Copyright
©The Author(s) 2015.
World J Hepatol. Feb 27, 2015; 7(2): 177-188
Published online Feb 27, 2015. doi: 10.4254/wjh.v7.i2.177
Published online Feb 27, 2015. doi: 10.4254/wjh.v7.i2.177
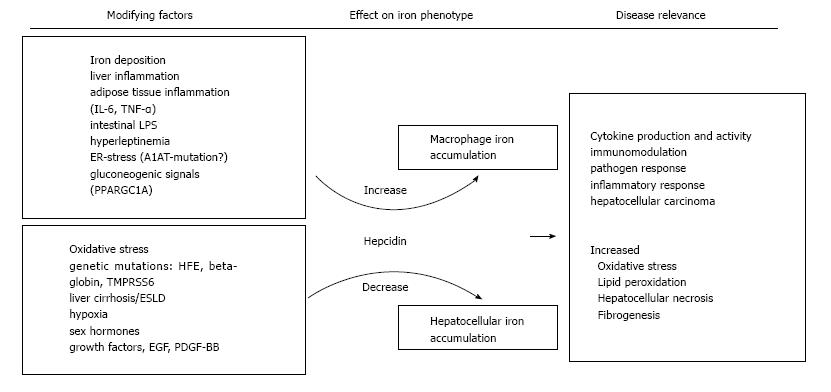
Figure 1 Summary of the potential stimuli that may affect iron homeostasis in non-alcoholic fatty liver disease.
Both, increasing and decreasing stimuli have been reported in non-alcoholic fatty liver disease and it appears likely that the net balance of these frequently counteracting forces finally determines the iron phenotype in the individual. Patterns of iron deposition may also be linked to distinct clinical consequences. IL-6: Interleukin 6; TNF-α: Tumor necrosis factor-α; LPS: Lipopolysaccharide; ER: Endoplasmatic reticulum; A1AT: α-1-antitrypsin; PPARGC1A: Peroxisome proliferator-activated receptor gamma coactivator 1-α; TMPRSS6: Transmembrane protease, serine 6; ESLD: End-stage liver disease; EGF: Epidermal growth factor; PDGF-BB: Platelet derived growth factor BB.
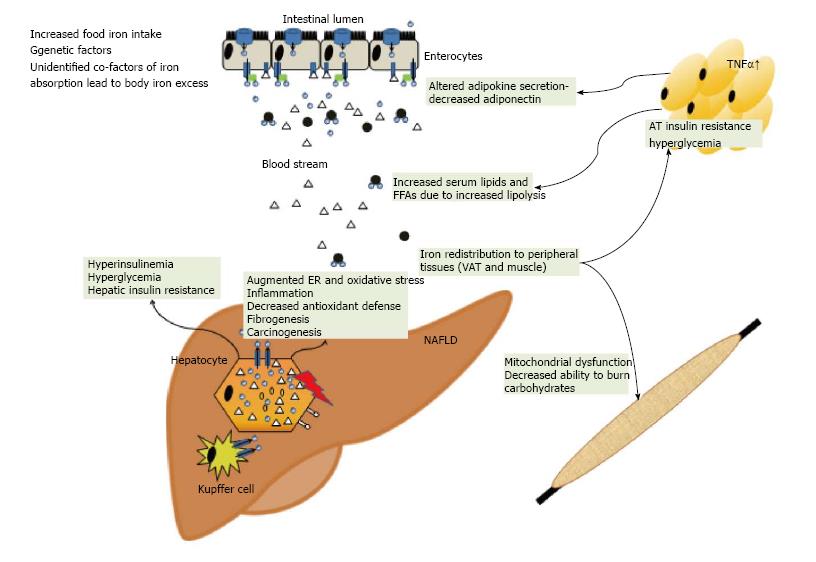
Figure 2 Summary of how iron excess and low copper availability may affect whole body glucose and lipid homeostasis.
Iron excess may promote insulin resistance in the liver, muscle and adipose tissue. Iron may increase ER and oxidative stress whereas low copper is potentially associated with an impaired antioxidant defence. These factors may result in the propagation of inflammation, fibrogenesis and hepatocarcinogenesis. TNF-α: Tumor necrosis factor-α; ER: Endoplasmatic reticulum; FFA: Free fatty acid; VAT: Visceral adipose tissue; AT: Adipose tissue.
- Citation: Aigner E, Weiss G, Datz C. Dysregulation of iron and copper homeostasis in nonalcoholic fatty liver. World J Hepatol 2015; 7(2): 177-188
- URL: https://www.wjgnet.com/1948-5182/full/v7/i2/177.htm
- DOI: https://dx.doi.org/10.4254/wjh.v7.i2.177