Published online May 15, 2003. doi: 10.3748/wjg.v9.i5.1082
Revised: August 23, 2002
Accepted: November 4, 2002
Published online: May 15, 2003
AIM: To explore the effect of the classical lay open technique or fistulotomy with the radio frequency surgical device in the treatment of fistula in anus.
METHODS: In our study, the conventional ‘lay open’ technique, or ‘fistulotomy’ was performed by employing the radio frequency surgical device as an alternative to the traditional knife and scissors. In a span of 18 months starting from July 1999 to December 2000, 210 cases with fistula in anus of varied types were operated in our nursing home exclusively applying the radio frequency device.
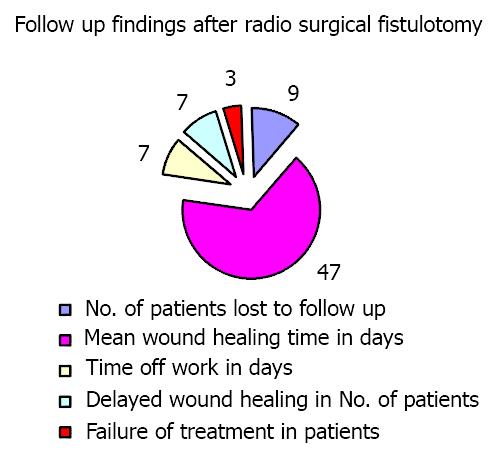
RESULTS: The results of the study were not only encouraging but also were satisfactory. A follow up of the operated patients with radio frequency surgery over a period of 15 months, i.e. from December 2000 to March 2002 was summarized as below: (a) average time taken by the patient to resume routine-7 days; (b) none of the patient had any interference with the continence; (c) the wounds were found healed within an average time of 47 days; (d) delayed wound healing was noticed only in 7 patients; (e) recurrence/failure rate was reduced to as low as 1.5 percent.
CONCLUSION: This technique has been found superior to the conventional fistulotomy in the sense that the time taken for the whole procedure is reduced to almost half, chances of bleeding are reduced to a minimum and the use of suture material is dispensed with. The procedure can safely be called a "Sutureless fistulotomy".
- Citation: Gupta PJ. Radio frequency "sutureless" fistulotomy- a new way of treating fistula in anus. World J Gastroenterol 2003; 9(5): 1082-1085
- URL: https://www.wjgnet.com/1007-9327/full/v9/i5/1082.htm
- DOI: https://dx.doi.org/10.3748/wjg.v9.i5.1082
Fistula in anus is defined as an abnormal communication lined by granulation tissue between the anal canal and the exterior i.e. the skin, which causes a chronic inflammatory response.
The most common cause is secondary to an anorectal abscess. These abscesses either have been treated inadequately, or have bursts spontaneously. Abscess is commonly formed secondary to infection of an anal gland (cryptoglandular hypothesis of Eisenhammer)[1]. Other causes are as follows: (a) Secondary to inflammatory bowel disease- Crohn’s or Ulcerative proctocolitis; (b) Secondary to introduction of a foreign body e.g. probing of an abscess or a low fistula; (c) Associated with anal fissure, i.e. post fissure fistula; (d) Rectum cancer especially the colloid carcinoma.
Causes of multiple fistulae include T.B, Crohn’s disease, ulcerative proctocolitis, lymphogranuloma inguinale, bilharziasis, hidradenitis suppurutiva, etc.
History Patients had the history of seropurulent discharge, persistent pruritus and discomfort in the surrounding skin[2]. Patients feel pain if the fistula tract is blocked for accumulation of secretions under pressure.
Inspection The external opening can usually be seen as an elevation of granulation tissue often active with purulent discharge. The number and location of external openings and the relationships to the anal canal provide a clue as to the internal origin. According to Goodsall’s rule, if the opening is anterior to a transverse anal line (coronal plane), the internal opening will be in a direct radial line to the nearest crypt. If the opening is posterior to the coronal line, the internal opening will usually be in a posterior midline crypt, and the tract will be curved[3]. Exceptions to Goodsall’s rule include anterior openings that are more than 3 cm far from the anal margin and multiple openings. In these situations, the internal opening is more likely to be located in one of the posterior crypts. Other clinical conditions can simulate the appearance of a fistula, including hidradenitis suppurativa, pilonidal sinus, and Bartholin’s gland abscess or sinus[4].
Palpation Palpation may reveal an indurated cord beneath the skin in the direction of the internal opening[5]. Digital anal palpation may reveal a suspicious scarred or retracted crypt. Further internal palpation may reveal posterior or lateral induration, indicating fistulas deep in the postanal space or horseshoe fistulas. Digital rectal examination also provides assessment of sphincter tone and voluntary squeeze pressure, which may indicate the need for preoperative manometry.
Anoscopy It may aid in identifying the internal opening in the anal canal. Massaging the tract may produce a bead of pus at the dentate line. Proctosigmoidoscopy may exclude a proximal internal opening, inflammatory bowel disease, or neoplasia. Colonoscopy is appropriate if the diagnosis of Crohn’s disease is suspected based on a history of recurrent or multiple fistulas or if examination is suggestive of inflammatory bowel disease. A small-bowel series also may be appropriate for patients with recurrent or multiple fistulas.
Fistulography This may have a role in evaluation of recurrent fistula, particularly when the prior surgical procedure has failed to identify the internal opening. The external opening is cannulated with a small caliber feeding tube, and contrast material is gently injected into the tract. X-ray images are then taken in the anteroposterior, oblique, and lateral positions. Complications are rare, and limiting the volume and pressure of contrast injection can minimize patient discomfort. Accuracy rates have been reported to range from 16 to 48 percent, with a false-positivity rate of 10%[6].
Classification There are four main types described: (1) Transphincteric low; (2) Transphincteric high; (3) Supra-levator; and (4) Intersphincteric. However, numerous variations of each can occur[7].
Treatment The classical lay open technique is still the most favoured procedure[8]. Slitting the complete tract from the external to internal opening is the basis of the traditional fistulotomy. Tissues around the external openings and internal opening are excised along with a small margin of tissue lining the tract and the wound is kept open for healing by secondary intention.
The traditional approach is as follows[9]. Preoperative cleansing enema is given. The patient is kept in lithotomic position. Anesthesia: general or regional block is OK. The procedures were as follows: Digital palpation- the tract is felt as nodule or cord. Proctoscopy- a hypertrophied anal papilla may be the point of internal opening. Probing- It is done with delicate hand either retrograde (preferred) or anterograde. Methylene blue dye or milk with hydrogen peroxide is injected from the external opening to locate the direction and path of the tract[10].
A director probe is inserted inside the fistula. Track is cut along probe. Edges of wounds were trimmed and 1-3 mm of tissue margins was removed. The excised tract is sent for histopathological. examination.
This conventional procedure encounters a lot of bleeding from the cut surfaces needing multiple ligatures to tie the bleeding vessels. At times, certain raw areas, which cannot be tied individually, may need under-running also. Due to all these hindrances, the whole procedure becomes somewhat messy and time consuming.
In our study, the radio frequency surgical device was used instead of the surgical knife and scissors. The device is called as the Ellman Dual Frequency 4MHz unit from Ellman International, Hewlett, N.Y.
In a span of 18 months starting from July 1999 to December 2000, 210 cases with fistula in anus of varied types have been operated in our nursing home exclusively employing the aforesaid radio frequency surgery device. There were 187 males and 23 females. The mean age was 37 years old (age range: from 22 to 63 years old). The mean duration of the disease was 19 months (ranging from 4months to 11years). Seventeen patients had an operation for fistula once before and they had a recurrence.
Radio frequency surgery is a technique for cutting and coagulating the tissues using a high frequency alternate current. It is a method of coagulating the tissues, which occurs because of heat produced by the tissue resistance to the passage of high frequency wave. The heat makes the intracellular water boil, increasing the cell inner pressure to the point of breaking it from inside to outside explosion[11]. This phenomenon is called as cellular volatilization. The principle of radio frequency wave surgery is using high frequency radio waves at 4.0 MHz, which delivers low temperature through RF micro-fiber electrodes and is similar to the frequency of marine band radio frequencies. The tissue serves as the resistance instead of the electrode; hence, there is no heating of the RF micro-fiber electrode. Instead, the intracellular tissue water provides the resistance and vaporizes without causing the heat and damage seen in electro surgery. This tissue vaporization also results in significant hemostasis without actually burning the tissue. In addition, there is no danger of shocking or burning the patient. Most important is the fact that there is controlled and minimal lateral tissue damage with the 4.0 MHz high frequency, low temperature radio frequency wave surgery[12].
The unit is provided with a handle to which different electrodes can be attached as per the requirement of the procedure. A ball electrode meant for coagulation, a needle electrode to incise the fistula tract and round loop electrode to shave the surrounding infected tissue has been used in our procedure.
All the patients under study were given to understand the use of the new technique to be employed in the procedure and were clearly explained the potential drawbacks like relapses and need for repetition that may follow. The patients were allowed an option to choose between the conventional method and the radio frequency technique. An informed consent was obtained from them before subjecting them to this new technique.
Only low fistulas having opening below the anus rectal ring were included for study. High trans sphincteric fistulas with or without high blind tract, suprasphincteric, extrasphincteric, and horseshoe fistulas as well as fistulas associated with inflammatory bowel disease were excluded from the study.
The steps in the fistulotomy[13] were the same as described above with the following modifications. (1) Injection of methylene blue dye with hydrogen peroxide. (2) Director probe inserted in the fistula. (3) To begin with, the skin overlying the probe, which is in the fistula tract, was coagulated by moving the ball electrode over its complete length. This reduced the amount of bleeding when the tract is slit opened. (4) The track was cut open along the probe with the help of the needle electrode that was kept in cutting and coagulation mode. This reduced the bleeding while cutting and the dissection became smooth without a drag on the tissues. (5) The bleeding edges were caught in the hemostat and were coagulated with the ball electrode kept in coagulation mode. This avoided need of suturing or under running of the bleeding points and raw areas. (6) The edges along with the surrounding infected, fibrotic tissues were shaved with the loop electrode on cut and coagulation mode. As cutting and coagulation worked simultaneously, the brisk bleeding often encountered in the conventional knife and scissor dissection was avoided. (7) At this stage, we used an accessory called the suction coagulator. This was an accessory supplied with the radio frequency surgical device. This helped in removing the ooze of blood from the raw area while the bleeding points are being coagulated. The use of this additional tool eliminated frequent mopping of the operative field while coagulating the bleeding point, as both could be done simultaneously.
Apart from the main procedure of fistulotomy, this radio frequency surgical device could also be used in coagulating associated skin tags, and internal pile masses if present.
This consisted of dressing the wound twice a day after warm sitz bath. The wound could be covered with sanitary napkin, which helped in mopping up the discharge and kept the wound dry. The patient was required to stay in the hospital for a day or two. Time off work was between 5-7 days after which patient could resume his routine.
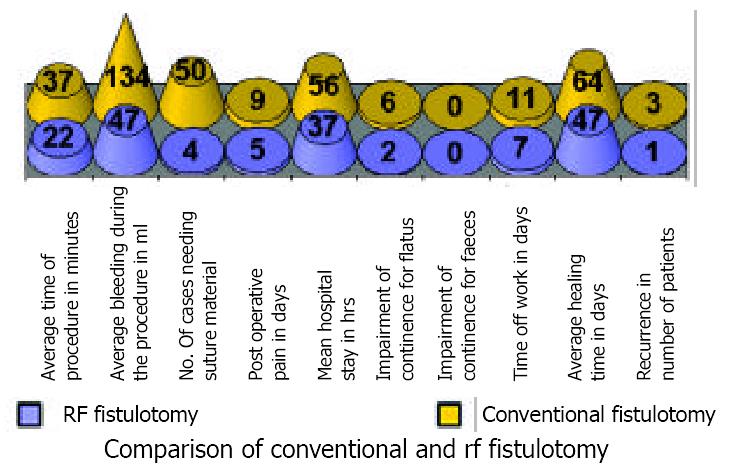
Encouraged by the outcome of the radio frequency fistulotomy, we carried out a separate study. This study was to compare the efficacy of radio frequency surgical fistulotomy over the conventional one. One hundred patients of low anal fistula treated by the classical ‘lay open’ technique were examined. Fifty patients were operated by conventional method, while fifty were operated by radio frequency fistulotomy.
Failure occur mainly due to premature union of the skin edges, failure to excise the internal opening, failure to locate an extra tract, failure to detect a cavity leading upwards from the main tract, presence of foreign bodies and poor post fistulotomy wound care[14]. In our study, the failure rate was as low as 1.5%.
A follow up of the operated patients of fistulotomy with radio frequency surgery over a period of 15 months, i.e. from December 2000 to March 2002 was as follows. None of patients lost during the follow up of 9 days. Average time taken for complete wound healing was 47 days. Average time taken by the patient to resume routine was 7 days. Delayed wound healing happened in 7 patients (took about 80-90 days for complete healing). It was observed that the fistula wounds which were close to the midline, i.e., near 12 or 6’O clock positions when the patient was in lithotomic position took longer time to heal than wounds at other places. The reason possibly could be an excess of stress on the wounds in that situation due to proximity with joints.
Four patients had a premature closure of the proximal wound while the distal remained unhealed. In case of these patients, the healed edges of the proximal wound were slit opened with needle electrode under local anaesthesia. One of them thereafter had an uneventful healing, while the wound remained unhealed in the remaining three.
The remaining three patients continued to have discharge from a small wound left behind, which despite repeated attempts of refreshing the edges remained unresolved. So, they were labeled as cases of ‘failure of wound healing’, rather than of recurrence. Out of these three patients, one patient was from the series of those seventeen patients who came with a recurrence after conventional procedure in the past.
None of these patients had any interference with the continence, anal stenosis, or mucosal prolapse[15].
The data of follow up findings was shown in Figure 1.
No major complications were encountered. Few minor ones were discussed as follows. Deep dissection may cause more scarring and longer time for healing. Excessive power of the unit can cause more smoke and charring. Either accidental burns on the part of the patient or operator due to unintended activation of hand piece has been noted. Development of edema in the surrounding tissue would occur, if power was too high. Excessive discharge from the open wound was found in few patients. This usually happened when the tissues at the base were coagulated in excess.
The comparative data of events obsevered after conventional and radio frequency surgical fistulotomy were shown in Table 1 and Figure 2.
| Events observed | Conventional fistulotomy (n = 50) | Radio frequency surgical fistulotomy (n = 50) |
| Average time of procedure | 37 minutes | 22 minutes |
| Average bleeding during procedure | 134 ml | 47 ml |
| Need of Suture material | 100% | 8% |
| Post operative pain | 9 days | 5 days |
| Hospital Stay [Mean] | 56 hrs | 37 hrs |
| Recurrence/Failure of Treatment | 6% | 2% |
| Time off work | 11 days | 7 days |
| Mean healing time | 64 days | 47 days |
| Impairment of continence | 12% for flatus | 4% for flatus |
Radio frequency surgery, not to be confused with electro surgery, diathermy, spark-gap circuitry, or electrocautry, uses a very high frequency radio frequency wave. Unlike electrocautry or diathermy, the electrode remains cold[16]. This is possible because of use of very high frequency current of 4 MHz, as compared to 0.5 to 1.5 MHz used in the electrocautry. As contrast to true cautery, which causes damage similar to 3rd degree burns, the tissue damage that does occur is very superficial and is comparable to that which occurs with Lasers. Histologically, it has been shown that tissue damage with radio frequency surgery is actually less than with a conventional scalpel and equals cold scalpel[17]. Radio frequency surgery creates minimal collateral heat damage in the tissue resulting in rapid healing and leaves no ugly scar. Biopsies performed of the skin tissue indicate a maximum thickness of heat-denatured collagen to be 75 micrometer. This is equal to or even better than carbon dioxide laser used for cutting[18].
Rapidity of treatment, a nearly bloodless field, minimal postoperative pain, and rapid healing are but few advantages of radio frequency surgery. Once proper technique is established, a scar by this method of treatment is often less pronounced than those produced by other surgical techniques. Excising too deeply increases the likelihood of scars[19].
Removing a lesion on someone who is on aspirin or anticoagulant therapy may be accompanied by increased bleeding.
The unit should not be used in presence of flammable or explosive liquids or gases. The surgeon must also remember to deactivate the hand piece whenever the electrodes are changed[20].
As with all radio frequency surgery machines, smoke is produced, this needs to be attended to avoid the unpleasant smell of burning. This could be achieved by employing a vacuum extractor with the help of the assistant[21].
The various techniques used for treating fistula[22] are fistulectomy, fistulotomy, fistulotomy with marsupialisation[23] of fistula, curettage of fistula and placement of flaps of mucosa or skin, placement of medicated Setons, insertion of antibiotic beads, and injection of commercial or autologous fibrin glue[24]. Out of these options available to the surgeon, majorities of them still rely on the classical lay open technique (fistulotomy) as the gold standard of treatment in over 90% of anal fistula cases[25].
Patients’ satisfaction after the surgical treatment for fistula-in-anus is associated with recurrence of the fistula, the development of anal incontinence, and the effects of anal incontinence on patient lifestyle[26]. The radio frequency surgical technique of fistulotomy has been found more acceptable than the conventional fistulotomy in the sense that the time taken for the whole procedure is reduced to half, bleeding is reduced to a minimum and the use of suture material is dispensed with. None of the patients in our study had any interference with the continence and the recurrence rate was as low as 1.5%.
If compared to electrocautery or laser, the active electrode does not heat up, so there is minimal or no heat generated to the surgical site. This allows the surgeon to work in direct proximity of the functional tissues that needs to be preserved[27].
This technique has been found superior to the conventional and can safely be called a "sutureless fistulotomy".
Edited by Xu XQ
| 1. | Adams D, Kovalcik PJ. Fistula in ano. Surg Gynecol Obstet. 1981;153:731-732. [PubMed] |
| 2. | Vasilevsky CA. Fistula-in-ano and abscess. Fundamentals of anorectal surgery. New York: McGraw-Hill 1992; 131-144. |
| 3. | Seow-Choen F, Nicholls RJ. Anal fistula. Br J Surg. 1992;79:197-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 82] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 4. | Isbister WH. Fistula in ano: a surgical audit. Int J Colorectal Dis. 1995;10:94-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Kuypers JH. Diagnosis and treatment of fistula-in-ano. Neth J Surg. 1982;34:147-152. [PubMed] |
| 6. | Kuijpers HC, Schulpen T. Fistulography for fistula-in-ano. Is it useful? Dis Colon Rectum. 1985;28:103-104. [PubMed] |
| 7. | Parks AG, Gordon PH, Hardcastle JD. A classification of fistula-in-ano. Br J Surg. 1976;63:1-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1072] [Cited by in RCA: 928] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 8. | Kronborg O. To lay open or excise a fistula-in-ano: a randomized trial. Br J Surg. 1985;72:970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 60] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | McLeod RS. Management of fistula-in-ano: 1990 Roussel Lecture. Can J Surg. 1991;34:581-585. [PubMed] |
| 10. | Gingold BS. Reducing the recurrence risk of fistula in ano. Surg Gynecol Obstet. 1983;156:661-662. [PubMed] |
| 11. | Pfenninger JL, Zainea GG. Common anorectal conditions: Part II. Lesions. Am Fam Physician. 2001;64:77-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Plant RL. Radiofrequency treatment of tonsillar hypertrophy. Laryngoscope. 2002;112:20-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 32] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Golighar J, Duthie H, Nixon H. Surgery of the anus rectum and colon. 5thed. London: Bailliere Tindal 1992; 196-197. |
| 14. | Vasilevsky CA, Gordon PH. Results of treatment of fistula-in-ano. Dis Colon Rectum. 1985;28:225-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 53] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Gustafsson UM, Graf W. Excision of anal fistula with closure of the internal opening: functional and manometric results. Dis Colon Rectum. 2002;45:1672-1678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 51] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 16. | Olivar AC, Forouhar FA, Gillies CG, Servanski DR. Transmission electron microscopy: evaluation of damage in human oviducts caused by different surgical instruments. Ann Clin Lab Sci. 1999;29:281-285. [PubMed] |
| 17. | Saidi MH, Setzler FD, Sadler RK, Farhart SA, Akright BD. Comparison of office loop electrosurgical conization and cold knife conization. J Am Assoc Gynecol Laparosc. 1994;1:135-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Bridenstine JB. Use of ultra-high frequency electrosurgery (radiosurgery) for cosmetic surgical procedures. Dermatol Surg. 1998;24:397-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Pfenninger JL, DeWitt DE. Radio frequency frequency surgery. Procedures for primary care physicians. St Louis: Mosby 1994; 91-101. |
| 20. | Valinsky MS, Hettinger DF, Gennett PM. Treatment of verrucae via radio wave surgery. J Am Podiatr Med Assoc. 1990;80:482-488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Inoue Y, Yozu R, Cho Y, Kawada S. Video-assisted thoracoscopy system guidance in linear radiofrequency ablation. Surg Today. 2000;30:811-815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 22. | Belliveau P. Anal fistula. Current therapy in colon and rectal surgery. Toronto: BC Decker 1990; 22-27. |
| 23. | Eu KW. Fistulotomy and marsupialisation for simple fistula-in-ano. Singapore Med J. 1992;33:532. [PubMed] |
| 24. | Abel ME, Chiu YS, Russell TR, Volpe PA. Autologous fibrin glue in the treatment of rectovaginal and complex fistulas. Dis Colon Rectum. 1993;36:447-449. [PubMed] |
| 25. | Ewerth S, Ahlberg J, Collste G, Holmström B. Fistula-in-ano. A six year follow up study of 143 operated patients. Acta Chir Scand Suppl. 1978;482:53-55. [PubMed] |
| 26. | García-Aguilar J, Davey CS, Le CT, Lowry AC, Rothenberger DA. Patient satisfaction after surgical treatment for fistula-in-ano. Dis Colon Rectum. 2000;43:1206-1212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 81] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 27. | Pfenninger JL. Modern treatments for internal haemorrhoids. BMJ. 1997;314:1211-1212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |