Copyright
©The Author(s) 2015.
World J Hepatol. Apr 28, 2015; 7(6): 874-884
Published online Apr 28, 2015. doi: 10.4254/wjh.v7.i6.874
Published online Apr 28, 2015. doi: 10.4254/wjh.v7.i6.874
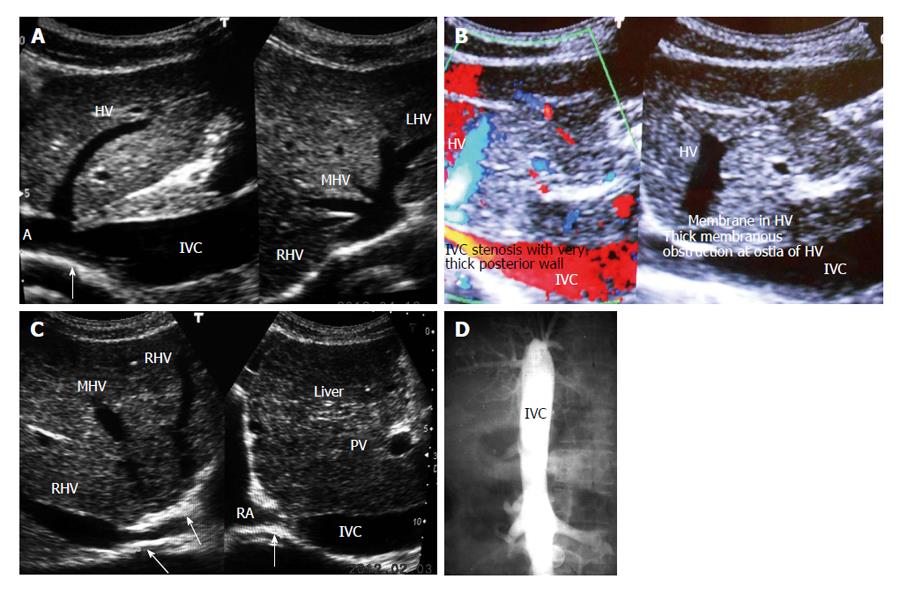
Figure 1 Inferior vena cava obstruction.
A: Ultrasonography showing stenosis of inferior vena cava (IVC) at cavo-atrial junction. Note patent orifices hepatic vein (HV)-right HV (RHV), middle HV (MHV) and left HV (LHV); B: Color Doppler ultrasonography of a patient with liver cirrhosis showing IVC stenosis, membranes in HV; C: Ultrasonography of a patient with liver cirrhosis showing complete obstruction of IVC at cavo-atrial junction and obstruction at orifices of MHV and LHV. Note dilated hepatic veins; D: Cavogram showing complete obstruction of the IVC. PV: Portal vein; RA: Right atrium.
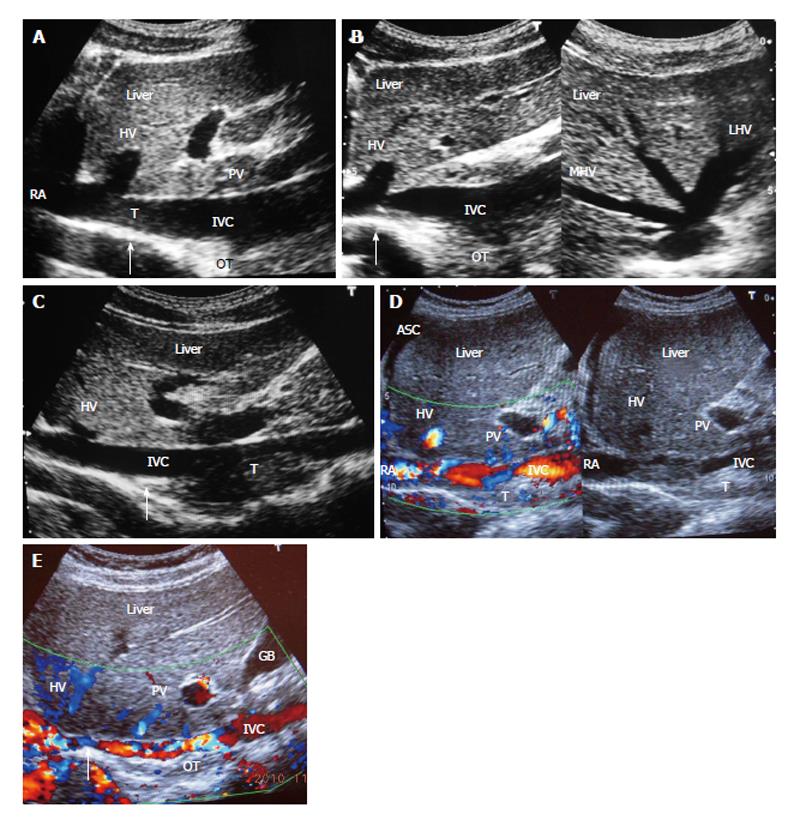
Figure 2 Ultrasonography showing thrombi of different ages in inferior vena cava due to recurrent acute exacerbations.
