled trial. Eur J Gastroenterol Hepatol. 2015;27:84-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 49. | Lo GH, Chen WC, Wang HM, Lee CC. Controlled trial of ligation plus nadolol versus nadolol alone for the prevention of first variceal bleeding. Hepatology. 2010;52:230-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 50. | Tripathi D, Hayes PC, Richardson P, Rowe I, Ferguson J, Devine P, Mathers J, Poyner C, Jowett S, Handley K, Grant M, Slinn G, Ahmed K, Brocklehurst P. Study protocol for a randomised controlled trial of carvedilol versus variceal band ligation in primary prevention of variceal bleeding in liver cirrhosis (CALIBRE trial). BMJ Open Gastroenterol. 2019;6:e000290. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 51. | Sersté T, Melot C, Francoz C, Durand F, Rautou PE, Valla D, Moreau R, Lebrec D. Deleterious effects of beta-blockers on survival in patients with cirrhosis and refractory ascites. Hepatology. 2010;52:1017-1022. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 372] [Cited by in RCA: 376] [Article Influence: 25.1] [Reference Citation Analysis (1)] |
| 52. | Sinha R, Lockman KA, Mallawaarachchi N, Robertson M, Plevris JN, Hayes PC. Carvedilol use is associated with improved survival in patients with liver cirrhosis and ascites. J Hepatol. 2017;67:40-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 76] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 53. | Kalambokis GN, Baltayiannis G, Christou L, Christodoulou D. Red signs and not severity of cirrhosis should determine non-selective β-blocker treatment in Child-Pugh C cirrhosis with small varices: increased risk of hepatorenal syndrome and death beyond 6 months of propranolol use. Gut. 2016;65:1228-1230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 54. | Njei B, McCarty TR, Garcia-Tsao G. Beta-blockers in patients with cirrhosis and ascites: type of beta-blocker matters. Gut. 2016;65:1393-1394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 55. | Mookerjee RP, Pavesi M, Thomsen KL, Mehta G, Macnaughtan J, Bendtsen F, Coenraad M, Sperl J, Gines P, Moreau R, Arroyo V, Jalan R; CANONIC Study Investigators of the EASL-CLIF Consortium. Treatment with non-selective beta blockers is associated with reduced severity of systemic inflammation and improved survival of patients with acute-on-chronic liver failure. J Hepatol. 2016;64:574-582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 184] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 56. | Reiberger T, Mandorfer M. Beta adrenergic blockade and decompensated cirrhosis. J Hepatol. 2017;66:849-859. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 112] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 57. | Téllez L, Ibáñez-Samaniego L, Pérez Del Villar C, Yotti R, Martínez J, Carrión L, Rodríguez de Santiago E, Rivera M, González-Mansilla A, Pastor Ó, Bermejo J, Bañares R, Albillos A. Non-selective beta-blockers impair global circulatory homeostasis and renal function in cirrhotic patients with refractory ascites. J Hepatol. 2020;73:1404-1414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 73] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 58. | Giannelli V, Roux O, Laouénan C, Manchon P, Ausloos F, Bachelet D, Rautou PE, Weiss E, Moreau R, Mebazaa A, Cohen-Solal A, Durand F, Francoz C. Impact of cardiac function, refractory ascites and beta blockers on the outcome of patients with cirrhosis listed for liver transplantation. J Hepatol. 2020;72:463-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 38] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 59. | Mandorfer M, Bota S, Schwabl P, Bucsics T, Pfisterer N, Kruzik M, Hagmann M, Blacky A, Ferlitsch A, Sieghart W, Trauner M, Peck-Radosavljevic M, Reiberger T. Nonselective β blockers increase risk for hepatorenal syndrome and death in patients with cirrhosis and spontaneous bacterial peritonitis. Gastroenterology. 2014;146:1680-1690.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 280] [Cited by in RCA: 280] [Article Influence: 25.5] [Reference Citation Analysis (0)] |
| 60. | Sersté T, Francoz C, Durand F, Rautou PE, Melot C, Valla D, Moreau R, Lebrec D. Beta-blockers cause paracentesis-induced circulatory dysfunction in patients with cirrhosis and refractory ascites: a cross-over study. J Hepatol. 2011;55:794-799. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 137] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 61. | Alvarado-Tapias E, Ardevol A, Garcia-Guix M, Montañés R, Pavel O, Cuyas B, Graupera I, Brujats A, Vilades D, Colomo A, Poca M, Torras X, Guarner C, Concepción M, Aracil C, Torres F, Villanueva C. Short-term hemodynamic effects of β-blockers influence survival of patients with decompensated cirrhosis. J Hepatol. 2020;73: 829-841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 44] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 62. | Leithead JA, Rajoriya N, Tehami N, Hodson J, Gunson BK, Tripathi D, Ferguson JW. Non-selective β-blockers are associated with improved survival in patients with ascites listed for liver transplantation. Gut. 2015;64:1111-1119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 140] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 63. | Bang UC, Benfield T, Hyldstrup L, Jensen JE, Bendtsen F. Effect of propranolol on survival in patients with decompensated cirrhosis: a nationwide study based Danish patient registers. Liver Int. 2016;36:1304-1312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 63] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 64. | Bossen L, Krag A, Vilstrup H, Watson H, Jepsen P. Nonselective β-blockers do not affect mortality in cirrhosis patients with ascites: Post Hoc analysis of three randomized controlled trials with 1198 patients. Hepatology. 2016;63:1968-1976. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 95] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 65. | Madsen BS, Nielsen KF, Fialla AD, Krag A. Keep the sick from harm in spontaneous bacterial peritonitis: Dose of beta blockers matters. J Hepatol. 2016;64:1455-1456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 66. | Tergast TL, Kimmann M, Laser H, Gerbel S, Manns MP, Cornberg M, Maasoumy B. Systemic arterial blood pressure determines the therapeutic window of non-selective beta blockers in decompensated cirrhosis. Aliment Pharmacol Ther. 2019;50:696-706. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 52] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 67. | Dai C, Liu WX, Jiang M, Sun MJ. Endoscopic variceal ligation compared with endoscopic injection sclerotherapy for treatment of esophageal variceal hemorrhage: a meta-analysis. World J Gastroenterol. 2015;21:2534-2541. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 96] [Cited by in RCA: 85] [Article Influence: 8.5] [Reference Citation Analysis (1)] |
| 68. | Drolz A, Schramm C, Seiz O, Groth S, Vettorazzi E, Horvatits T, Wehmeyer MH, Goeser T, Roesch T, Lohse AW, Kluwe J. Risk factors associated with bleeding after prophylactic endoscopic variceal ligation in cirrhosis. Endoscopy. 2021;53:226-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 69. | Sinclair M, Vaughan R, Angus PW, Gow PJ, Parker F, Hey P, Efthymiou M. Risk factors for band-induced ulcer bleeding after prophylactic and therapeutic endoscopic variceal band ligation. Eur J Gastroenterol Hepatol. 2015;27:928-932. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 70. | Sarin SK, Govil A, Jain AK, Guptan RC, Issar SK, Jain M, Murthy NS. Prospective randomized trial of endoscopic sclerotherapy versus variceal band ligation for esophageal varices: influence on gastropathy, gastric varices and variceal recurrence. J Hepatol. 1997;26:826-832. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 141] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 71. | Shaheen NJ, Stuart E, Schmitz SM, Mitchell KL, Fried MW, Zacks S, Russo MW, Galanko J, Shrestha R. Pantoprazole reduces the size of postbanding ulcers after variceal band ligation: a randomized, controlled trial. Hepatology. 2005;41:588-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 129] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 72. | Stiegmann GV, Goff JS, Michaletz-Onody PA, Korula J, Lieberman D, Saeed ZA, Reveille RM, Sun JH, Lowenstein SR. Endoscopic sclerotherapy as compared with endoscopic ligation for bleeding esophageal varices. N Engl J Med. 1992;326:1527-1532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 504] [Cited by in RCA: 415] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 73. | Seno H, Konishi Y, Wada M, Fukui H, Okazaki K, Chiba T. Improvement of collateral vessels in the vicinity of gastric cardia after endoscopic variceal ligation therapy for esophageal varices. Clin Gastroenterol Hepatol. 2004;2:400-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 74. | Carbonell N, Pauwels A, Serfaty L, Fourdan O, Lévy VG, Poupon R. Improved survival after variceal bleeding in patients with cirrhosis over the past two decades. Hepatology. 2004;40:652-659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 568] [Cited by in RCA: 527] [Article Influence: 25.1] [Reference Citation Analysis (0)] |
| 75. | Villanueva C, Colomo A, Bosch A, Concepción M, Hernandez-Gea V, Aracil C, Graupera I, Poca M, Alvarez-Urturi C, Gordillo J, Guarner-Argente C, Santaló M, Muñiz E, Guarner C. Transfusion strategies for acute upper gastrointestinal bleeding. N Engl J Med. 2013;368:11-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1186] [Cited by in RCA: 1069] [Article Influence: 89.1] [Reference Citation Analysis (0)] |
| 76. | Bosch J, Thabut D, Bendtsen F, D'Amico G, Albillos A, González Abraldes J, Fabricius S, Erhardtsen E, de Franchis R; European Study Group on rFVIIa in UGI Haemorrhage. Recombinant factor VIIa for upper gastrointestinal bleeding in patients with cirrhosis: a randomized, double-blind trial. Gastroenterology. 2004;127:1123-1130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 301] [Cited by in RCA: 260] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 77. | Bosch J, Thabut D, Albillos A, Carbonell N, Spicak J, Massard J, D'Amico G, Lebrec D, de Franchis R, Fabricius S, Cai Y, Bendtsen F; International Study Group on rFVIIa in UGI Hemorrhage. Recombinant factor VIIa for variceal bleeding in patients with advanced cirrhosis: A randomized, controlled trial. Hepatology. 2008;47:1604-1614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 226] [Cited by in RCA: 190] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 78. | Seo YS. Prevention and management of gastroesophageal varices. Clin Mol Hepatol. 2018;24:20-42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 70] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 79. | Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W; Practice Guidelines Committee of the American Association for the Study of Liver Diseases; Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007;46:922-938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1229] [Cited by in RCA: 1210] [Article Influence: 67.2] [Reference Citation Analysis (0)] |
| 80. | Seo YS, Park SY, Kim MY, Kim JH, Park JY, Yim HJ, Jang BK, Kim HS, Hahn T, Kim BI, Heo J, An H, Tak WY, Baik SK, Han KH, Hwang JS, Park SH, Cho M, Um SH. Lack of difference among terlipressin, somatostatin, and octreotide in the control of acute gastroesophageal variceal hemorrhage. Hepatology. 2014;60:954-963. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 143] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 81. | Wells M, Chande N, Adams P, Beaton M, Levstik M, Boyce E, Mrkobrada M. Meta-analysis: vasoactive medications for the management of acute variceal bleeds. Aliment Pharmacol Ther. 2012;35:1267-1278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 147] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 82. | Goulis J, Armonis A, Patch D, Sabin C, Greenslade L, Burroughs AK. Bacterial infection is independently associated with failure to control bleeding in cirrhotic patients with gastrointestinal hemorrhage. Hepatology. 1998;27:1207-1212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 312] [Cited by in RCA: 256] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 83. | Bañares R, Albillos A, Rincón D, Alonso S, González M, Ruiz-del-Arbol L, Salcedo M, Molinero LM. Endoscopic treatment versus endoscopic plus pharmacologic treatment for acute variceal bleeding: a meta-analysis. Hepatology. 2002;35:609-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 315] [Cited by in RCA: 277] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 84. | Hsu YC, Chung CS, Tseng CH, Lin TL, Liou JM, Wu MS, Hu FC, Wang HP. Delayed endoscopy as a risk factor for in-hospital mortality in cirrhotic patients with acute variceal hemorrhage. J Gastroenterol Hepatol. 2009;24:1294-1299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 49] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 85. | Chen PH, Chen WC, Hou MC, Liu TT, Chang CJ, Liao WC, Su CW, Wang HM, Lin HC, Lee FY, Lee SD. Delayed endoscopy increases re-bleeding and mortality in patients with hematemesis and active esophageal variceal bleeding: a cohort study. J Hepatol. 2012;57:1207-1213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 82] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 86. | Laine L, Deborah Cook MD. Endoscopic ligation compared with sclerotherapyfor treatment of esophageal variceal bleeding: A meta-analysis. Ann Intern Med. 1995;123:280-287. |
| 87. | Hernández-Gea V, Procopet B, Giráldez Á, Amitrano L, Villanueva C, Thabut D, Ibañez-Samaniego L, Silva-Junior G, Martinez J, Genescà J, Bureau C, Trebicka J, Llop E, Laleman W, Palazon JM, Castellote J, Rodrigues S, Gluud LL, Noronha Ferreira C, Barcelo R, Cañete N, Rodríguez M, Ferlitsch A, Mundi JL, Gronbaek H, Hernández-Guerra M, Sassatelli R, Dell'Era A, Senzolo M, Abraldes JG, Romero-Gómez M, Zipprich A, Casas M, Masnou H, Primignani M, Krag A, Nevens F, Calleja JL, Jansen C, Robic MA, Conejo I, Catalina MV, Albillos A, Rudler M, Alvarado E, Guardascione MA, Tantau M, Bosch J, Torres F, Garcia-Pagán JC; International Variceal Bleeding Observational Study Group and Baveno Cooperation. Preemptive-TIPS Improves Outcome in High-Risk Variceal Bleeding: An Observational Study. Hepatology. 2019;69:282-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 96] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 88. | Vangeli M, Patch D, Burroughs AK. Salvage tips for uncontrolled variceal bleeding. J Hepatol. 2002;37:703-704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 66] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 89. | Garcia-Pagán JC, Di Pascoli M, Caca K, Laleman W, Bureau C, Appenrodt B, Luca A, Zipprich A, Abraldes JG, Nevens F, Vinel JP, Sauerbruch T, Bosch J. Use of early-TIPS for high-risk variceal bleeding: results of a post-RCT surveillance study. J Hepatol. 2013;58:45-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 198] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 90. | Thabut D, Pauwels A, Carbonell N, Remy AJ, Nahon P, Causse X, Cervoni JP, Cadranel JF, Archambeaud I, Bramli S, Ehrhard F, Ah-Soune P, Rostain F, Pariente A, Vergniol J, Dupuychaffray JP, Pelletier AL, Skinazi F, Guillygomarc'h A, Vitte RL, Henrion J, Combet S, Rudler M, Bureau C; des Hépato-Gastroentérologues des Hôpitaux Généraux (ANGH); Club Francophone pour l'Etude de l'Hypertension Portale (CFETHTP); CHOC Study Group collaborators:. Cirrhotic patients with portal hypertension-related bleeding and an indication for early-TIPS: a large multicentre audit with real-life results. J Hepatol. 2017;68:73-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 89] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 91. | Terés J, Cecilia A, Bordas JM, Rimola A, Bru C, Rodés J. Esophageal tamponade for bleeding varices. Controlled trial between the Sengstaken-Blakemore tube and the Linton-Nachlas tube. Gastroenterology. 1978;75:566-569. [PubMed] |
| 92. | Fort E, Sautereau D, Silvain C, Ingrand P, Pillegand B, Beauchant M. A randomized trial of terlipressin plus nitroglycerin vs. balloon tamponade in the control of acute variceal hemorrhage. Hepatology. 1990;11:678-681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 48] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 93. | Pinto-Marques P, Romãozinho JM, Ferreira M, Amaro P, Freitas D. Esophageal perforation--associated risk with balloon tamponade after endoscopic therapy. Myth or reality? Hepatogastroenterology. 2006;53:536-539. [PubMed] |
| 94. | D'Amico G, Pagliaro L, Bosch J. The treatment of portal hypertension: a meta-analytic review. Hepatology. 1995;22:332-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 454] [Cited by in RCA: 467] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 95. | Avgerinos A, Armonis A. Balloon tamponade technique and efficacy in variceal haemorrhage. Scand J Gastroenterol Suppl. 1994;207:11-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 59] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 96. | Jaramillo JL, de la Mata M, Miño G, Costán G, Gómez-Camacho F. Somatostatin versus Sengstaken balloon tamponade for primary haemostasia of bleeding esophageal varices. A randomized pilot study. J Hepatol. 1991;12:100-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 46] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 97. | García-Compeán D, Blanc P, Bories JM, Michel J, Desprez D, Pageaux GP, David XR, Larrey D, Michel H. Treatment of active gastroesophageal variceal bleeding with terlipressin or hemostatic balloon in patients with cirrhosis. A randomized controlled trial. Arch Med Res. 1997;28:241-245. [PubMed] |
| 98. | de Franchis R. Evolving consensus in portal hypertension. Report of the Baveno IV consensus workshop on methodology of diagnosis and therapy in portal hypertension. J Hepatol. 2005;43:167-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 794] [Cited by in RCA: 733] [Article Influence: 36.7] [Reference Citation Analysis (0)] |
| 99. | Zehetner J, Shamiyeh A, Wayand W, Hubmann R. Results of a new method to stop acute bleeding from esophageal varices: implantation of a self-expanding stent. Surg Endosc. 2008;22:2149-2152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 60] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 100. | Hubmann R, Bodlaj G, Czompo M, Benkö L, Pichler P, Al-Kathib S, Kiblböck P, Shamyieh A, Biesenbach G. The use of self-expanding metal stents to treat acute esophageal variceal bleeding. Endoscopy. 2006;38:896-901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 96] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 101. | Pfisterer N, Riedl F, Pachofszky T, Gschwantler M, König K, Schuster B, Mandorfer M, Gessl I, Illiasch C, Fuchs EM, Unger L, Dolak W, Maieron A, Kramer L, Madl C, Trauner M, Reiberger T. Outcomes after placement of a SX-ELLA oesophageal stent for refractory variceal bleeding-A national multicentre study. Liver Int. 2019;39:290-298. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 102. | Escorsell À, Pavel O, Cárdenas A, Morillas R, Llop E, Villanueva C, Garcia-Pagán JC, Bosch J; Variceal Bleeding Study Group. Esophageal balloon tamponade versus esophageal stent in controlling acute refractory variceal bleeding: A multicenter randomized, controlled trial. Hepatology. 2016;63:1957-1967. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 128] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 103. | Escorsell A, Bosch J. Self-expandable metal stents in the treatment of acute esophageal variceal bleeding. Gastroenterol Res Pract. 2011;2011:910986. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 104. | Pfisterer N, Schmidbauer C, Riedl F, Maieron A, Stadlbauer V, Hennlich B, Schwarzer R, Puespoek A, Bucsics T, Effenberger M, Bota S, Gschwantler M, Peck-Radosavljevic M, Mandorfer M, Madl C, Trauner M, Reiberger T. Perceptions on the management of varices and on the use of albumin in patients with cirrhosis among GI specialists in Austria. Wien Klin Wochenschr. 2021;133:421-431. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 105. | Saad WEA, Darcy MD. Transjugular Intrahepatic portosystemic shunt (TIPS) vs balloon-occluded retrograde transvenous obliteration (BRTO) for the management of gastric varices. Semin Intervent Radiol. 2011;28:339-349. [RCA] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 91] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 106. | Paleti S, Nutalapati V, Fathallah J, Jeepalyam S, Rustagi T. Balloon-Occluded Retrograde Transvenous Obliteration (BRTO) Versus Transjugular Intrahepatic Portosystemic Shunt (TIPS) for Treatment of Gastric Varices Because of Portal Hypertension: A Systematic Review and Meta-Analysis. J Clin Gastroenterol. 2020;54:655-660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 107. | Lee SJ, Kim SU, Kim MD, Kim YH, Kim GM, Park SI, Won JY, Lee DY, Lee KH. Comparison of treatment outcomes between balloon-occluded retrograde transvenous obliteration and transjugular intrahepatic portosystemic shunt for gastric variceal bleeding hemostasis. J Gastroenterol Hepatol. 2017;32:1487-1494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 108. | Garcia-Tsao G, Bosch J. Varices and Variceal Hemorrhage in Cirrhosis: A New View of an Old Problem. Clin Gastroenterol Hepatol. 2015;13:2109-2117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 60] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 109. | Moitinho E, Escorsell A, Bandi JC, Salmerón JM, García-Pagán JC, Rodés J, Bosch J. Prognostic value of early measurements of portal pressure in acute variceal bleeding. Gastroenterology. 1999;117:626-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 342] [Cited by in RCA: 305] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 110. | Kraja B, Mone I, Akshija I, Koçollari A, Prifti S, Burazeri G. Predictors of esophageal varices and first variceal bleeding in liver cirrhosis patients. World J Gastroenterol. 2017;23:4806-4814. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 53] [Cited by in RCA: 56] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 111. | Hong WD, Zhu QH, Huang ZM, Chen XR, Jiang ZC, Xu SH, Jin K. Predictors of esophageal varices in patients with HBV-related cirrhosis: a retrospective study. BMC Gastroenterol. 2009;9:11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 59] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 112. | Sen S, Griffiths WJ. Non-invasive prediction of oesophageal varices in cirrhosis. World J Gastroenterol. 2008;14:2454-2455. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 17] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 113. | Tafarel JR, Tolentino LH, Correa LM, Bonilha DR, Piauilino P, Martins FP, Rodrigues RA, Nakao FS, Libera ED, Ferrari AP, da Silveira Röhr MR. Prediction of esophageal varices in hepatic cirrhosis by noninvasive markers. Eur J Gastroenterol Hepatol. 2011;23:754-758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 114. | Caldwell SH, Hoffman M, Lisman T, Macik BG, Northup PG, Reddy KR, Tripodi A, Sanyal AJ; Coagulation in Liver Disease Group. Coagulation disorders and hemostasis in liver disease: pathophysiology and critical assessment of current management. Hepatology. 2006;44:1039-1046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 359] [Cited by in RCA: 341] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 115. | Drolz A, Horvatits T, Roedl K, Rutter K, Staufer K, Kneidinger N, Holzinger U, Zauner C, Schellongowski P, Heinz G, Perkmann T, Kluge S, Trauner M, Fuhrmann V. Coagulation parameters and major bleeding in critically ill patients with cirrhosis. Hepatology. 2016;64:556-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 145] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 116. | Tantai XX, Liu N, Yang LB, Wei ZC, Xiao CL, Song YH, Wang JH. Prognostic value of risk scoring systems for cirrhotic patients with variceal bleeding. World J Gastroenterol. 2019;25:6668-6680. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 29] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (1)] |
| 117. | Shafaghi A, Gharibpoor F, Mahdipour Z, Samadani AA. Comparison of three risk scores to predict outcomes in upper gastrointestinal bleeding; modifying Glasgow-Blatchford with albumin. Rom J Intern Med. 2019;57:322-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 118. | Monteiro S, Gonçalves TC, Magalhães J, Cotter J. Upper gastrointestinal bleeding risk scores: Who, when and why? World J Gastrointest Pathophysiol. 2016;7:86-96. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 40] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 119. | Lo GH, Lai KH, Cheng JS, Chen MH, Huang HC, Hsu PI, Lin CK. Endoscopic variceal ligation plus nadolol and sucralfate compared with ligation alone for the prevention of variceal rebleeding: a prospective, randomized trial. Hepatology. 2000;32:461-465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 164] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 120. | Thiele M, Krag A, Rohde U, Gluud LL. Meta-analysis: banding ligation and medical interventions for the prevention of rebleeding from oesophageal varices. Aliment Pharmacol Ther. 2012;35:1155-1165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 64] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 121. | Holster IL, Tjwa ET, Moelker A, Wils A, Hansen BE, Vermeijden JR, Scholten P, van Hoek B, Nicolai JJ, Kuipers EJ, Pattynama PM, van Buuren HR. Covered transjugular intrahepatic portosystemic shunt versus endoscopic therapy + β-blocker for prevention of variceal rebleeding. Hepatology. 2016;63:581-589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 164] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 122. | Sauerbruch T, Mengel M, Dollinger M, Zipprich A, Rössle M, Panther E, Wiest R, Caca K, Hoffmeister A, Lutz H, Schoo R, Lorenzen H, Trebicka J, Appenrodt B, Schepke M, Fimmers R; German Study Group for Prophylaxis of Variceal Rebleeding. Prevention of Rebleeding From Esophageal Varices in Patients With Cirrhosis Receiving Small-Diameter Stents Versus Hemodynamically Controlled Medical Therapy. Gastroenterology. 2015;149:660-668.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 181] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 123. | Unger LW, Stork T, Bucsics T, Rasoul-Rockenschaub S, Staufer K, Trauner M, Maschke S, Pawloff M, Soliman T, Reiberger T, Berlakovich GA. The role of TIPS in the management of liver transplant candidates. United European Gastroenterol J. 2017;5:1100-1107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 124. | Jachs M, Hartl L, Schaufler D, Desbalmes C, Simbrunner B, Eigenbauer E, Bauer DJM, Paternostro R, Schwabl P, Scheiner B, Bucsics T, Stättermayer AF, Pinter M, Trauner M, Mandorfer M, Reiberger T. Amelioration of systemic inflammation in advanced chronic liver disease upon beta-blocker therapy translates into improved clinical outcomes. Gut. 2020;gutjnl-2020. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 61] [Article Influence: 15.3] [Reference Citation Analysis (1)] |
| 125. | Kim HY, So YH, Kim W, Ahn DW, Jung YJ, Woo H, Kim D, Kim MY, Baik SK. Non-invasive response prediction in prophylactic carvedilol therapy for cirrhotic patients with esophageal varices. J Hepatol. 2019;70:412-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 60] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 126. | Marasco G, Dajti E, Ravaioli F, Alemanni LV, Capuano F, Gjini K, Colecchia L, Puppini G, Cusumano C, Renzulli M, Golfieri R, Festi D, Colecchia A. Spleen stiffness measurement for assessing the response to β-blockers therapy for high-risk esophageal varices patients. Hepatol Int. 2020;14:850-857. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 42] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 127. | García-Pagán JC, Saffo S, Mandorfer M, Garcia-Tsao G. Where does TIPS fit in the management of patients with cirrhosis? JHEP Rep. 2020;2:100122. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 81] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 128. | Bucsics T, Schoder M, Mandorfer M, Schwabl P, Riedl F, Bauer D, Trauner M, Peck-Radosavljevic M, Karner J, Karnel F, Reiberger T. Effectiveness of “early” TIPS implantation vs “late” TIPS vs standard endoscopic treatment for acute variceal bleeding in patients with liver cirrhosis. J Hepatol. 2018;68:S694-S695. [DOI] [Full Text] |