Copyright
©The Author(s) 2020.
World J Hepatol. Aug 27, 2020; 12(8): 451-474
Published online Aug 27, 2020. doi: 10.4254/wjh.v12.i8.451
Published online Aug 27, 2020. doi: 10.4254/wjh.v12.i8.451
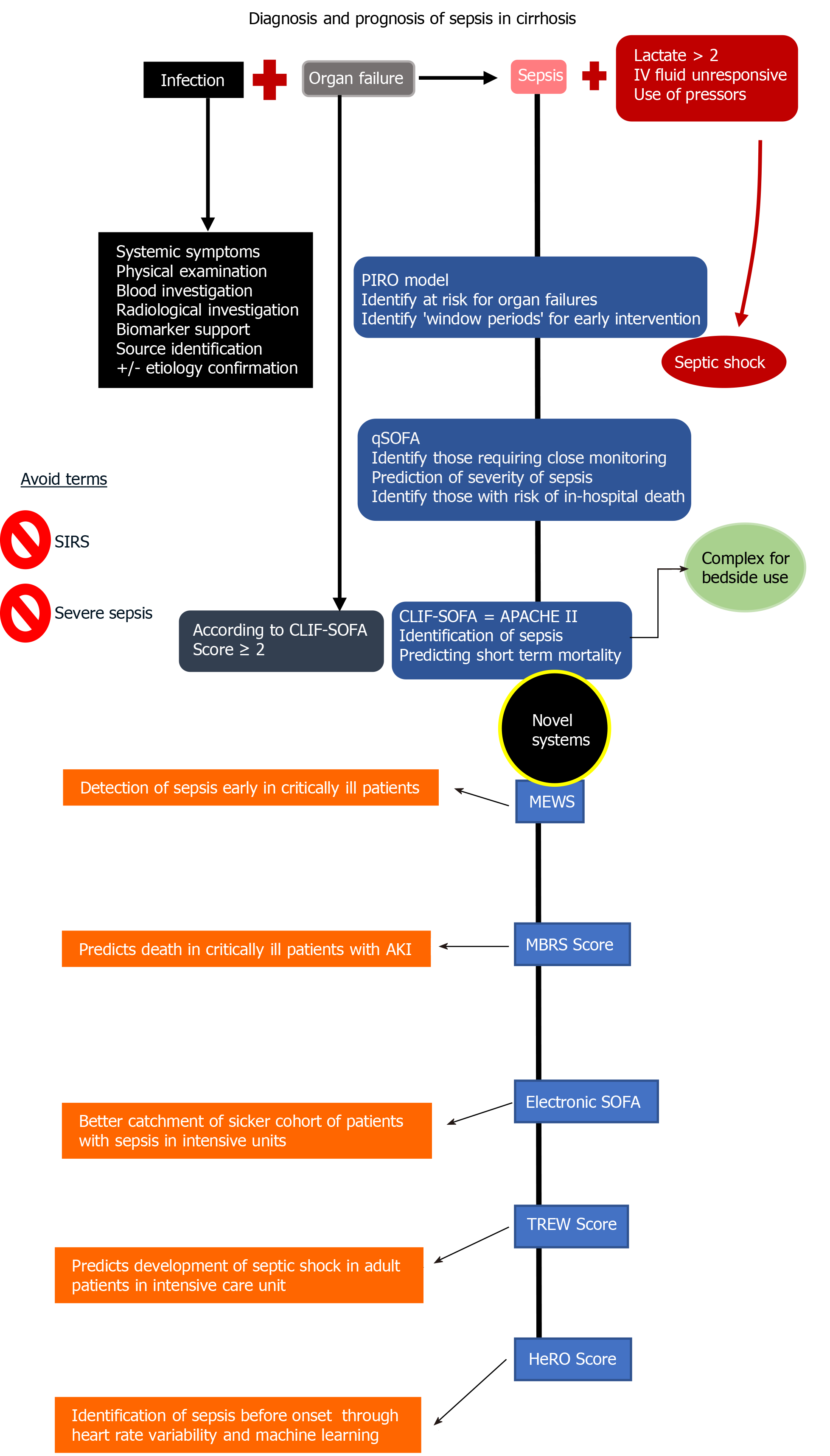
Figure 1 Definitions, diagnosis, and summary of prognostic scoring systems of sepsis[2,4,6,58,63-65].
Sepsis is defined as presence of suspected or confirmed infection in the presence of an organ failure as defined by the sequential organ failure assessment tool. After diagnosis of sepsis, a prognostic tool is utilized to identify patients at risk of worsening or death. APACHE: Acute physiology and chronic health evaluation; CLIF: Chronic liver failure; HeRO: Heart rate index; MBRS: Mean arterial pressure, bilirubin, respiratory failure, sepsis; MEWS: Modified early warning score; PIRO: Predisposition, insult, response, organ failure; qSOFA: Quick sequential organ failure assessment; SIRS: Systemic inflammatory response syndrome; SOFA: Sequential organ failure assessment; TREW: Targeted real-time early warning score.
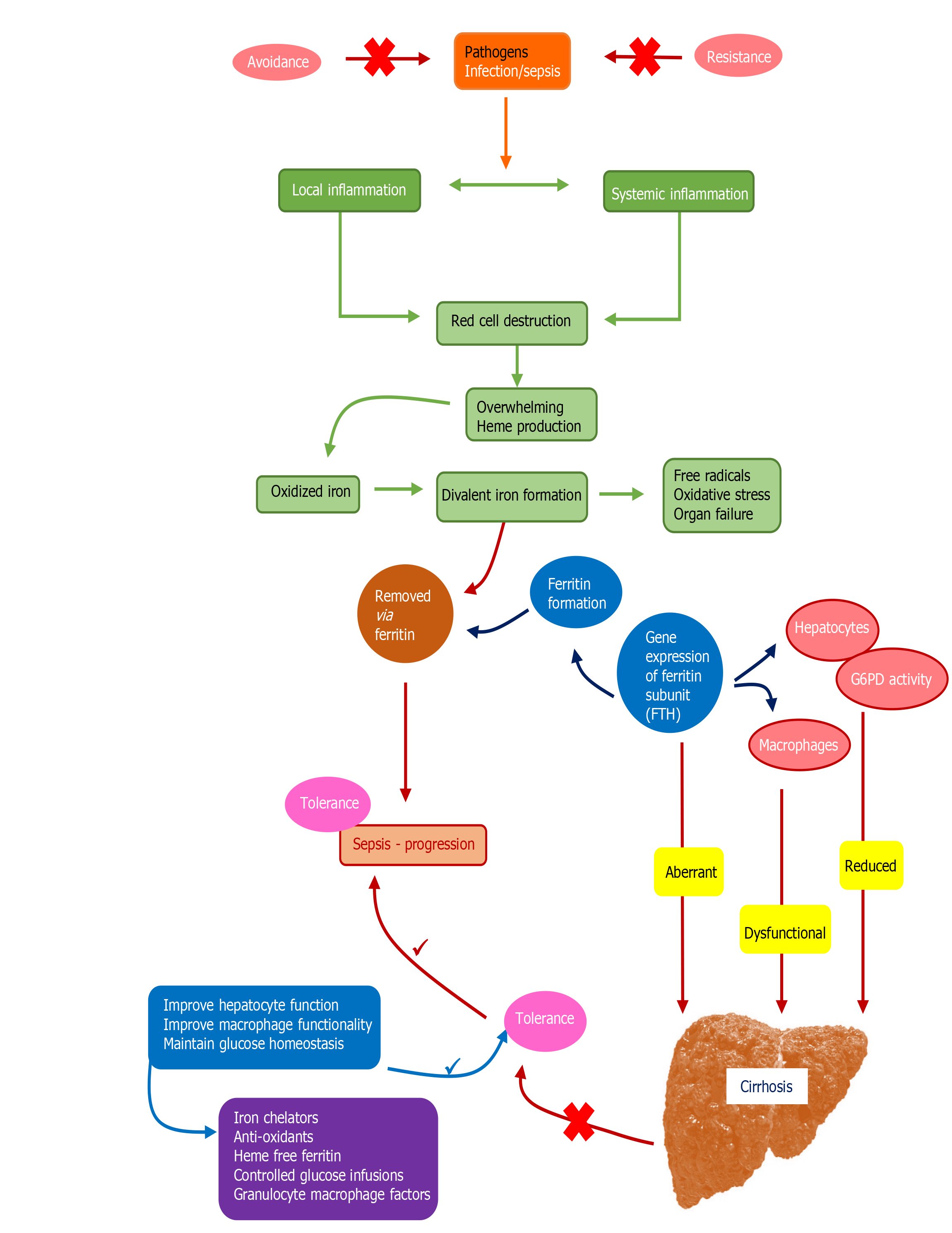
Figure 2 Insights into pathophysiology of tolerance toward sepsis and loss of tolerance leading to higher risk of sepsis in cirrhosis patients[4,23-25].
