Published online Apr 27, 2021. doi: 10.4254/wjh.v13.i4.472
Peer-review started: January 26, 2021
First decision: February 13, 2021
Revised: March 8, 2021
Accepted: April 7, 2021
Article in press: April 7, 2021
Published online: April 27, 2021
Processing time: 79 Days and 13.5 Hours
There is minimal objective data regarding adverse events related to endoscopic retrograde cholangio-pancreatography (ERCP) in patients with cirrhosis compared to those without cirrhosis and even fewer data comparing com
To determine if patients with cirrhosis are at increased risk of adverse events related to ERCP: mainly pancreatitis, bleeding, perforation, cholangitis, and mortality; And to see if higher Child-Pugh (CP) score and Model for End-Stage Liver Disease (MELD) score are associated with higher post-ERCP complications.
We performed a retrospective analysis of 692 patients who underwent ERCP and analyzed the impact of cirrhosis etiology, gender, type of sedation used during procedure, interventions performed, and co-morbidities on the rate of complications in cirrhosis patients as compared to non-cirrhosis patients.
Overall complications were higher in those with cirrhosis as compared to those without cirrhosis (P = 0.015 at significance level of 0.05). CP class, especially CP class C, was shown to be associated with a significantly higher rate of ERCP complications as compared to CP class A and CP class B (P = 0.010 at significance level of 0.05).
The results of our study reaffirm that liver cirrhosis has an impact on the occurrence of complications during ERCP. Our study shows that CP class seems to be more reliable as compared to MELD score in predicting complications of ERCP in cirrhosis patients.
Core Tip: What is previously known is that endoscopic retrograde cholangio-pancreatography is associated with a risk of adverse events. What is new in this manuscript is that complications are increased in patients with cirrhosis as compared to patients without cirrhosis. Statistical significance was demonstrated in patients classified as Child-Pugh (CP) Class C as compared to CP Classes A and B.
- Citation: Bernshteyn M, Hu L, Masood U, Sharma AV, Huang D, Sapkota B. Retrospective analysis of complications related to endoscopic retrograde cholangio-pancreatography in patients with cirrhosis vs patients without cirrhosis. World J Hepatol 2021; 13(4): 472-482
- URL: https://www.wjgnet.com/1948-5182/full/v13/i4/472.htm
- DOI: https://dx.doi.org/10.4254/wjh.v13.i4.472
Endoscopic retrograde cholangio-pancreatography (ERCP) is a procedure utilized for the management of pancreatobiliary disorders, including but not limited to choledocolithiasis, biliary strictures, pancreatitis, and cholangitis[1]. However, like all procedures, there is an associated risk of adverse events, such as post-ERCP pancreatitis, bleeding, infection, perforation, and even death[2].
Patients with chronic liver disease and cirrhosis often require ERCP. However, because of hepatic synthetic dysfunction and portal hypertension, patients with cirrhosis have a much higher risk of developing adverse events and complications after invasive procedures[3]. Despite this, there remains a scarce amount of data investigating complications associated with ERCP in patients with cirrhosis as compared to patients without cirrhosis. There is even less information regarding adverse effects among patient with cirrhosis based upon cirrhosis severity.
Thus, our study aims to add to the limited body of knowledge regarding complications of ERCP in patients with cirrhosis. We hypothesized that patients with an underlying diagnosis of cirrhosis are at elevated risk of complications associated to ERCP, including mortality, pancreatitis, bleeding, perforation, and cholangitis. A secondary objective was to examine our hypothesis that a higher Child-Pugh (CP) score and/or Model for End-Stage Liver Disease (MELD) score is related to a greater number of post-ERCP complications in cirrhosis.
This study was a retrospective review of all patients who underwent ERCP at a University hospital in Syracuse, NY, United States from 2012-2019. The project was presented to the Institutional Review Board and approved prior to its initiation. Chart review of 692 patients who underwent ERCP between January 1, 2012 and December 31, 2019 was conducted. Of the 692 patients, 174 patients had a diagnosis of cirrhosis at the time of ERCP, and 518 patients did not. Demographics, co-morbidities [including chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), hypertension (HTN), diabetes mellitus (DM), chronic kidney disease (CKD), and hyperlipidemia (HLD)], indication for procedure, type of sedation used, type of intervention(s) performed, and complications within a 30-d period were analyzed for all subjects. Of the 174 patients with cirrhosis, we also recorded cirrhosis etiology and calculated their MELD score and CP class.
