Published online Oct 27, 2018. doi: 10.4254/wjh.v10.i10.761
Peer-review started: May 3, 2018
First decision: May 17, 2018
Revised: June 24, 2018
Accepted: June 28, 2018
Article in press: June 29, 2018
Published online: October 27, 2018
Processing time: 179 Days and 17.6 Hours
To assess prevalence of pre-existing atrial fibrillation (AF) and/or incidence of AF following liver transplantation, and the trends of patient’s outcomes overtime; to evaluate impact of pre-existing AF and post-operative AF on patient outcomes following liver transplantation.
A literature search was conducted utilizing MEDLINE, EMBASE and Cochrane Database from inception through March 2018. We included studies that reported: (1) prevalence of pre-existing AF or incidence of AF following liver transplantation; or (2) outcomes of liver transplant recipients with AF. Effect estimates from the individual study were extracted and combined utilizing random-effect, generic inverse variance method of DerSimonian and Laird. The protocol for this meta-analysis is registered with PROSPERO (International Prospective Register of Systematic Reviews, No. CRD42018093644).
Twelve observational studies with a total of 38586 liver transplant patients were enrolled. Overall, the pooled estimated prevalence of pre-existing AF in patients undergoing liver transplantation was 5.4% (95%CI: 4.9%-5.9%) and pooled estimated incidence of AF following liver transplantation was 8.5% (95%CI: 5.2%-13.6%). Meta-regression analyses were performed and showed no significant correlations between year of study and either prevalence of pre-existing AF (P = 0.08) or post-operative AF after liver transplantation (P = 0.54). The pooled OR of mortality among liver transplant recipients with pre-existing AF was 2.34 (2 studies; 95%CI: 1.10-5.00). In addition, pre-existing AF is associated with postoperative cardiovascular complications among liver transplant recipients (3 studies; OR: 5.15, 95%CI: 2.67-9.92, I2 = 64%). With limited studies, two studies suggested significant association between new-onset AF and poor clinical outcomes including mortality, cerebrovascular events, post-transplant acute kidney injury, and increased risk of graft failure among liver transplant recipients (P < 0.05).
The overall estimated prevalence of pre-existing AF and incidence of AF following liver transplantation are 5.4% and 8.5%, respectively. Incidence of AF following liver transplant does not seem to decrease overtime. Pre-existing AF and new-onset AF are potentially associated with poor clinical outcomes post liver transplantation.
Core tip: Atrial fibrillation (AF) occurs in a substantial number of postoperative and post-transplantation patients. In addition, postoperative AF confers both short-term and long-term morbidity and mortality in liver transplant patients. However, the incidence of postoperative AF in patients undergoing liver transplantation and its impacts remain unclear. To further investigate, we conducted a meta-analysis to assess the rates of preexisting AF and AF following liver transplantation as well as the outcomes of liver transplant patients with AF. Incidence of AF following liver transplant does not seem to decrease overtime. Pre-existing AF and new-onset AF are potentially associated with poor clinical outcomes post liver transplantation.
- Citation: Chokesuwattanaskul R, Thongprayoon C, Bathini T, Ungprasert P, Sharma K, Wijarnpreecha K, Pachariyanon P, Cheungpasitporn W. Liver transplantation and atrial fibrillation: A meta-analysis. World J Hepatol 2018; 10(10): 761-771
- URL: https://www.wjgnet.com/1948-5182/full/v10/i10/761.htm
- DOI: https://dx.doi.org/10.4254/wjh.v10.i10.761
Atrial fibrillation (AF) is one of the most common heart diseases, affecting 3 to 6 million populations in the United States, almost 30 million people worldwide, which is expected to reach 50 million peoples worldwide in 2050[1-4]. Patients with AF carry a higher risk of adverse cardiovascular events and reduced survival[5,6]. Incidence of AF increases with age. At the same time, aging population is likely to develop other chronic diseases and one of them is end-stage liver disease or cirrhosis[7-9]. This treatment of cirrhosis comprises of multidisciplinary approach ranging from very simple, symptomatic treatment with diuretic or treatment of primary cause, down the road to the most advanced treatment; liver transplantation[10-13].
Liver transplantation is the treatment of choice for end-stage liver diseases[10,13]. In 2017, around 8000 patients all over the United State suffered from end-stage liver disease receiving liver transplantation and the number trends to increase 3% to 5% annually in the past 20 years along with the excellent outcomes with almost 95% survival rate at 1-year post-procedure and some patients could live even more than 30 years after liver transplantation[14-17]. Recent advances in basic and clinical sciences, including surgical technique, immunosuppressive therapy and postoperative supportive care, have led to the substantial improvement in quality of life and survival after liver transplantation[18,19]. In addition, higher risk patients tend to receive transplantation in a higher proportion than they did before. In the view of higher risk patients, they tend to carry the risk factors that accompany with older age such as cardiovascular diseases.
In transplant centers, AF and liver transplantation are entities that we commonly encounter in the practice[20-23]. However, the occurrence rates of preexisting AF and AF following liver transplantation as well as clinical outcomes of liver transplant patients with AF remain unclear[20-31]. Thus, we conduct this meta-analysis: (1) to assess prevalence of pre-existing AF and/or incidence of AF following liver transplantation, and the trends of patient’s outcomes overtime; and (2) to evaluate impact of pre-existing AF and post-operative AF on patient outcomes following liver transplantation.
We registered this systematic review protocol with International Prospective Register of Systematic Reviews, No. CRD42018093644 (PROSPERO). We conducted a systematic literature search of EMBASE (between January 1988 and March 2018), Ovid MEDLINE (between January 1946 and March 2018), and the Cochrane Database of Systematic Reviews (from database inception to March 2018): (1) to estimate prevalence of pre-existing AF and/or incidence of AF following liver transplantation; and (2) to evaluate impact of pre-existing AF and post-operative AF on patient outcomes following liver transplantation. Ronpichai Chokesuwattanaskul and Charat Thongprayoon, two investigators, independently performed the systematic literature review using the search strategy that consolidated the terms of “liver” OR “hepatic” AND “transplant” OR “transplantation” AND “atrial fibrillation”, described in online supplementary data 1. No language restriction was implemented. We followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)[32] and the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement[33].
Our inclusion criteria comprised: (1) clinical trials or observational studies such as cohort, cross-sectional, or case-control studies; (2) available data on prevalence of pre-existing AF or incidence of AF following liver transplantation or outcomes of liver transplant recipients with AF; and (3) available data on prevalence, incidence, odds ratios (OR), hazard ratios, or relative risks. Retrieved articles were individually reviewed for eligibility by the two investigators as mentioned prior. Inclusion was not restricted by the size of study. Contrarieties were discussed and solved through joint agreement. We used Newcastle-Ottawa quality assessment scale to assess the quality of study for cohort and case-control studies[34], as shown in Table 1.
| Fouad et al[24] | VanWagner et al[25] | Nicalau-Raducu et al[26] | Josefsson et al[27] | |
| Country | Canada | United States | United States | Sweden |
| Study design | Retrospective Cohort | Case-Control | Retrospective Cohort | Retrospective Cohort |
| Yr | 2009 | 2012 | 2014 | 2014 |
| Total number | 197 | 242 | 389 | 186 |
| Mean age ± SD | 56 | 55 | 55 | 52 |
| Duration (yr) | 6 mo | 1 yr | 3.4 | 4 |
| Outcome definition | Cardiac complication after LTx | CV complication after LTx | Early (< 1 yr) and Late (> 1 yr) post LTx AF | Incident cardiac event post LTx |
| Outcome ascertainment | Review EKG in medical records | EKG, Echo, LHC, RHC, DSE as indicated | Review medical records | Review medical records |
| Incidence of pre-operative AF | NA | All 12/242 (5.0%) NASH 7/115 (6.1%) Alcohol 5/127 (3.9%) | NA | Atrial fibrillation/flutter 4/186 (2.2%) |
| Incidence of post-operative AF | Intraoperative 1/197 (0.5%) Early postoperative (0-30 d) 3/197 (1.5%) Late postoperative (1-6 mo) 2/197 (1.0%) | All 21/242 (8.7%) NASH 11/115 (9.6%) Alcohol 10/127 (7.9%) | All 12/389 (3.1%) Early (< 1 yr after transplant) 10/389 (2.6%) Late (> 1 yr after transplant) 2/389 (0.5%) | Arrhythmia (mainly AF or flutter) All 36/186 (19.4%) Peri-transplant 24/186 (12.9%) Late 12/186 (6.5%) |
| Outcomes | NA (study aim to identify predictor of cardiac complication 6 mo after LTX) | NA (study aim to compare CV event between liver disease before liver transplant) | NA (study demonstrated target DSE prior liver transplant associated with increased risk of AF) | NA (study aim to assess pretransplant EKG as a predictor of post liver transplant event) |
| Confounder adjustment | NA | NA | NA | NA |
| Newcastle-Ottawa scale | S3 C0 O3 | S4 C2 O3 | S3 C3 O3 | S4 C2 O3 |
| Vannucci et al[20] | Bargehr et al[21] | Xia et al[22] | Piazza et al[23] | |
| Country | United States | United States | United States | Italy |
| Study design | Retrospective Cohort | Case-Control study | Retrospective Cohort | Retrospective Cohort |
| Yr | 2014 | 2015 | 2015 | 2016 |
| Total number | 757 | 717 | 1387 | 143 |
| Mean age ± SD | 57.9 ± 6.8 | 58 | 54 | 55 |
| Duration (yr) | 1 yr | NA | 30 d | 3 |
| Outcome definition | 30 d and 1-yr survival after Liver Tx. | Cardiac complication after LTX | POAF (postoperative AF in LTX) | Incident AF (also other CVE) in NASH and alcoholic s/p LTx |
| Outcome ascertainment | Medical records | Review Medical records | EKG, Holter and medical records | Review medical records |
| Incidence of pre-operative AF | 19/757 (2.5%) | 32/717 (4.5%) | 77/1387 (5.6%) | Alcoholic cirrhosis 2/65 (3.1%) NASH cirrhosis 3/78 (3.8%) |
| Incidence of post-operative AF | NA | 1/63 (1.6%) | New onset AF within 30 d after LT 102/1387 (7.4%) | 2/143 (1.4%) |
| Outcomes | 1-mo mortality 5.29 (1.73-16.18) 1-yr mortality 3.28 (1.63-6.59) | Intraoperative cardiac complications 7.83 (1.94-31.49) Mortality 1.50 (0.61-3.69) | Median Hospital stays 31 d (16-67) in POAF vs 20 d (12-37) AKI 2.5 (1.06-5.70) Mortality 2.36 (1.45-3.85) Graft failure 2.28 (1.44-3.59) | NA (study aim to compare outcome as CV event after liver transplant between patients with NASH and those with alcoholic cirrhosis who receive liver transplant) |
| Confounder adjustment | NA | Age, MELD, donor risk index, DM | Age, MELD, intraoperative blood transfusion | NA |
| Newcastle-Ottawa scale | S3 C0 O3 | S4 C2 E3 | S4 C2 O3 | S4 C2 O3 |
| VanWagner et al[28] | VanWagner et al[31] | VanWagner et al[29] | Wange et al[30] | |
| Country | United States | United States | United States | Sweden |
| Study design | Retrospective Cohort | Case Control | Retrospective Cohort | Retrospective Cohort |
| Yr | 2016 | 2017 | 2018 | 2018 |
| Total number | 32810 | 1024 | 671 | 63 |
| Mean age ± SD | 55 ± 10 | 56 | Various by renal disease classification group | 45 |
| Duration (yr) | 90 d | 1 yr | NA | 10 |
| Outcome definition | MACE after Liver transplantation | CVD complication vs No CVD complication group | 1-yr CV complication | Incident AF post LTx who survive > 3 yr (LTx ATTRm amyloidosis) |
| Outcome ascertainment | Medical record in patient admitted by MACE | EKG, Holter and medical records | Medical record | Echo and Holter every visit |
| Incidence of pre-operative AF | 1969/32810 (6.0%) | 62/1024 (6.1%) | 2145/37322 (5.7%) | 1/63 (1.6%) |
| Incidence of post-operative AF | 204/32810 (0.6%) | 130/1024 (12.7%) | 65/671 (9.7%) | Incident AF 20/63 (31.7%) All AF post-op 21/63 (33.3%) (Median diagnosis 2 yr) |
| Outcomes | Pre-transplant AF and 30-d MACE (MI, HF, AF, cardiac arrest, PE, stroke) 6.9 (5.0-9.6) Pre-transplant AF and 90-d MACE 6.1 (4.5-8.3) | Pre-transplant AF and CVD complication 8.96 (3.70-22.0) | NA (study aim to assess degree of renal disease to 1-yr CV outcome in liver transplant patient) | Cerebrovascular events (TIA, ischemic stroke, intracerebral hemorrhage, subarachnoid hemorrhage) 3.8 (1.1-9.5) |
| Confounder adjustment | Sex, age, history of stroke, type of cirrhosis, and pre- transplant creatinine | Age, sex, race, working status, education, respiratory failure on ventilator at transplant, pulmonary hypertension, HCC, hypertension, DM, heart failure | NA | Cardiomyopathy, ischemic heart disease |
| Newcastle-Ottawa scale | S3 C0 O3 | S4 C2 E3 | S4 C2 O3 | S3 C0 O3 |
We used a structured information collecting form to collect the data from individual article including last name of the first investigator, title, year of publication, country that the research was carried out, baseline characteristics of liver transplant patients, processes utilized to diagnose AF, prevalence of pre-existing AF, incidence of post-operative AF, patient outcomes following liver transplantation.