Apart from tolerance, loss of resistance and exposure to pathogens (shown as red crosses in the upper part of the figure) can initiate infections that can lead to development of sepsis. In patients with infections who develop sepsis, local and systemic inflammation lead to dysregulated red cell homeostasis and development of toxic oxidants especially iron ligands that are removed by ferritin. Ferritin formation and oxidant sweep are regulated systematically through hepatocyte and macrophage functions in the healthy liver through expression of glucose-6-phosphatase (G6PD) and ferritin H gene subunit (FTH). In cirrhosis, liver dysfunction results in aberrant FTH activity, defective macrophage and hepatocyte functions and reduction in G6PD activity, resulting in increased oxidant stress and loss of tolerance to infection, leading to progression of sepsis through reduction in functional ferritin (shown as red crosses at the bottom). The blue and purple boxes demonstrate steps and measures for correction of dysregulated responses in a patient with cirrhosis, respectively, so as to improve tolerance to infection and prevention of sepsis. FTH: Ferritin H gene subunit; G6PD: Glucose-6-phosphatase.
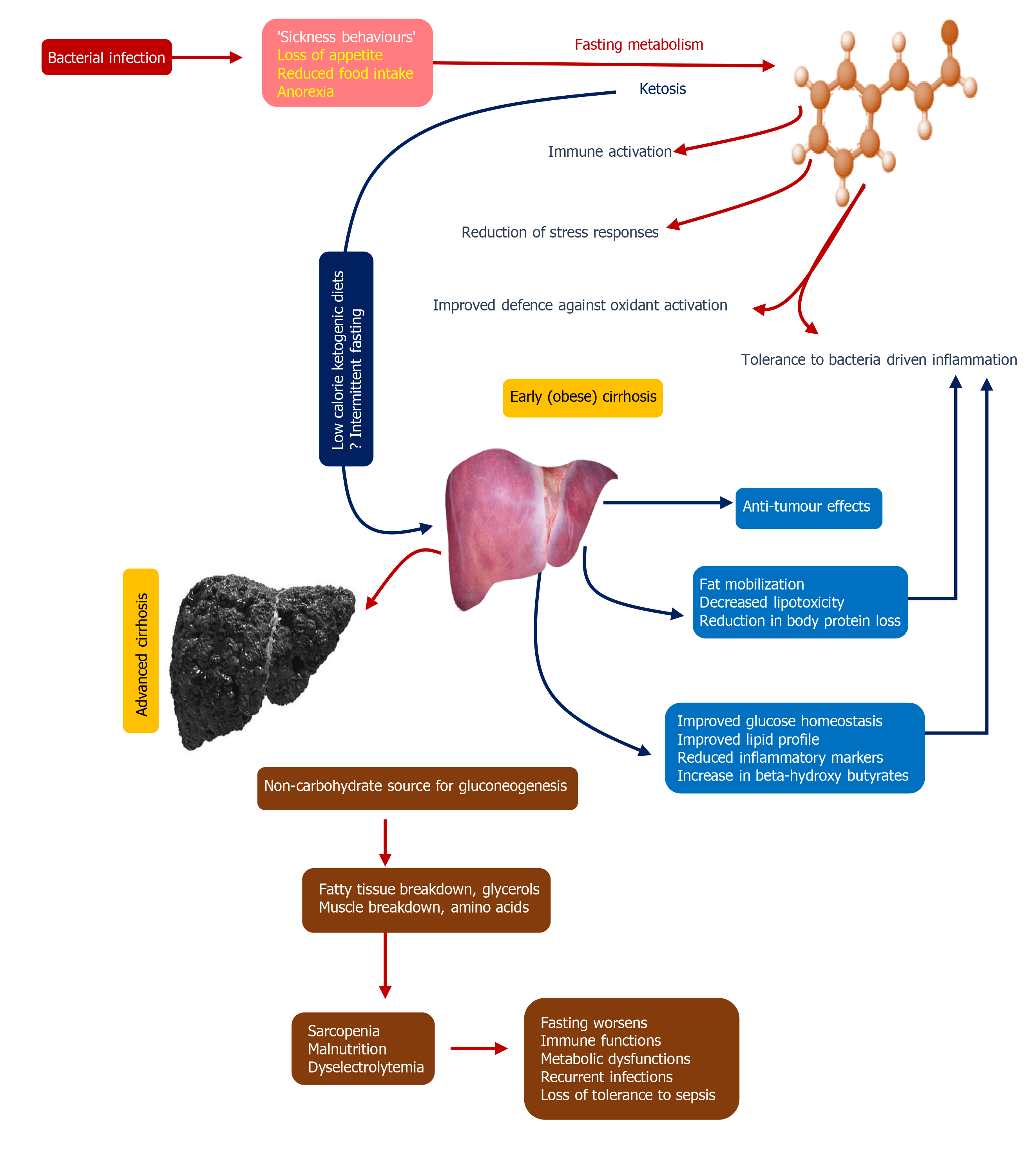
Figure 3 Fasting metabolism and its impact on immune homeostasis and enhanced tolerance to infections[26-28].
The figure demonstrates the potential mechanisms associated with fasting metabolism on immune functions that ultimately prove beneficial for prevention of and combating infections. This could be hypothesized to have benefits in patients with early cirrhosis, especially in those who are obese, pending bench to bedside translational studies. Nonetheless, in advanced cirrhosis, on the contrary, nutritional management to improve immune functions, prevention of infections, and boosting tolerance to sepsis is of importance.
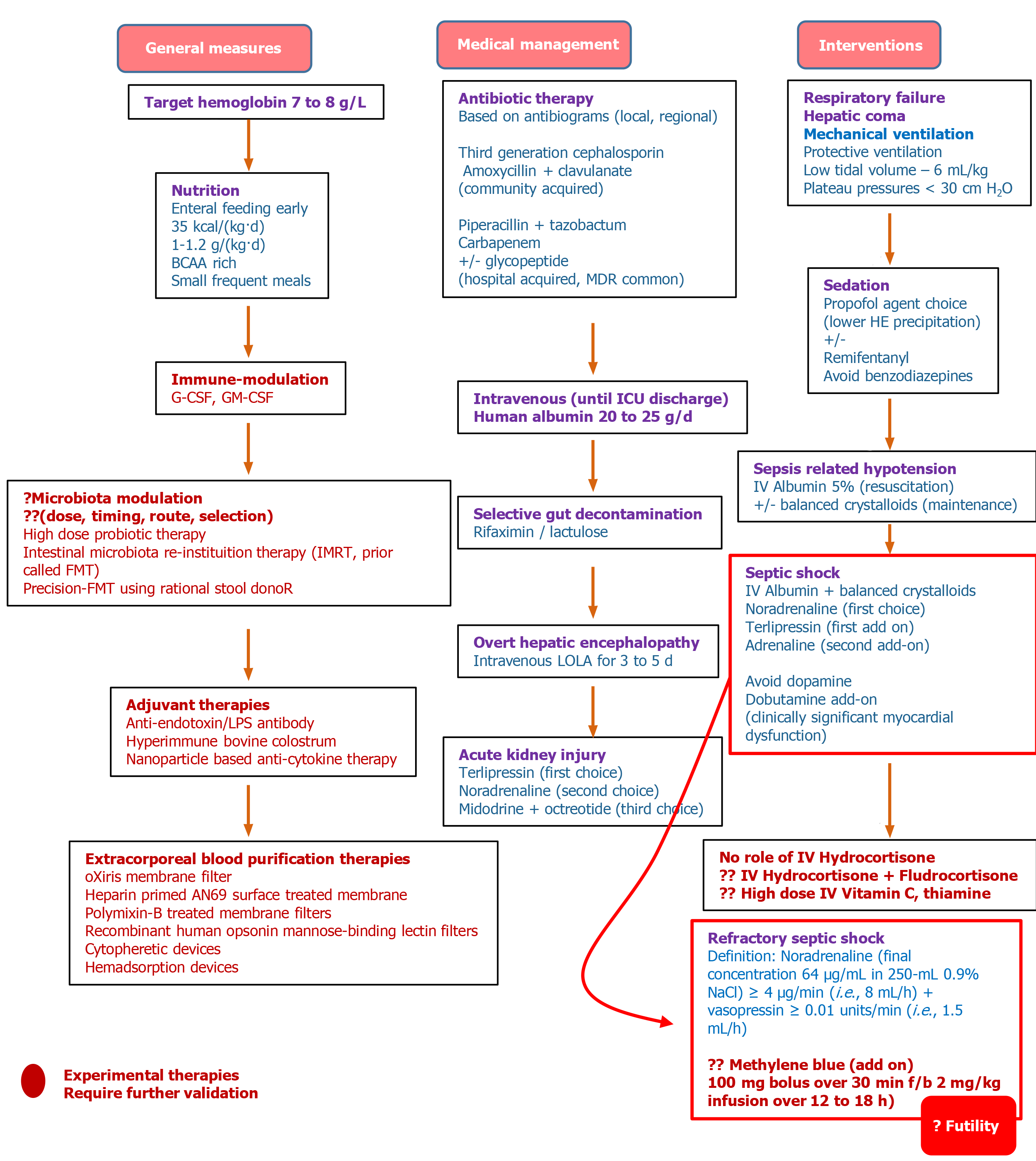
Figure 5 The proposed treatment algorithm for sepsis in cirrhosis[66,68,70-72,75].
BCAA: Branched-chain amino acids; FMT: Faecal microbiota transplantation; G-CSF: Granulocyte-colony stimulating factor; GM: Granulocyte-macrophage; ICU: Intensive care unit; IMRT: Intestinal microbiota re-instituition therapy; IV: Intravenous; LOLA: L-ornitine L-aspartate; LPS: Lipopolysaccharide; MDR: Multidrug resistant.
