Copyright
©The Author(s) 2015.
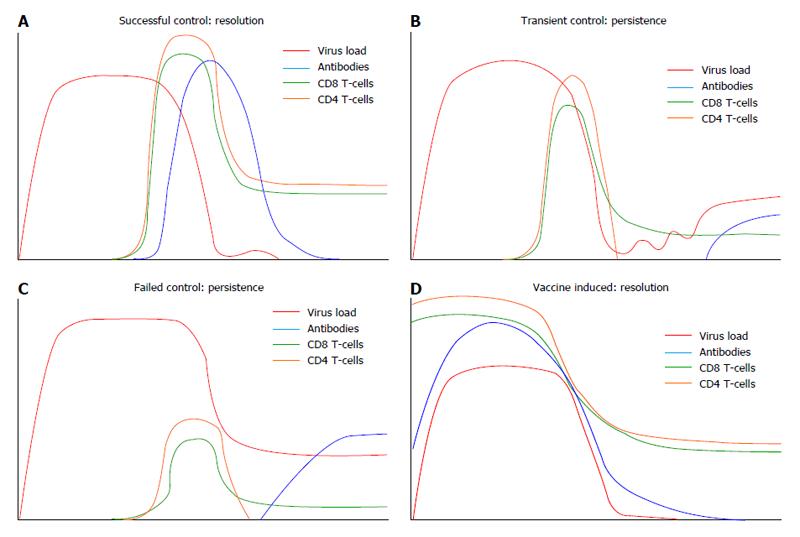
Figure 1 Schematic overview of the different causes of hepatitis C virus infection in relation to modulation of the adaptive immune response.
A: Viral clearance. Viral RNA (red line) is normally detected in blood within 1-2 wk after exposure. The virus load will increase until the emergence of HCV specific CD4 (yellow line) and CD8 T-cell (green line) responses 4 to 8 wk after infection[98]. Ideally, strain specific neutralizing antibodies (blue line) are present around the same time[88,89]. After viral elimination, antibody responses can either remain present or decrease to undetectable levels. Memory T-cells remain usually present and can be detected by in vitro assays; B: Transient control. After the initial peak viremia (red line), T-cell responses emerge and virus load decreases but remains detectable in serum. CD8 T-cells (green line) remain detectable but CD4 T-cell (yellow line) responses decrease to low levels. There appears to be a constant battle between virus and the immune system. De novo escape variants are able to evade the T and B-cell responses but at the same time lose viral fitness. When effective T and B-cell responses contract because the correct epitopes are no longer present, the virus “mutates back” to a more fit variant and virus load may increase again. Thinner lines of the adaptive immune responses represent decreased functionality of CD4 (yellow), CD8 T-cell (green) and antibodies (blue); C: Failed control leading to persistent infection; After the initial peak viremia, T-cell responses emerge and virus load decrease to lower levels but virus remains detectable in serum. T and B cells are functionally impaired or present in too low numbers to efficiently eliminate the virus. The virus remains present at steady state levels. Thinner lines of the adaptive immune responses represent decreased functionality of CD4 (yellow), CD8 T-cell (green) and antibodies (blue); D: Vaccine induced protection model. Vaccine-induced broadly neutralizing antibodies are present at the time of exposure and prevent virus production by infected hepatocytes. The hepatocytes that are infected are successfully eliminated by cytolytic T-cells in the liver.
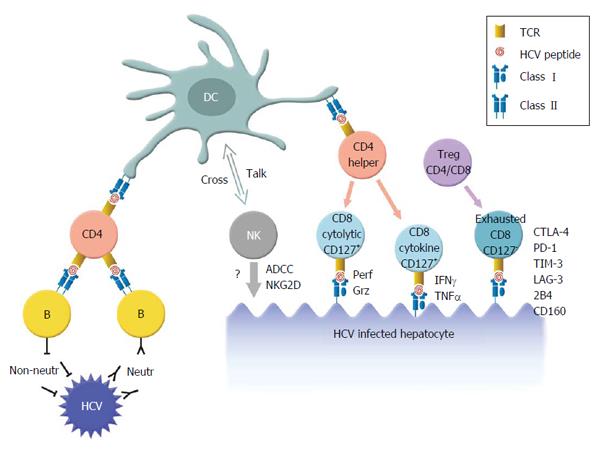
Figure 2 Summary of immune responses in hepatitis C virus immunized chimpanzees.
Antigen presenting cells (DCs or Kupffer cells in the liver) present HCV peptides in the context of major histocompatibility complex class II molecules to the T-cell receptor (TCR) on CD4 T-cells. CD4 cells may activate B-cells. Antibodies produced may be neutralizing and bind to circulating HCV particles and prevent the infection of hepatocytes. Or the antibodies may be non-neutralizing antibodies and potentially play a role in ADCC. CD4-helper T-cells can also stimulate cytolytic T-cells. CD8 T-cells may be directly responsible for lysis when they produce degranulation molecules like granzymes or perforin after the recognition of a peptide on the surface of an HCV infected hepatocyte. Or via indirect lysis, mediated by the secretion of cytokines. CD8 T-cells affected by Tregs and exhausted CD8 T-cells are functionally impaired and are incapable of lysing HCV infected hepatocytes. HCV: Hepatitis C virus; CTLA-4: Cytotoxic T-lymphocyte-associated protein 4; IFN: Interferon; TNFα: Tumor necrosis factor alpha; ADCC: Antibody dependent cellular cytotoxicity; DC: Dentritic cell; PD-1: Programmed cell death protein 1; TIM-3: T cell immunoglobulin and mucin protein 3; LAG-3: Lymphocyte-activation gene 3.
- Citation: Verstrepen BE, Boonstra A, Koopman G. Immune mechanisms of vaccine induced protection against chronic hepatitis C virus infection in chimpanzees. World J Hepatol 2015; 7(1): 53-69
- URL: https://www.wjgnet.com/1948-5182/full/v7/i1/53.htm
- DOI: https://dx.doi.org/10.4254/wjh.v7.i1.53