A: Ultrasonography showing mild stenosis of inferior vena cava (IVC) with thick echoic posterior wall at cavo-atrial junction. It shows recent thrombus (T) and old organized thrombus (OT) deposited during recurrent acute exacerbation (AE); B: Ultrasonography showing stenosis of IVC at cavo-atrial junction, with OT along posterior wall just distal to it. Middle hepatic vein (MHV) and left hepatic vein (LHV) hepatic veins are patent; C: Ultrasonography showing mild stenosis of IVC at cavo-atrial junction and thrombus of different ages along the posterior wall of the IVC; D: Ultrasonography showing features of HV outflow obstruction-hepatomegaly and ascites (ASC) in a patient with IVC stenosis near cavo-atrial junction and IVC filled with recent and old organized T; E: Ultrasonographic evidence of recurrent AE; Color Doppler ultrasonography showing layers of linear old OT along posterior wall of the hepatic portion of the IVC narrowing its lumen. Arrow indicates to the site of initial lesion in IVC. USG also shows segmental stenosis of HV. PV: Portal vein; HV: Hepatic vein; RA: Right atrium; GB: Gall bladder.
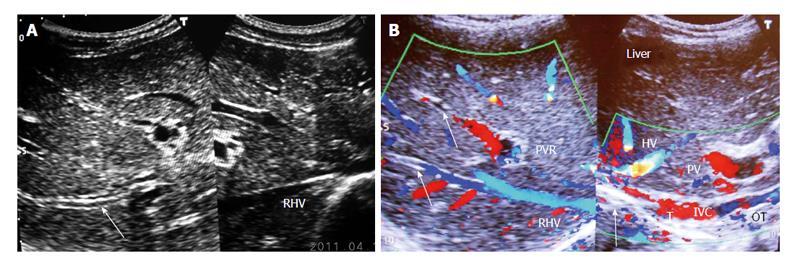
Figure 3 Ultrasonography showing thrombosed intra-hepatic veins.
A: Ultrasonography showing diffuse thrombosed and echoic walls of large and medium-sized intra-hepatic veins (one of which is indicated by an arrow) that occurred during acute exacerbation. Right hepatic vein (RHV) orifice is narrowed; B: Color Doppler Ultrasonography of patient with cirrhosis. It shows long segment stenosis of inferior vena cava (IVC) with recent thrombus (T) and old organized thrombi (OT) on thick posterior wall. Arrow shows thrombosed large and medium-sized intra-hepatic veins. HV: Hepatic vein; PV: Portal vein; PVR: Portal vein radical.
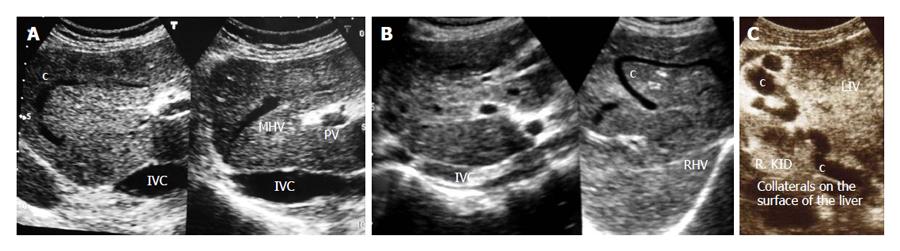
Figure 4 Ultrasonography showing collaterals.
