Published online Nov 15, 2003. doi: 10.3748/wjg.v9.i11.2519
Revised: April 1, 2003
Accepted: April 11, 2003
Published online: November 15, 2003
AIM: To understand the influence of Kupffer cell (KC) on signal transduction pathways in the liver.
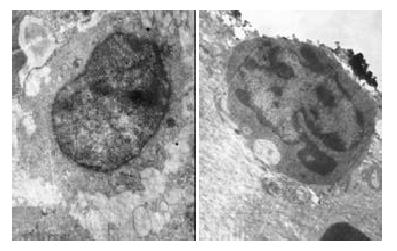
METHODS: To decrease selectively the number and function of KC, Kunming mice were ip injected with a single dose of gadolinium chloride (GdCl3, 20 mg•kg-1), the time-effect relationship assessment was performed after 1 d, 3 d and 6 d. sALT, sGST, liver glycogen content, phagocytic index, and expression of CD68 were assessed as the indexes of hepatotoxicity and functions of KC respectively, and morphology of KC was observed with transmission electron microscopy. Furthermore, cAMP, PGE2 level, nitric oxide (NO) content, and mRNA expression of NFkappaBp65, Erk1, STAT1 were examined.
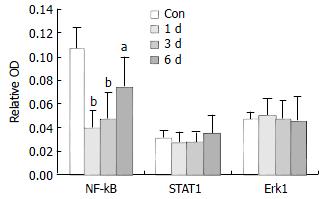
RESULTS: GdCl3 could selectively cause apoptosis of KC and obvious reduction of KC’s activity, but no hepatotoxicity was observed. One day after KC blockade, NO, PGE2, cAMP contents in the liver were reduced 21.0%, 6.94-fold, 8.3%, respectively, and mRNA expression of NFkappaBp65 was decreased 3.0-fold. The change tendency of NO, PGE2, and cAMP contents and mRNA expression of NFkappaBp65 were concomitant with recovery of the functions of KC. The contents of NO, PEG2, cAMP were increased when the functions of KC was recovered. However, all of the changes could not return to the normal level except NO content after 6 d Gdcl3 treatment. No obvious changes were found in STAT1 and Erk1 mRNA expression in the present study.
CONCLUSION: Hepatic NO, PGE2, cAMP level and mRNA expression of NFkappaBp65 are closely related with the status of KC. It suggests that KC may play an important role in the cell to cell signal transduction in the liver.
- Citation: Ding H, Huang JA, Tong J, Yu X, Yu JP. Influence of Kupffer cells on hepatic signal transduction as demonstrated by second messengers and nuclear transcription factors. World J Gastroenterol 2003; 9(11): 2519-2522
- URL: https://www.wjgnet.com/1007-9327/full/v9/i11/2519.htm
- DOI: https://dx.doi.org/10.3748/wjg.v9.i11.2519
Kupffer cells (KCs) account for a major portion of the tissue macrophages and play an important role in the defense mechanisms of the body[1]. KCs are involved in the pathogenesis of chemically mediated liver injury through release of biologically active mediators that promote the pathogenic process[2]. KCs can synthesize and release a variety of immuno-modulating and inflammatory mediators such as oxygen-derived free radicals, nitric oxide, lipid mediators, and cytokines, etc. There are certain points to be elucidated that KCs involve in the pathophysiologic response of liver injury[3]. And now, many new functions have been found. KCs can reverse liver fibrosis and are critical for the progression of alcoholic injury[3,4]. Abolishment of KCs sensitization could prevent alcoholic liver injury[5]. KCs are major contributors to cytokine production in hepatic ischemia/reperfusion[6] and play a stimulatory role in liver regeneration[7]. Up to now, few studies about the influence of KCs on signal transduction in the liver have been reported. NO, PGE2, cAMP are important second messengers transmitting and magnifying messages to modulate gene expression. NFkappaB, STAT, Erk are important nuclear transcription factors, which are involved in the regulation of cell proliferation and differentiation[8,9]. To understand the effect of KCs on the second messengers and nuclear transcription factors is of great importance in studying the mechanism of liver diseases. Gdcl3, as an inhibitor of KCs, is often used as a tool for studying the role of KC[10]. Kupffer cell toxicant GdCl3 prevents stellate cell activation and the development of fibrosis[11]. The present study was designed to clarify the effect of KC on signal transduction pathway in the liver following GdCl3-induced KC blockade.
Gadolinium chloride (GdCl3), collagenase IV, Indian ink were purchased from Sigma, USA. NO, PGE2 detection kits were obtained from Bangding Biotechnology Co., Ltd. cAMP detection kit was obtained from Shanghai College of Chinese Traditional Medicine. CD68 immunohistochemical kit and NFkappaBp65, STAT1, Erk1 in situ hybridization kit were purchased from Wuhan Boster Biological Technology Co., Ltd. Other reagents were all of A.R.
Kunming ♂mice (aged 4-6 wk), weighing 22 ± 3 g were obtained from the Experimental Animal Center of School of Medicine, Wuhan University. The animals were fed on a standard diet in pellets, and allowed free access to water. The mice were randomly distributed to control group, GdCl3-1 d group, GdCl3-3 d group, GdCl3-6 d group, in which the mice received ip injection of a single dose of 20 mg·kg-1 of GdCl3, and were sacrificed after administration of GdCl3 for 1 d, 3 d, 6 d, respectively.
14% Indian ink (10 mL·kg-1) was injected into the mice tail vein. After 1 min and 5 min, 20 μL blood was obtained from the orbital vein of the mice and added into 2 mL of 0.1% Na2CO3 solution. Absorbance (OD) at 600 nm was read, and the phagocytic activity (α) of KCs was calculated as described[12].
Twenty-five percent liver homogenate was prepared, the glycogen content was quantified by an enzymatic reaction as previously described[13]. NO content was measured by Griess reaction[14]. PGE2 and cAMP concentration were determined by radioimmunoassay, and the radioactivity of the samples was measured with a P△CK△RD CA-2000 liquid scintillation spectrometer[15]. The protein content of liver homogenate was determined by Lowry[16].
The livers were briefly washed in cold 0.1 M phosphate buffer containing 0.1% DEPC and then fixed in cold 4% formaldehyde (in 0.1 M phosphate buffer, pH7.4), paraffin-embedded sections in 5-6 μm thickness were cut and placed onto aminopropyltriethoxysilane-coated glass slides. The expression of CD68 was determined by in situ hybridization with DIG detection system kit. The anti-sense sequence of the probe was 5’-AAGCTTGGCCCAAGCCACCTTGGTTTTAGA-3’ for Erk1 (extracellular signal-regulated kinase), 5’-CAGGTTGTCTGTGGTCTGAAGTCTAGAAGG-3’ for STAT1 (signal transducers and activators of transcription), 5’-AGTTGATGTCCGCAATGGAGGTCTT-3’ for NF-κBp65 (nuclear factor kappa B p65).
Microscopic images through an interference filter (Nikon, Tokyo, Japan) were transferred to the processor (HPIAS image analysis system, Wuhan Tongji Medical University). Average absorbances in defined areas of the sections were measured, relative optical density (OD) was used to evaluate expression level.
Liver cells were isolated as described[17]. In brief, after washed in D-Hanks, liver tissue was digested with 0.075% collagenase for 30 min. The resulting suspension was passed through 70 μm gaze and then 1 g of sediment was generated after 10 min. Hepatocytes were fixed in 2.5% glutaraldehyde in 0.1 mol•L-1 phosphate buffer, transmission electron- microscope was used to observe the morphology of KCs.
The data were presented as ¯x ± s, and statistical analysis was performed with Student’s t-test.
After administration of GdCl3, no changes in sALT, sGST level and liver glycogen content were observed. Liver expression of CD68 (specific surface antigen of macrophage) and phagocytic activity (α) obviously reduced 102%, 86% respectively after 1 d of GdCl3 treatment, then the function of KCs was gradually recovered. However they could not return to the normal level after 6 d of GdCl3 treatment.
The characteristics of apoptosis (the membrane of KCs was integrate, chromatin in the nucleus presented uneven distribution and was close to nuclear measure) were observed after treatment of GdCl3 (Figure 1).
After 1 d of GdCl3 treatment, NO, PGE2, cAMP contents were reduced 21.0%, 6.94-fold, 8.3%, respectively, and then they were gradually recovered. However, PGE2 and cAMP contents could not return to the normal level after 6 d of treatment.
The time course of alteration of NFkappaB, STAT1 and Erk1 mRNA expressions after administration of 20 mg•kg-1 GdCl3 showed that NFkappaB mRNA expression was decreased (3-fold) after administration of GdCl3 for 1 d, then it was gradually recovered, but did not return to the normal level after 6 d of treament. No obvious influence on STAT1, Erk1 mRNA expressions was observed (Figure 2).
In the present study, ip injection of a single dose of GdCl3 could selectively cause apoptosis of KCs, but did not induce hepatotoxicity. Therefore, it can be used as a tool for studying the role of KCs.
KCs are the phagocytic macrophages in the liver. NO, PGE2, and cAMP could transmit and magnify extracellular messages to cells through a cascade system to regulate gene expression and cell proliferation and differentiation[18]. NO, PGE2, and cAMP had different functions in hepatoprotection and hepatic injury. NO from KCs could induce membrane barrier dysfunction in liver sinusoid[19]. But according to Abou-Elella et al[20], the exacerbation of hepatocyte death by KCs was not related to NO. Hsu et al[21-23], sproposed that KCs be the major source of induction of inducible NO synthase (iNOS) activity and NO production have a beneficial role in hepatic IR injury and the constitutive isoforms of NOS play a hepatoprotective role in hepatic injury. The protective function of NO against hepatic injury might lie in that it could reduce tissue oxygenation[24]. PGE2 derived from KCs increased cAMP, which caused triglyceride accumulation in the liver and fatty liver[3]. Increase of cAMP levels in KCs occurred during the late stage of polymicrobial sepsis, and might contribute to the depression of macrophage phagocytic function[25]. The current study showed that NO, PGE2, and cAMP contents in the liver were reduced following KC blockade, and recovered following the functional recovery of KCs. It suggests that Kupffer cells may mediate signaling of second messengers in the liver. Moreover, in the present experiment, the hepatic function did not change following the alterations of NO, PGE2, and cAMP content, the reasons remain to be researched.
It has widely been accepted that NFkappaB activation plays an important role in the pathophysiology of inflammatory disorders[26]. NFkappaB is an essential component of TNF proliferative pathway and TNF-induced changes in IL-6 mRNA, STAT3, and c-myc mRNA are dependent on NFkappaB activation[27]. NFkappaB activation may be important in "switching off" the cytokine cascade during acute pancreatitis[28]. The current study showed that mRNA expression of NFkappaB in the liver was down-regulated after KC blockade, suggesting that KCs may play an important role in mediating liver diseases and inflammatory disorders via changes of the signal transduction pathway in the liver.
In this experiment, STAT1 and Erk1 mRNA expressions were not affected by GdCl3. STAT1 played a harmful role in Con A-mediated hepatitis, whereas STAT3 protected against liver injury[29]. Inhibition of STAT1 activation without reduction of STAT1 protein level might be one of the factors that are involved in the cAMP-dependent stellate cell growth arrest[30]. In this study, we only examined the expression of STAT1 mRNA, the relationship between STAT1 and hepatic injury needs to be further studied.
Edited by Zhu LH and Wang XL
| 1. | Fukumura D, Yonei Y, Kurose I, Saito H, Ohishi T, Higuchi H, Miura S, Kato S, Kimura H, Ebinuma H. Role in nitric oxide in Kupffer cell-mediated hepatoma cell cytotoxicity in vitro and ex vivo. Hepatology. 1996;24:141-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Luckey SW, Petersen DR. Activation of Kupffer cells during the course of carbon tetrachloride-induced liver injury and fibrosis in rats. Exp Mol Pathol. 2001;71:226-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 112] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 3. | Enomoto N, Ikejima K, Yamashina S, Enomoto A, Nishiura T, Nishimura T, Brenner DA, Schemmer P, Bradford BU, Rivera CA. Kupffer cell-derived prostaglandin E (2) is involved in alcohol-induced fat accumulation in rat liver. Am J Physiol Gastrointest Liver Physiol. 2000;279:G100-G106. [PubMed] |
| 4. | Sakaida I, Hironaka K, Terai S, Okita K. Gadolinium chloride reverses dimethylnitrosamine (DMN)-induced rat liver fibrosis with increased matrix metalloproteinases (MMPs) of Kupffer cells. Life Sci. 2003;72:943-959. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 41] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 5. | Enomoto N, Takei Y, Hirose M, Ikejima K, Miwa H, Kitamura T, Sato N. Thalidomide prevents alcoholic liver injury in rats through suppression of Kupffer cell sensitization and TNF-alpha production. Gastroenterology. 2002;123:291-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 68] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Mosher B, Dean R, Harkema J, Remick D, Palma J, Crockett E. Inhibition of Kupffer cells reduced CXC chemokine production and liver injury. J Surg Res. 2001;99:201-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 88] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 7. | Takeishi T, Hirano K, Kobayashi T, Hasegawa G, Hatakeyama K, Naito M. The role of Kupffer cells in liver regeneration. Arch Histol Cytol. 1999;62:413-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 68] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 8. | Liu DY, Gorrod JW. Effects of cAMP-dependent protein kinase and ATP on N1-oxidation of 9-benzyladenine by animal hepatic microsomes. Life Sci. 2000;66:77-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Wheeler MD, Kono H, Rusyn I, Arteel GE, McCarty D, Samulski RJ, Thurman RG. Chronic ethanol increases adeno-associated viral transgene expression in rat liver via oxidant and NFkappaB-dependent mechanisms. Hepatology. 2000;32:1050-1059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Neyrinck A, Eeckhoudt SL, Meunier CJ, Pampfer S, Taper HS, Verbeeck RK, Delzenne N. Modulation of paracetamol metabolism by Kupffer cells: A study on rat liver slices. Life Sci. 1999;65:2851-2859. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 21] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Rivera CA, Bradford BU, Hunt KJ, Adachi Y, Schrum LW, Koop DR, Burchardt ER, Rippe RA, Thurman RG. Attenuation of CCl (4)-induced hepatic fibrosis by GdCl (3) treatment or dietary glycine. Am J Physiol Gastrointest Liver Physiol. 2001;281:G200-G207. [PubMed] |
| 12. | Joseph B, Malhi H, Bhargava KK, Palestro CJ, McCuskey RS, Gupta S. Kupffer cells participate in early clearance of syngeneic hepatocytes transplanted in the rat liver. Gastroenterology. 2002;123:1677-1685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 108] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 13. | Renau-Piqueras J, Guasch R, Azorín I, Seguí JM, Guerri C. Prenatal alcohol exposure affects galactosyltransferase activity and glycoconjugates in the Golgi apparatus of fetal rat hepatocytes. Hepatology. 1997;25:343-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Bartholomew B. A rapid method for the assay of nitrate in urine using the nitrate reductase enzyme of Escherichia coli. Food Chem Toxicol. 1984;22:541-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 105] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 15. | Hahn PY, Yoo P, Ba ZF, Chaudry IH, Wang P. Upregulation of Kupffer cell beta-adrenoceptors and cAMP levels during the late stage of sepsis. Biochim Biophys Acta. 1998;1404:377-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | LOWRY OH, ROSEBROUGH NJ, FARR AL, RANDALL RJ. Protein measurement with the Folin phenol reagent. J Biol Chem. 1951;193:265-275. [PubMed] |
| 17. | Nanni G, Majorani F, Maloberti G, Canepa C, Casu A. Action of chronic CC14 on the retinol and dolichol content of rat liver parenchymal and non-parenchymal cells. Life Sci. 2000;67:2293-2304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | O'Dell TJ, Hawkins RD, Kandel ER, Arancio O. Tests of the roles of two diffusible substances in long-term potentiation: evidence for nitric oxide as a possible early retrograde messenger. Proc Natl Acad Sci USA. 1991;88:11285-11289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 657] [Cited by in RCA: 690] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 19. | Fukumura D, Yonei Y, Kurose I, Saito H, Ohishi T, Higuchi H, Miura S, Kato S, Kimura H, Ebinuma H. Role in nitric oxide in Kupffer cell-mediated hepatoma cell cytotoxicity in vitro and ex vivo. Hepatology. 1996;24:141-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Abou-Elella AM, Siendones E, Padillo J, Montero JL, De la Mata M, Muntané Relat J. Tumour necrosis factor-alpha and nitric oxide mediate apoptosis by D-galactosamine in a primary culture of rat hepatocytes: exacerbation of cell death by cocultured Kupffer cells. Can J Gastroenterol. 2002;16:791-799. [PubMed] |
| 21. | Hsu CM, Wang JS, Liu CH, Chen LW. Kupffer cells protect liver from ischemia-reperfusion injury by an inducible nitric oxide synthase-dependent mechanism. Shock. 2002;17:280-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 63] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 22. | Liu TH, Robinson EK, Helmer KS, West SD, Castaneda AA, Chang L, Mercer DW. Does upregulation of inducible nitric oxide synthase play a role in hepatic injury. Shock. 2002;18:549-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 23. | Rhee JE, Jung SE, Shin SD, Suh GJ, Noh DY, Youn YK, Oh SK, Choe KJ. The effects of antioxidants and nitric oxide modulators on hepatic ischemic-reperfusion injury in rats. J Korean Med Sci. 2002;17:502-506. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 24. | Koti RS, Seifalian AM, McBride AG, Yang W, Davidson BR. The relationship of hepatic tissue oxygenation with nitric oxide metabolism in ischemic preconditioning of the liver. FASEB J. 2002;16:1654-1656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 47] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 25. | Hahn PY, Yoo P, Ba ZF, Chaudry IH, Wang P. Upregulation of Kupffer cell beta-adrenoceptors and cAMP levels during the late stage of sepsis. Biochim Biophys Acta. 1998;1404:377-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 26. | Renard P, Raes M. The proinflammatory transcription factor NFkappaB: A potential target for novel therapeutical strategies. Cell Biol Toxicol. 1999;15:341-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 74] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 27. | Kirillova I, Chaisson M, Fausto N. Tumor necrosis factor induces DNA replication in hepatic cells through nuclear factor kappaB activation. Cell Growth Differ. 1999;10:819-828. [PubMed] |
| 28. | Murr MM, Yang J, Fier A, Gallagher SF, Carter G, Gower WR, Norman JG. Regulation of Kupffer cell TNF gene expression during experimental acute pancreatitis: the role of p38-MAPK, ERK1/2, SAPK/JNK, and NF-kappaB. J Gastrointest Surg. 2003;7:20-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 65] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 29. | Hong F, Jaruga B, Kim WH, Radaeva S, El-Assal ON, Tian Z, Nguyen VA, Gao B. Opposing roles of STAT1 and STAT3 in T cell-mediated hepatitis: regulation by SOCS. J Clin Invest. 2002;110:1503-1513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 202] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 30. | Kawada N, Uoya M, Seki S, Kuroki T, Kobayashi K. Regulation by cAMP of STAT1 activation in hepatic stellate cells. Biochem Biophys Res Commun. 1997;233:464-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |