Published online Oct 15, 1998. doi: 10.3748/wjg.v4.iSuppl2.45
Revised: August 9, 1998
Accepted: September 4, 1998
Published online: October 15, 1998
AIM: The study was aimed at the unknown mechanisms of gastroin testinal symptoms and accompanied malnutrition in patients following partial gastrectomy.
METHODS: Thirty-six patients who had their gastric resection at least five years ago and forty-one normal controls were included in the study. Nutritional status as indicated by anthropometry measurements, glucose hydrogen breath test G-HBT) before and after antibiotic treatment and mouth-cecum trans it time (MCTT) with lactose hydrogen breath test (L-HBT) were simultaneously determined. The Student’s t test was used for statistical analysis of all the data of the study.
RESULTS: Anthropometry measurements showed that decreased values (at least 10% lower than the ideal values) of body weight (BW), triceps skinfol d thickness (TSF) and mid-arm circumference (MC) were observed in 63.2%, 94.7 % and 73.3% of the patients studied respectively. A positive result of 50g G-H HBT was seen in 10 cases out of 26 patients (38.5%) who were undertaken the test. Six of the 9 patients with negative 50 g G-HBT were positive following a 80 g G-HBT. Hydrogen excretion in six patients with positive 50 g or 80 g G-BHT were significantly decreased after antibiotic treatment. Further studies of 25 L-BHT showed a significant difference of MCTTs either between the post-gastrectomy patients with or without chronic diarrhea, or between patient and control groups, i.e. an average MCTT of 58.8, 85.7 and 105.9 min in each group.
CONCLUSION: Malnutrition was common in patients a few years aft er their gastrectomies. About forty percent of positive G-HBT, and effective antibiotic treatment and reduced MCTT determination were observed in these patients. The results suggested that bacterial overgrowth and increased small bowel transit may play a role in the development of gastrointestinal symptoms and related malnutrition in patients following gastrectomy.
- Citation: Zheng JJ, Zhu XS, Wang YM. Breath hydrogen determination in patients following partial gastrectomy. World J Gastroenterol 1998; 4(Suppl2): 45-48
- URL: https://www.wjgnet.com/1007-9327/full/v4/iSuppl2/45.htm
- DOI: https://dx.doi.org/10.3748/wjg.v4.iSuppl2.45
Malnutrition with gastrointestinal symptoms including chronic diarrhea has been commonly observed in patients following partial gastrectomy. However, the causes of the symptoms and accompanied malutrition are obscure[1,2]. The present study was aimed at the target of unknow etiology of the entity using the method of breath hydrogen determination which has been well demonstrated as an indicator of carbohydrate malabsorption and also widely used for diagnosing bacterial overgrowth or dertermining small bowel transit time.
Thirty-six patients who had their gastric resection (partial gastrectomy) at least five years ago were included in the investigation. Forty-one healthy medical students and hospital staffs as control were included in the study.
A detailed history was taken and physical examination were performed for each patient and control subject. Indications for gastric surgery were stomach carcinoma, pepticulcer diseases and their complications including massive upper gastrointestinal bleeding. Pre-and post operatiively body weights were recorded.
Body weight (BW) as percent of ideal weight, tripeps skinfold thickness (TSF) and Mid-arm circumference (MC) were determined and normalized using age-and sex-specific reference tables of healthy Chinese adults[3-5].
Breath excreation tests with glucose challenge were performed using the protocol as below: each patient and volunteer was first asked to have a dose of 50 g glucose (in 250 mL of warm water) (50 g G-HBT), and then H2 was collected and determined at every 30 min interval as the method reported by Kotler, Metz and Kings et al[6-9]. The model CM2 Microlyzer (Quin Tron Instrument Co. Inc., Milwaukee, Wisc. United States.) was used for H2 determinations.
Both peak H2 concentration and its time of occurrence and cumulative H2 excretion after glucose ingestion were recorded. The later indicator was estimated by calculating the area under the curve of H2 concentration against time, with the following equation for the sum of the areas of consecutive trapezoids. A = (1/2H1 + H2 + H3 + … + Hn-1 + 1/2Hn) × t. Where A stands for area, H stands for breath H2 concentration in ppm (parts per million) and t is 30 min.
