INTRODUCTION
The delivery of stem cells, regardless of their source, is expected to be within, or surrounding regions of tissue injuries. This editorial discusses the mechanisms by which stem cells could interact with different molecules at and within areas of tissue injury. For the purpose of this review, the area of injury and molecules found within the zones of injuries are referred as microenvironments. The sources of molecules with regions of tissue damage are varied. For example, cytokines can be produced by cells within and around the damaged tissue; neurotransmitters can be released from damaged and/or intact nerve fibers as well as from infiltrating immune cells. While the sources of molecules are varied, the types of molecules belong to different families. These include, but are not limited to, peptides, cytokines, and extracellular matrix proteins. Interactions between cells and soluble molecules are two-way processes. While the stem cells respond by producing other factors, these factors stimulate the stem cells, through autocrine and paracrine mechanisms, to induce further changes in the stem cells. The mechanisms of these interactions could be positive and/or negative to the injuries. The questions that are pertinent for stem cells therapy include the method by which stem cells should be implanted at the region of injury. Intuitively, one should consider if the implanted stem cells should be delivered to allow for modulation of the damaged microenvironment or vice versa. The answer to this key question will depend on the goal of the therapy. Another question is whether the aim of stem cell therapy is to attain protection that prevents further damage to the tissue or to replace damaged cells. This would require the stem cells to generate differentiated or specialized cells. In any event, the stem cells or specialized cells will establish crosstalk with cells and molecules within the microenvironment.
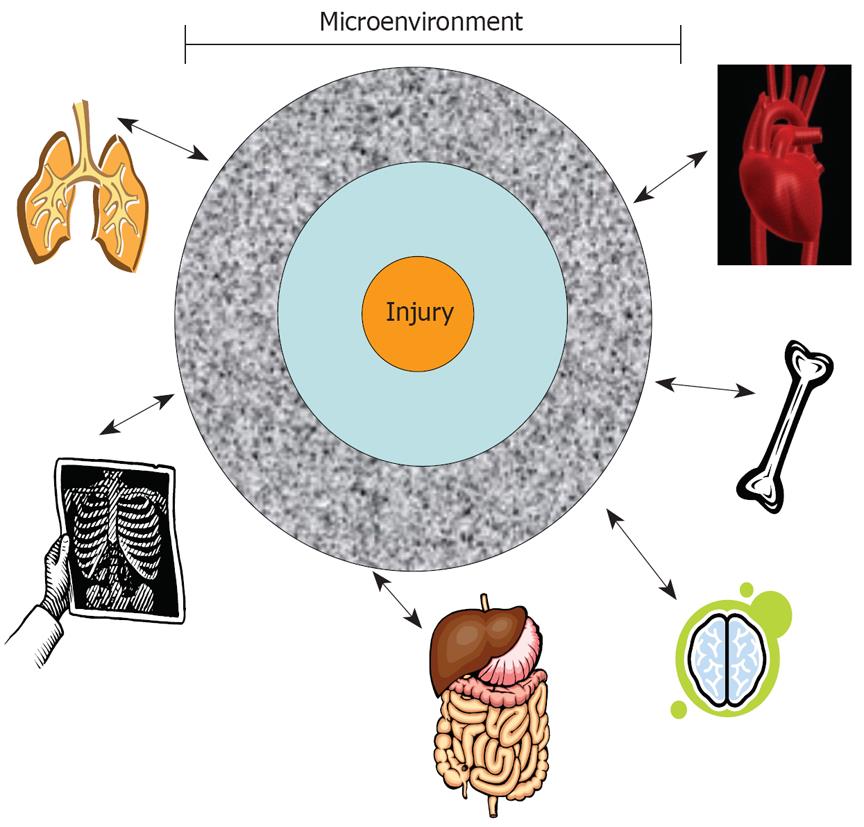
Future therapies will need to consider the degree of changes within the microenvironment because tissue injuries differ. Furthermore, the milieu would differ at zones away from the area of injury (Figure 1). If future research studies show that altered tissue microenvironments could attain effective therapy by stem cells, such information will be crucial to stem cell therapies. Adjuvant treatments will be required for drugs to achieve the desired changes. Drugs are available to target a variety of molecules and, when administered with stem cells, will enhance stem cell treatments. This editorial discusses general issues facing adult human mesenchymal stem cells (MSCs). These discussions could be extrapolated for any type of stem cell and for methods to repair damaged tissues.
Figure 1 A representative focal point of tissue injury.
This central point expands to zones of injury with each region showing varied degrees of tissue damage. The responses from the zones of injuries, through nerve fibers, soluble factors, or immune cells, could establish cross communications with other distant organs.
The immune properties of adult human MSCs have been well studied. A review of the list of clinical trials with these stem cells (clinicaltrials.gov) shows their global application for various diseases. Based on the current large numbers of trials with MSCs, it appears that these stem cells are safe for use in humans. However, a clear statement on their safety awaits longitudinal follow-up.
ALLOGENEIC VARIATIONS IN KEY CONSIDERATIONS FOR CHOICE OF STEM CELL TYPE
A major consideration in stem cell therapy is the availability of “off the shelf” sources of stem cells. In theory, all stem cells could be readily available for transplantation. The issue is whether particular “off the shelf” stem cells would be rejected by immunological reactions. While such rejections are expected for allogeneic stem cells, thus far, allogeneic MSCs seem to behave contrary to this dogma. It is important to discern the differences between the immune suppressive property of a stem cell and its ability to elicit an immune response. In the case of immune suppression, stem cells negatively regulate a reaction of immune stimulation. If a stem cell initiates an immune response from a host, that stem cell is perceived as foreign to the host. The latter response will be initiated by differences in the major histocompatibility class II and/or class I (MHC II or MHC I) molecules on the stem cells. On the other hand, although less studied, a stem cell can also act as an immune cell and initiate inflammatory responses by autologous immune cells.
Autologous stem cells, or stem cells from fraternal twins, are ideal cases for avoiding rejection of the transplanted stem cells. However, probability of obtaining stem cells from fraternal twins would be low. Furthermore, in cases where the fraternal twin exists, if there is an injury that requires immune transplantation of stem cells, it would be problematic to wait for expansion of the stem cells. Immediate needs for stem cells include repair or protection of brain injuries and cardiac infarct. It could be argued that some forms of brain injuries could wait for the inflammation to subside, thereby providing healthcare workers a few days for the use of autologous stem cells. There are two problems with this scenario; firstly, the stem cells might require weeks for expansion and characterization in a good manufacturing facility. Secondly, a particular organ is not mutually exclusive of the other; thus, injury to one organ could cause damage to another where the stem cells might be located (Figure 1). Thus, during injury, stem cells from a distant organ could be defective, thereby leaving autologous stem cells as the preferred source for therapy.
If organ-specific autologous stem cells are transiently damaged during injury, the time before these stem cells are ready for therapy would be significantly delayed. Additional studies are needed on the integrity of autologous stem cells at sites distant from injuries. Several reports show a brain-bone marrow connection, based on functional studies and anatomical evidence by nerve tracing analyses[1-3]. Furthermore, studies with surgical trauma patients reported dysfunctional bone marrow-derived hematopoietic stem cells (HSCs)[4]. The next section discusses the immune properties of MSCs and argues for investigational studies on the bidirectional communication between these stem cells and inflammatory mediators within tissue microenvironments. It is imperative to dissect the responses of MSCs at areas of tissue injuries, especially because these stem cells are in various trials for immune-mediated disorders[5].
MSCs
MSCs are ubiquitously expressed, with the adult bone marrow as the major source[6-9]. MSCs differentiate into specialized cells, for example stroma, osteoblasts, adipocytes and chrondrocytes, via distinct lineages[10]. Stroma and osteoblasts are key supporting cells for hematopoietic stem cells functions, and form functional links between the two major bone marrow resident stem cells: hematopoietic and MSCs[6,11,12]. MSCs and HSCs are located at distinct regions of human bone marrow[13]. Hematopoietic stem cells prefer areas of low oxygen, close to the endosteum, whereas MSCs surround the blood vessels where oxygen levels are relatively high [6,14,15].
Blood vessels and nerve fibers generally follow each other into bone marrow. Therefore nerve endings would be in close contact with MSCs surrounding the abluminal blood vessels of bone marrow[6]. In fact, the anatomical literature shows nerve fibers forming synapse-like structures with reticular type cells of bone marrow[8]. MSCs have been referred to as reticular cells[6], indicating that MSCs are in contact with the nerve endings. In other reports, MSCs, are referred to as pericytes and form contacts with neurons[16]. The nerve contact with MSCs could be significant, based on the identification of neurotransmitter receptors on MSCs[17,18].
MSCs show potential for clinical application with evidence of tissue regeneration[19-23]. These stem cells could overcome the major obstacle associated with those of allogeneic sources. MSCs show unique immune properties, underscoring their clinical use for preventing graft vs host disease (GVHD)[24,25]. MSCs exhibit a veto property, indicating that they could thwart GVDH as third party cells[26,28]. Interestingly, the veto function of MSCs is specific for GVDH-type reactions because similar suppression has not been observed in responses to recall antigens[28].
MSCs express genes for different cytokines and their receptors and act as antigen presenting cells (APCs), underscoring the immune plasticity of MSCs as immune suppressor and immune enhancer cells[29-31]. The APC property occurs within a narrow window, followed by its reversion to an immune suppressor cell[29]. This bimodal property of MSCs is important to prevent exacerbated inflammation. It is suggested that this dual role of MSCs is responsible for homeostasis in bone marrow and prevents exacerbated hematopoietic suppression during inflammation[32-34].
The mechanisms by which MSCs exert immune suppression are complex. These functions involve reactions ranging from the production of cytokines with immune suppressor functions to the stimulation of regulatory T-cells and suppression of T cytotoxic activity[5,30,35]. The expression of MHC-II, as well as the involvement of interferon-gamma (IFN-γ) in the immune function of MSCs, needs special attention[29,30]. A subset of MSCs expresses MHC-II, which is decreased as the stem cells become specialized cells. This has been demonstrated in studies where the MSCs, transdifferentiated to neurons, show a gradual decrease in MHC-II expression[36]. The addition of IFNγ to the MSC-derived neurons resulted in re-expression of MHC-II. This indicates that in future stem cell therapy, the repair of organs with replaced cells could re-express MHC-II. These patients will need to be followed for long-term tolerance. However, these findings underscore the need further investigation to determine methods of inducing anergy to the “foreign” MHC molecules.
PERSPECTIVE
Issues of allogeneic vs autologous stem cell delivery are key points when considering stem cell therapies. Another consideration for effective stem cell therapy is changes to stem cells by microenvironmental-induced responses by the implanted stem cells. Another major consideration is the possibility of tumor formation by the stem cells, even though the incidence of such an occurrence would be greater in embryonic stem cells. However, one cannot be certain that tumors would not be a problem for adult stem cells.
The maintenance of stem cells involves several genes, in particular those that are linked to cancer biology. During tissue injury, such as in traumatic brain injury, spinal cord injury, or myocardial infarction, the immune system will migrate towards the regions of insult. Once in the area, the immune cells will produce several soluble mediators, such as cytokines and chemokines. These two families of mediators can act locally through specific receptors on MSCs[37]. The resulting functions will depend on the concentrations of cytokines and the responses by the MSCs. The responses of the stem cells could be beneficial and assist in the repair process, or can be deleterious. The latter could occur if the reaction attracts additional immune cells to exacerbate inflammation, activates genes in the stem cells that can cause tumor formation, or activates genes in the stem cells to produce factors prematurely, which would be produced by specialized cells. On the other hand, exacerbated immune reactions could be protective. Thus, the biology of stem cells and the microenvironment of the area of tissue injury will determine the methods by which the therapies are developed.
The following are relevant questions when considering stem cell delivery within the context of varying microenvironments: (1) Should one type of stem cell serve as effective therapy for a particular type of tissue injury over another type? It is possible that one type of stem cell would be effective for a particular repair and another for a distinct injury; (2) Should the particular type of stem cell depend on the extent of tissue injury? That is, one type of stem cell might be better for acute injury and another for chronic injury; (3) Would the microenvironment influence the developmental stage at which stem cells are delivered? It is possible that the factors present would determine if effective repair could be caused by undifferentiated vs partly vs completely differentiated stem cells; and (4) Would translational science be more effective by partnership between academia and pharmaceuticals? The latter would have drugs readily available to combine with stem cells for therapies.
In addition to variations among regions of tissue injuries, the method by which the stem cells are delivered is also an issue. While bioengineering has been an intense area of investigation, other methods are also available. These types of questions would entail inter- and multi-disciplinary teams to deliver stem cells to the clinic. There are numerous clinical trials of stem cells; thus, it is time for the scientific community to determine if stem cells can be referred to as drugs. This will be finally determined by the pharmaceutical companies as medicine moves to include stem cell therapies, perhaps for all types of disorders.
Peer reviewer: Anna Chiara Piscaglia, MD, Specialist in Gastroenterology and Digestive Endoscopy, GI & Liver Stem Cell Research Group (GILSteR), Department of Internal Medicine - Digestive Endoscopy Unit, Gemelli Hospital - Catholic University of Rome, Largo A. Gemelli, 8 - 00168 Rome, Italy
S- Editor Li LF L- Editor Stewart GJ E- Editor Lin YP