Published online Jan 27, 2019. doi: 10.4254/wjh.v11.i1.74
Peer-review started: October 15, 2018
First decision: November 1, 2018
Revised: December 29, 2015
Accepted: January 9, 2019
Article in press: January 9, 2019
Published online: January 27, 2019
Processing time: 107 Days and 21.9 Hours
Chronic liver disease and cirrhosis is the 12th leading cause of death in the United States. Patients with decompensated-cirrhosis, especially with hepatic encephalopathy/coma (HC), have a higher rate of early readmission and contribute to higher healthcare cost.
To evaluate the national inpatient trends of discharges, mortalities and financial impacts associated with four common conditions of cirrhosis.
The publicly available Healthcare Cost and Utilization Project National Inpatient Sample database was utilized to examine the temporal trends of total number of discharges, mortalities and inpatient costs related to hospitalization with a primary diagnosis of HC, transjugular intrahepatic portosystemic shunt (TIPS), esophageal varices with bleeding (EV) and spontaneous bacterial peritonitis (SBP) from 2005 to 2014. The ten-year temporal trends were assessed using simple linear regressions and multiple regression analysis. Two-sided P < 0.05 was considered statistically significant.
From 2005 to 2014, the total number of discharges with cirrhosis-associated complications trended up for HC, SBP and EV (HC by 70% increase, P < 0.0001; SBP by 819% increase, P = 0.0002; EV by 9% increase, P = 0.016), but not for TIPS (P = 0.90). HC related to viral hepatitis showed faster increase by 357% (P < 0.0001) in comparison to HC not related to viral hepatitis by 33 % (P = 0.0006). Overall, in-hospital mortality rates for each condition decreased from 2005 to 2014 (HC by 29% reduction, P = 0.0024; SBP by 26% reduction, P = 0.0038; TIPS by 32% reduction, P = 0.021) except for EV (P = 0.34). After adjustment for inflation, aggregate cost of hospitalization for EV, HC, and SBP significantly increased by 20%, 86%, and 980%, respectively, from 2005 to 2014 (all P < 0.02), while TIPS had trend toward decreasing cost by 3% (P = 0.95).
The number of hospitalizations and costs for some of the cirrhosis-associated conditions increased. However, the inpatient mortality rates for most of these conditions decreased.
Core tip: Understanding recent temporal trends of cirrhosis-associated conditions is an important aspect of developing strategies to reduce health care cost. Our study showed increasing trends of hospital discharges related to cirrhosis-associated conditions despite the decreasing trends for total hospital discharges across the nation. Importantly, hepatic coma associated with viral hepatitis showed rapid increase in discharge volume in comparison to hepatic coma not associated with viral hepatitis. After adjusting for inflation, cirrhosis associated conditions showed disproportionately greater increase in aggregate cost compare to national trends. This suggests that prevention of hospitalizations secondary to cirrhosis-associated conditions likely reduces overall health care cost.
- Citation: Sempokuya T, Zhang G, Nakagawa K. Temporal trends of cirrhosis associated conditions. World J Hepatol 2019; 11(1): 74-85
- URL: https://www.wjgnet.com/1948-5182/full/v11/i1/74.htm
- DOI: https://dx.doi.org/10.4254/wjh.v11.i1.74
Chronic liver disease and cirrhosis is the 12th leading cause of death in the United States[1]. Cirrhosis is associated with multiple life-threatening complications such as intraabdominal infections, hepatic encephalopathy/coma (HC), portal hypertension, esophageal varices and hepatocellular carcinoma. These complications are suggestive of decompensated-cirrhosis and are indicative of worse prognosis among patients with cirrhosis[2,3]. In addition, patients with decompensated-cirrhosis, especially with HC, have a higher rate of early readmission and contribute to higher healthcare cost[4-6]. Other cirrhosis-associated complications such as portal hypertension, renal dysfunction and infections were also associated with higher inpatient mortality[7].
Reducing the preventable hospitalizations and readmissions are the focus of recent national initiatives with the goal of improving quality of care and reducing health care costs. Therefore, optimal management of cirrhosis to prevent decompensated-cirrhosis is emphasized. However, there is limited data on the temporal trend of hospitalizations and mortality associated with cirrhosis-associated complications. Recent retrospective studies showed a decline in the number of hospitalizations for esophageal varices with bleeding (EV)[8-10]. However, there is paucity of data on other cirrhosis-associated conditions. Therefore, we conducted a larger population-based study to evaluate the national temporal trends of hospitalizations, mortalities and financial impact associated with four common conditions of cirrhosis: HC; intraabdominal venous shunt (transjugular intrahepatic portosystemic shunt or TIPS); EV; spontaneous bacterial peritonitis (SBP).
National Inpatient Sample (NIS), the largest all-payer database of inpatient care in the United States, from the Healthcare Cost and Utilization Project (HCUP) published by the Agency for Healthcare Research and Quality, contains data from over 7-million hospital discharges each year from over 1000 hospitals and is weighted to produce national estimates[11]. The HCUP validates the NIS for biases by comparing it with other population-based data sets[12] and NIS data have been utilized and published in the past[13-17]. There was a change in sampling methods in 2012, but the collection date was adjusted for this change[11,18]. Data reporting met the NIS data use agreement as established by the HCUP[11]. Since we utilized publicly-accessible, de-identified administrative level aggregate data, rather than patient-specific data, approval from the institutional review board was not required to conduct the study.
