Copyright
©The Author(s) 2017.
World J Stem Cells. Mar 26, 2017; 9(3): 45-67
Published online Mar 26, 2017. doi: 10.4252/wjsc.v9.i3.45
Published online Mar 26, 2017. doi: 10.4252/wjsc.v9.i3.45
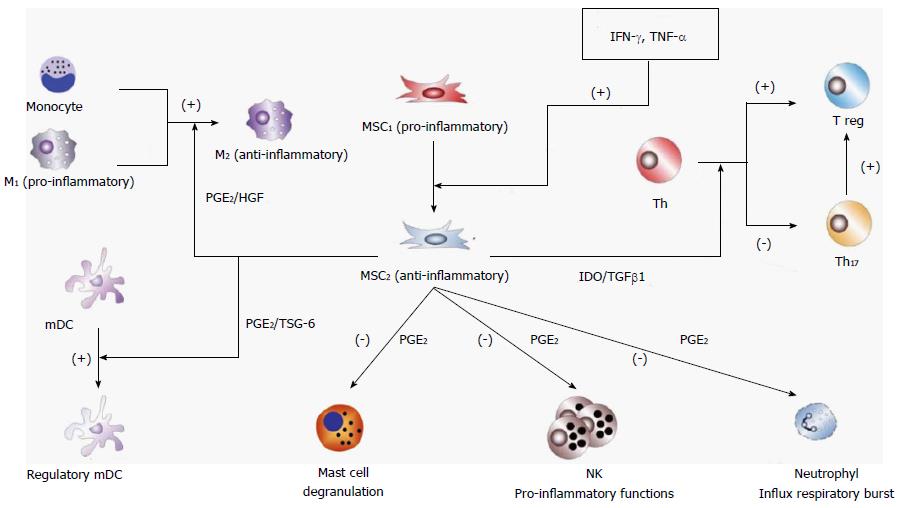
Figure 1 Mesenchymal stem cell immunosuppressive regulatory effects.
MSCs are polarized to an immunosuppressive stage (MSC2) by a high relative concentration of pro-inflammatory cytokines such as IFN-γ and TNF-α. MSC2 induce macrophage polarization of monocytes and pro-inflammatory macrophages (M1) to the immunosuppressive stage M2 by secreting immunomodulatory mediators such as PGE2 and HGF. MSC2 also induce differentiation of Th and Th17 to T regulatory cells (Treg) by secretion of TGF-β1 and indoleamine 2,3-dioxygenase (IDO). Furthermore, MSC2 induce differentiation of mDCs to a regulatory anti-inflammatory stage (mDCreg), inhibit mast cell degranulation, inhibit NK cell pro-inflammatory functions and suppresses neutrophil respiratory burst. MSC2-derived PGE2 contributes to all of these effects. Other cytokines that have been implicated in at least some of the MSC2 immune-suppressive effects are IL-6 and GM-CSF[8]. MSC: Mesenchymal stem cell; IFN-γ: Interferon-gamma; TNF-α: Tumor necrosis factor-alpha; PGE2: Prostaglandin E2; Th: T helper; HGF: Hepatic growth factor; TGF-β1: Transforming growth factor-beta 1; mDCs: Monocyte-derived dendritic cells; NK: Natural killer; IL-6: Interleukin-6; GM-CSF: Granulocyte macrophage-colony stimulating factor.
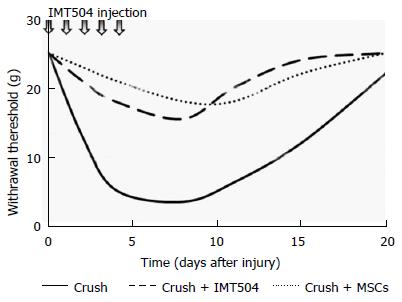
Figure 2 Effect of IMT504 or mesenchymal stem cell treatment on the development of mechanical allodynia in rats.
Sciatic nerve crush induced a significant decrease in paw withdrawal threshold to the von Frey filaments. It is noticeable that the administration of either IMT504 or MSCs prevents the development of allodynia. Experimental details are described in Coronel et al[343]. MSC: Mesenchymal stem cell.
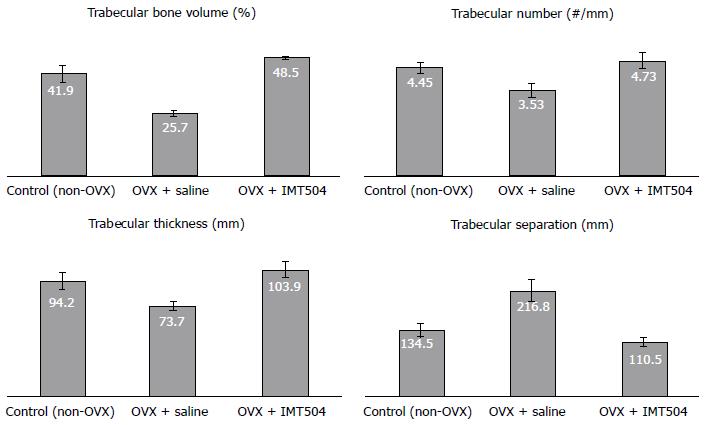
Figure 3 Effect of the IMT504 treatment on bone structure in ovariectomized (osteoporotic) rats.
Female Sprague-Dawley 16-wk-old rats underwent ovariectomy (OVX). When animals were 1-year-old, half of them (treated group) received a subcutaneous dose of IMT504 (20 mg/kg per dose in saline) injected daily for 5 successive days. The other half-received saline under the same scheme (non-treated group). The treatment was repeated 30 d later. A group of non-OVX rats served as control. Body weight and general health was measured weekly. One month after the last treatment, animals were euthanized and femurs dissected, decalcified and embedded in paraffin. Slides of 0.5-μm sections of the distal femur were generated using a Leica RM2145 microtome, stained with hematoxylin and eosin, and examined by light microscopy. Digital images were recorded with a Nikon Coolpix 4500 camera at 16.5-fold magnification under a Leica MZ16A stereomicroscope. Three fields in each slide were evaluated, totaling a combined area of 3 mm2. Trabecular bone was identified, and its perimeter and area measured. Histomorphometric analysis was performed using the Image Pro-Plus 4.5 software and standard histomorphometric parameters calculated (our unpublished results).
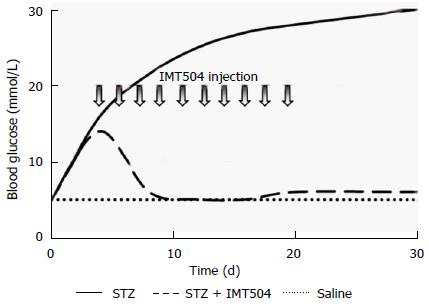
Figure 4 IMT504 treatment induced a marked recovery of the diabetic condition in streptozotocin-treated rats.
Arrows indicate IMT504 treatment, which consisted of daily subcutaneous injections containing 4 mg of IMT504 over 10 successive days. Experimental details are described in Bianchi et al[357]. STZ: Streptozotocin.
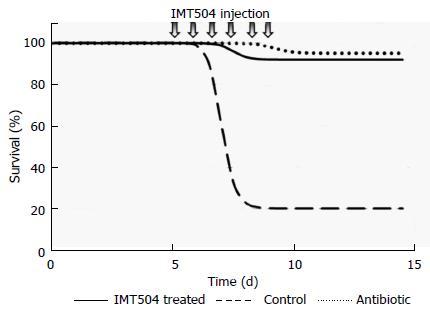
Figure 5 IMT504 protects neutropenic animals from fatal Pseudomonas aeruginosa bacteremia and sepsis.
Kaplan-Meier survival plot representing IMT504 monotherapy vs antibiotic (cefepime) monotherapy vs control. IMT504 daily doses were started at day 5 after bacterial infection. Arrows indicate IMT504 treatment, which consisted of subcutaneous injections containing 50 g of IMT504 over 5 successive days. Experimental details described in Chahin et al[363].
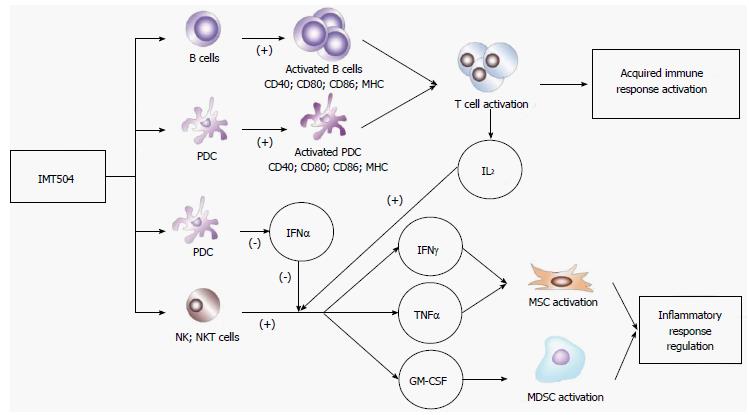
Figure 6 IMT504 effects on the immune system.
Primary targets of IMT504 are B lymphocytes (B), PDCs, NK and NKT cells. IMT504 acting on B and PDCs induces a phenotype of antigen presenting cells, which in the presence of an appropriate antigenic stimulus initiates a strong adaptive immune response[371-373]. On the other hand, IMT504 acting on NK and NKT cells, in collaboration with IL-2, induces the strong secretion of IFN-γ and TNF-α that can induce MSC immunosuppressive properties and of GM-CSF that can activate MDSCs. This immunosuppressive pathway is inhibited by the presence of IFN-α. Reciprocally, IMT504 inhibits IFN-α secretion by PDCs. Therefore, activation of this immunosuppressive pathway depends on the balance between IMT504 activity and activity of IFN-α inducers that are present[331]. PDCs: Plasmacytoid dendritic cells; NK: Natural killer; NKT: Natural killer T; IL-2: Interleukin-2; IFN-γ: Interferon-gamma; TNF-α: Tumor necrosis factor-alpha; GM-CSF: Granulocyte macrophage colony-stimulating factor; MDSCs: Myeloid-derived suppressor cells.
- Citation: Zorzopulos J, Opal SM, Hernando-Insúa A, Rodriguez JM, Elías F, Fló J, López RA, Chasseing NA, Lux-Lantos VA, Coronel MF, Franco R, Montaner AD, Horn DL. Immunomodulatory oligonucleotide IMT504: Effects on mesenchymal stem cells as a first-in-class immunoprotective/immunoregenerative therapy. World J Stem Cells 2017; 9(3): 45-67
- URL: https://www.wjgnet.com/1948-0210/full/v9/i3/45.htm
- DOI: https://dx.doi.org/10.4252/wjsc.v9.i3.45