Statistical analysis of the complication rates in the groups with and without cirrhosis was performed using a chi-squared test, and fishers exact test when there were < 5 individuals in a category. Pearson’s chi square test is sufficient when testing the impact of a single factor on binary outcome. Of those with cirrhosis, the complication rates in subjects grouped by Child score A, B, and C, as well as MELD score, were also compared using a chi-squared or fishers exact test. A P value of < 0.05 was considered statistically significant. Odds ratios with 95% confidence intervals were derived from logistic regression as a supportive method in confirming the findings of Child score significance.
A total number of 692 patients were included in our study. Of the 692, 174 had an underlying diagnosis of cirrhosis while 518 did not. Mean patient age was 58.6 years. Overall, there was a higher rate of complications in those with cirrhosis as compared to those without cirrhosis (P = 0.015) (Table 1). There was no statistical significance comparing the specific types of complications across the two groups (P = 0.897), including bleeding, pancreatitis, cholangitis, perforation, mortality, or other.
| With cirrhosis (n = 174) | Without cirrhosis (n = 518) | P value | |
| Any complication? | 0.015a | ||
| No | 133 (78.70) | 448 (86.49) | |
| Yes | 36 (21.30) | 70 (13.51) | |
| Complications | 0.8971 | ||
| Bleeding | 2 (5.56) | 7 (10.00) | |
| Pancreatitis | 11 (30.56) | 25 (35.71) | |
| Cholangitis | 2 (5.56) | 5 (7.14) | |
| Perforation | 1 (2.78) | 2 (2.86) | |
| Mortality attributed to ERCP | 0 (0.00) | 1 (1.43) | |
| Other mortality | 5 (13.89) | 12 (17.14) | |
| Other | 15 (41.67) | 18 (25.71) |
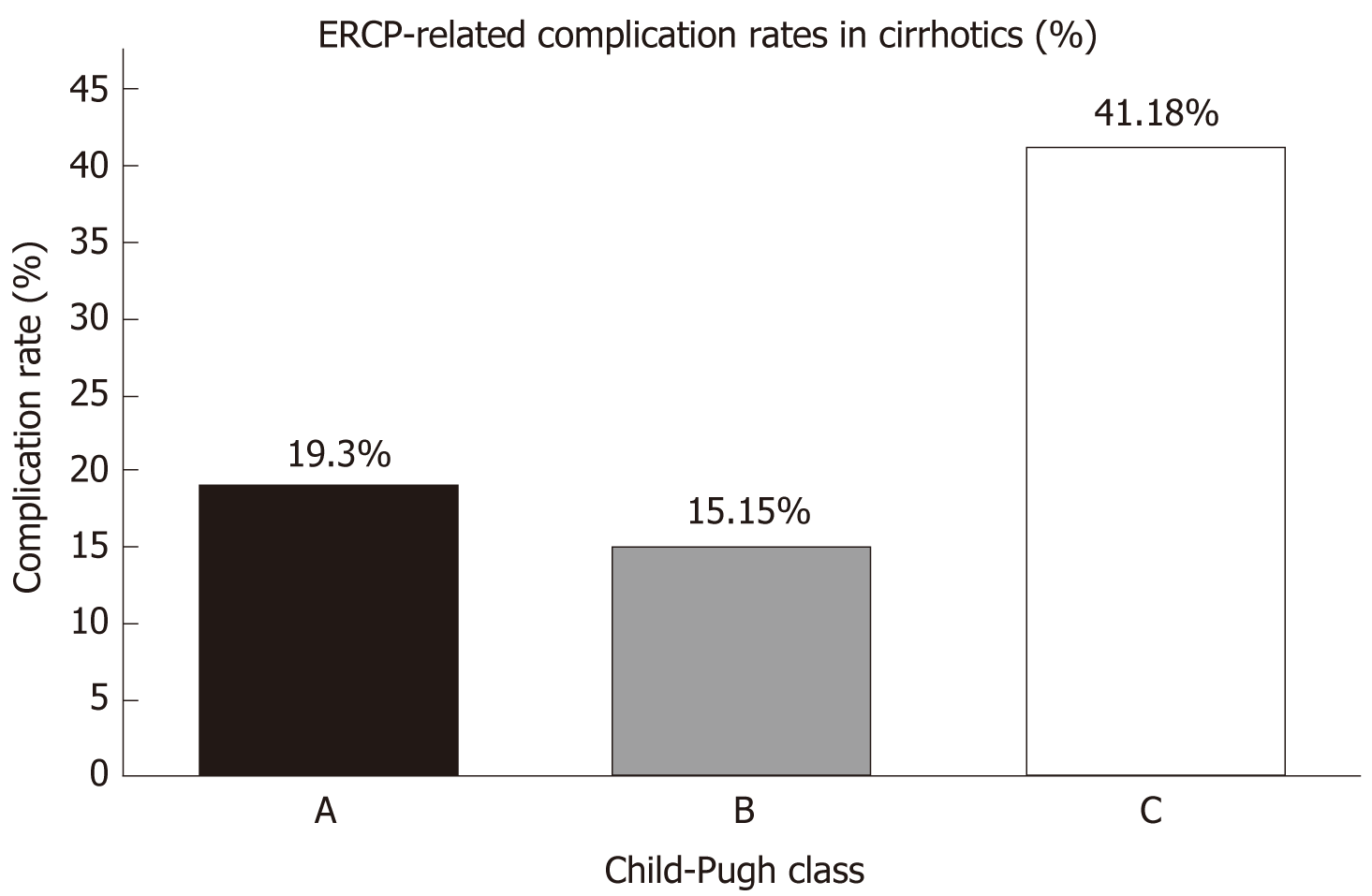