We conducted a retrospective study utilizing the NIS to assess 10 year temporal trends from 2005 to 2014 for total number of discharges, death, mortality, length of stay (LOS), mean charges, aggregate charges, aggregate costs, age, sex, insurance types (Medicare, Medicaid, Private insurance, Uninsured, Other or Missing) and bed size (Small, Medium and Large) related to hospitalization, with a primary diagnosis of HC, TIPS, EV and SBP, using International Classification of Diseases (ICD)-9 codes (HC: 572.2; HC secondary to viral hepatitis: 070.0, 070.20-23, 070.41-44, 070.49, 070.6, 070.71; TIPS: 39.1; EV: 456.0; SBP: 567.23)[11,19]. A primary diagnosis is the main reason why patients are hospitalized, rather than a secondary diagnosis which sometimes used to identify continuation of treatment for chronic conditions in the hospital. These ICD-9 codes have been validated in literature except HC secondary to viral hepatitis[19]. Codes for HC secondary to viral hepatitis include acute viral hepatitis resulted in HC. However, if providers used codes for unspecified acute liver failure which resulted in HC from viral hepatitis, our analysis was unable to include these populations due to lack of specificity of codes. As the coding behavior is becoming more specific due to insurance requirement, we expect that inclusion codes related to HC secondary to viral hepatitis will be an important part of analysis. This will allow us to evaluate if the changes related to HC is merely an artifact of coding behavior. We also obtained data for a National all-cause hospitalization (national) for a comparison. Importantly, the ICD-9 code for SBP, 567.23, was introduced in 2005[13]. We only evaluated a primary diagnosis of ICD-9 codes rather than a secondary diagnosis to avoid duplication in the data. We chose to end the study period in 2014 since the official transition from ICD-9 codes to ICD-10 codes occurred nationally in 2015.
A biomedical statistician GZ reviewed and performed statistical analysis. Both charges and costs were inflation-adjusted using the appropriate Consumer Price Index (http://www.bls.gov/cpi/) and all converted to 2014 United States dollars. We compared the 10-year temporal trends of discharges, mortalities, charges and costs data using simple linear regressions using SAS version 9.4 (SAS Institute Inc., Cary, NC). We also used multiple regression analysis to explore the adjustments of mean age and LOS for outcomes that showed significant temporal trends in simple regressions. Nonrandom temporal trends (or “special-cause variation”) were also demonstrated by run charts using the statistical process control decision rule: there are 6 or more consecutive data points always going up or going down over time[20]. Two-sided P < 0.05 was considered statistically significant without multiple comparison adjustments.
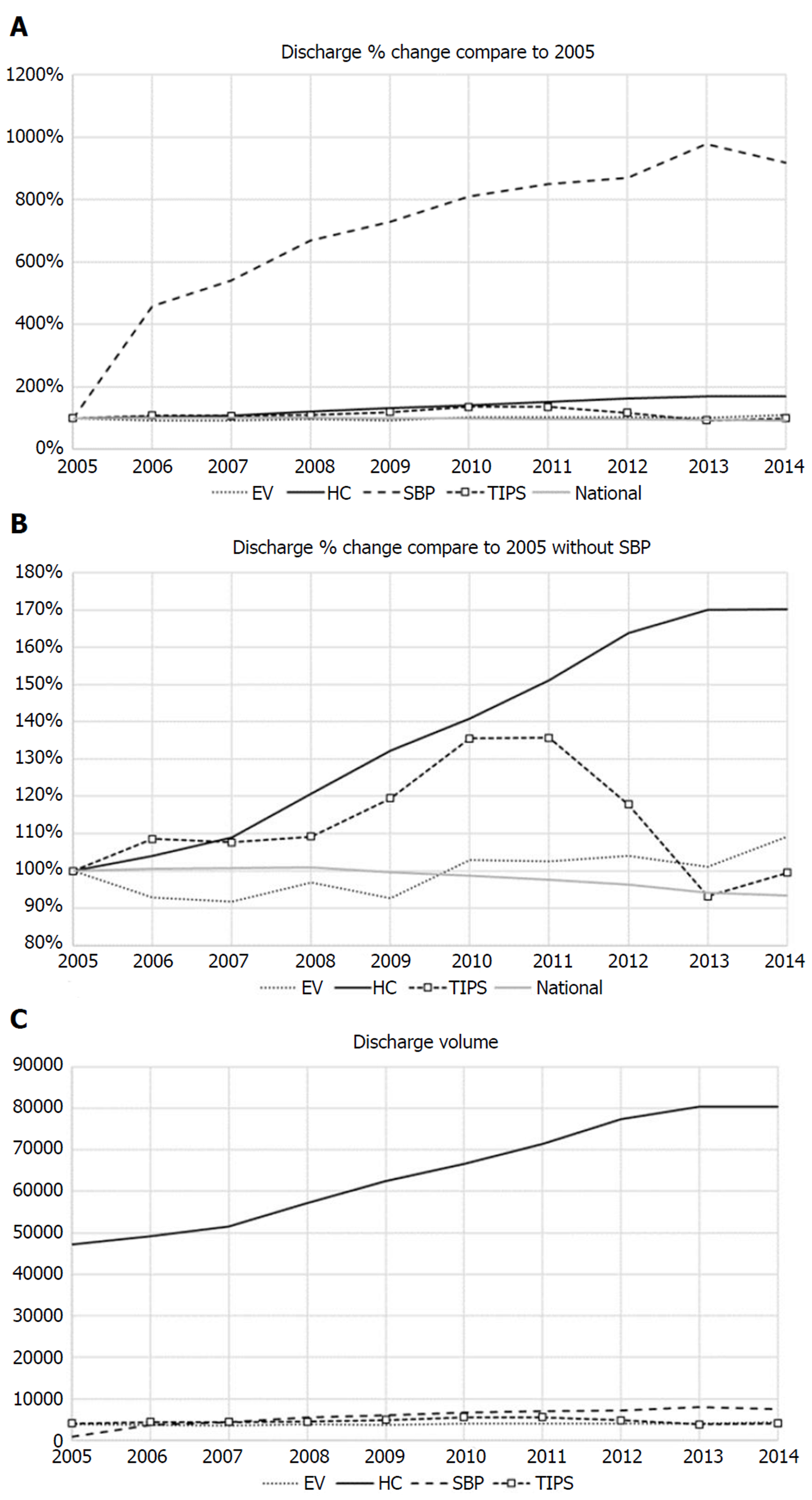
Temporal trends of discharges for cirrhosis-associated conditions are shown in Figure 1A-C. From 2005 to 2014, the primary diagnosis of four cirrhosis related pathologies were all trending up except TIPS [HC, 47268 to 80470 by 70% increase, slope estimate (annual change rate) = 4205 [95% confidence interval (CI) = 3739 to 4671], P < 0.0001; SBP, 821 to 7545 by 819% increase, slope = 660 (428 to 893), P = 0.0002; EV, 3942 to 4305 by 9% increase, slope = 55 (13 to 96), P = 0.016; TIPS, 4079 to 4060 by < 1% decrease, slope = 9 (-151 to 168), P = 0.90]. Nationally, the total number of discharges decreased from 37843039 to 35358818 by 7% [slope = -316319 (-433063 to -199576), P = 0.0002]. Similar significance of temporal trends of these discharges remained if adjusted for mean age and LOS, and both variables did not show significant change over time (all P > 0.11). HC not related to viral hepatitis (ICD-9 code 572.2) increased from 41796 to 55485 by 33% from 2005 to 2014 [slope = 1688 (968 to 2408), P = 0.0006], while HC related to viral hepatitis (070.0, 070.20-23, 070.41-44, 070.49, 070.6, 070.71) increased faster, from 5472 to 24985 by 357% [slope = 2517 (1732 to 3302), P < 0.0001].
