Published online May 15, 2003. doi: 10.3748/wjg.v9.i5.1090
Revised: September 23, 2002
Accepted: November 4, 2002
Published online: May 15, 2003
AIM: To develop a technique of combined endoscopic sclerotherapy and ligation (ESL) in which both techniques of endoscopic sclerotherapy (ES) and endoscopic variceal ligation (EVL) can be optimally used.
METHODS: ESL was performed in 10 patients (age 46.4 ± 7.9; 9 males, 1 female) with cirrhosis of liver using sclerotherapy needle and Speedband, Superview multiple band ligater (Boston Scientific, Microvasive, Watertown, MA). A single band was placed 5-10 cm proximal to the gastro-esophageal junction over each varix from proximal to distal margin, followed by intravariceal injection of 1.5% ethoxysclerol (4 ml each) 2 to 3 cm proximal to the gastroesophageal junction on the ligated varices distal to deployed band. EVL was then performed at the injection site. Similarly other varices were also injected and ligated from distal to proximally. In the subsequent sessions, ES alone was performed to sclerose small varices at the gastroesophageal junction.
RESULTS: ESL was successfully performed in all patients. A median of 3 (ESL 1, ES 2) sessions (ranged 1-4) were required to eradicate the varices in 9 (90%) of 10 patients. Recurrence of varices without bleed was seen in 1 patient during a mean follow-up of 10.3 months (ranged 6-15). Two patients died of liver failure. None died of variceal bleeding. None of the patients had procedure related complications.
CONCLUSION: ESL may be useful in the fast eradication of esophageal varices. However, randomised controlled trials are required to find out its relative efficacy and impact on variceal recurrence in comparison to ES or EVL.
- Citation: Dhiman RK, Chawla YK. A new technique of combined endoscopic sclerotherapy and ligation for variceal bleeding. World J Gastroenterol 2003; 9(5): 1090-1093
- URL: https://www.wjgnet.com/1007-9327/full/v9/i5/1090.htm
- DOI: https://dx.doi.org/10.3748/wjg.v9.i5.1090
Endoscopic sclerotherapy (ES) and endoscopic variceal ligation (EVL) are well-established nonsurgical procedures for the secondary prevention of bleeding from esophageal varices. EVL, developed by Stiegmann et al[1], has been shown to have lesser complications and also require fewer endoscopy sessions to obliterate esophageal varices[2]. However, EVL is associated with higher variceal recurrence rate in the long term[3-7]. High recurrence rates following EVL could be related to inability to further ligate varices once they became small and had no effect on perforating veins and paraesophageal collaterals[8-10]. The presence of paraesophageal varices predicts the recurrence of esophageal varices and recurrent bleeding[8-10]. The mechanisms of ES and EVL in achieving variceal sclerosis are quite different. The effect induced by EVL is localized to the submucosa, whereas the chemical effect of ES is deeper, i.e. on perforating veins and paraesophageal collaterals[8-10]. We have proposed a new technique of combined endoscopic sclerotherapy and ligation (ESL) in which both techniques of ES and EVL can be optimally utilized to achieve rapid eradication and decreased recurrence of esophageal varices[11]. In this pilot study, we reported our initial experience with this new technique of ESL.
Ten patients (mean age 46.4 ± 7.9 years, ranged 38-60; 9 males, 1 female) with cirrhosis of liver and upper gastrointestinal bleeding underwent ESL for variceal eradication. None of the patients was actively bleeding. The diagnosis of cirrhosis was based on clinical, biochemical and ultrasound findings. All patients had a patent splenoportovenous axis on Doppler ultrasound. The etiology of cirrhosis was related to alcohol in 6 patients, hepatitis B virus in 2, autoimmune hepatitis in 1 and cryptogenic in 1. One patient was in Child’s grade A, 3 in Child’s grade B and 6 patients were in Child’s grade C. All patients received first session of ESL followed by ES alone with 1.5% ethoxysclerol every 2 to 3 weeks.
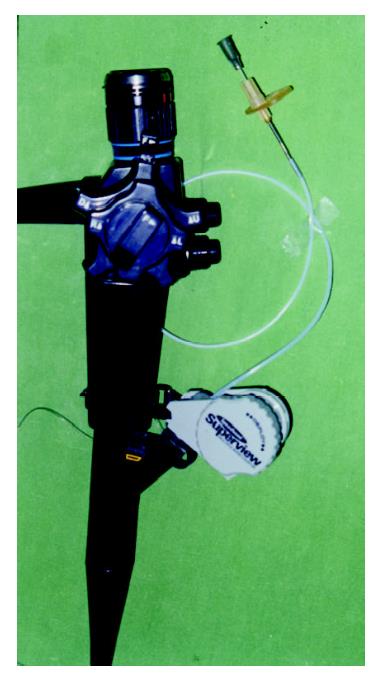
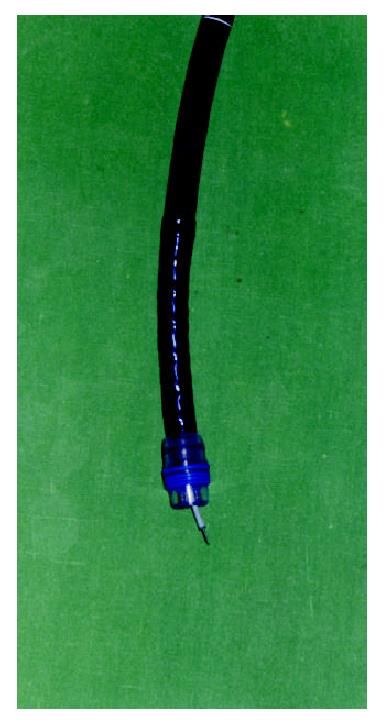
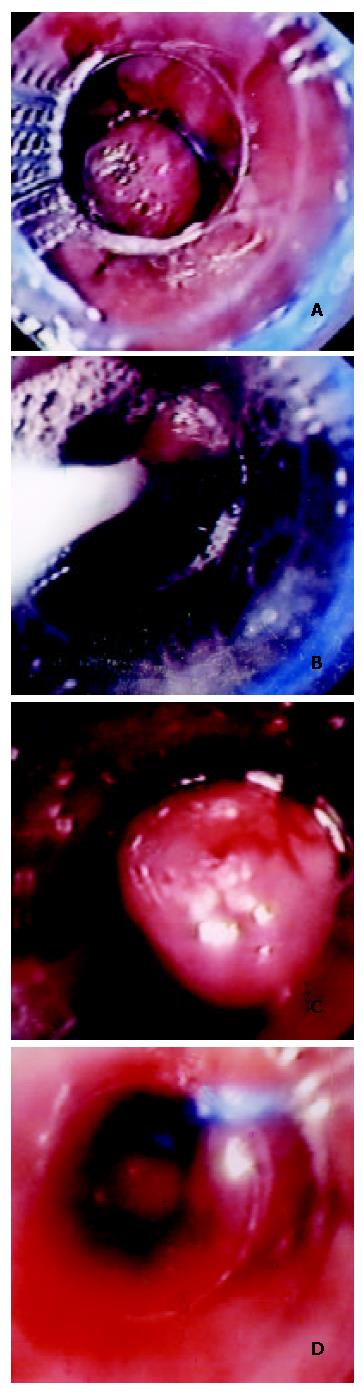
ESL was performed with the Olympus EVIS GIF-Type 100 or OES GIF-XQ20 forward-viewing fiberoptic endoscope and Superview, a multiple band ligator device (Boston Scientific Co., Watertown, MA, USA) and a locally fabricated sclerotherapy needle with an outer diameter of 1.8 mm[12]. The scope was loaded with multiple band ligator devices according to manufacturer’s instructions. A small nick with a sharp, pointed blade was made in the plastic covering near the trip wire of the handle unit for the introduction of the sclerotherapy needle (Figure 1). The sclerotherapy needle was thus passed through the working channel of the scope and could be brought out distally through the cylinder of the ligating unit for ES (Figure 2). The scope was loaded with multiple band ligator device containing 5 or 8 bands, then it was introduced into the esophagus and a single band was applied 5-10 cm proximal to the gastroesophageal junction over the varix starting from proximal to distal margin (Figure 3). This was followed by intravariceal injection of 1.5% ethoxysclerol (4 ml each) 2 to 3 cm proximal to gastroesophageal junction on the ligated varices distal to the deployed bands. The sclerotherapy needle was removed and EVL was then performed at the injection site. Similarly, other varices were also injected and ligated from distal to proximal margin. The scope was then removed after ensuring complete hemostasis.
There was marked reduction in the size of esophageal varices after the ESL; therefore in the subsequent treatment sessions, ES alone was performed with 1.5% ethoxysclerol to eradicate the remaining varices by intravariceal injection method every 2 to 3 weeks. The patients were then followed-up every 3 to 4 months.
All results were showed in Table 1. Eight patients had large esophageal varices (grade 3 or 4) and 2 patients had small (grade 2) varices. Each patient received 1 session of ESL as described. Esophageal varices were eradicated in 9 (90%) patients. Marked reduction in variceal size was found following ESL in all patients on the first follow-up of ES session after 2 to 3 weeks. One patient need not require ES as the varices were completely eradicated after the first session of ESL. Three patients each required 1 and 2 sessions of ES with 1.5% ethoxysclerol, respectively and two patients required 3 ES sessions for complete eradication of esophageal varices. Thus, eradication of varices was achieved in a median of 3 (ESL 1, ESL 2) sessions (range 1-4). None of the patient had procedure-related complications. None of them underwent a "second look" endoscopy after the therapy for evaluation of any symptoms. Large liner superficial ulcers were seen in 3 patients on the first follow-up endoscopy after 2 weeks, which healed uneventfully with marked reduction in variceal size. None of the patient received β-blockers.
| Grade of esophageal varices | Number of patients |
| Grade 3 or 4 | 8 |
| Grade 2 | 2 |
| ESL sessions | 1 |
| Follow-up ES sessions (median, range) | 2 (0-3) |
| Total ESL + ES sessions (median, range) | 3 (1-4) |
| Gastric varices | |
| Before eradication of esophageal varicesa | 1 |
| After eradication of esophageal varices | 0 |
| Portal hypertensive gastropathy | |
| Before | 1 |
| After | 3 |
| Deathb | 2 |
Nine patients, in whom variceal eradication was achieved, were followed-up for a mean of 10.3 months (range 6-15). Small (grade 2) esophageal varices recurred in 1 (11.1%) patient without variceal bleeding. ES was carried out to eradicate the varices again. Two patients died of liver failure. While 1 patient died before the varices could be eradicated, another died during follow-up for 9 months after the eradication of varices. None of the patient died of variceal bleeding.
One patient had large fundal varices with cherry red spots. This patient received undiluted 2.5 ml of intravariceal injection of n-butyl-2-cyanoacrylate into the fundal varices in 2 sessions. Fundal varices disappeared following extrusions of cyanoacrylate cast 3 months later. Mild portal hypertensive gastropathy was present in 1 patient before the eradication of esophageal varices and in 3 patients after the eradication of varices.
We successfully performed this new technique in all patients with cirrhosis of liver, thus showing its efficacy in a clinical setting. Large paraesophageal collaterals on endosonography predict recurrence of esophageal varices[10,13]. We have earlier shown that the ES has an effect on the perforating veins and paraesophageal collaterals as evidenced by reduction in their number and size, while no effect could be demonstrated on these venous structures with EVL[7,8]. In order to reduce the early recurrence of the varices, the present technique aimed at augmenting the effect of sclerosant on perforating veins and on paraesophageal collaterals, while at the same time maintaining the efficacy of EVL to quickly obliterate the esophageal varices.
In this technique, proximal ligation of varices with a band not only interrupts the cephalic variceal blood flow but also divert it into the paraesophageal collaterals via perforating veins, thereby, augmenting the effect of sclerosant on the perforating veins and paraesophageal collaterals or feeders. The effect of this technique may be similar to the technique of ESL used by Umehara et al[4], or the technique of ES used by Takase et al[14] where the effect of sclerosant on feeder vessels of the varices could be increased by interrupting variceal blood flow by inflating the proximal balloon affixed to endoscope. In both the techniques, fluoroscopy was used to confirm the opacification of feeders with sclerosant and contrast mixture. However, our technique was simple and did not require fluoroscopy thereby reducing the radiation exposure to the patient. This method had another advantage. The effectiveness of ES also depended on the time that sclerosant remained in contact with endothelial cells in blood vessels[15]. Proximal ligation of varices in this technique thus increased the effectiveness of sclerosant by increasing the contact time with endothelial cells. After the ES, a band was placed either on the injection site or distal to it, to achieve complete hemostasis and the optimal effect of EVL. The endoscopist however must be careful while negotiating the scope beyond the proximally ligated varices. We did not experience the displacement of proximally deployed band.
If the effect of EVL and ES in this technique is additive then the variceal eradication rate should be higher, the varices should be eradicated in fewer sessions and the recurrence of the varices should be low. In this pilot study, complete eradication of esophageal varices was achieved in 9 (90%) patients in a median of 3 (ESL1, ES2) sessions (range 1-4), while our previous experience with ES alone showed that 6.8 ± 4.9 (mean ± SD) sessions were required to obliterate varices in 45% of patients with cirrhosis of liver[16]. Recurrence of esophageal varices in our previous experience was 25.9%[16]. These results comparing with historical control, indicate that the present technique of ESL is not only effective in reducing the number of sessions for eradication of esophageal varices but also in achieving eradication of varices in a higher proportion of patients. However, prospective, multi-center randomised trials are required to substantiate these results as well as to observe the impact on variceal recurrence with this technique.
ES was done easily without any complication as the injector could be passed though the working channel of the scope. We, however, observed large linear superficial ulcers over the varices on follow-up endoscopy. This finding is not unexpected as the effect of sclerosant is increased by the interruption of the variceal blood flow proximally by a band. These ulcers were superficial and healed without any complication, and were associated with eradication or marked reduction in the variceal size.
In conclusion, our new technique of ESL may be useful in the fast eradication and in achieving lower recurrence of esophageal varices. It, however, requires further randomised controlled trials with EVL or ES to find out its efficacy and impact on the variceal recurrence.
Edited by Xu XQ
| 1. | Van Stiegmann G, Cambre T, Sun JH. A new endoscopic elastic band ligating device. Gastrointest Endosc. 1986;32:230-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 162] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 2. | Laine L, Cook D. Endoscopic ligation compared with sclerotherapy for treatment of esophageal variceal bleeding. A meta-analysis. Ann Intern Med. 1995;123:280-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 500] [Cited by in RCA: 417] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 3. | Hou MC, Lin HC, Kuo BI, Chen CH, Lee FY, Lee SD. Comparison of endoscopic variceal injection sclerotherapy and ligation for the treatment of esophageal variceal hemorrhage: a prospective randomized trial. Hepatology. 1995;21:1517-1522. [PubMed] |
| 4. | Umehara M, Onda M, Tajiri T, Toba M, Yoshida H, Yamashita K. Sclerotherapy plus ligation versus ligation for the treatment of esophageal varices: a prospective randomized study. Gastrointest Endosc. 1999;50:7-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 54] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 5. | Baroncini D, Milandri GL, Borioni D, Piemontese A, Cennamo V, Billi P, Dal Monte PP, D'Imperio N. A prospective randomized trial of sclerotherapy versus ligation in the elective treatment of bleeding esophageal varices. Endoscopy. 1997;29:235-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 97] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 6. | Sarin SK, Govil A, Jain AK, Guptan RC, Issar SK, Jain M, Murthy NS. Prospective randomized trial of endoscopic sclerotherapy versus variceal band ligation for esophageal varices: influence on gastropathy, gastric varices and variceal recurrence. J Hepatol. 1997;26:826-832. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 141] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 7. | Bohnacker S, Sriram PV, Soehendra N. The role of endoscopic therapy in the treatment of bleeding varices. Baillieres Best Pract Res Clin Gastroenterol. 2000;14:477-494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Dhiman RK, Choudhuri G, Saraswat VA, Agarwal DK, Naik SR. Role of paraoesophageal collaterals and perforating veins on outcome of endoscopic sclerotherapy for oesophageal varices: an endosonographic study. Gut. 1996;38:759-764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 47] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Choudhuri G, Srivastava A, Agarwal DK, Dhiman RK. Endosonographic evaluation of venous changes around the gas-troesophageal junction during sclerotherapy and band ligation of varices. Gastroenterology. 1996;110:A1170. |
| 10. | Lo GH, Lai KH, Cheng JS, Huang RL, Wang SJ, Chiang HT. Prevalence of paraesophageal varices and gastric varices in patients achieving variceal obliteration by banding ligation and by injection sclerotherapy. Gastrointest Endosc. 1999;49:428-436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 68] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 11. | Dhiman RK, Chawla YK. Is the technique of endoscopic sclerotherapy and ligation (ESL) optimum. Gastrointest Endosc. 2000;51:639-640. [PubMed] |
| 12. | Dilawari JB, Chawla Y, Locham HS, Prakash S. A low cost endoscopic sclerotherapy needle. Trop Gastroenterol. 1985;6:104-106. [PubMed] |
| 13. | Leung VK, Sung JJ, Ahuja AT, Tumala IE, Lee YT, Lau JY, Chung SC. Large paraesophageal varices on endosonography predict recurrence of esophageal varices and rebleeding. Gastroenterology. 1997;112:1811-1816. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 66] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 14. | Takase Y, Shibuya S, Chikamori F, Orii K, Iwasaki Y. Recurrence factors studied by percutaneous transhepatic portography before and after endoscopic sclerotherapy for esophageal varices. Hepatology. 1990;11:348-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 59] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 15. | Masaki M, Obara K, Suzuki S, Orikasa K, Mitsuhashi H, Iwasaki K, Sakamoto H, Morito T, Kasukawa R. The destructive effects of sclerosant ethanolamine oleate on mammalian vessel endothelium. Gastroenterol Jpn. 1990;25:230-235. [PubMed] |
| 16. | Chawla YK, Dilawari JB, Kaur U. Variceal sclerotherapy in cirrhosis. Indian J Gastroenterol. 1988;7:215-217. [PubMed] |