Copyright
©The Author(s) 2021.
World J Hepatol. Jun 27, 2021; 13(6): 650-661
Published online Jun 27, 2021. doi: 10.4254/wjh.v13.i6.650
Published online Jun 27, 2021. doi: 10.4254/wjh.v13.i6.650
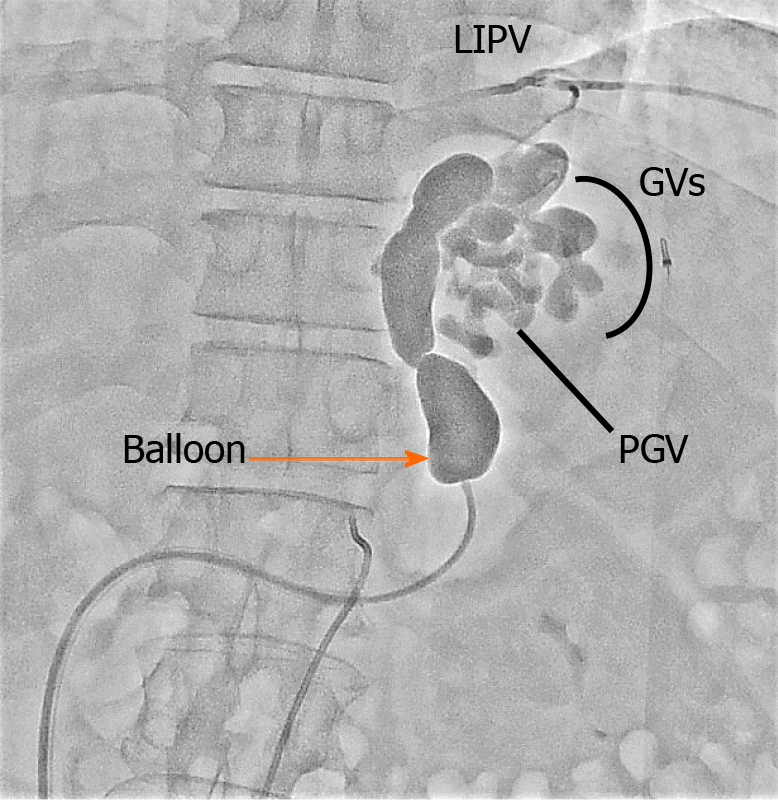
Figure 1 Balloon-occluded retrograde transvenous venography.
When the gastrorenal shunt is balloon-occluded (arrow) and retrogradely imaged, the posterior gastric vein, which is the inflow vessel, is visualized via the gastric varices. A part of the left inferior phrenic vein as an outflow vessel is also demonstrated. PGV: Posterior gastric vein; GV: Gastric varices; LIPV: Left inferior phrenic vein.
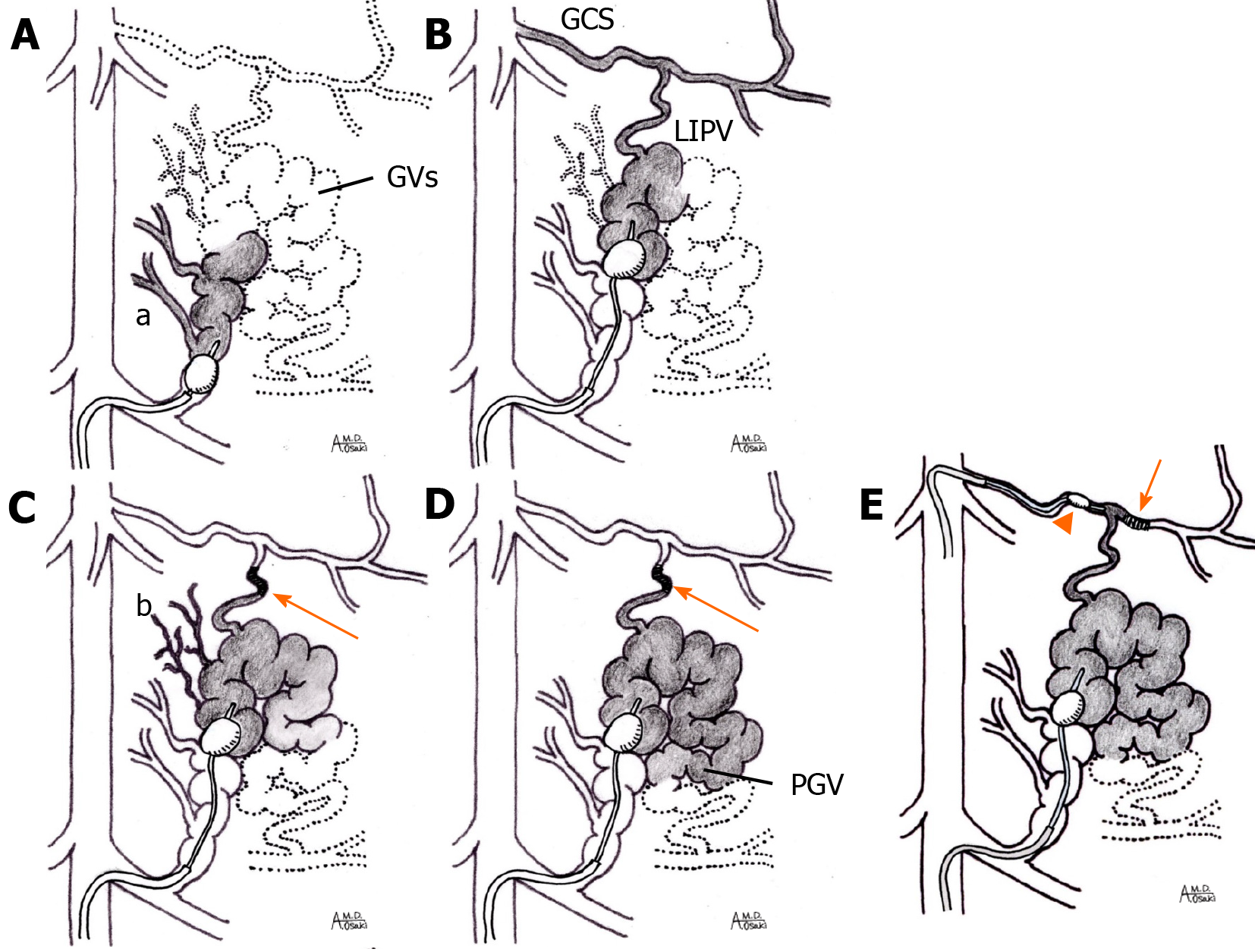
Figure 2 Illustration of the balloon-occluded retrograde transvenous obliteration procedure.
A: Balloon-occluded retrograde transvenous venography (BRTV). The initial BRTV does not visualize the main body of the gastric varices (GVs) because multiple draining vessels are present (a); B: When the balloon catheter is advanced beyond the small drainage vessels (downgrading method), the relatively large diameter left inferior phrenic vein (LIPV) becomes visualized as another drainage route to the gastrocaval shunt (GCS); C: GVs become visualized when selective coil embolization (arrow) of the LIPV is performed. As small amounts of sclerosant are injected sequentially over time, the smaller drainage vessels (b) are gradually embolized (stepwise injection method); D: After stepwise injection, BRTV demonstrated the GVs in their entirety as well as the inflowing posterior gastric vein; E: If selective coil embolization of the LIPV is impossible, the GCS should be occluded with another balloon catheter for balloon-occluded retrograde transvenous obliteration (BRTO) (dual-BRTO). Selective coil embolization of the LIPV branch (arrow) is performed through the catheter via the GCS. PGV: Posterior gastric vein; GVs: Gastric varices; LIPV: Left inferior phrenic vein; GCS: Gastrocaval shunt.
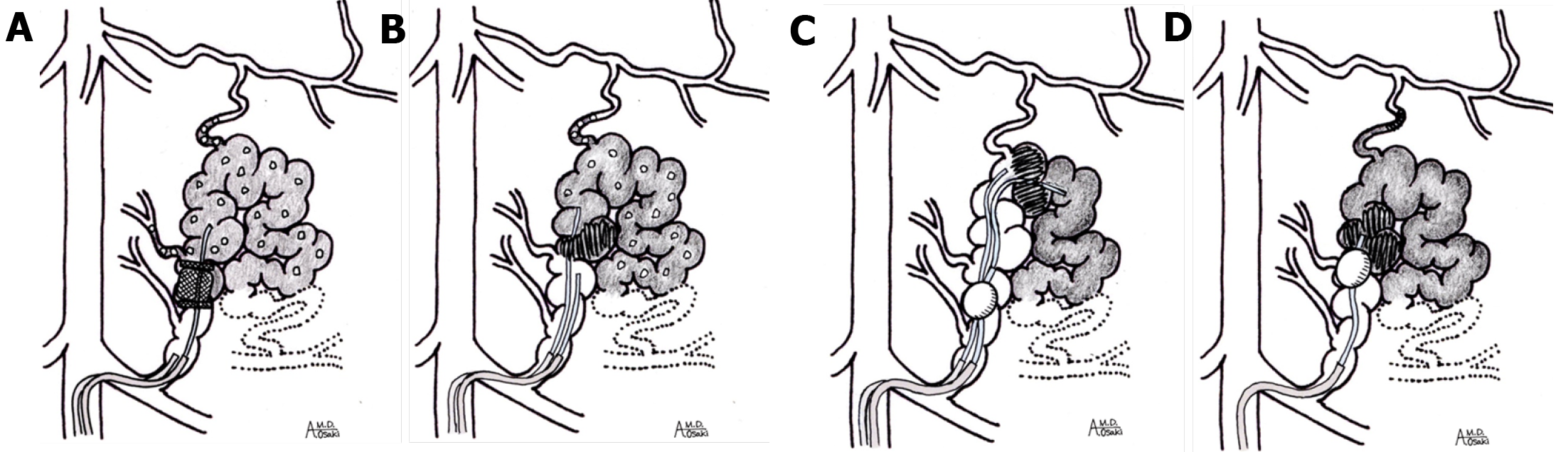
Figure 3 Schema of balloon-occluded retrograde transvenous obliteration modified variants.