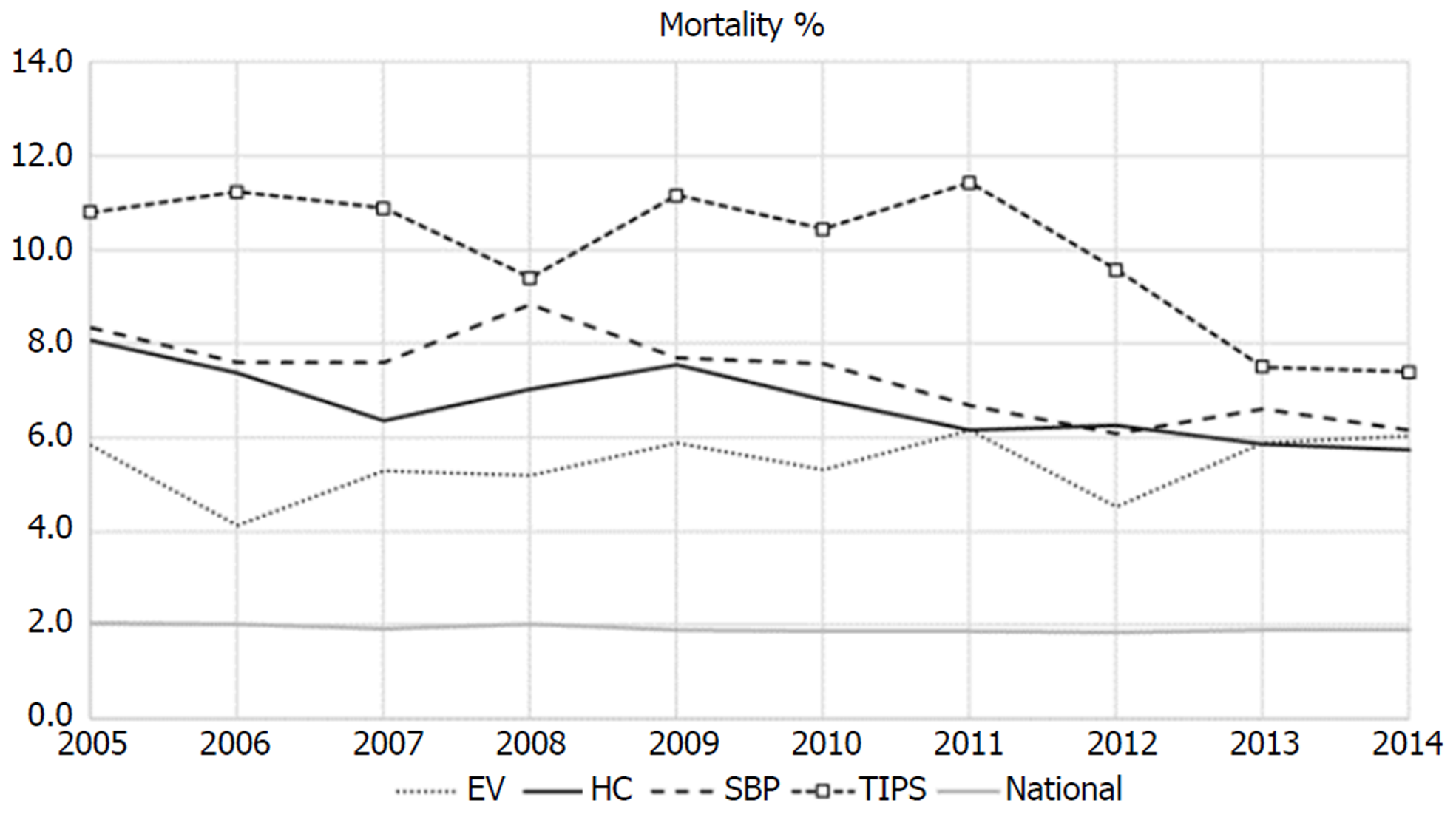
Overall as described in Figure 2, in-hospital mortality rates for each condition significantly decreased from 2005 to 2014 [HC: 8.06% to 5.73% by 29% reduction, slope = -0.21% (-0.33% to -0.10%), P = 0.0024; SBP: 8.34% to 6.16% by 26% reduction, slope = -0.25% (-0.39% to -0.10%), P = 0.0038; TIPS: 10.81% to 7.39% by 32% reduction, slope = -0.35% (-0.64% to -0.07%), P = 0.021] except for EV (5.84% to 6.04%; P = 0.34). If adjusted for mean age and LOS, SBP was still reduced significantly (P = 0.034), but TIPS were no longer significant (P = 0.067). The changes in in-hospital mortality rates might be associated with the variations of mean LOS but not with mean age. For example, one-day reduction in mean LOS seemed significantly associated with a reduction in TIPS mortality rates of 1.73% (0.69% to 2.76%), P = 0.007. There was also a statistically significant reduction on national mortality rate, from 2.04% to 1.90%, or a 7% reduction, slope = -0.018% (-0.031% to -0.006%), P = 0.011.
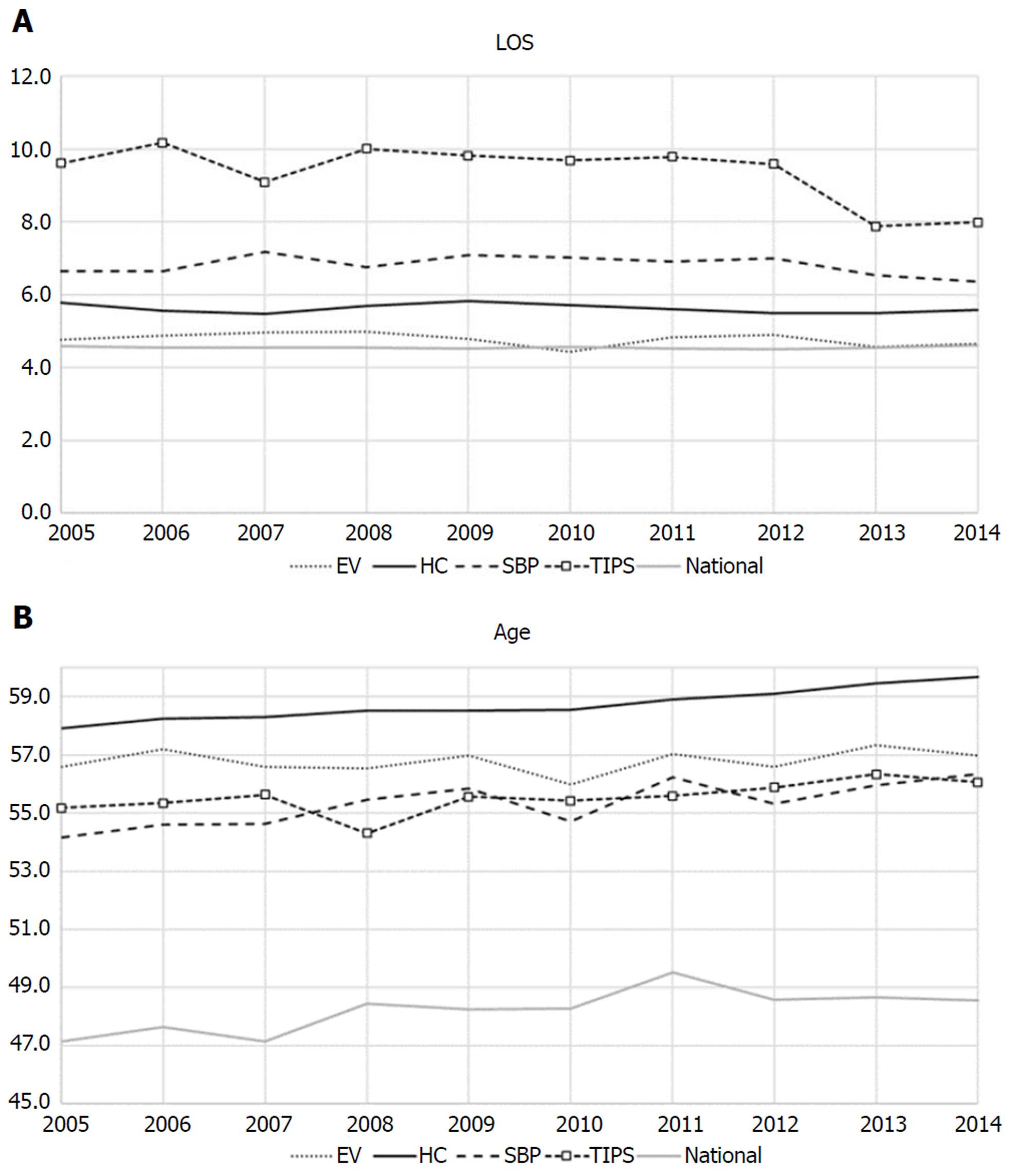
Figure 3 shows the 10-year trends for mean LOS and mean ages. Mean LOS for TIPS decreased from 9.6 d in 2005 to 8.0 in 2014 with 17% decrease [slope = -0.18 (-0.34 to -0.01), P = 0.038]. However, other cirrhosis related conditions and national LOS did not show any significant changes. TIPS had persistently higher LOS as compared to other conditions. Mean ages of cirrhosis-associated conditions were consistently higher than national average, and HC persistently had the highest mean age.
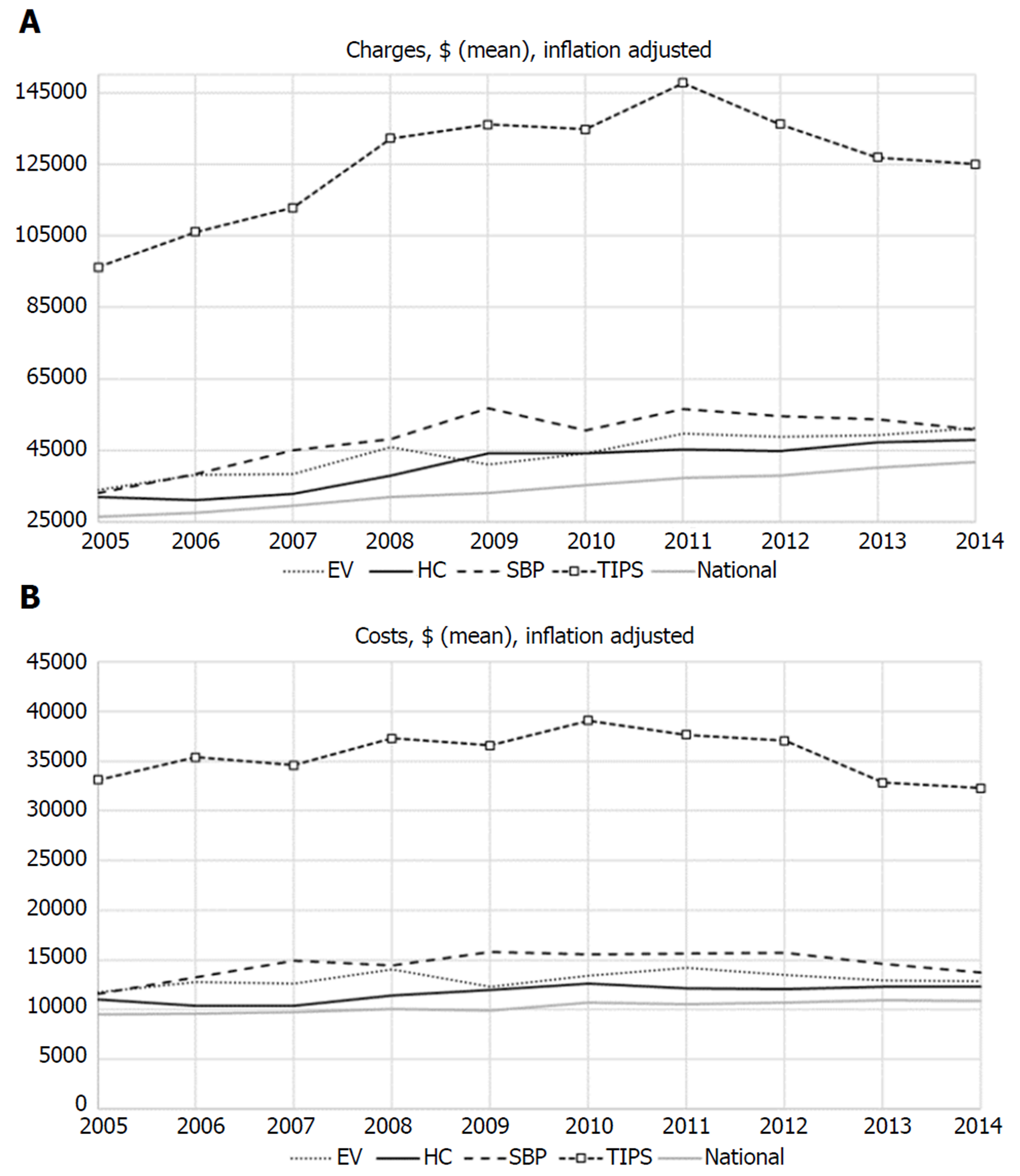
Figure 4A shows mean charges of four cirrhosis-associated conditions that have been increasing more than 30% compared to 2005 data, after adjustment for inflation [HC, $32045 to $47929 by 50% up, slope = 2042$/year (1425 to 2660), P < 0.0001; EV, $33979 to $51336 by 51% up, slope = 1822$/year (1238 to 2406), P < 0.0001; TIPS, $45425 to $59130 by 30% up, P = 0.0022; SBP, $33151 to $50824 by 53% up, slope = 2019$/year (687 to 3352), P=0.008; from 2005 to 2014). Nationally, mean charge increased from $26323 to $41633, or a 58% increase [slope = 1739$/year (1646 to 1833), P < 0.0001]. Temporal trends of these mean charges were still significant (all P < 0.012) after further adjustment for mean age and LOS. Figure 4B shows mean costs associated with four cirrhosis-associated conditions. This figure demonstrates that TIPS has persistently higher cost related to hospitalizations. Compared to mean charges, mean costs had less variation over time. The mean costs of TIPS, EV and SBP did not increase significantly over time (all P > 0.15). Only HC significantly increased mean costs from $11041 in 2005 to $12282, or a 12% increase, slope = 217$/year (92 to 341), P = 0.004 (after adjusting for mean age and LOS, P = 0.002).
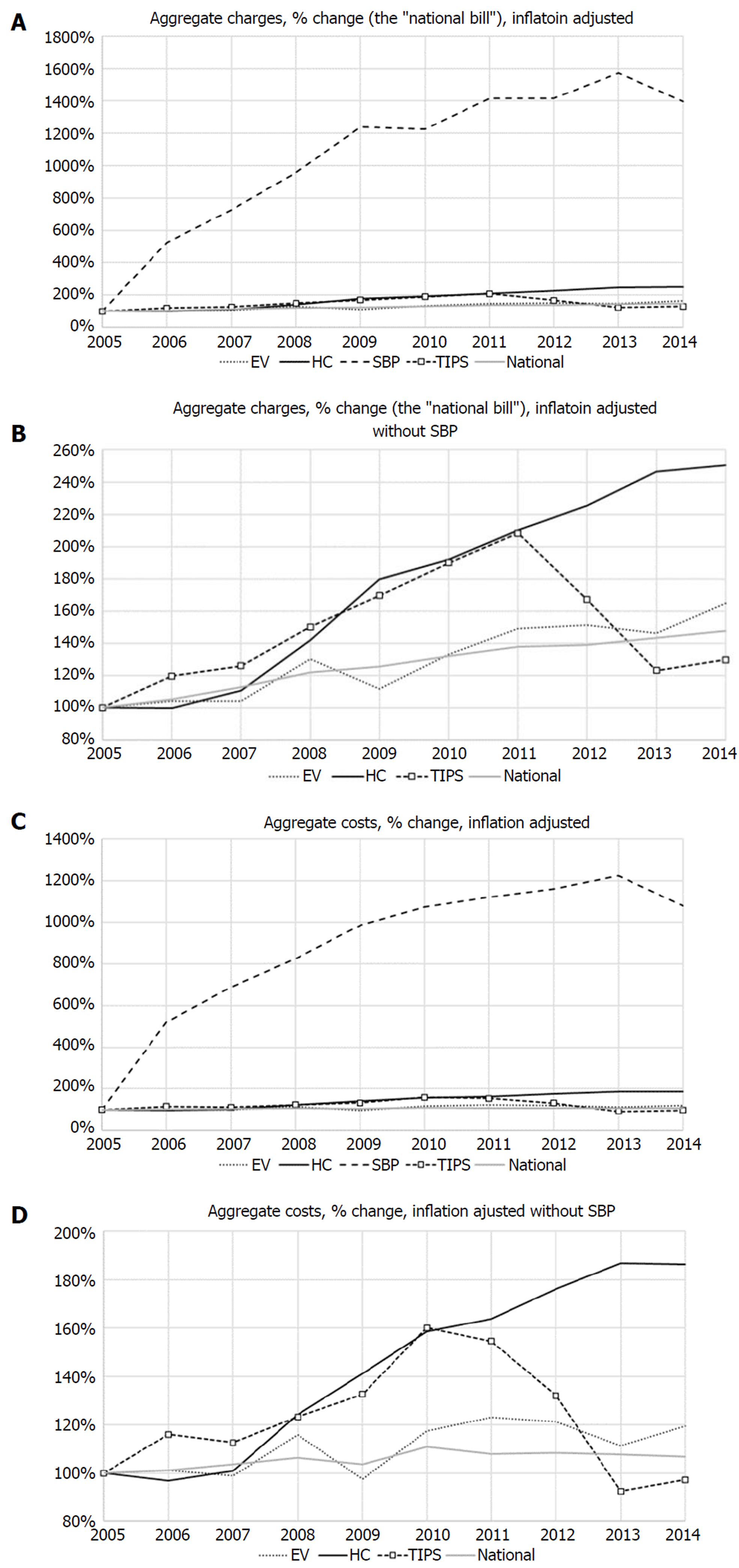
After adjustment for inflation, aggregate charges (so called “national bill”) for hospitalizations related to EV, HC, SBP, TIPS and national increased by 65%, 150%, 1296%, 30 % and 48 %, respectively, from 2005 to 2014 (all P ≤ 0.0001 except for EV, P = 0.30) (Figure 5a and 5b). Inflation adjusted aggregate costs of hospitalization for EV, HC, SBP and national increased by 20%, 86%, 980% and 7%, respectively, from 2005 to 2014 (all P < 0.02), while TIPS trended toward a decreased by 3% (P = 0.95) (Figure 5C and 5D).
Table 1 and Table 2 shows age and sex distributions, insurance coverage and bed size for 2005 and 2014 respectively. For four cirrhosis-associated conditions, proportions of patients are shifting from large hospitals to small-medium sized hospitals.
| Diagnosis (2005) | HC | SBP | EV | TIPS | ||||
| All discharges | 47268 | 821 | 3942 | 4079 | ||||
| Male (%) | 61.4 | 66.7 | 67.7 | 66.5 | ||||
| Age, mean | 57.9 | 54.2 | 56.6 | 55.2 | ||||
| Age | n | % | n | % | n | % | n | % |
| 18-44 | 4648 | 9.8 | 136 | 16.6 | 566 | 14.4 | 479 | 11.8 |
| 45-64 | 29350 | 62.1 | 471 | 57.4 | 2196 | 55.7 | 2600 | 63.7 |
| 65-84 | 12623 | 26.7 | 189 | 23.0 | 996 | 25.3 | 888 | 21.8 |
| 85+ | 622 | 1.3 | N/A | N/A | 122 | 3.1 | N/A | N/A |
| Payer | ||||||||
| Medicare | 20002 | 42.3 | 338 | 41.2 | 1298 | 32.9 | 1243 | 30.5 |
| Medicaid | 11819 | 25.0 | 181 | 22.1 | 639 | 16.2 | 870 | 21.3 |
| Private insurance | 10833 | 22.9 | 193 | 23.5 | 1271 | 32.2 | 1555 | 38.1 |
| Uninsured | 2785 | 5.9 | 65 | 7.9 | 537 | 13.6 | 237 | 5.8 |
| Other | 1782 | 3.8 | N/A | N/A | 192 | 4.9 | 174 | 4.3 |
| Missing | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Bed sizes | ||||||||
| Small | 4869 | 10.3 | 111 | 13.5 | 520 | 13.2 | 55 | 1.3 |
| Medium | 12046 | 25.5 | 167 | 20.4 | 1017 | 25.8 | 861 | 21.1 |
| Large | 30354 | 64.2 | 543 | 66.1 | 2405 | 61.0 | 3163 | 77.5 |
| Diagnosis (2014) | HC | SBP | EV | TIPS | ||||
| All discharges | 80470 | 7545 | 4305 | 4060 | ||||
| Male (%) | 60.4 | 62.5 | 65.5 | 64.3 | ||||
| Age, mean | 59.7 | 56.3 | 57.0 | 56.1 | ||||
| Age | n | % | n | % | n | % | n | % |
| 18-44 | 5525 | 6.9 | 945 | 12.5 | 600 | 13.9 | 425 | 10.5 |
| 45-64 | 50085 | 62.2 | 4715 | 62.5 | 2540 | 59.0 | 2660 | 65.5 |
| 65-84 | 23770 | 29.5 | 1680 | 22.3 | 1000 | 23.2 | 885 | 21.8 |
| 85+ | 1080 | 1.3 | 105 | 1.4 | 125 | 2.9 | N/A | N/A |
| Payer | ||||||||
| Medicare | 38995 | 48.5 | 3005 | 39.8 | 1445 | 33.6 | 1455 | 35.8 |
| Medicaid | 19545 | 24.3 | 2005 | 26.6 | 985 | 22.9 | 990 | 24.4 |
| Private insurance | 15745 | 19.6 | 1940 | 25.7 | 1225 | 28.5 | 1200 | 29.6 |
| Uninsured | 3240 | 4.0 | 360 | 4.8 | 470 | 10.9 | 270 | 6.7 |
| Other | 2715 | 3.4 | 220 | 2.9 | 175 | 4.1 | 125 | 3.1 |
| Missing | 229.999 | 0.3 | N/A | N/A | N/A | N/A | N/A | N/A |
| Bed sizes | ||||||||
| Small | 13620 | 16.9 | 1065 | 14.1 | 830 | 19.3 | 255 | 6.3 |
| Medium | 23280 | 28.9 | 2060 | 27.3 | 1265 | 29.4 | 1000 | 24.6 |
| Large | 43570 | 54.1 | 4420 | 58.6 | 2210 | 51.3 | 2805 | 69.1 |
Discharges with a primary diagnosis of HC, SBP, or EV showed increasing trends despite the decreasing trend for total hospitalizations across the nation over a 10-year period, from 2005 to 2014. Especially for SBP, trends show an 819% increase in hospitalization for this primary diagnosis over 10 years. Hospitalization due to HC also demonstrated significant increase over the study period, mainly attributable to the increase in HC coding specifically related to viral hepatitis. Approximately 20.5% of HC is precipitated by SBP[21]. Therefore, increasing SBP with increasing HC suggests actual increase in case number along with change in coding behavior. One recent study showed that there was an increase in hepatitis C virus infection-related mortality from 2007 to 2013, and this may explain increasing trends of hepatic coma related to viral hepatitis[22]. The referenced study also noted decreasing mortality related to hepatitis C infection from 2014 to 2016 due to introduction of direct-acting antiviral agents[22]. Therefore, trends may change beyond 2014 and future study to assess this change will be necessary. Previous population-based studies[8-10] showed declining numbers of esophageal varices-related hospitalizations, which is in contrast to our findings. One possible explanation is that our study consisted of more recent data compared to the published studies. Jamal et al[8] used data from 1988 to 2002, Lim et al[9] used data from 1998 to 2009 and Pant et al[10] used data from 2002 to 2012. Furthermore, Pant et al[10] who also utilized data from NIS by HCUP, studied only the EV patients who had concurrent diagnosis of cirrhosis. Our study only looked at a primary diagnosis of EV, therefore secondary diagnosis of EV was not included which may have accounted for the differences in the study results. In addition, there was a change in sampling methods for NIS in 2012, which may have also impacted the differences in our results compared to the prior studies[11].
