Copyright
©The Author(s) 2021.
World J Hepatol. Jan 27, 2021; 13(1): 151-161
Published online Jan 27, 2021. doi: 10.4254/wjh.v13.i1.151
Published online Jan 27, 2021. doi: 10.4254/wjh.v13.i1.151
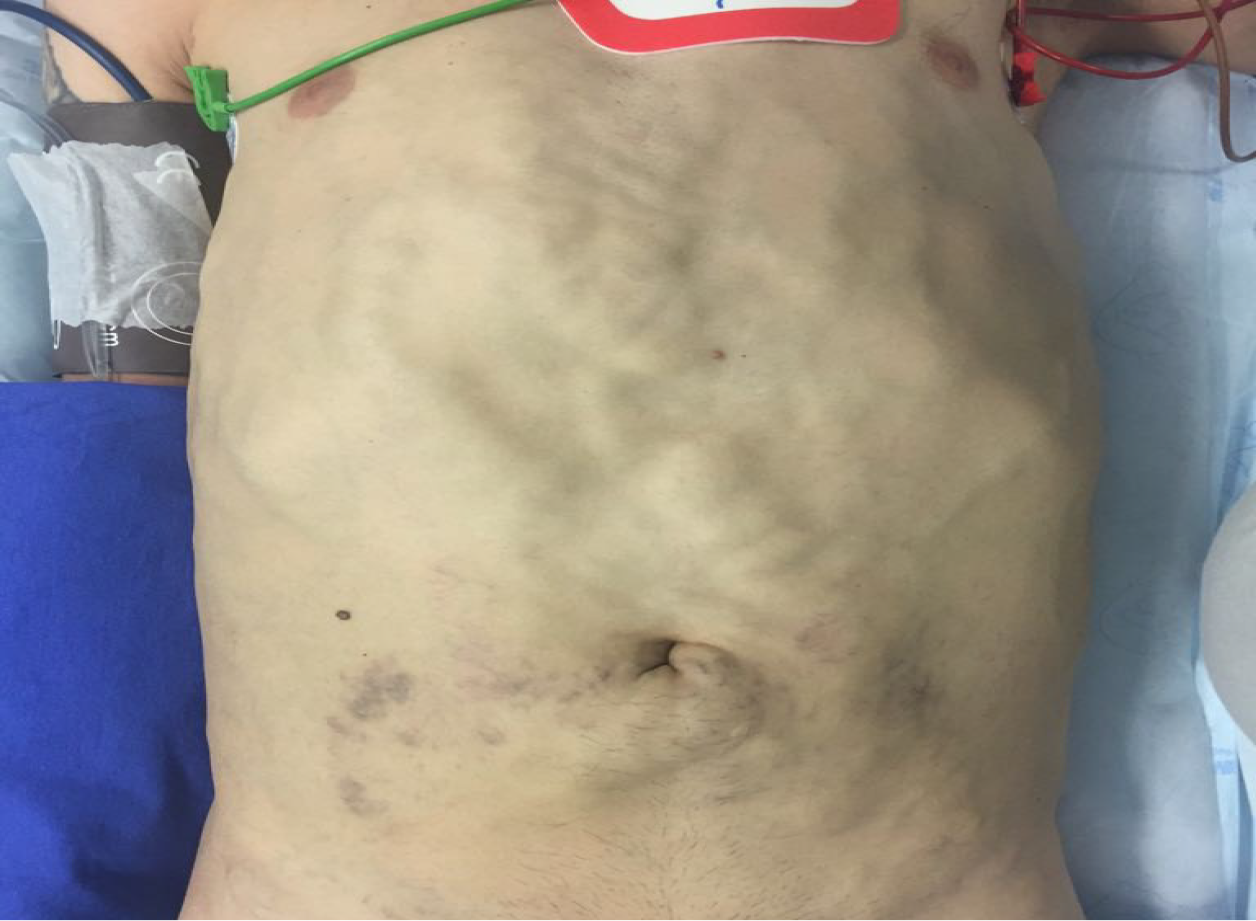
Figure 1 Massive blood return by subcutaneous veins in the anterior abdominal wall, which required the use of venovenous bypass prior to the abdominal incision.
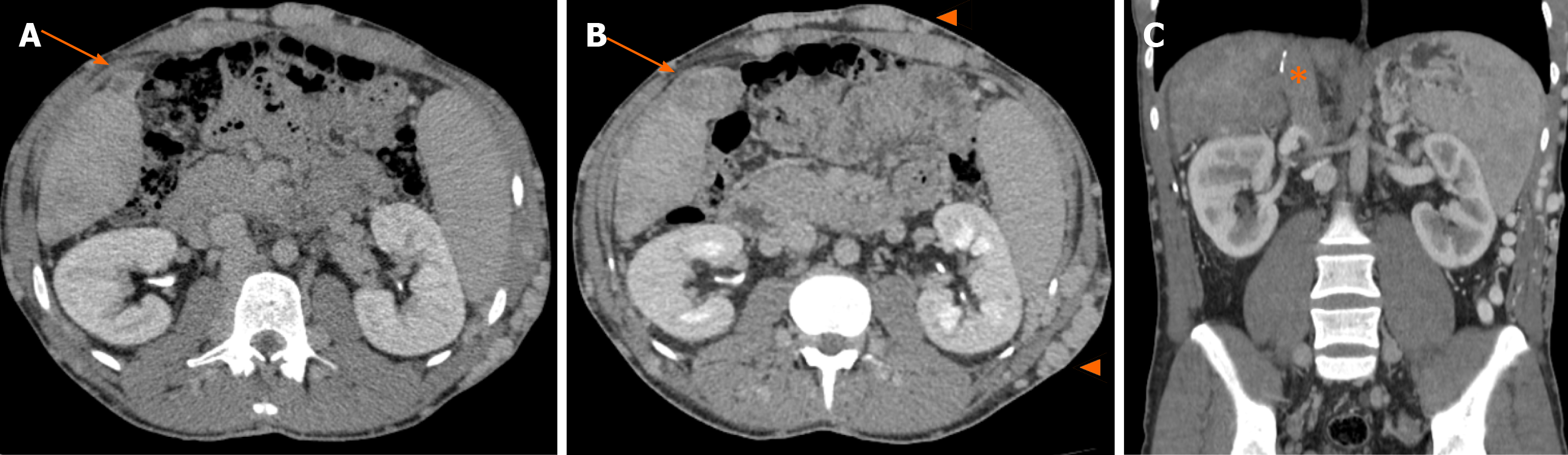
Figure 2 Abdominal computed tomography scans, with a 3-year interval.
A: Heterogeneously vascularized nodule in segment V, of 2 cm, more visible in delayed phase due to hypocaptation (arrow); B: Same nodule in segment V in an exam scan performed 3 years later, with 4 cm (arrow). Massive subcutaneous veins in the abdominal wall are noted (arrowhead); C: The retrohepatic vena cava is completely thrombosed, up to almost the right atrium (asterisk).
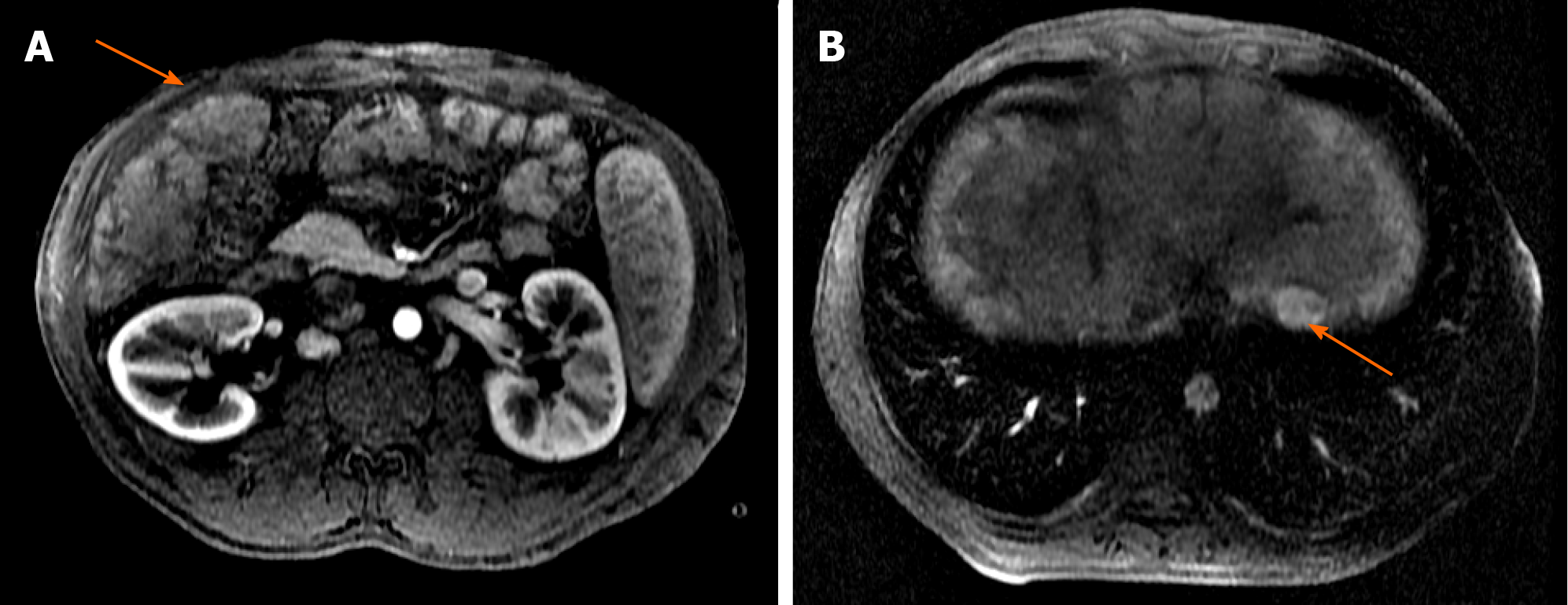
Figure 3 Liver magnetic resonance imaging with hepatobiliary contrast (arterial phase).
A: Hypervascularized nodule in segment V of 4 cm (arrow); B: Hypervascularized nodule in segment II of 2.3 cm (arrow).
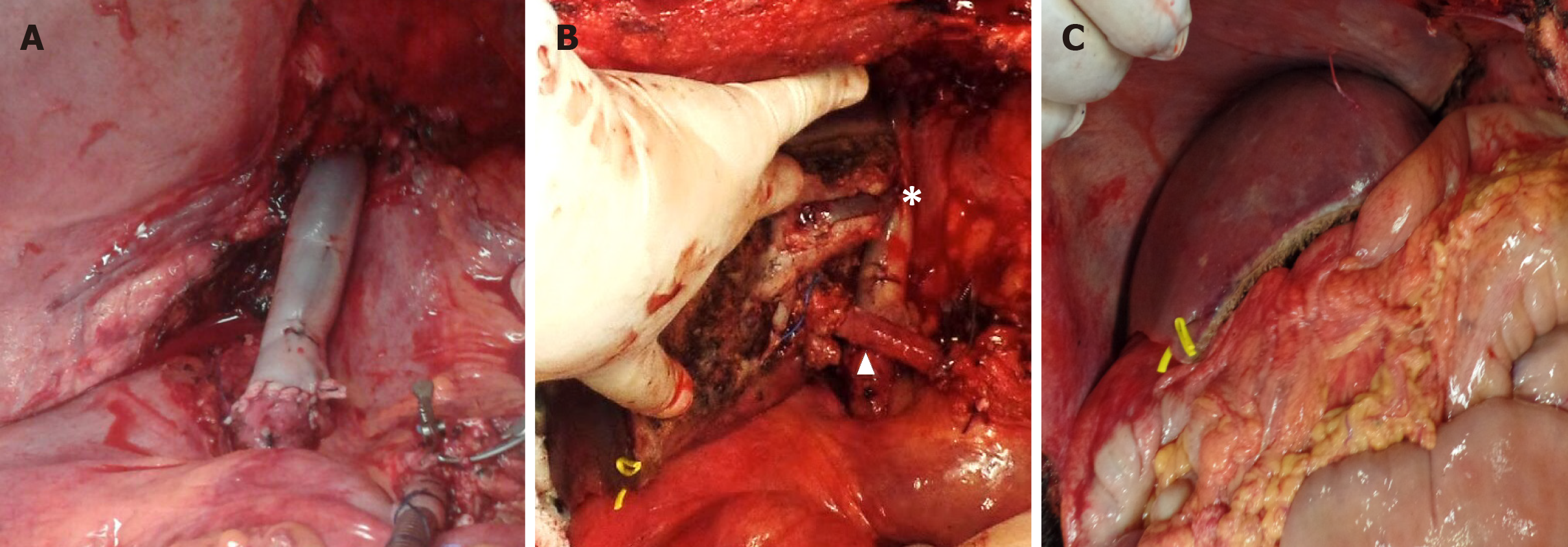
Figure 4 Intraoperative images.
A: Reconstructed retrohepatic vena cava using an infrahepatic vena cava graft of a deceased donor; B: Revascularized graft showing the venous conduit anastomosed to the newly formed vena cava (asterisk) and the portal vein anastomosis (arrowhead); C: Graft final aspect after arterialization at the end of transplantation.
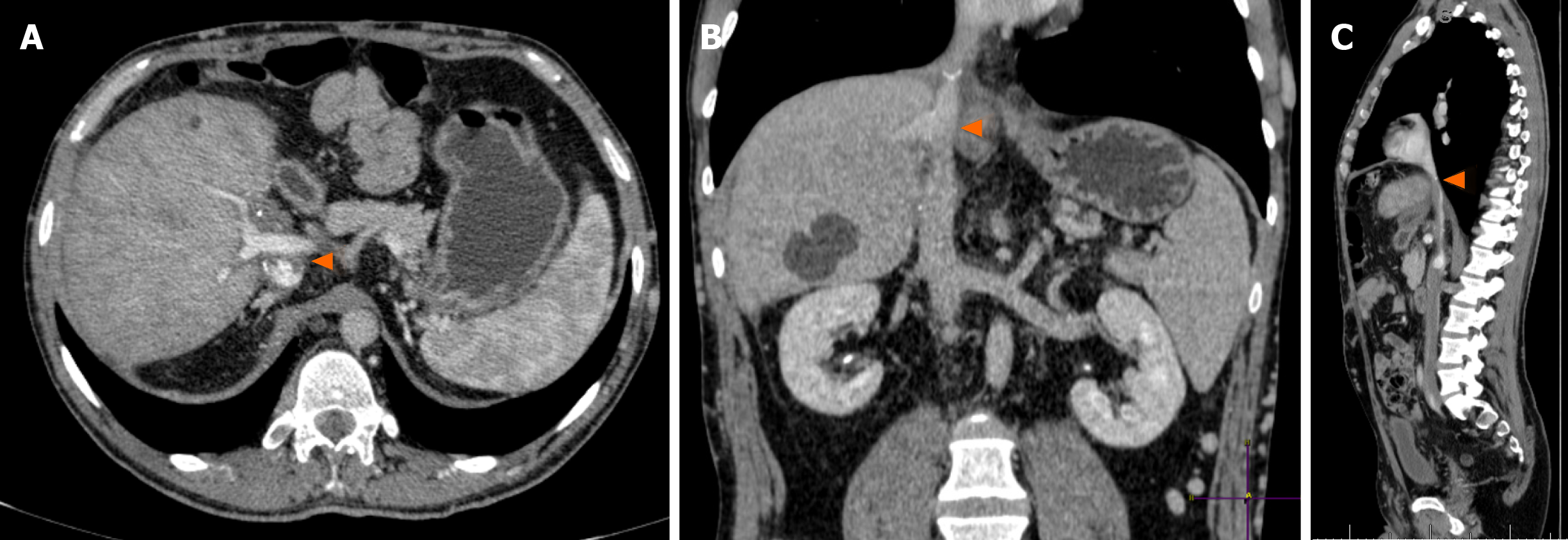
Figure 5 Late postoperative abdominal computed tomography scan, portal phase.
A: Graft with adequate aspect and preserved portal inflow (arrowhead); B: Coronal view showing patent retrohepatic vena cava (arrowhead) and preserved graft outflow; C: Sagittal view of patent retrohepatic vena cava (arrowhead).
- Citation: Rocha-Santos V, Waisberg DR, Pinheiro RS, Nacif LS, Arantes RM, Ducatti L, Martino RB, Haddad LB, Galvao FH, Andraus W, Carneiro-D'Alburquerque LA. Living-donor liver transplantation in Budd-Chiari syndrome with inferior vena cava complete thrombosis: A case report and review of the literature. World J Hepatol 2021; 13(1): 151-161
- URL: https://www.wjgnet.com/1948-5182/full/v13/i1/151.htm
- DOI: https://dx.doi.org/10.4254/wjh.v13.i1.151