We used Comprehensive Meta-Analysis Version 3.3.070 software (Biostat Inc., Englewood, NJ, United States) for all analyses. Estimated prevalence, incidence and estimated risks from each study were incorporated by the random-effect, generic inverse-variance approach of DerSimonian and Laird[35]. Given the possibility of between-study variance, we used a random-effect model rather than a fixed-effect model. Cochran’s Q test and I2 statistic were implemented to assess heterogeneity caused by between-study differences. I2 values of 0%-25% indicate insignificant heterogeneity. I2 values of 26%-50% indicate low heterogeneity. I2 values of 51%-75% indicate moderate heterogeneity and I2 value of 76%-100% indicate high heterogeneity[36]. Egger test was used to evaluate publication bias[37].
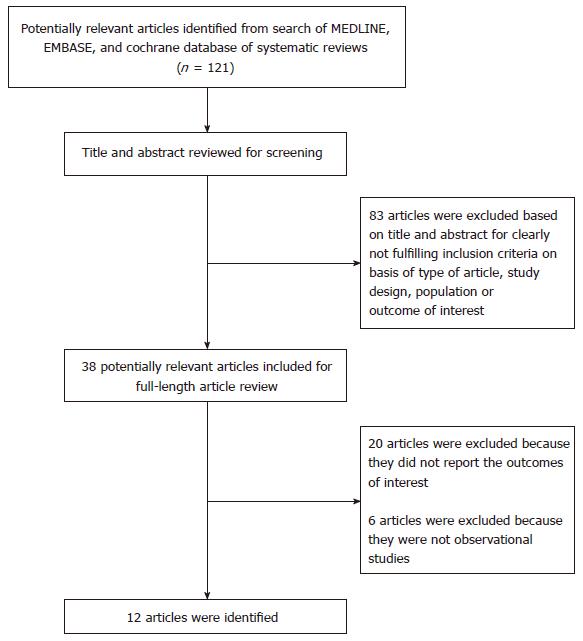
Applying our search strategy, 121 potential studies were selected. Following the elimination of 83 studies (title and abstract clearly not meeting inclusion criteria due to study design, type of study, patient population or reported outcomes), 38 studies were included for complete examination. After the complete review, twenty articles were omitted because the outcome of interest was not provided and six articles were excluded since they were descriptive studies without data of interest. Hence, we included 12 articles[20-31] into the final analysis including 9 cohort studies[20,22-24,26-30] and 3 case-control studies[21,25,31] with 38586 liver transplant recipients were enrolled, as demonstrated in Figure 1. Study characteristics and quality appraisal of studies are shown in Table 1[20-31].
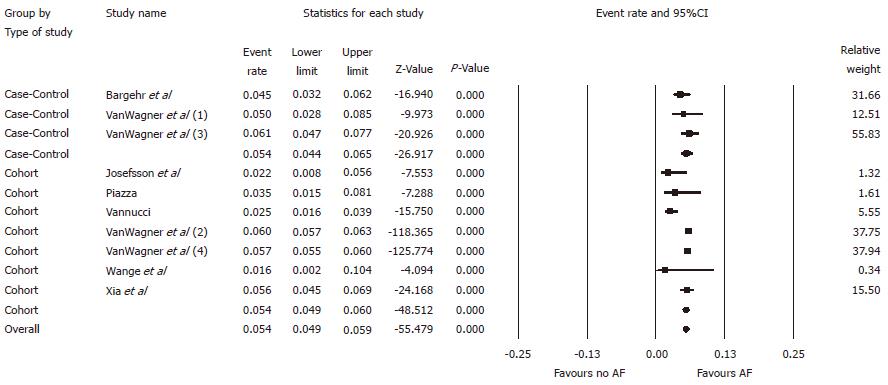
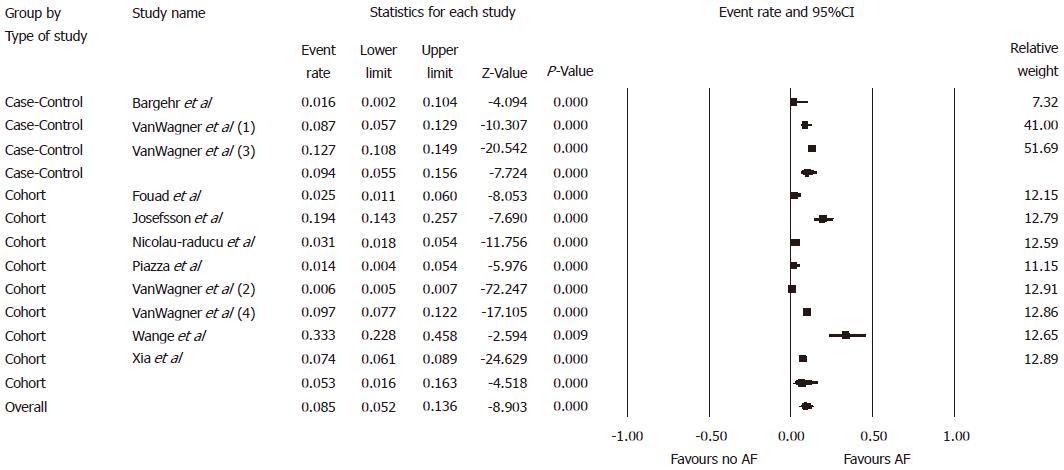
Overall, the pooled estimated prevalence of pre-existing AF in patients undergoing liver transplantation was 5.4% [95% confidence intervals (CI): 4.9%-5.9%, I2 = 66%, Figure 2]. The pooled estimated prevalence of pre-existing AF in patients undergoing liver transplantation was 5.4% (95%CI: 4.4%-6.5%, I2 = 8%) in case-control studies and 5.4% (95%CI: 4.9%-6.0%, I2 = 75) in cohort studies, respectively, when analysis was conducted based on type of study. The pooled estimated incidence of AF following liver transplantation was 8.5% (95%CI: 5.2%-13.6%, I2 = 99%, Figure 3). When analysis was performed based on type of study, the pooled estimated incidence of AF following liver transplantation was 9.4% (95%CI: 5.5%-15.6%, I2= 73%) in case-control studies and 5.3% (95%CI: 1.6%-16.3%, I2= 99%) in cohort studies, respectively.
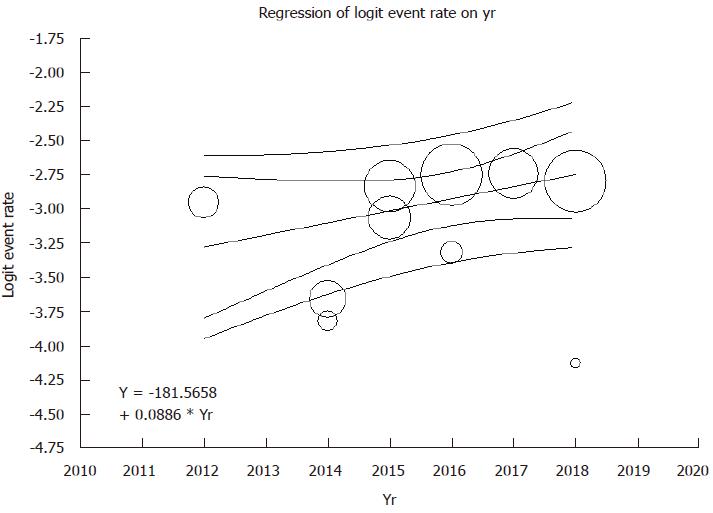
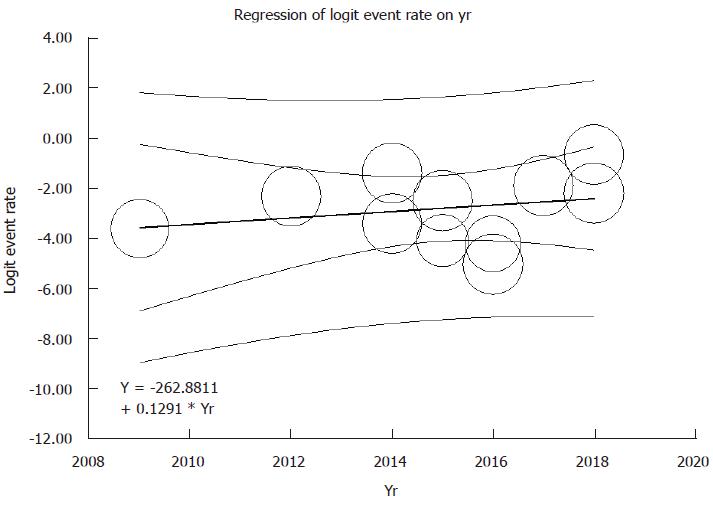
Meta-regression analyses were performed and showed no significant correlations between year of study and either prevalence of pre-existing AF (P = 0.08) or post-operative AF after liver transplantation (P = 0.54), as shown in Figures 4 and 5.
Data on the association between pre-existing AF and the risk of mortality were limited in two studies[20,21]. The pooled OR of mortality among liver transplant recipients was 2.34 (95%CI: 1.10-5.00, I2 = 45%). In addition, pre-existing AF is associated with postoperative cardiovascular complications among liver transplant recipients (3 studies[21,28,31]; OR: 5.15, 95%CI: 2.67-9.92, I2 = 64%). New onset AF is associated with poor outcomes after liver transplantation[22,30]. Wange et al[30] demonstrated a significant association between incident AF and cerebrovascular events in liver transplant patients with OR of 3.80 (95%CI: 1.10-9.50). In addition to increased mortality risk, Xia et al[22] demonstrated significant associations of new-onset AF with post-transplant acute kidney injury (OR: 2.50, 95%CI: 1.06-5.70), and increased risk of graft failure (OR: 2.28, 95%CI: 1.44-3.59) among liver transplant recipients.
Funnel plots, as demonstrated in Supplementary Figures 1 and 2, and Egger tests were conducted to assess for possibility of publication bias in analyses evaluating prevalence of pre-existing AF and incidence of postoperative AF in liver transplant patients, respectively. The graph is somewhat asymmetric and implies the possibility of publication bias towards negative studies in analysis of prevalence of pre-existing AF (P = 0.01). However, we found no significant publication bias in analysis evaluating incidence of postoperative AF in liver transplant patients, P = 0.32.
In this meta-analysis, we demonstrated that end stage liver disease patients who received liver transplantation had a prevalence of AF of 5.6%, which was higher than prevalence of AF in general patient population of 2.5%[38]. This number of higher prevalence may imply that patients who received liver transplantation appeared to carry the higher risk profiles. In addition, our study showed the pooled incidence of post-liver transplant AF of 8.5%, which is lower incidence, when compared to those patients who underwent heart transplantation (incidence of AF up to 40%)[39-44] or other open-heart surgeries (incidence of AF up to 50%)[5,45,46]. This mitigated number of incidence of postoperative AF in liver transplantation could be explained by the use of intensive postoperative hemodynamic care and, immunosuppressive therapy, the surgical technique, and not physically direct impact to the heart[28-31].
In general population, AF can put the patients at higher mortality risk, compared to those without AF[47]. In addition to mortality risk, our study also revealed the association of pre-existing AF and incident AF with poor clinical outcomes following liver transplantation. New-onset AF following liver transplantation is also associated with post-transplant acute kidney injury, cerebrovascular events, and increased risk of graft failure among liver transplant recipients. There are several mechanisms that put the liver transplant patients with AF at higher risk of postoperative morbidity and mortality compared to those without AF[24,48]. Patients with AF reflect that they are frail and have already been at higher risk profiles accompanying with other cardiovascular risks (left ventricular hypertrophy, heart failure, stroke, etc.) at the time even before liver transplantation, so that they will inevitably develop higher complication rates at postoperative period[21,49,50]. Furthermore, AF itself plays a critical role as marker of underlying heart diseases that make patients vulnerable to perioperative hemodynamic challenges[51,52].
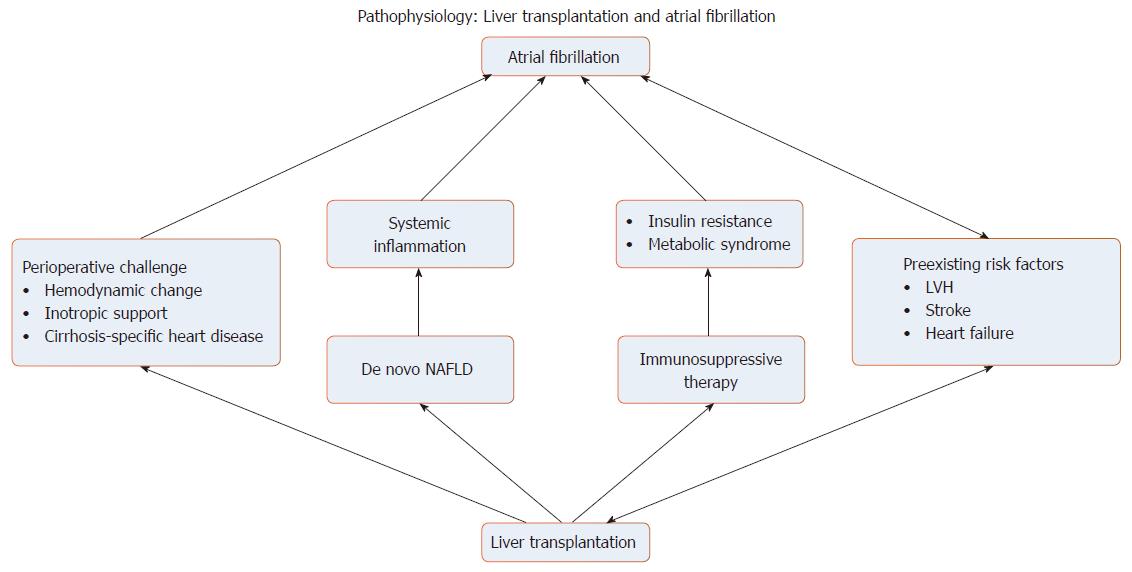
There are also several mechanisms explained why liver transplantation promotes the occurrence of AF during postoperative period (Figure 6). Firstly, conventional postoperative hemodynamic challenge could provoke AF through hemodynamic instability or inotropic administration[50]. Also, some preexisting liver diseases, such as nonalcoholic fatty liver disease (NAFLD), share a common risk factor, that is diabetes and obesity, with the AF patients[53]. In addition, NAFLD could also occur as de novo after liver transplantation and subsequently enhances the postoperative complications, contributed by systematic inflammatory mechanism[54-56]. Furthermore, immunosuppressive therapy increases the risk to develop insulin resistance which eventually leads to metabolic syndrome[57]. Various kind of cirrhosis-specific heart diseases, such as a well-known entity called congestive hepatopathy, prior to transplantation play a substantial arrhythmogenesis role as a substrate for pathogenesis of AF[50,58]. Various underlying medical problems including AF would, in the future, be used to identify high-risk patient population that needs to be optimized the treatment to achieve higher outcome after liver transplantation.
Leading cause of long term mortality in patients with liver transplantation is cardiovascular complications which, other than AF, include heart failure and myocardial infarction. These complications are predominantly driven by the development of metabolic syndrome after liver transplantation. However, this topic of interest is beyond the scope of our study and could be explained elsewhere[50]. More or less, these cardiovascular complications were also considered as potential risk modification strategy that should not be overlooked. Our study has noteworthy limitations. Firstly, an inconsistent in definition, for an example how to define the timing of AF as an early or late onset, among the different studies preclude to draw the generalized conclusion. Such this limitation, data use needs tailoring to the individual patient. Secondly, duration of follow up during the postoperative period by some study prospectively monitored a cardiovascular event for just 30 d post-transplantation, which this time frame does not long enough to reveal the long-term morbidity and mortality outcome. However, with the potential of higher morbidity and mortality in liver transplant patients with AF by our meta-analysis, future studies, preferable with population-based or national database studies, are required to discover whether focused AF cares for liver transplanted patients can improve patient outcomes after liver transplantation. Finally, since our study is a meta-analysis of observational studies, it could entirely prove association, but could not demonstrate a cause-effect (causal) relationship, between liver transplantation and AF.
In conclusion, our study demonstrated the actual prevalence of preexisting AF in patient underwent liver transplantation, incidence of AF post-liver transplantation. Our study also highlighted the association of AF with higher morbidity and mortality among liver transplant recipients. Further well-designed studies are needed to explore the impact of AF in liver transplant patients, which we strongly believe that AF management, specified to liver transplant patients, would be an important strategy to augment standard of care in this particular population.
Among liver transplant patients with atrial fibrillation (AF), there are lacks of data about incidence, prevalence and prognosis of AF in this specific group of patients. In spite of improvement of liver transplant care to the point of achieving almost 90% of 1-year survival rate, outcomes of liver transplantation related to AF remain unclear.
With excellent results of liver transplantation in term of survival, current indications of the transplantation have been extending into higher risk candidates due to higher amount of donors and more advanced treatment, which include preoperative preparation, surgical technique, immunosuppressive therapy and post-transplantation care. The high-risk liver transplant candidates tend to experience the adverse effects throughout perioperative period and worse outcomes, compared to those with less comorbidity. AF is one of the most common cardiac rhythm abnormalities and its prevalence increases with older age and higher comorbidities. Therefore, a number of patients with AF who received liver transplantation would definitely increase.
To examine outcomes of liver transplant recipients with AF, we performed this meta-analysis: (1) to assess prevalence of pre-existing AF and/or incidence of AF following liver transplantation, and the trends of patient's outcomes overtime; and (2) to evaluate impact of pre-existing AF and post-operative AF on patient outcomes following liver transplantation. Innovations and breakthroughs.
We conducted a systematic literature search of EMBASE, Ovid MEDLINE, and the Cochrane Database (from database inception to March 2018): (1) to estimate prevalence of pre-existing AF and/or incidence of AF following liver transplantation; and (2) to evaluate impact of pre-existing AF and post-operative AF on patient outcomes following liver transplantation. Estimated prevalence, incidence and estimated risks from each study were incorporated by the random-effect, generic inverse-variance approach of DerSimonian and Laird.
There were significant associations of AF with worse clinical outcomes following liver transplantation including 2.3-fold higher risk of death and 5.1-fold higher risk of postoperative cardiovascular complications, and poor clinical outcomes such as stroke, acute kidney injury and graft failure. We also showed the incidence of postoperative AF, namely 8.5%, consistently across different type of studies without the change overtime by meta-regression.
The overall estimated prevalence of pre-existing AF and incidence of AF following liver transplantation are 5.4% and 8.5%, respectively. Incidence of AF following liver transplant does not seem to decrease overtime. Pre-existing AF and new-onset AF are potentially associated with poor clinical outcomes post liver transplantation.
This systematic review confirmed higher risks of death and postoperative complications in liver transplant patients with AF. Our findings indicate that AF may be an independent predictor for worse clinical outcomes following liver transplantation.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Cerwenka H, Chiu KW, Gencdal G, Kanda T S- Editor: Ji FF L- Editor: A E- Editor: Song H
| 1. | Lip GYH, Brechin CM, Lane DA. The global burden of atrial fibrillation and stroke: a systematic review of the epidemiology of atrial fibrillation in regions outside North America and Europe. Chest. 2012;142:1489-1498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 313] [Cited by in RCA: 297] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 2. | Schnabel RB, Yin X, Gona P, Larson MG, Beiser AS, McManus DD, Newton-Cheh C, Lubitz SA, Magnani JW, Ellinor PT. 50 year trends in atrial fibrillation prevalence, incidence, risk factors, and mortality in the Framingham Heart Study: a cohort study. Lancet. 2015;386:154-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 890] [Cited by in RCA: 1217] [Article Influence: 121.7] [Reference Citation Analysis (0)] |
| 3. | Zoni-Berisso M, Lercari F, Carazza T, Domenicucci S. Epidemiology of atrial fibrillation: European perspective. Clin Epidemiol. 2014;6:213-220. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 661] [Cited by in RCA: 806] [Article Influence: 73.3] [Reference Citation Analysis (0)] |
| 4. | Andrade J, Khairy P, Dobrev D, Nattel S. The clinical profile and pathophysiology of atrial fibrillation: relationships among clinical features, epidemiology, and mechanisms. Circ Res. 2014;114:1453-1468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 657] [Cited by in RCA: 887] [Article Influence: 80.6] [Reference Citation Analysis (0)] |
| 5. | January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, Conti JB, Ellinor PT, Ezekowitz MD, Field ME, Murray KT, Sacco RL, Stevenson WG, Tchou PJ, Tracy CM, Yancy CW; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014;64:e1-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2373] [Cited by in RCA: 2927] [Article Influence: 266.1] [Reference Citation Analysis (0)] |
| 6. | Odutayo A, Wong CX, Hsiao AJ, Hopewell S, Altman DG, Emdin CA. Atrial fibrillation and risks of cardiovascular disease, renal disease, and death: systematic review and meta-analysis. BMJ. 2016;354:i4482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 596] [Cited by in RCA: 549] [Article Influence: 61.0] [Reference Citation Analysis (0)] |
| 7. | Lee H, Choi EK, Rhee TM, Lee SR, Lim WH, Kang SH, Han KD, Cha MJ, Oh S. Cirrhosis is a risk factor for atrial fibrillation: A nationwide, population-based study. Liver Int. 2017;37:1660-1667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 55] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 8. | Mwalitsa JP, Maimone S, Filomia R, Alibrandi A, Saitta C, Caccamo G, Cacciola I, Spinella R, Oliva G, Lembo T. Atrial fibrillation in patients with cirrhosis. Liver Int. 2016;36:395-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Biviano AB, Nazif T, Dizon J, Garan H, Abrams M, Fleitman J, Hassan D, Kapadia S, Babaliaros V, Xu K. Atrial Fibrillation is Associated with Increased Pacemaker Implantation Rates in the Placement of AoRTic Transcatheter Valve (PARTNER) Trial. J Atr Fibrillation. 2017;10:1494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Foundation AL. Liver Transplantation. 2018; Available from: https://www.liverfoundation.org/for-patients/about-the-liver/the-progression-of-liver-disease/liver-transplant/#information-for-the-newly-diagnosed. |
| 11. | Martin P, DiMartini A, Feng S, Brown R Jr, Fallon M. Evaluation for liver transplantation in adults: 2013 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. Hepatology. 2014;59:1144-1165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 581] [Cited by in RCA: 698] [Article Influence: 63.5] [Reference Citation Analysis (1)] |
| 12. | Kling CE, Perkins JD, Carithers RL, Donovan DM, Sibulesky L. Recent trends in liver transplantation for alcoholic liver disease in the United States. World J Hepatol. 2017;9:1315-1321. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 13. | Dutkowski P, Linecker M, DeOliveira ML, Müllhaupt B, Clavien PA. Challenges to liver transplantation and strategies to improve outcomes. Gastroenterology. 2015;148:307-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 202] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 14. | Organ Procurement and Transplantation Network. National data on liver transplantation. 2018; Available from: https://optn.transplant.hrsa.gov/data/view-data-reports/national-data. |
| 15. | Reddy KR, Ellerbe C, Schilsky M, Stravitz RT, Fontana RJ, Durkalski V, Lee WM; Acute Liver Failure Study Group. Determinants of outcome among patients with acute liver failure listed for liver transplantation in the United States. Liver Transpl. 2016;22:505-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 83] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 16. | Young K, Liu B, Bhuket T, Younossi Z, Saab S, Ahmed A, Wong RJ. Long-term trends in chronic hepatitis B virus infection associated liver transplantation outcomes in the United States. J Viral Hepat. 2017;24:789-796. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 17. | Urrunaga NH, Rachakonda VP, Magder LS, Mindikoglu AL. Outcomes of living versus deceased donor liver transplantation for acute liver failure in the United States. Transplant Proc. 2014;46:219-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 18. | Wan P, Yu X, Xia Q. Operative outcomes of adult living donor liver transplantation and deceased donor liver transplantation: a systematic review and meta-analysis. Liver Transpl. 2014;20:425-436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 90] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 19. | Mathur AK, Talwalkar J. Quality measurement and improvement in liver transplantation. J Hepatol. 2018;68:1300-1310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 20. | Vannucci A, Rathor R, Vachharajani N, Chapman W, Kangrga I. Atrial fibrillation in patients undergoing liver transplantation-a single-center experience. Transplant Proc. 2014;46:1432-1437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 26] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 21. | Bargehr J, Trejo-Gutierrez JF, Patel T, Rosser B, Aranda-Michel J, Yataco ML, Taner CB. Preexisting atrial fibrillation and cardiac complications after liver transplantation. Liver Transpl. 2015;21:314-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 42] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 22. | Xia VW, Worapot A, Huang S, Dhillon A, Gudzenko V, Backon A, Agopian VG, Aksoy O, Vorobiof G, Busuttil RW. Postoperative atrial fibrillation in liver transplantation. Am J Transplant. 2015;15:687-694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 45] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 23. | Piazza NA, Singal AK. Frequency of Cardiovascular Events and Effect on Survival in Liver Transplant Recipients for Cirrhosis Due to Alcoholic or Nonalcoholic Steatohepatitis. Exp Clin Transplant. 2016;14:79-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 24. | Fouad TR, Abdel-Razek WM, Burak KW, Bain VG, Lee SS. Prediction of cardiac complications after liver transplantation. Transplantation. 2009;87:763-770. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 101] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 25. | Vanwagner LB, Bhave M, Te HS, Feinglass J, Alvarez L, Rinella ME. Patients transplanted for nonalcoholic steatohepatitis are at increased risk for postoperative cardiovascular events. Hepatology. 2012;56:1741-1750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 176] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 26. | Nicolau-Raducu R, Gitman M, Ganier D, Loss GE, Cohen AJ, Patel H, Girgrah N, Sekar K, Nossaman B. Adverse cardiac events after orthotopic liver transplantation: a cross-sectional study in 389 consecutive patients. Liver Transpl. 2015;21:13-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 83] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 27. | Josefsson A, Fu M, Björnsson E, Kalaitzakis E. Prevalence of pre-transplant electrocardiographic abnormalities and post-transplant cardiac events in patients with liver cirrhosis. BMC Gastroenterol. 2014;14:65. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 28. | VanWagner LB, Serper M, Kang R, Levitsky J, Hohmann S, Abecassis M, Skaro A, Lloyd-Jones DM. Factors Associated With Major Adverse Cardiovascular Events After Liver Transplantation Among a National Sample. Am J Transplant. 2016;16:2684-2694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 142] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 29. | VanWagner LB, Montag S, Zhao L, Allen NB, Lloyd-Jones DM, Das A, Skaro AI, Hohmann S, Friedewald JJ, Levitsky J. Cardiovascular Disease Outcomes Related to Early Stage Renal Impairment Following Liver Transplantation. Transplantation. 2018;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 30. | Wange N, Anan I, Ericzon BG, Pennlert J, Pilebro B, Suhr OB, Wixner J. Atrial Fibrillation and Central Nervous Complications in Liver Transplanted Hereditary Transthyretin Amyloidosis Patients. Transplantation. 2018;102:e59-e66. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 31. | VanWagner LB, Ning H, Whitsett M, Levitsky J, Uttal S, Wilkins JT, Abecassis MM, Ladner DP, Skaro AI, Lloyd-Jones DM. A point-based prediction model for cardiovascular risk in orthotopic liver transplantation: The CAR-OLT score. Hepatology. 2017;66:1968-1979. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 93] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 32. | von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4:e296. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2924] [Cited by in RCA: 3444] [Article Influence: 191.3] [Reference Citation Analysis (0)] |
| 33. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52948] [Cited by in RCA: 47089] [Article Influence: 2943.1] [Reference Citation Analysis (0)] |
| 34. | Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8858] [Cited by in RCA: 12607] [Article Influence: 840.5] [Reference Citation Analysis (0)] |
| 35. | DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26739] [Cited by in RCA: 30378] [Article Influence: 778.9] [Reference Citation Analysis (0)] |
| 36. | Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39087] [Cited by in RCA: 46410] [Article Influence: 2109.5] [Reference Citation Analysis (3)] |