A: Ultrasonography of a patient with liver cirrhosis due to complete inferior vena cava (IVC) obstruction at cavo-atrial junction showing obstruction of middle hepatic vein (MHV) and a intra-hepatic collateral (c); B: Ultrasonography of a young girl with liver cirrhosis: IVC is filled with old organized thrombi of different ages, right hepatic vein (RHV) is thrombosed and a large intra-hepatic collateral is seen; C: Ultrasonography showing dilated collaterals on the surface of liver (LIV) close to right kidney (R. KID) in a patient with liver cirrhosis. PV: Portal vein.
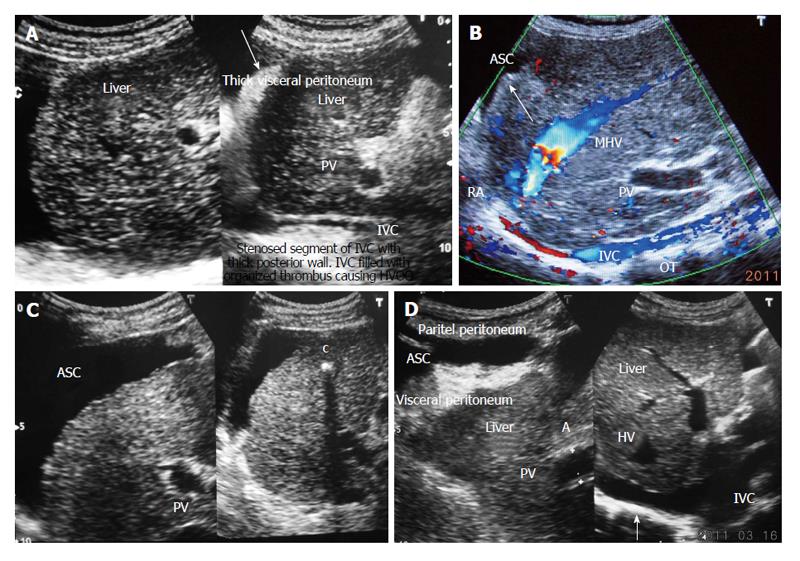
Figure 5 Ultrasonography showing ascites and evidence of chronic peritonitis in a patient with cirrhosis.
A: Acute exacerbation in a patient with liver cirrhosis showing hepatic portion of the inferior vena cava (IVC) filled with organizing thrombus and ascites with thick visceral peritoneum-indicating presence of bacterial peritonitis; B: Ultrasonography of a patient with liver cirrhosis due to HVCS: showing long segment stenosis of IVC with thick old organized thrombus (OT) along the posterior wall of the hepatic portion of the IVC. Note the presence of ascites (ASC) and irregular margin of the liver indicated by an arrow. Middle hepatic vein (MHV) is obstructed at its orifice and shows distal segmental stenosis; C: Ultrasonography of a patient with liver cirrhosis due to HVCS showing inferior vena cava stenosis, a calcified focus (c) in the liver and ascites; D: Ultrasonography of patient with liver cirrhosis due to HVCS showing IVC stenosis with organized thrombus on posterior wall and ASC and thick visceral peritoneum, suggestive of chronic bacterial peritonitis. PV: Portal vein; HVCS: Hepatic vena cava syndrome; RA: Right atrium; HV: Hepatic vein.
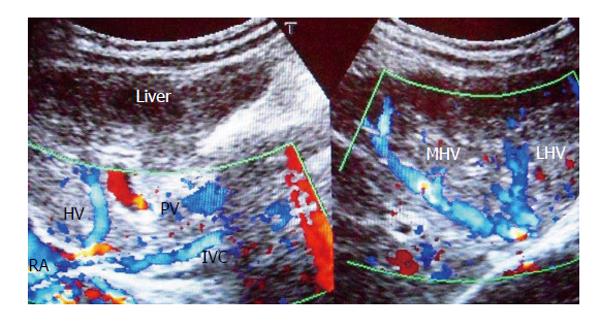
Figure 6 Liver cirrhosis in a young girl due to hepatic vena cava syndrome.
Note long segment obstruction of the inferior vena cava (IVC) at cavo-atrial junction and irregular narrowing of its hepatic portion. Middle hepatic vena (MHV) and left hepatic vena (LHV) are dilated with irregular caliber. PV: Portal vein; HV: Hepatic vein; RA: Right atrium.