Complications in subjects with cirrhosis grouped by CP class are shown in Table 2. CP class, especially CP class C, was shown to be associated with a significantly higher rate of ERCP complications as compared to CP class A and CP class B (P = 0.010). In other words, a statistically significant proportion of cirrhosis patients with CP class A or class B are less likely to develop complications than those in CP class C (Figure 1). The odds ratios 0.342 with (0.132, 0.882) as 95% confidence interval for group A vs group C and 0.251 with (0.096, 0.6253) as 95% confidence interval for group B vs group C, as derived from logistic regression support the above conclusion (Table 3).
| A | B | C | P value | |
| Any complication? | 0.010a | |||
| No | 46 (80.70) | 56 (84.85) | 20 (58.82) | |
| Yes | 11 (19.30) | 10 (15.15) | 14 (41.18) |
| Odds ratio | Estimate | 95%CI | Limits |
| Child A vs B | 1.363 | 0.532 | 3.491 |
| Child A vs C | 0.342 | 0.132 | 0.882 |
| Child B vs C | 0.251 | 0.096 | 0.653 |
Complications in subjects with cirrhosis grouped by MELD score are shown in Table 4. There was no statistical significance when comparing complications in patients with cirrhosis with a MELD score of < 15 vs > 15 (P = 0.949). Thus, CP class was more reliable than MELD score in terms of predicating complications in cirrhosis.
| < 10 | 10-15 | > 15 | P value | |
| Any complication? | 0.626 | |||
| No | 56 (74.67) | 41 (82.00) | 25 (78.13) | |
| Yes | 19 (25.33) | 9 (18.00) | 7 (21.88) | |
| < 10 | ≥ 10 | |||
| Any complication? | 0.381 | |||
| No | 56 (74.67) | 66 (80.49) | ||
| Yes | 19 (25.33) | 16 (19.51) | ||
| ≤ 15 | > 15 | |||
| Any complication? | 0.949 | |||
| No | 97 (77.60) | 25 (78.13) | ||
| Yes | 28 (22.40) | 7 (21.88) | ||
We also analyzed the complication occurrence in cirrhosis patients based on underlying etiology. This included: Alcohol, hepatitis C, and non-alcoholic fatty liver disease. Etiology of cirrhosis did not have a significant difference in respect to complications related to ERCP (Table 5).