A further 80 g of glucose challenge (80 g G-HBT) was given next morning if the 50 g G-HBT showed a negative result, i.e. H2 excretion was increased less than 20 ppm within 2 h after glucose ingestion. When 80 g G-HBT showed a negative result again, the study would be finished and was considered as a normal result. Antibiotic (terramycin 0.5 g four timese very 6 h and metronidazole 0.2 g three times a d for a total of 3 d) were given orally for three d when 50 or 80 g of glucose loading showing a positive result, i.e. breath H2 excretion increased at least 20 ppm more than fast H2 concentration. A positive bacterial overgrowth (BOG) in the upper part of the small bowel was suggested only if HBT returned negative or there was a significant decrease of H2 excretion after antibiotics adminitration. The patients stools studied were all cultured and found no growth of pathogenic organisms. For normal controls, only 50 G-HBTs was performed.
Lactose malabsorption was also determined among the patients and volunteers next morning following G-HBT, or at least three d later if antibiotics were given during the study. The method using hydrogen breath test was as previously described[10,11]. A positive result with lactose malabsorption was defined as H2 output after 25 g of lactose loading increased 20 ppm higher than the fast level.
Transit time using 25 g L-HBT was only measured in patients and volunteers who had been document as lactose malabsorbers according to the criterion mentioned above. The time elapsing between lactose ingestion and the earliest 20 ppm rise of exhaled H2 was considered to represent MCTT of the lactose column as it passed through the small bowels[1,6,10].
Twenty-six patients with definite midical records were divided without diarrhea . Postprandial bloating and abdominal distention were seen in 8 cases, and brobo rygmus in 4 cases. Only 3 patients showed no significant gastrointestinal symptoms.
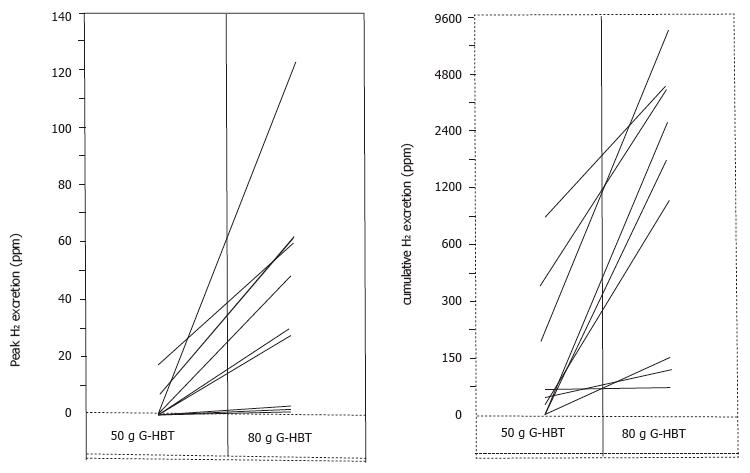
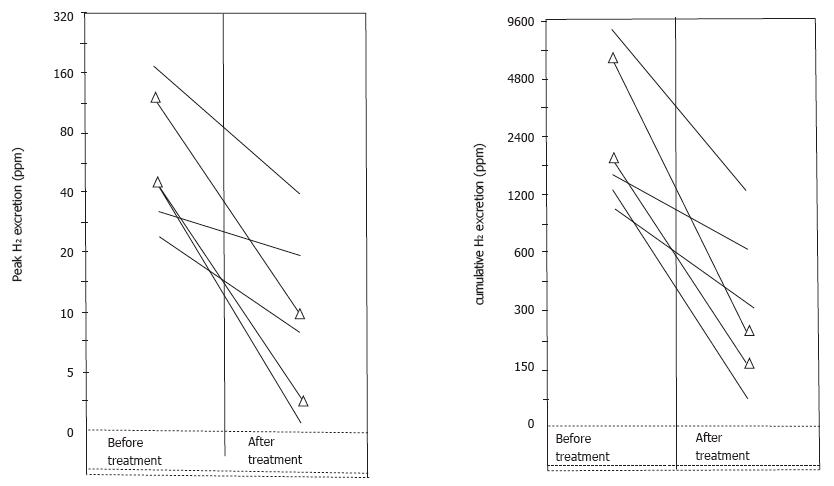
Anthropometrical measurements were taken in 19 out of above 36 patients, and most patients including non-diarrhea group showed lower results, i.e. BW. TSF and MC as expressed at least 10% lower than ideal value were seen in 63.2 (12/19 ), 94.7 (18/19) and 73.3% (14/19) respectively (Table 1). 50 g G-HBT were performed in all 36 patients and were positive in 10 cases (27.8%), including 4 with diarrhea and 6 without diarrhea. Nine patients with negative results of 50 g G-HBT were tested again with 80 g glucose. Six of the 9 patients became positive according to both peak and cumulative H2 concentration determinations (Figure 1). In addition, Hydrogen excretions in six patients with positive results following either 50 g or 80 g of glucose loading were significantly decreased after antibiotics treatment (Figure 2). The symptoms of diarrhea, postprandial distention or borborygmus were all obviously improved. All six normal controls showed a negative result of 50 g G-HBT.
| % of ideal value Nutritional status | > 90 | 80-90 | 60-80 | < 60 |
| Normal | Malnutrition | |||
| Mild | Moderate | Severe | ||
| BW | ||||
| Diarrhea (n = 7) | 3 | 3 | 1 | 0 |
| Non-diarrhea (n = 12) | 4 | 5 | 3 | 0 |
| TSF | ||||
| Diarrhea (n = 7) | 1 | 0 | 1 | 5 |
| Non-diarrhea (n = 12) | 0 | 0 | 1 | 11 |
| MC | ||||
| Diarrhea (n = 7) | 1 | 5 | 1 | 0 |
| Non-diarrhea (n = 12) | 4 | 4 | 4 | 0 |
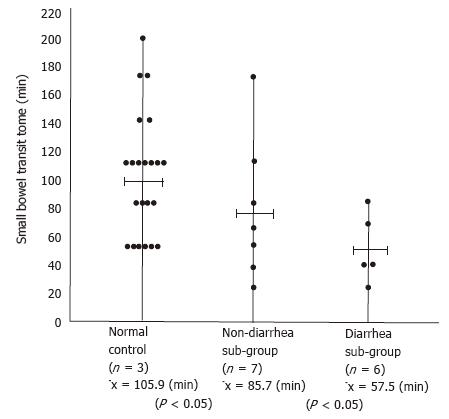
Twenty-five g L-HBTs were performed in fourteen patients, and H2 excretion after lactose loading was significantly increased (more than 20 ppm) in thirteen patients with a positive rate of 92.3% (13/14) in contrast to 78% (32/41) of the normal voluteers (P < 0.05). MCTTs were determined in all above thirteen latose malabsorbers. Six with permanent diarrhea had a 57.5 s of transit time. However, the rest seven without diarrhea and normal volunteers had 85.7 and 105.9 s respectively (Figure 3). Statistical analysis showed a significant difference between the two sub-groups and also between the patients and normal groups (P < 005).
Malnutrition and accompanied gastrointestinal symptoms have been paid much attention in patients following partial gastrectomy, and were usually attributed to factors such as accelerated transit time, and bacterial overgrowth through the small intestine, and poor mixing of nutrients with digestive enzymes due to a reduced gastric surface following gastrectomy ect[1,2]. The present study using HBT method documented a result consistent with the above hypothesis[1,2]. The results showed that malnutrition in patients following partial gastrectomy was common, i.e., most of the patients have decreased BW, TSF and MC value as compared to the reference table (Table 1). However, gastrointestinal symptoms including chronic diarrhea were only observed in less than one third of the patients. The fact that most of these malnourished patients have no remarkable clinical symptoms may further exacerbate their nutritional status, and therefore, a high incidence of malnutrition was observed in these gastrectomized patients in the investigation.