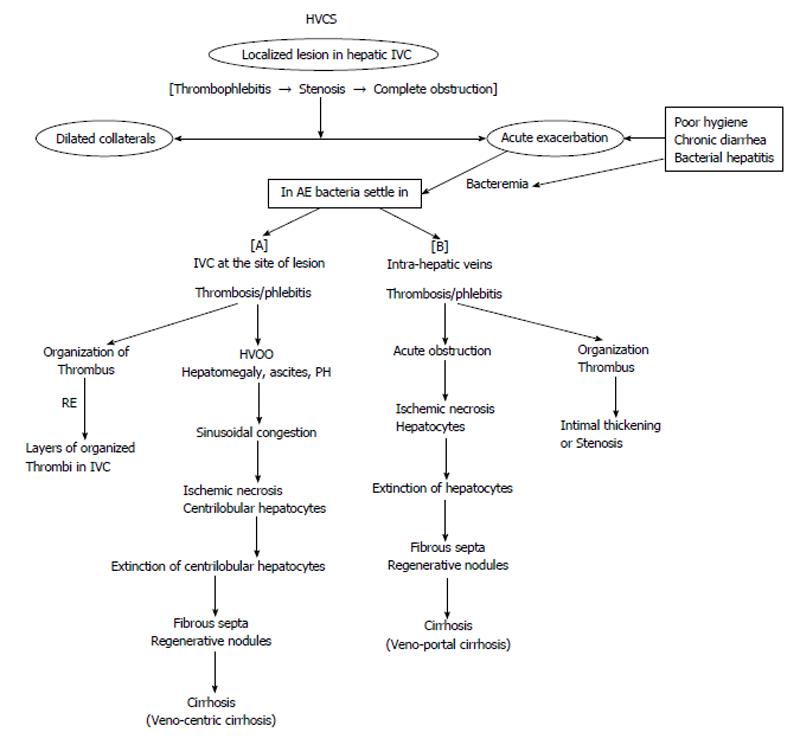
Figure 7 Mechanism of development of cirrhosis in hepatic vena cava syndrome.
IVC: Inferior vena cava; HVOO: Hepatic venous outflow obstruction; PH: Portal hypertension; AE: Acute exacerbation; RE: Recurrent AE; HVCS: Hepatic vena cava syndrome.
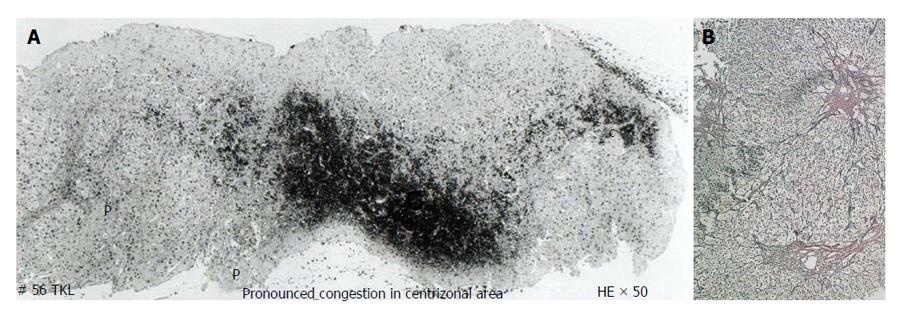
Figure 8 Histology showing fibrosis in centri-lobular areas.
A: Histology of liver of a patient with hepatic vena cava syndrome during acute exacerbation showing acute congestive changes around central vein (c) and sparing of liver around portal tract (P) due to hepatic venous outflow obstruction; B: Histology of liver of patient with hepatic vena cava syndrome a few months after development of hepatic venous outflow obstruction during acute exacerbation showing fibrosis around central vein. Histology of liver of a patient with hepatic vena cava syndrome showing the wall of a thrombosed medium sized intra-hepatic vein that occurred during acute exacerbation. HE: Hematoxylin eosin stain.
- Citation: Shrestha SM. Liver cirrhosis in hepatic vena cava syndrome (or membranous obstruction of inferior vena cava). World J Hepatol 2015; 7(6): 874-884
- URL: https://www.wjgnet.com/1948-5182/full/v7/i6/874.htm
- DOI: https://dx.doi.org/10.4254/wjh.v7.i6.874