| Any complication? | No | Yes | P value |
| Alcohol etiology | 0.192 | ||
| No | 65 (74.1) | 22 (25.29) | |
| Yes | 68 (82.93) | 14 (17.07) | |
| HEPC etiology | |||
| No | 112 (78.87) | 30 (21.13) | 0.899 |
| Yes | 21 (77.78) | 6 (22.22) | |
| NAFLD etiology | |||
| No | 123 (77.85) | 35 (22.15) | 0.4611 |
| Yes | 10 (90.91) | 1 (9.09) | |
| Gender | |||
| Female | 51 (76.12) | 16 (23.88) | 0.507 |
| Male | 82 (80.39) | 20 (19.61) | |
| Type of Anesthesia | |||
| General Anesthesia | 105 (78.36) | 29 (21.64) | 0.271 |
| MAC | 4 (57.14) | 3 (42.86) | |
| Moderate conscious sedation | 23 (85.19) | 4 (14.81) |
Gender did not have a statistically significant effect on complications between cirrhosis and non-cirrhosis patients (Table 5 and 6).
| Any complication? | No | Yes | P value |
| Gender | 0.692 | ||
| Female | 264 (85.99) | 43 (14.01) | |
| Male | 184 (87.20) | 27 (12.80) | |
| Type of Anesthesia | |||
| General Anesthesia | 308 (85.56) | 52 (14.44) | 0.511 |
| MAC | 131 (89.12) | 16 (10.88) | |
| Moderate conscious sedation | 9 (81.82) | 2 (18.18) |
Type of anesthesia used during the ERCP did not have any statistically significant difference regarding complications between both cirrhosis and non-cirrhosis patients (Table 5 and 6).
We collected data on whether the ERCP was for diagnostic or therapeutic purposes, as well as the types of intervention performed during the ERCP (Table 7 and 8). In non-cirrhosis patients, a “Diagnostic ERCP” showed a higher risk for complications (P = 0.039). Otherwise, type of intervention done did not have any statistically significant effect on complication occurrence between cirrhosis and non-cirrhosis patients.
| Any complication? | No | Yes | P value |
| Diagnostic ERCP | 0.7371 | ||
| No | 122 (78.21) | 34 (21.79) | |
| Yes | 11 (84.62) | 2 (15.38) | 0.192 |
| Sphincterotomy/sphincteroplasty | |||
| No | 86 (81.90) | 19 (18.10) | |
| Yes | 47 (73.44) | 17 (26.56) | |
| Biliary intervention (stent, sweeping, dilatation, brushing) | 1.0001 | ||
| No | 17 (80.95) | 4 (19.05) | |
| Yes | 116 (78.38) | 32 (21.62) | |
| Spyglass | 0.0981 | ||
| No | 128 (80.00) | 32 (20.00) | |
| Yes | 5 (55.56) | 4 (44.44) | |
| Pancreatic intervention | 1.0001 | ||
| No | 17 (80.95) | 4 (19.05) | |
| Yes | 116 (78.38) | 32 (21.62) | |
| Manometry | |||
| No | 133 (78.7) | 36 (21.3) | |
| Yes | 0 (0) | 0 (0) |
| Any complication? | No | Yes | P value |
| Diagnostic ERCP | 0.0391 | ||
| No | 422 (87.37) | 61 (12.63) | |
| Yes | 26 (74.29) | 9 (25.71) | |
| Sphincterotomy/sphincteroplasty | 0.252 | ||
| No | 262 (85.06) | 46 (14.94) | |
| Yes | 186 (88.57) | 24 (11.43) | |
| Biliary intervention (stent, sweeping, dilatation, brushing) | 0.133 | ||
| No | 70 (81.40) | 16 (18.60) | |
| Yes | 377 (87.47) | 54 (12.53) | |
| Spyglass | 0.1181 | ||
| No | 430 (87.04) | 64 (12.96) | |
| Yes | 18 (75.00) | 6 (25.00) | |
| Pancreatic intervention | 0.133 | ||
| No | 70 (81.40) | 16 (18.60) | |
| Yes | 377 (87.47) | 54 (12.53) | |
| Manometry | 0.2521 | ||
| No | 447 (86.63) | 69 (13.37) | |
| Yes | 1 (50.00) | 1 (50.00) |
It was noted whether the patient had any of these comorbidities at the time of ERCP: COPD, CHF, HTN, DM, CKD, and HLD. In cirrhosis patients, COPD and HTN demonstrated significantly higher rates of complications (P = 0.009 and 0.003 correspondingly) (Table 9). In patients without cirrhosis, statistically significant complication rates were only demonstrated in those with an underlying diagnosis of COPD (P = 0.003) (Table 10).
| Any complication? | No | Yes | P value |
| Chronic obstructive pulmonary disease | 0.009a | ||
| No | 114 (82.61) | 24 (17.39) | |
| Yes | 19 (61.29) | 12 (38.71) | |
| Congestive heart failure | 0.5721 | ||
| No | 116 (77.85) | 33 (22.15) | |
| Yes | 17 (85.00) | 3 (15.00) | |
| Essential hypertension | 0.003a | ||
| No | 42 (66.67) | 21 (33.33) | |
| Yes | 91 (85.85) | 15 (14.15) | |
| Diabetes mellitus | 0.515 | ||
| No | 89 (80.18) | 22 (19.82) | |
| Yes | 44 (75.86) | 14 (24.14) | |
| Chronic kidney disease | 0.4781 | ||
| No | 124 (79.49) | 32 (20.51) | |
| Yes | 9 (69.23) | 4 (30.77) | |
| Hyperlipidemia | |||
| No | 95 (76.00) | 30 (24.00) | 0.149 |
| Yes | 38 (86.36) | 6 (13.64) |
| Any complication? | No | Yes | P value |
| Chronic obstructive pulmonary disease | 0.003a | ||
| No | 421 (87.71) | 59 (12.29) | |
| Yes | 26 (70.27) | 11 (29.73) | |
| Congestive heart failure | 0.7821 | ||
| No | 424 (86.53) | 24 (85.71) | |
| Yes | 24 (85.71) | 4 (14.29) | |
| Essential hypertension | 0.071 | ||
| No | 237 (89.10) | 29 (10.90) | |
| Yes | 210 (83.67) | 41 (16.33) | |
| Diabetes mellitus | 0.652 | ||
| No | 350 (86.85) | 53 (13.15) | |
| Yes | 98 (85.22) | 17 (14.78) | |
| Chronic kidney disease | 0.827 | ||
| No | 413 (86.58) | 64 (13.42) | |
| Yes | 35 (85.37) | 6 (14.63) | |
| Hyperlipidemia | 0.531 | ||
| No | 350 (86.00) | 57 (14.00) | |
| Yes | 98 (88.29) | 13 (11.71) |
In this retrospective cohort study of 692 patients, 174 with cirrhosis and 518 without cirrhosis, we found that the overall occurrence of complications was increased in those with cirrhosis to a statistically significant level. In subgroup analysis of CP class and MELD score, we found that CP class C was associated with higher risk of complications, and that CP class was a more reliable predictor of complications than MELD score. The years of experience amongst the advanced endoscopists ranged from approximately five to thirty years, with each performing approximately one-hundred procedures per year.
There remains a scarcity in the literature regarding complications and adverse events after ERCP in cirrhosis patients, particularly those incorporating CP class and MELD score or type of intervention as predictors. A retrospective matched case-control study by Navaneethan et al[4] showed a higher risk of ERCP-associated hemorrhage in cirrhosis patients vs non-cirrhosis patients[4]. Similarly, Inamdar et al[5] found a higher rate of post-ERCP pancreatitis and bleeding in cirrhosis patients compared to non-cirrhosis patients. Furthermore, in subgroup analysis, compensated cirrhosis patients and non-cirrhosis patients had a similar complication profile as compared to decompensated cirrhosis patients except for a 2.2% higher rate of pancreatitis[5]. More recently, Leal et al[6] reaffirmed a higher rate of adverse events after ERCP in cirrhosis vs non-cirrhosis patients[6]. In our study, no statistical significance was calculated when comparing the specific types of adverse events across the two groups, including bleeding, pancreatitis, cholangitis, perforation, mortality, or other. There have been other studies, such as ours, that demonstrated similar outcomes between groups[7]. Importantly, there remains a lack of conclusive evidence warranting further studies.
Data regarding the relationship of ERCP complications and CP class or MELD score are even more limited and contradictory. For instance, Adler et al[8] demonstrated that CP class A was associated with a lower risk of ERCP adverse events compared to class B and C combined[8]. Jagtap et al[9] found that overall post-ERCP adverse events were increased in patients with CP class C and MELD score > 18[9]. Li et al[10] demonstrated that CP class C was associated with a statistically significant higher risk of post-ERCP bleeding, however showed no difference in bleeding between cirrhosis and non-cirrhosis patients[10]. Similarly, multiple studies have found higher rates of post-ERCP bleeding in CP class C compared to class A and B[11,12]. Our analysis correlates with these findings. However, Zhang et al[13] found no association of rates of adverse events with respect to CP class, and instead demonstrated MELD score as a more reliable predictor of higher rates of complications[13]. Interestingly, our study demonstrated a statistically significant proportion of cirrhosis patients with CP class A or class B were less likely to develop complications than those in CP class C. Our study demonstrated that MELD score was not reliable in predicting complications. Whereas our findings correlate with some of the already published studies, it takes research a step further by investigating the impact of cirrhosis etiology, gender, type of sedation used during procedure, interventions performed, and co-morbidities on the rate of complications of ERCP in cirrhosis patients as compared to non-cirrhosis patients.
Our study had several limitations. This includes its retrospective design and moderate sample size. Several patients did not have all the necessary lab values and information on the day of the documented ERCP. In these cases, we had to use the necessary data points obtained at the date closest to their ERCP to calculate MELD scores and CP class. Similarly, many of the data points we collected relied on accurate and complete physician documentation, which can have significant variance. In our data collection, we could not include all comorbidities of each patient, and therefore chose to include six common ones that can affect risk of procedural complications. We encourage that further studies include a broader scope of comorbidities, such as immunocompromising diseases, etc. Furthermore, we did not analyze specific pancreatic duct stenting, use of indomethacin, or coagulopathy in respect to outcome. Lastly, we only considered complications that occurred within the span of 30 d of ERCP. The clinical course of a cirrhosis patient who has undergone an invasive procedure may be more complex and indirect complications may occur further down the line.
In conclusion, the results of our study reaffirm that liver cirrhosis has an impact on the occurrence of complications during ERCP. Our study shows that CP class seems to be more reliable as compared to MELD score in predicting complications of ERCP in cirrhosis patients. However, we are also aware that CP and MELD scores are complementary to each other while evaluating outcomes of any surgery in patients with cirrhosis. These findings should encourage clinicians to be aware of the increased risk when referring for, or performing, an ERCP on a patient with cirrhosis. It is imperative to perform a thorough risk-benefit assessment taking into consideration the extent of liver disease and comorbidities prior to ERCP, as doing so may improve clinical outcomes. Further studies, particularly prospective studies, are required to confirm this risk and further delineate the relationship between cirrhosis and complication risk during ERCP.
Endoscopic retrograde cholangio-pancreatography (ERCP) is associated with a risk of adverse events. There remains a scarce amount of data investigating complications associated with ERCP in patients with cirrhosis as compared to patients without cirrhosis.
Our aim was to determine if patients with cirrhosis are at increased risk of complications associated with ERCP and if a higher Child-Pugh (CP) score and Model for End-Stage Liver Disease (MELD) score are linked to higher post-ERCP adverse events. Findings should encourage clinicians to be aware of the increased risk when referring for, or performing, an ERCP on a patient with cirrhosis.
Our primary aim was to determine if patients with an underlying diagnosis of cirrhosis are at elevated risk of complications compared to patients without cirrhosis, specifically pancreatitis, bleeding, perforation, cholangitis, and mortality. Our study takes previous research a step further by investigating the impact of cirrhosis etiology, gender, type of sedation used during procedure, interventions performed, and co-morbidities on the rate of complications of ERCP.
This was a retrospective analysis in which a statistical analysis of the complication rates in the groups with and without cirrhosis was performed using a chi-squared test, and fishers exact test when there were < 5 individuals in a category. Odds ratios with 95% confidence intervals were derived from logistic regression as a supportive method in confirming the findings of Child score significance.
The results of our study reaffirm that liver cirrhosis has an impact on the occurrence of complications during ERCP. Our study demonstrated a statistically significant proportion of cirrhosis patients with CP class A or class B were less likely to develop complications than those in CP class C. Our study demonstrated that MELD score was not reliable in predicting complications.
Complications are increased in patients with cirrhosis, especially those in CP Class C.