| 37. | Easterbrook PJ, Berlin JA, Gopalan R, Matthews DR. Publication bias in clinical research. Lancet. 1991;337:867-872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2020] [Cited by in RCA: 2003] [Article Influence: 58.9] [Reference Citation Analysis (0)] |
| 38. | Chugh SS, Havmoeller R, Narayanan K, Singh D, Rienstra M, Benjamin EJ, Gillum RF, Kim YH, McAnulty JH Jr, Zheng ZJ, Forouzanfar MH, Naghavi M, Mensah GA, Ezzati M, Murray CJ. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation. 2014;129:837-847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2658] [Cited by in RCA: 3333] [Article Influence: 277.8] [Reference Citation Analysis (0)] |
| 39. | Brandt M, Harringer W, Hirt SW, Walluscheck KP, Cremer J, Sievers HH, Haverich A. Influence of bicaval anastomoses on late occurrence of atrial arrhythmia after heart transplantation. Ann Thorac Surg. 1997;64:70-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 57] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 40. | Cohn WE, Gregoric ID, Radovancevic B, Wolf RK, Frazier OH. Atrial fibrillation after cardiac transplantation: experience in 498 consecutive cases. Ann Thorac Surg. 2008;85:56-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 33] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 41. | el Gamel A, Yonan NA, Grant S, Deiraniya AK, Rahman AN, Sarsam MA, Campbell CS. Orthotopic cardiac transplantation: a comparison of standard and bicaval Wythenshawe techniques. J Thorac Cardiovasc Surg. 1995;109:721-729; discussion 729-730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 79] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 42. | Dasari TW, Pavlovic-Surjancev B, Patel N, Williams AA, Ezidinma P, Rupani A, Sinacore JL, Heroux AL. Incidence, risk factors, and clinical outcomes of atrial fibrillation and atrial flutter after heart transplantation. Am J Cardiol. 2010;106:737-741. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 42] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 43. | Rivinius R, Helmschrott M, Ruhparwar A, Erbel C, Gleissner CA, Darche FF, Thomas D, Bruckner T, Katus HA, Doesch AO. The influence of surgical technique on early posttransplant atrial fibrillation - comparison of biatrial, bicaval, and total orthotopic heart transplantation. Ther Clin Risk Manag. 2017;13:287-297. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 44. | Sattiraju S, Vats S, Krishnan B, K Kim S, Austin E, Can I, Tholakanahalli V, G Benditt D, Y Chen L. Operative Technique and Atrial Tachyarrhythmias After Orthotopic Heart Transplantation. J Atr Fibrillation. 2012;5:690. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 45. | Auer J, Weber T, Berent R, Ng CK, Lamm G, Eber B. Risk factors of postoperative atrial fibrillation after cardiac surgery. J Card Surg. 2005;20:425-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 108] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 46. | Nisanoglu V, Erdil N, Aldemir M, Ozgur B, Berat Cihan H, Yologlu S, Battaloglu B. Atrial fibrillation after coronary artery bypass grafting in elderly patients: incidence and risk factor analysis. Thorac Cardiovasc Surg. 2007;55:32-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 47. | January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, Conti JB, Ellinor PT, Ezekowitz MD, Field ME, Murray KT, Sacco RL, Stevenson WG, Tchou PJ, Tracy CM, Yancy CW; ACC/AHA Task Force Members. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014;130:2071-2104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1393] [Cited by in RCA: 1591] [Article Influence: 144.6] [Reference Citation Analysis (0)] |
| 48. | Keeffe EB. Liver transplantation at the millennium. Past, present, and future. Clin Liver Dis. 2000;4:241-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 49. | Bargehr J, Trejo-Gutierrez JF, Rosser BG, Patel T, Yataco ML, Pungpapong S, Taner CB, Aranda-Michel J. Liver transplantation in patients with atrial fibrillation. Transplant Proc. 2013;45:2302-2306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 50. | Gallegos-Orozco JF, Charlton MR. Predictors of Cardiovascular Events After Liver Transplantation. Clin Liver Dis. 2017;21:367-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 51. | Benjamin EJ, Levy D, Vaziri SM, D’Agostino RB, Belanger AJ, Wolf PA. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA. 1994;271:840-844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 249] [Cited by in RCA: 216] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 52. | Stewart S, Hart CL, Hole DJ, McMurray JJ. A population-based study of the long-term risks associated with atrial fibrillation: 20-year follow-up of the Renfrew/Paisley study. Am J Med. 2002;113:359-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1057] [Cited by in RCA: 1137] [Article Influence: 49.4] [Reference Citation Analysis (0)] |
| 53. | Tanner RM, Baber U, Carson AP, Voeks J, Brown TM, Soliman EZ, Howard VJ, Muntner P. Association of the metabolic syndrome with atrial fibrillation among United States adults (from the REasons for Geographic and Racial Differences in Stroke [REGARDS] Study). Am J Cardiol. 2011;108:227-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 57] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 54. | Pagadala M, Dasarathy S, Eghtesad B, McCullough AJ. Posttransplant metabolic syndrome: an epidemic waiting to happen. Liver Transpl. 2009;15:1662-1670. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 111] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 55. | Laryea M, Watt KD, Molinari M, Walsh MJ, McAlister VC, Marotta PJ, Nashan B, Peltekian KM. Metabolic syndrome in liver transplant recipients: prevalence and association with major vascular events. Liver Transpl. 2007;13:1109-1114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 237] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 56. | Moon JI, Barbeito R, Faradji RN, Gaynor JJ, Tzakis AG. Negative impact of new-onset diabetes mellitus on patient and graft survival after liver transplantation: Long-term follow up. Transplantation. 2006;82:1625-1628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 139] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 57. | Pisano G, Fracanzani AL, Caccamo L, Donato MF, Fargion S. Cardiovascular risk after orthotopic liver transplantation, a review of the literature and preliminary results of a prospective study. World J Gastroenterol. 2016;22:8869-8882. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 22] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 58. | Møller S, Bernardi M. Interactions of the heart and the liver. Eur Heart J. 2013;34:2804-2811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 259] [Cited by in RCA: 319] [Article Influence: 26.6] [Reference Citation Analysis (0)] |