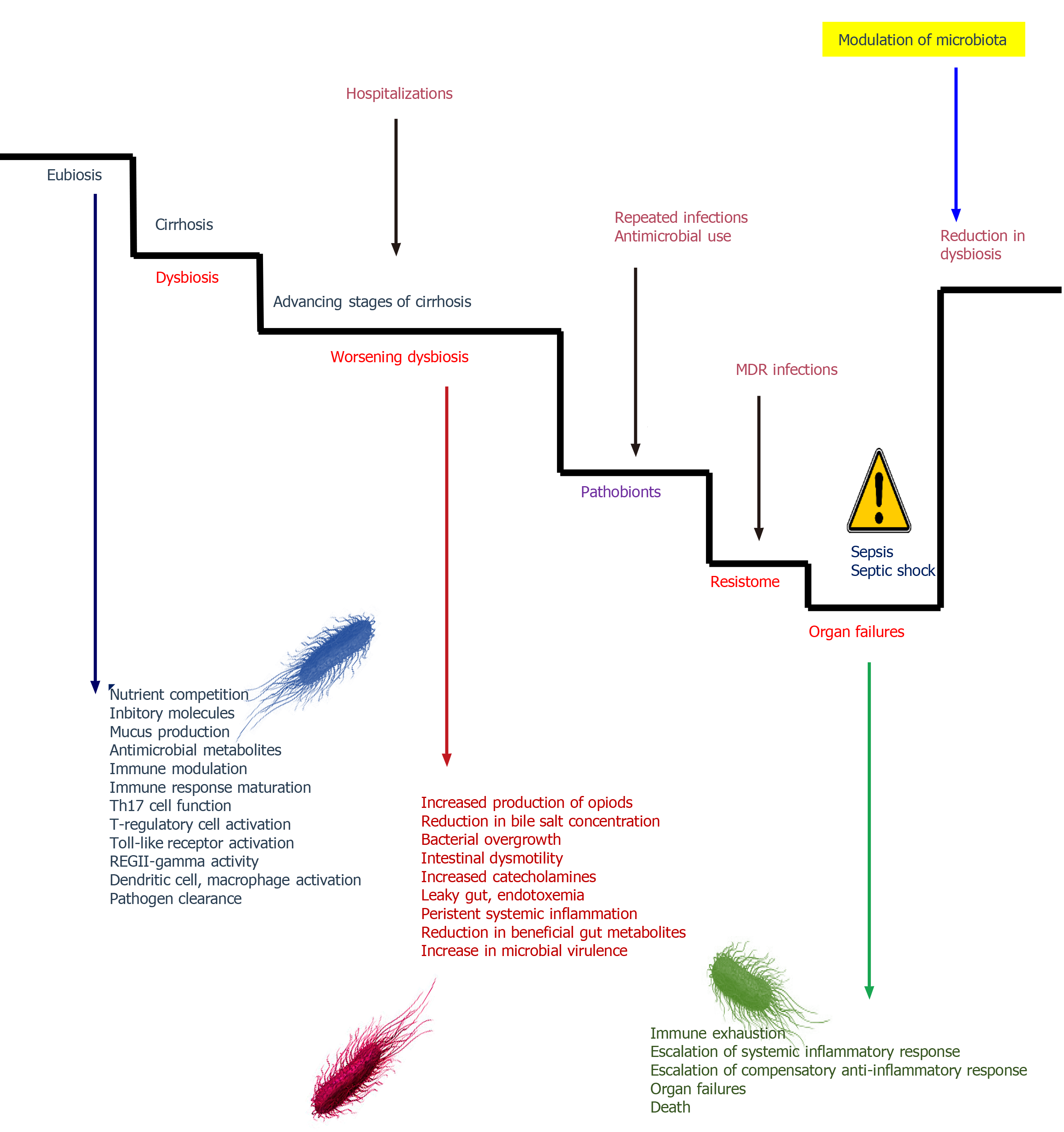
Figure 6 The role of gut microbiota in driving and worsening sepsis and cirrhosis[78,80,81].
Gut microbiota modulation is an interesting approach to management of sepsis in the future. Reducing dysbiotic bacterial communities and favouring commensals that improve host immune functions, promote endogenous antimicrobial metabolite formation and resist pathogenic colonization could be achieved through high dose probiotics or intestinal microbiota re-institution therapy. MDR: Multidrug resistant.
- Citation: Philips CA, Ahamed R, Rajesh S, George T, Mohanan M, Augustine P. Update on diagnosis and management of sepsis in cirrhosis: Current advances. World J Hepatol 2020; 12(8): 451-474
- URL: https://www.wjgnet.com/1948-5182/full/v12/i8/451.htm
- DOI: https://dx.doi.org/10.4254/wjh.v12.i8.451