A: In plug-assisted retrograde transvenous obliteration, a vascular plug is placed instead of a balloon catheter to block shunt blood flow. In the original method, gelatin sponge suspension is injected instead of sclerosant; B: In coil-assisted retrograde transvenous obliteration (CARTO), shunt blood flow is blocked using microcoils and gelatin sponge suspension is injected to embolize the gastric varices; C: In modified CARTO, instead of downgrading by advancing the balloon catheter, embolization is performed using microcoils and sclerosant is injected upstream into the gastric varices; D: In CARTO-II, sclerosant is injected from a balloon catheter in the same manner as conventional balloon-occluded retrograde transvenous obliteration, coil embolization is performed just above the balloon, and the balloon catheter is finally removed.
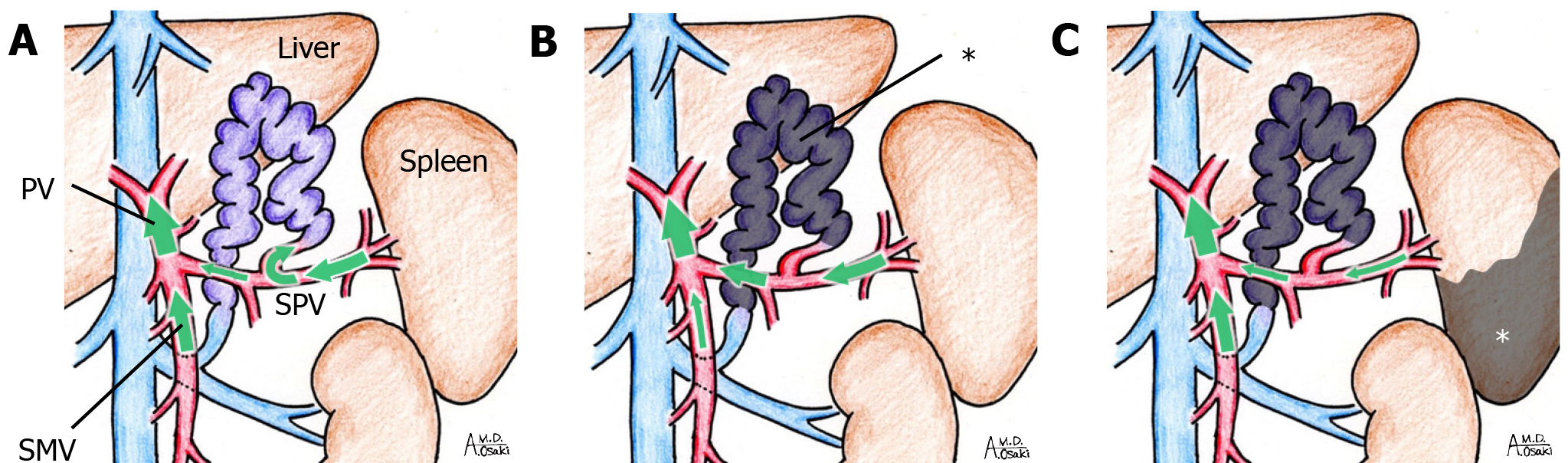
Figure 4 Schema of changes in portal hemodynamics due to combined balloon-occluded retrograde transvenous obliteration and partial splenic embolization.
A: Before treatment, most of the splenic blood flow is short-circuited to the systemic circulation via the gastrorenal shunt (GRS); B: The GRS is embolized by balloon-occluded retrograde transvenous obliteration (BRTO) (black asterisk). The increase in portal venous flow after BRTO is mainly caused by increased splenic venous blood flow without a substantial increase in hepatopetal mesenteric venous blood flow; C: The lower half of the spleen is infarcted by partial splenic embolization (PSE) (white asterisk). Hepatopetal mesenteric venous blood flow increases after splenic venous blood flow is decreased by PSE. PV: portal vein, SPV: splenic vein, SMV: superior mesenteric vein.
- Citation: Waguri N, Osaki A, Watanabe Y. Balloon-occluded retrograde transvenous obliteration for treatment of gastric varices. World J Hepatol 2021; 13(6): 650-661
- URL: https://www.wjgnet.com/1948-5182/full/v13/i6/650.htm
- DOI: https://dx.doi.org/10.4254/wjh.v13.i6.650