Overall, in-hospital mortality rates for cirrhosis-associated conditions generally decreased over a 10-year period except for EV, even though there were no significant trends in the overall all-cause inpatient national mortality rate. This may reflect the advances in pharmacotherapy such as introduction of rifaximin for HC treatment. Another possible explanation is that mortality related to hepatitis B virus infection declined from 2007 to 2016, likely due to improvement of care of hepatitis B virus infection[22]. Since patients with decompensated cirrhosis, especially from HC, are at risk for increased frequency of hospital readmission[4-6], reducing the in-patient mortality rates may be contributing to the number of readmissions following the index admission. However, our study was not designed to assess the number of readmissions in order to address this possibility. Kanwal et al[23] showed there is an increasing trend for post discharge mortality related to cirrhosis admission, which has likely replaced inpatient mortality. Therefore, decreasing inpatient mortality may not reflect actual improvement of care related to cirrhosis. Interestingly, TIPS showed significant decrease in the hospital LOS from 9.6 in 2005 to 8.0 in 2014 by 17% down (P < 0.04), but other cirrhosis-associated conditions did not play a significant role in the LOS. This finding is different from a previous study that evaluated TIPS from 1998 to 2012, which showed relatively constant LOS for TIPS-related admissions[24]. TIPS had persistently high LOS compared to other diagnosis, however this comparison may not be appropriate as the ICD-9 code for TIPS was a procedure code rather than a diagnostic code. In addition, there was a recent trend of minimizing post-procedural hospital stays[25].
Finally, our aggregate financial analysis suggests that mean charges of cirrhosis-associated conditions increased over a 10-year period after adjusting for inflation. A similar increased trend was also seen in the national all-cause hospitalization. However, increase in aggregate cost for primary diagnosis of EV, HC and SBP was disproportionately greater (45% increase) than the increase in aggregate cost for national trends (7% increase) after adjusting for inflation. This suggests that prevention of hospitalizations secondary to cirrhosis-associated conditions likely reduces overall health care cost.
There are some limitations to our study, which are mostly associated with the lack of patient-level, detailed clinical information as a result of using an aggregate claims database. Also, we cannot rule out the possibility of temporal changes in the reporting bias for these conditions, since the reporting process for the discharge diagnoses may have become more specific over recent years with more prevalent use of electronic medical records. Therefore, it is unclear if increasing numbers of cirrhosis-associated discharges based on ICD-9 codes reflects actual increases in prevalence of the conditions vs increase in more accurate reporting of these conditions. In addition, previous studies have not validated ICD-9 codes related to HC secondary to viral hepatitis. Therefore, use of unvalidated codes may skew results. Further prospective studies are needed to find the explanations of these trends. We also utilized ICD-9 diagnostic codes for HC, EV and SBP, and an ICD-9 procedure code was utilized for TIPS. Therefore, comparison between ICD-9 diagnostic codes and procedure codes may not reflect differences in the respective trends. We understand that determining the reason for TIPS is important as prognosis may differ for different causes. However, NIS data did not allow us to separate etiologies. Additional studies to look at this difference would be appropriate.
In summary, we observed significant temporal increase in hospitalization due to cirrhosis-associated complications except for TIPS[2,3]. EV, HC and especially SBP had significant increases in aggregate hospitalization cost. Strategies to prevent readmission in the era of decreasing mortality rate are needed to effectively reduce healthcare cost.
There is limited data on recent temporal trends of cirrhosis associated conditions in the United States, which is critical to identify problems related to hospitalizations.
Healthcare cost reduction, especially in the United States, is a current focus on providing cost-effective care. Recognizing problems in temporal trends enables to create action plan to reduce unnecessary costs.
We aim to conduct a descriptive study to identify 10-year temporal trends of cirrhosis associated conditions which can guide future prospective studies.
We used publicly available National Inpatient Sample to conduct 10-year trends analysis of cirrhosis associated conditions identified by ICD-9 codes from 2005 to 2014. Simple linear regression and multiple regression models were utilized for statistical analysis.
The total number of discharges of Hepatic encephalopathy/coma (HC), Spontaneous bacteria peritonitis (SBP) and esophageal varices with bleeding (EV) had significant increase. Notably, HC associated with viral hepatitis showed faster rate of increase of hospitalizations. Mortalities has decreased for HC, SBP and transjugular intrahepatic portosystemic shunt (TIPS), but no change was observed for EV. Aggregate cost of hospitalizations for HC, EV and SBP had significant increase after adjustment for inflation; however TIPS showed non-significant trends toward decreasing cost.
The number of hospitalizations and costs for some of the cirrhosis-associated conditions increased. Especially, HC related to viral hepatitis showed fast rate of increase which suggest appropriate treatment of viral hepatitis maybe necessary to reduce HC in these population. In addition, the inpatient mortality rates for most of these conditions decreased.
Viral hepatitis related cirrhosis maybe contributing to high cost of hospitalization especially hospitalization related to HC. These findings suggest necessity of studies beyond 2014 after introduction of newer antiviral agents for hepatitis C as well as studies to identify trends of re-admission and post-hospitalization mortality.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Silva LD, Loustaud-Ratti V S- Editor: Dou Y L- Editor: A E- Editor: Tan WW
| 1. | Kochanek KD, Murphy SL, Xu J, Tejada-Vera B. Deaths: Final Data for 2014. Natl Vital Stat Rep. 2016;65:1-122. [PubMed] |
| 2. | Zipprich A, Garcia-Tsao G, Rogowski S, Fleig WE, Seufferlein T, Dollinger MM. Prognostic indicators of survival in patients with compensated and decompensated cirrhosis. Liver Int. 2012;32:1407-1414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 197] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 3. | Ampuero J, Montoliú C, Simón-Talero M, Aguilera V, Millán R, Márquez C, Jover R, Rico MC, Sendra C, Serra MÁ, Romero-Gómez M. Minimal hepatic encephalopathy identifies patients at risk of faster cirrhosis progression. J Gastroenterol Hepatol. 2018;33:718-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 39] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 4. | Volk ML, Tocco RS, Bazick J, Rakoski MO, Lok AS. Hospital readmissions among patients with decompensated cirrhosis. Am J Gastroenterol. 2012;107:247-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 303] [Cited by in RCA: 363] [Article Influence: 27.9] [Reference Citation Analysis (0)] |
| 5. | Bajaj JS, Reddy KR, Tandon P, Wong F, Kamath PS, Garcia-Tsao G, Maliakkal B, Biggins SW, Thuluvath PJ, Fallon MB, Subramanian RM, Vargas H, Thacker LR, O'Leary JG; North American Consortium for the Study of End-Stage Liver Disease. The 3-month readmission rate remains unacceptably high in a large North American cohort of patients with cirrhosis. Hepatology. 2016;64:200-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 194] [Article Influence: 21.6] [Reference Citation Analysis (0)] |
| 6. | Tapper EB, Halbert B, Mellinger J. Rates of and Reasons for Hospital Readmissions in Patients With Cirrhosis: A Multistate Population-based Cohort Study. Clin Gastroenterol Hepatol. 2016;14:1181-1188.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 169] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 7. | Charatcharoenwitthaya P, Soonthornworasiri N, Karaketklang K, Poovorawan K, Pan-Ngum W, Chotiyaputta W, Tanwandee T, Phaosawasdi K. Factors affecting mortality and resource use for hospitalized patients with cirrhosis: A population-based study. Medicine (Baltimore). 2017;96:e7782. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Jamal MM, Samarasena JB, Hashemzadeh M, Vega KJ. Declining hospitalization rate of esophageal variceal bleeding in the United States. Clin Gastroenterol Hepatol. 2008;6:689-95; quiz 605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Lim N, Desarno MJ, Lidofsky SD, Ganguly E. Hospitalization for variceal hemorrhage in an era with more prevalent cirrhosis. World J Gastroenterol. 2014;20:11326-11332. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Pant C, Desai M, Deshpande A, Taylor R, Olyaee M, Gilroy R. Esophageal variceal bleeding in hospitalized patients with cirrhosis. J Hosp Med. 2015;10:453-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project. Available from: https://hcupnet.ahrq.gov/. |
| 12. | Agency for Healthcare Research and Quality. Healthcare cost and utilization project methods series; 2011. Available from: https://www.hcup-us.ahrq.gov/reports/methods/methods.jsp. |
| 13. | Allen AM, Kim WR, Moriarty JP, Shah ND, Larson JJ, Kamath PS. Time trends in the health care burden and mortality of acute on chronic liver failure in the United States. Hepatology. 2016;64:2165-2172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 137] [Article Influence: 15.2] [Reference Citation Analysis (1)] |
| 14. | Wang YR, Fisher RS, Parkman HP. Gastroparesis-related hospitalizations in the United States: trends, characteristics, and outcomes, 1995-2004. Am J Gastroenterol. 2008;103:313-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 221] [Cited by in RCA: 217] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 15. | Zogg CK, Najjar P, Diaz AJ, Zogg DL, Tsai TC, Rose JA, Scott JW, Gani F, Alshaikh H, Canner JK, Schneider EB, Goldberg JE, Haider AH. Rethinking Priorities: Cost of Complications After Elective Colectomy. Ann Surg. 2016;264:312-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 56] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 16. | Reddy SK, Zhan M, Alexander HR, El-Kamary SS. Nonalcoholic fatty liver disease is associated with benign gastrointestinal disorders. World J Gastroenterol. 2013;19:8301-8311. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 26] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 17. | Peck JR, Latchana N, Michaels A, Hanje AJ, Hinton A, Elkhammas EA, Black SM, Mumtaz K. Diagnosis of morbid obesity may not impact healthcare utilization for orthotopic liver transplantation: A propensity matched study. World J Hepatol. 2017;9:595-602. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Khera R, Angraal S, Couch T, Welsh JW, Nallamothu BK, Girotra S, Chan PS, Krumholz HM. Adherence to Methodological Standards in Research Using the National Inpatient Sample. JAMA. 2017;318:2011-2018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 434] [Cited by in RCA: 577] [Article Influence: 72.1] [Reference Citation Analysis (0)] |
| 19. | Nehra MS, Ma Y, Clark C, Amarasingham R, Rockey DC, Singal AG. Use of administrative claims data for identifying patients with cirrhosis. J Clin Gastroenterol. 2013;47:e50-e54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 186] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 20. | Perla RJ, Provost LP, Murray SK. The run chart: a simple analytical tool for learning from variation in healthcare processes. BMJ Qual Saf. 2011;20:46-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 316] [Cited by in RCA: 398] [Article Influence: 30.6] [Reference Citation Analysis (0)] |
| 21. | Mumtaz K, Ahmed US, Abid S, Baig N, Hamid S, Jafri W. Precipitating factors and the outcome of hepatic encephalopathy in liver cirrhosis. J Coll Physicians Surg Pak. 2010;20:514-518. [PubMed] |
| 22. | Kim D, Li AA, Gadiparthi C, Khan MA, Cholankeril G, Glenn JS, Ahmed A. Changing Trends in Etiology-Based Annual Mortality From Chronic Liver Disease, From 2007 Through 2016. Gastroenterology. 2018;155:1154-1163.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 174] [Article Influence: 24.9] [Reference Citation Analysis (0)] |
| 23. | Kanwal F, Tansel A, Kramer JR, Feng H, Asch SM, El-Serag HB. Trends in 30-Day and 1-Year Mortality Among Patients Hospitalized With Cirrhosis From 2004 to 2013. Am J Gastroenterol. 2017;112:1287-1297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 47] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 24. | Lee EW, Kuei A, Saab S, Busuttil RW, Durazo F, Han SH, El-Kabany MM, McWilliams JP, Kee ST. Nationwide trends and predictors of inpatient mortality in 83884 transjugular intrahepatic portosystemic shunt. World J Gastroenterol. 2016;22:5780-5789. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 19] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 25. | Goodney PP, Stukel TA, Lucas FL, Finlayson EV, Birkmeyer JD. Hospital volume, length of stay, and readmission rates in high-risk surgery. Ann Surg. 2003;238:161-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 195] [Cited by in RCA: 227] [Article Influence: 10.3] [Reference Citation Analysis (0)] |