Though a few hypothesis it was proposed that the pathophysiology of this type of malnutrition is unclear[1,2]. The 50 and 80 g G-HBT in the present study revealed more than one third of gastrectomized patients have increased H2 excretion following glucose challenge. Interestingly, H2 excretion in six patients had a remarkable decrease with clinical improvements after antibiotic treatment (Figure 2). The results appeared to suggest a possible mechanism of bacterial overgrowth in the development of malnutrition and related gastrointestinal symptoms in the patients studied. However, there was no statistical difference of the occurrence of bacterial overgrowth between the sub-groups with or without chronic diarrhea. In combination with the fact that the anthropometric measurements were not different between these two sub-groups, we hypothesized that the mechanism of the entity must be multifactored or individualized in different patients.
The study of 25 g L-HBT showed an accelerated SBTT (58.6 min) in diarrhea subgroup, as compared to 85.7 and 105.9 min in non-diarrhea patients and normal volunteers (Figure 3), indicating an altered MCTT may play a important role in addition to the BOG mechanism in the occurrence of diarrhea. Further more in the present study, a much higher incidence of lactose malabsorption which may reflect a lower quantity of lactase in the gut was seen in gastrectomized patients than in normal controls, and most interestingly all the patients with diarrhea were fallen into the positive group of 25 g L-HBT. All these facts that suggested a poor mixing of nutrients with digestive enzymes may participate in the development of chronic diarrhea and finally malnutrition after gastric resection.
We also obtained an increased positive result of HBT using 80 g glucose challenge (Figure 1). The result was were consistent with the conclusion that 80 g G-HBT may be a more sensitive and useful procedure than 50 g G-HBT for BOG diagnosis[9].
Supported in part by a research grant from the Suzhou Municipal Bureau of Public Health.
The hydrogen microanalyser was kindly a gift of Dr. Irwin H. Rosenberg (The University of Chicago, and now Tufts University, United States).
E- Editor: Li RF
| 1. | Kotler DP, Sherman D, Bloom SR, Holt PR. Malnutrition after gastric surgery. Association with exaggerated distal intestinal hormone release. Dig Dis Sci. 1985;30:193-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | King CE, Toskes PP, Ahmed EP, Hardy ER. The 80 gram glucose-hydrogen breath test: a quick alternatives to the urine xylose screening test. Gastroenterology. 1983;84:1208. |
| 3. | Both JH, Levitt MD. Use of breath hydrogen (H2) to quantitate small bowel transit time following partial gastrectomy. J Lab Clin Med. 1997;9:30-36. |
| 4. | Bond JH, Levitt MD. Use of breath hydrogen (H2) to quantitate small bowel transit time following partial gastrectomy. J Lab Clin Med. 1977;90:30-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 118] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 5. | Shao JZ. Evaluation of nutritional status. In Shao (ED): Intravenous Alimentation Therapy Ed. 1, Shanghai: Shanghai Scientific and Technological Press, Shanghai 1984; 130-138. |
| 6. | Li SH. An investigation on the normal value of the body weights for adults with different heights in North China. Yingyang Xuebao. 1986;8:98-108. |
| 7. | Wang HM, Wang HM, Zhao JT. A study on the standards for upper arm muscle circumference and other anthropometric parameters in healthy Chinese. Yingyang Xuebao. 1986;8:70-74. |
| 8. | Kotler DP, Holt PR, Rosensweig NS. Modification of the breath hydrogen test: increased sensitivity for the detection of carbohydrate malabsorption. J Lab Clin Med. 1982;100:798-805. [PubMed] |
| 9. | Isaacs PE, Kim YS. Blind loop syndrome and small bowel bacterial contamination. Clin Gastroenterol. 1983;12:395-414. [PubMed] |
| 10. | Yap I, Berris B, Kang JY, Math M, Chu M, Miller D, Pollard A. Lactase deficiency in Singapore-born and Canadian-born Chinese. Dig Dis Sci. 1989;34:1085-1088. [PubMed] |
| 11. | Solomons NW, Rosenberg IH. Breath-analysis tests in clinical nutrition and gastroenterology. Clin Gastroenterol. 1978;2:21-25. |
| 12. | Zheng JJ. Rosenberg IH. Lactose malabsorption in healthy Chinese adults. Shipin Yu Yingyang Shengtaixue. 1984;15:1-6. |