Further studies, particularly prospective studies, are required to confirm the risk of performing an ERCP on a patient with cirrhosis, and further delineate the relationship between cirrhosis and complication risk during ERCP.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kovacevic B S-Editor: Fan JR L-Editor: A P-Editor: Zhang YL
| 1. | Adler DG, Baron TH, Davila RE, Egan J, Hirota WK, Leighton JA, Qureshi W, Rajan E, Zuckerman MJ, Fanelli R, Wheeler-Harbaugh J, Faigel DO; Standards of Practice Committee of American Society for Gastrointestinal Endoscopy. ASGE guideline: the role of ERCP in diseases of the biliary tract and the pancreas. Gastrointest Endosc. 2005;62:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 292] [Cited by in RCA: 286] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 2. | Christensen M, Matzen P, Schulze S, Rosenberg J. Complications of ERCP: a prospective study. Gastrointest Endosc. 2004;60:721-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 305] [Cited by in RCA: 299] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 3. | Northup PG, Friedman LS, Kamath PS. AGA Clinical Practice Update on Surgical Risk Assessment and Perioperative Management in Cirrhosis: Expert Review. Clin Gastroenterol Hepatol. 2019;17:595-606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 88] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 4. | Navaneethan U, Njei B, Zhu X, Kommaraju K, Parsi MA, Varadarajulu S. Safety of ERCP in patients with liver cirrhosis: a national database study. Endosc Int Open. 2017;5:E303-E314. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Inamdar S, Berzin TM, Berkowitz J, Sejpal DV, Sawhney MS, Chutanni R, Pleskow DK, Trindade AJ. Decompensated cirrhosis may be a risk factor for adverse events in endoscopic retrograde cholangiopancreatography. Liver Int. 2016;36:1457-1463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Leal C, Prado V, Colan J, Chavez-Rivera K, Sendino O, Blasi A, Roura P, Juanola A, Rodriguez de Miguel C, Pavesi M, Gomez C, Guarner C, Guarner-Argente C, Fernández J, Cardenas A. Adverse Events and Acute Chronic Liver Failure in Patients With Cirrhosis Undergoing Endoscopic Retrograde Cholangiopancreatography: A Multicenter Matched-Cohort Study. Am J Gastroenterol. 2019;114:89-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 7. | Macías-Rodríguez RU, Ruiz-Margáin A, Rodriguez-Garcia JL, Zepeda-Gómez S, Torre A. Risk factors associated with complications in cirrhotic patients undergoing endoscopic retrograde cholangio-pancreatography. Eur J Gastroenterol Hepatol. 2017;29:238-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Adler DG, Haseeb A, Francis G, Kistler CA, Kaplan J, Ghumman SS, Laique SN, Munigala S, Taylor LJ, Cox K, Root B, Hayat U, Siddiqui A. Efficacy and safety of therapeutic ERCP in patients with cirrhosis: a large multicenter study. Gastrointest Endosc. 2016;83:353-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 42] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 9. | Jagtap N, Nabi Z, Tandan M, Ramchandani M, Sharma M, Lakhtakia S, Rao PN, Gupta R, Kalapala R, Basha J, Darishetty S, Rao GV, Reddy DN. Is It Safe to Perform Endoscopic Retrograde Cholangiopancreatography in Decompensated Cirrhosis? J Clin Exp Hepatol. 2019;9:554-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 10. | Li DM, Zhao J, Zhao Q, Qin H, Wang B, Li RX, Zhang M, Hu JF, Yang M. Safety and efficacy of endoscopic retrograde cholangiopancreatography for common bile duct stones in liver cirrhotic patients. J Huazhong Univ Sci Technolog Med Sci. 2014;34:612-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 11. | Park DH, Kim MH, Lee SK, Lee SS, Choi JS, Song MH, Seo DW, Min YI. Endoscopic sphincterotomy vs. endoscopic papillary balloon dilation for choledocholithiasis in patients with liver cirrhosis and coagulopathy. Gastrointest Endosc. 2004;60:180-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 78] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 12. | Kim JY, Lee HS, Chung MJ, Park JY, Park SW, Song SY, Bang S. Bleeding Complications and Clinical Safety of Endoscopic Retrograde Cholangiopancreatography in Patients with Liver Cirrhosis. Yonsei Med J. 2019;60:440-445. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 13. | Zhang J, Ye L, Zhang J, Lin M, He S, Mao X, Zhou X, Zhi F. MELD scores and Child-Pugh classifications predict the outcomes of ERCP in cirrhotic patients with choledocholithiasis: a retrospective cohort study. Medicine (Baltimore). 2015;94:e433. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |