Published online Mar 7, 2024. doi: 10.3748/wjg.v30.i9.1154
Peer-review started: November 11, 2023
First decision: December 15, 2023
Revised: December 23, 2023
Accepted: February 8, 2024
Article in press: February 8, 2024
Published online: March 7, 2024
Processing time: 115 Days and 16.9 Hours
Inflammatory bowel disease (IBD) was previously regarded as a Western disease; however, its incidence is increasing in the East. The epidemiology of IBD in Asia differs significantly from the patterns in the West.
To comprehensively investigate the epidemiology of IBD in South Korea, inclu
We analyzed claims data from the Health Insurance Review and Assessment Service and Rare and Intractable Diseases (RIDs), operated by the National Health Insurance Service of South Korea. Patients with IBD were identified based on the International Classification of Diseases, Tenth Revision, and RID diagnostic codes for Crohn’s disease (CD) and ulcerative colitis (UC) from 2010 to 2018.
In total, 14498 and 31409 patients were newly diagnosed with CD and UC, respectively, between 2010 and 2018. The annual average incidence of CD was 3.11 cases per 105 person-years, and that of UC was 6.74 cases per 105 person-years. Since 2014, the incidence rate of CD has been stable, while that of UC has steadily increased, shifting the peak age group from 50-year-olds in 2010 to 20-year-olds in 2018. The CD and UC prevalence increased consistently over the study period; the use of 5-aminosalicylates and corticosteroids gradually decreased, while that of immunomodulators and biologics steadily increased in both CD and UC. The clinical outcomes of IBD, such as hospitalization and surgery, decreased during the study period.
The CD incidence has been stable since 2014, but that of UC has increased with a shift to a younger age at peak incidence between 2010 and 2018. IBD clinical outcomes improved over time, with increased use of immunomodulators and biologics.
Core Tip: Inflammatory bowel disease (IBD) was previously regarded as a Western disease; however, its incidence is increasing in the East, with a different epidemiological pattern. This nationwide cohort study analyzed claims data from South Korea between 2010 and 2018. The incidence of ulcerative colitis increased continuously, particularly among younger demographic groups, during this period, whereas the incidence of Crohn’s disease remained stable from 2014. Additionally, in this period, hospitalization and surgery rates for IBD decreased as the use of immunomodulators and biologics increased.
- Citation: Kim S, Lee HJ, Lee SW, Park S, Koh SJ, Im JP, Kim BG, Han KD, Kim JS. Recent trends in the epidemiology and clinical outcomes of inflammatory bowel disease in South Korea, 2010-2018. World J Gastroenterol 2024; 30(9): 1154-1163
- URL: https://www.wjgnet.com/1007-9327/full/v30/i9/1154.htm
- DOI: https://dx.doi.org/10.3748/wjg.v30.i9.1154
Inflammatory bowel disease (IBD), which includes Crohn’s disease (CD) and ulcerative colitis (UC), is a chronic relapsing inflammatory disease of the gastrointestinal tract. Although it was previously regarded as a Western disease, its incidence has increased in newly industrialized countries, including South Korea, since the start of the twenty-first century[1,2].
South Korea is a representative Asian country in which the incidence and prevalence of IBD are rapidly increasing[1]. According to a longitudinal population-based study conducted in the Songpa-Kangdong (SK) district of Seoul, South Korea, the incidence rates of both CD and UC have rapidly increased since the first diagnosis of a patient with IBD in Korea in 1986 (from 0.06/105[3] inhabitants/year in 1986-1990 to 2.44/105 inhabitants/year in 2011-2015 for CD, and from 0.29/105 inhabitants/year in 1986-1990 to 5.82/105 inhabitants/year in 2011-2015 for UC)[4]. Several nationwide population-based studies have investigated the epidemiology of IBD in South Korea[3,5,6]. Jung et al[3] reported the average annual incidence of UC and CD to be 5.0 and 2.8 per 105 person-years, respectively, from 2011 to 2014, and Kwak et al[6] reported that both the prevalence and incidence of CD and UC showed an increase between 2007 and 2016 (1.9-fold and 1.2-fold increase in the prevalence and incidence of CD, respectively, and 1.6-fold and 1.3-fold increase in the prevalence and incidence of UC, respectively). However, despite the previous epidemiological data on IBD in South Korea, studies on recent trends are still lacking. Furthermore, although the clinical course of IBD has changed due to the recent introduction of various new therapeutic agents, there are very few demographic studies on its clinical outcomes.
The current study aimed to explore the incidence and prevalence of IBD using a nationwide population-based cohort from the National Health Insurance Service (NHIS) database and to investigate the temporal changes in medication and clinical outcomes of IBD in South Korea.
The NHIS is a mandatory nationwide insurance system operated by the government that covers approximately 97% of the entire population of South Korea. It contains medical claims data, including patient demographics, principal diagnosis, and comorbidities, using the International Classification of Disease 10th revision (ICD-10) codes and prescriptions, admissions, and procedures[7]. All the information from the NHIS is integrated into the Health Insurance Review and Assessment Service (HIRA) claims database, which is a comprehensive data source for epidemiological studies in South Korea[3,5,6].
The NHIS established the Rare and Intractable Disease (RID) registration program in 2006 to provide a medical copayment reduction of 10% to patients with RIDs, including IBD. To register in this program and obtain a special code (V code), patients must obtain diagnostic approval from a physician based on the strict diagnostic criteria defined by the NHIS[5]. Because it is directly related to the government’s support for medical expenses, RID registration is conducted strictly to ensure a high reliability in RID diagnosis.
The current retrospective nationwide cohort study used claims data from HIRA and RIDs (operated by the NHIS) and was approved by the Seoul National University Hospital Institutional Review Board (1806-060-949). Because there are no personal identifiers, informed consent was waived.
Patients diagnosed with IBD between 2010 and 2018 were included in this study. To establish an accurate definition for identifying patients with IBD, we compared two different definitions: one defined patients with IBD using only ICD-10 codes, whereas the other used both ICD-10 and V codes. Finally, we identified patients with CD as those with both ICD-10 code K50 and RID code V130 and patients with UC as those with ICD-10 code K51 and RID code V131. The diagnostic accuracy of each definition for identifying patients with IBD was assessed using data from the SK-IBD study in which all IBD cases were strictly identified through a medical record review conducted by two experts[4].
The following information was collected from the HIRA claims database: date of diagnosis, comorbidities, prescription records, and IBD-related clinical outcomes, including emergency room (ER) visits, hospitalizations, and surgery.
IBD-related medications included 5-aminosalicylates (5-ASA), immunomodulators (azathioprine or 6-mercaptopurine), systemic corticosteroids (including both oral and intravenous corticosteroids), and biologics (infliximab, adalimumab, vedolizumab, ustekinumab, or tofacitinib), prescribed at least once, along with the diagnostic codes. ER visit was defined as a visit to the ER for a primary diagnosis of IBD. Hospitalization was defined as an admission for ≥ 3 d with the principal diagnosis of IBD. Surgery was defined as resection of the small bowel, colon, or rectum in patients diagnosed with IBD.
The annual incidence of IBD was defined as the number of newly diagnosed cases of IBD per 105 individuals in the respective year, based on the registered resident population for that year. Prevalence was defined as the number of patients with IBD per 105 person-years based on the registered resident population for that year. Incidence and prevalence were calculated for different age and sex groups, and each value was expressed as the number of cases per 105 person-years.
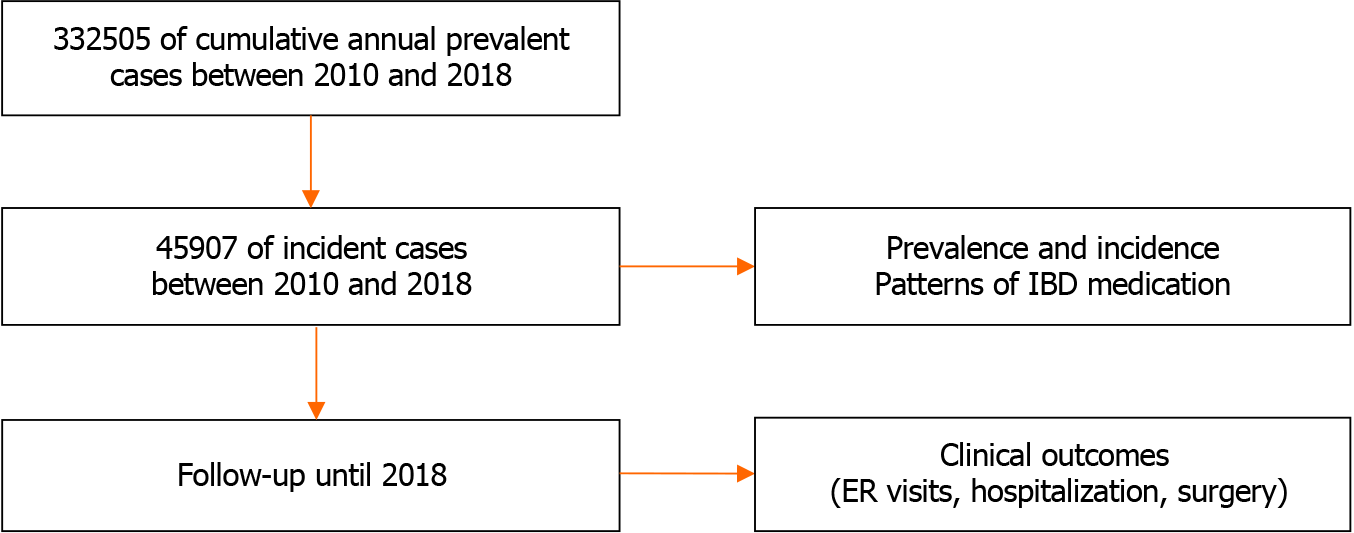
Trends in IBD-related prescriptions and clinical outcomes, including ER visits, hospitalization, and surgery, between 2010 and 2018 were examined. Trends in prescriptions and clinical outcomes were described based on the number of patients who were prescribed IBD-related medications or had an ER visit, hospitalization, or surgery annually. Statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, United States) and R version 3.4.3 (The R Foundation for Statistical Computing, Vienna, Austria). Figure 1 provides an overview of the study’s selection process.
To assess the accuracy of the diagnostic definitions, we identified patients with IBD from the healthcare data of the SK district, using only ICD-10 codes or both ICD-10 codes and V-codes, and compared them with the published results of the SK-IBD study from 2011 to 2015[4]. Compared to using ICD-10 and V codes for identifying patients with IBD, using only ICD-10 codes overestimated the incidence and prevalence (mean annual incidence rate per 105 inhabitants: 17.34 for CD and 109.05 for UC). However, when V-codes were applied in addition to the ICD-10 codes, the results (mean annual incidence rate per 105 inhabitants: 3.79 for CD and 7.40 for UC) were similar to the incidence rates reported in a previous study for the SK district (mean annual incidence rate per 105 inhabitants: 2.44 for CD and 5.82 for UC) (Supplemen
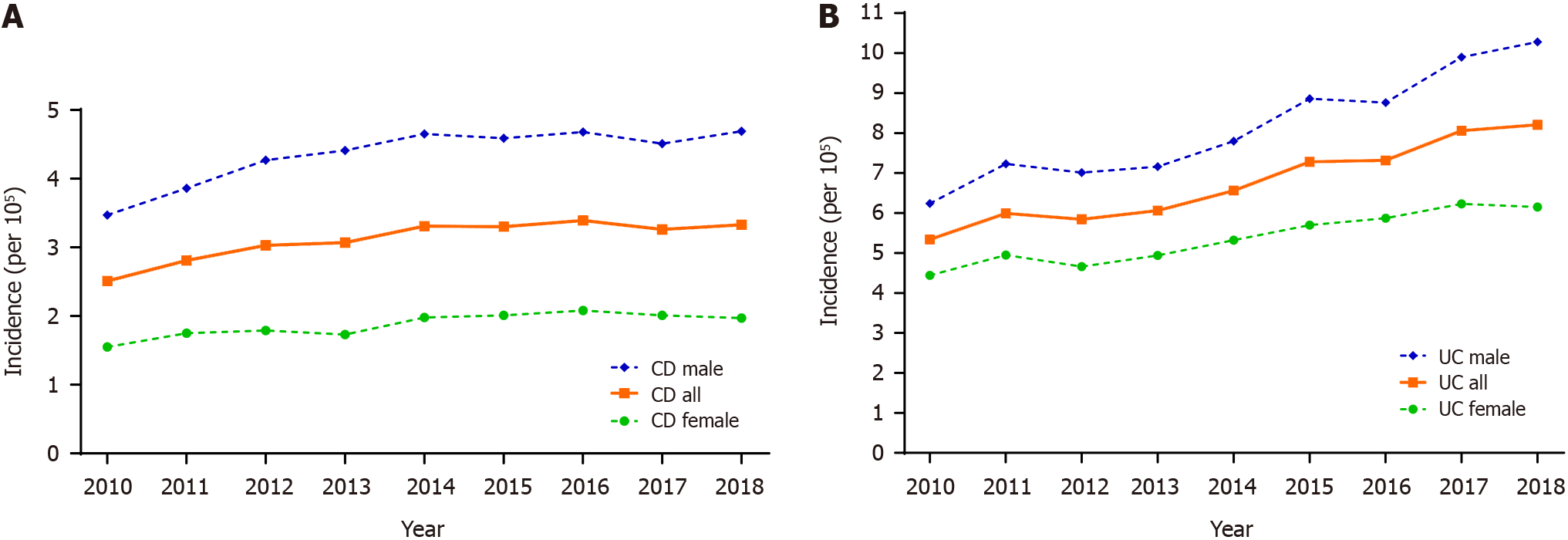
Between 2010 and 2018, 45907 patients were newly diagnosed with IBD; specifically, 14498 (31.6%) and 31409 (68.4%) patients were diagnosed with CD and UC, respectively. Table 1 and Figure 2 present the incidence of IBD in South Korea between 2010 and 2018. The mean annual incidence rates during the study period were 3.1 per 105 and 6.7 per 105 for CD and UC, respectively. The incidence of UC increased steadily throughout the study period from 5.3 to 8.2 per 105 between 2010 and 2018, with an annual increase of approximately 0.4%. Meanwhile, the incidence of CD increased from 2.5 to 3.3 per 105 between 2010 and 2014 and remained relatively stable thereafter at approximately 3.3 per105. In 2018, the UC-to-CD incidence ratio was 2.5.
| Year of diagnosis | |||||||||
| 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | |
| CD | |||||||||
| No. of incident cases | 1271 | 1431 | 1552 | 1581 | 1717 | 1718 | 1770 | 1709 | 1749 |
| Incidence rate1 | 2.51 | 2.81 | 3.03 | 3.07 | 3.32 | 3.30 | 3.39 | 3.26 | 3.33 |
| Male | 3.47 | 3.86 | 4.27 | 4.41 | 4.65 | 4.59 | 4.68 | 4.51 | 4.69 |
| Female | 1.55 | 1.75 | 1.79 | 1.73 | 1.98 | 2.01 | 2.08 | 2.01 | 1.97 |
| M/F ratio | 2.24 | 2.20 | 2.38 | 2.54 | 2.35 | 2.28 | 2.25 | 2.25 | 2.38 |
| UC | |||||||||
| No. of incident cases | 2701 | 3050 | 2987 | 3116 | 3397 | 3788 | 3826 | 4227 | 4317 |
| Incidence rate1 | 5.34 | 5.99 | 5.84 | 6.06 | 6.56 | 7.28 | 7.32 | 8.06 | 8.21 |
| Male | 6.24 | 7.03 | 7.01 | 7.16 | 7.80 | 8.86 | 8.76 | 9.89 | 10.28 |
| Female | 4.44 | 4.95 | 4.66 | 4.94 | 5.32 | 5.70 | 5.87 | 6.23 | 6.15 |
| M/F ratio | 1.41 | 1.42 | 1.50 | 1.50 | 1.47 | 1.56 | 1.49 | 1.59 | 1.67 |
| UC/CD ratio | 2.13 | 2.13 | 1.92 | 1.97 | 1.98 | 2.20 | 2.16 | 2.47 | 2.47 |
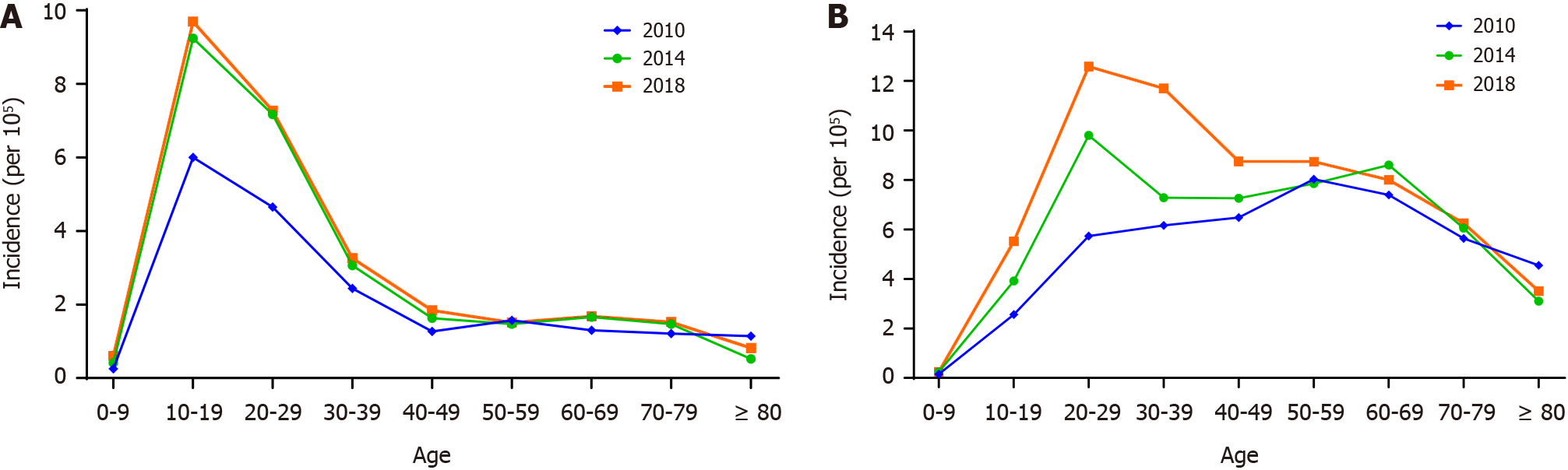
Age-specific incidence rates showed different patterns for CD and UC throughout the study period (Figure 3). For CD, the peak incidence was observed in individuals aged 10-19 years. The incidence rate remained relatively high in the 20-29-year-olds but decreased significantly after age 30, exhibiting a consistent pattern over time. In contrast, there was a shift in the peak incidence age for UC, decreasing from 50-59 years in 2010 to 20-29 years in 2018.
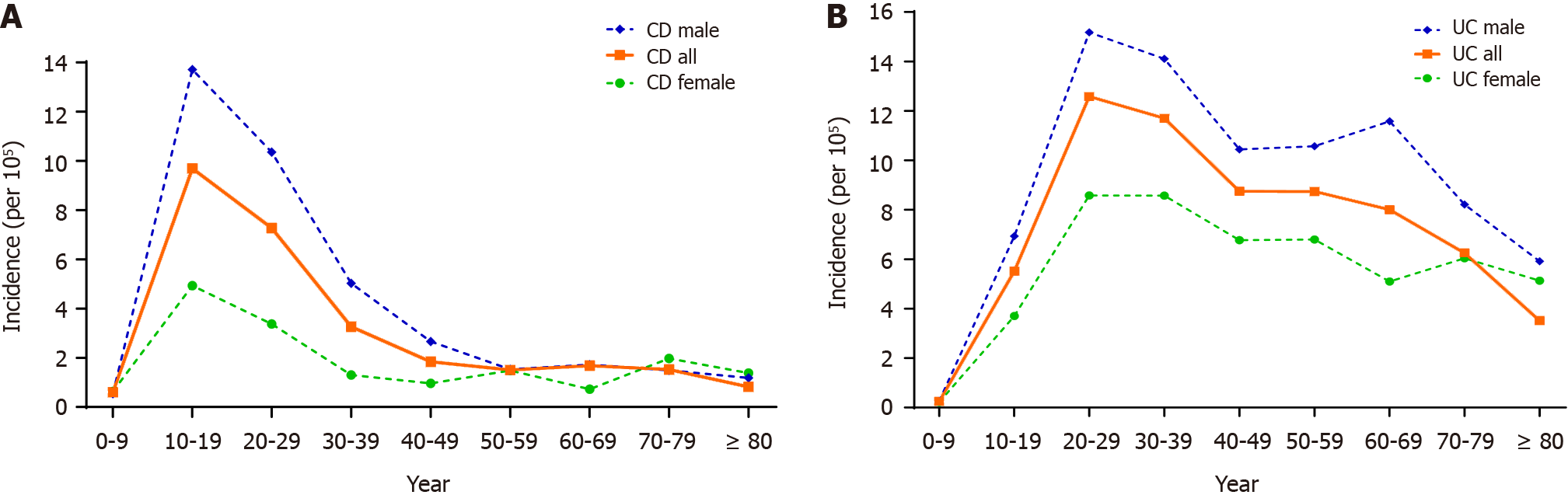
Both CD and UC showed higher incidence rates in men than in women over the study period, with sex differences being more prominent in patients with CD than in those with UC. In 2018, the male-to-female ratios for CD and UC were 2.4 and 1.7, respectively. Additionally, age- and sex-specific incidence rates demonstrated distinct patterns for CD and UC in 2018 (Figure 4). The peak incidence of CD occurred in patients aged 10-19 years in both men and women. In contrast, while the incidence of UC peaked in the 20-29-year-olds for both men and women, the second peak incidence of UC was observed only in males in the 60-69-year-old age group.
The prevalence of IBD steadily increased between 2010 and 2018, reaching 17168 and 34420 patients with CD and UC, respectively, in 2018. CD and UC showed more than double the prevalence over the study period, from 15.1 per 105 in 2010 to 32.7 per 105 in 2018 for CD, and from 31.6 per 105 in 2010 to 65.5 per 105 in 2018 for UC. The prevalence rate was higher in men than in women for both CD and UC, with a greater sex difference observed, especially for CD; the values were 46.8 per 105 in men and 18.5 per 105 in women for CD, and 77.1 per 105 in men and 53.9 per 105 in women for UC (Supplementary Figure 1). Furthermore, the prevalence of IBD increased in all age groups throughout the study period. The peak prevalence of CD occurred in the 20-29-year-old age group, whereas that of UC occurred in the 60-69-year-old age group, which was consistent for both men and women (Supplementary Figures 2 and 3).
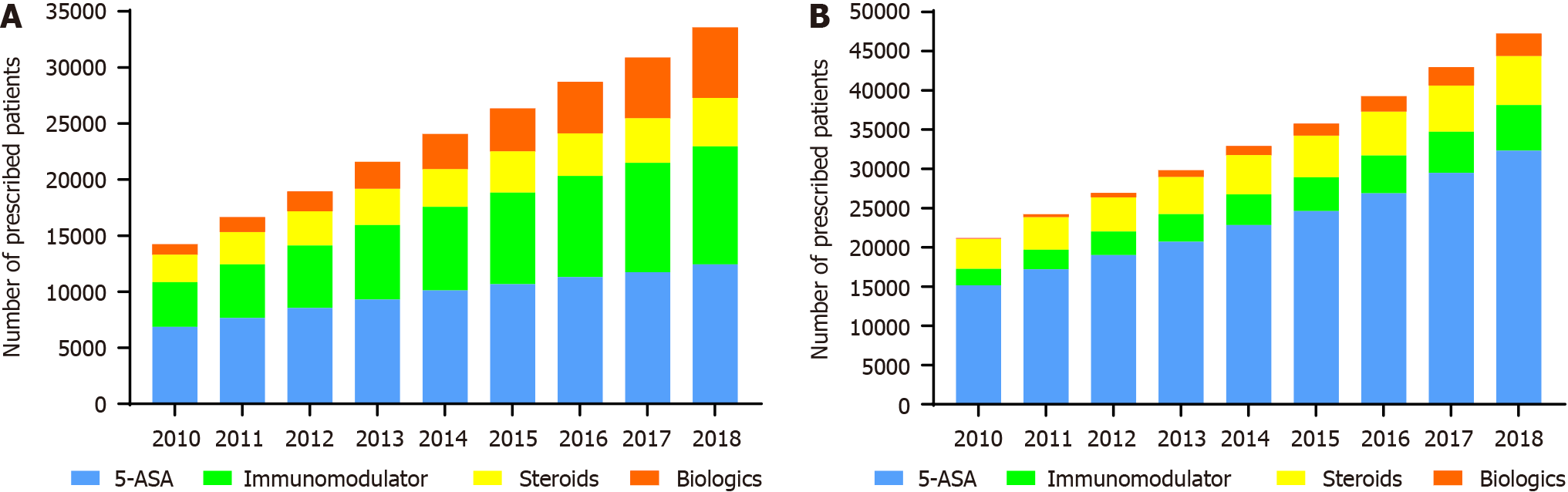
5-ASA, immunomodulators, systemic corticosteroids, and biologics were administered to 12435 (72.4%), 10516 (61.3%), 4323 (25.2%), and 6278 (36.6%) patients with CD, respectively, in 2018. In the UC group, 5-ASA was administered to almost all patients (32323; 93%), whereas immunomodulators, systemic corticosteroids, and biologics were administered to 5789 (16.8%), 6271 (18.2%), and 2822 (8.2%) patients, respectively.
Figure 5 shows the temporal changes in the use of IBD medications between 2010 and 2018. The number of patients using immunomodulators and biologics increased in both the CD and UC groups during the study period. In patients with CD, the use of immunomodulators increased from 52.1% in 2010 to 61.3% in 2018, and that of biologics increased from 11.9% in 2010 to 36.6% in 2018. Moreover, in patients with UC, the use of immunomodulators increased from 13.1% in 2010 to 16.8% in 2018, whereas that of biologics increased from 0.7% in 2010 to 8.2% in 2018. Conversely, the use of steroids decreased during the same period, from 32.1% in 2010 to 25.2% in 2018 for CD and from 23.8% in 2010 to 18.2% in 2018 for UC. Finally, the use of 5-ASA decreased from 87.9% in 2010 to 72.4% in 2018 in CD while remaining relatively unchanged in UC patients throughout the study period.
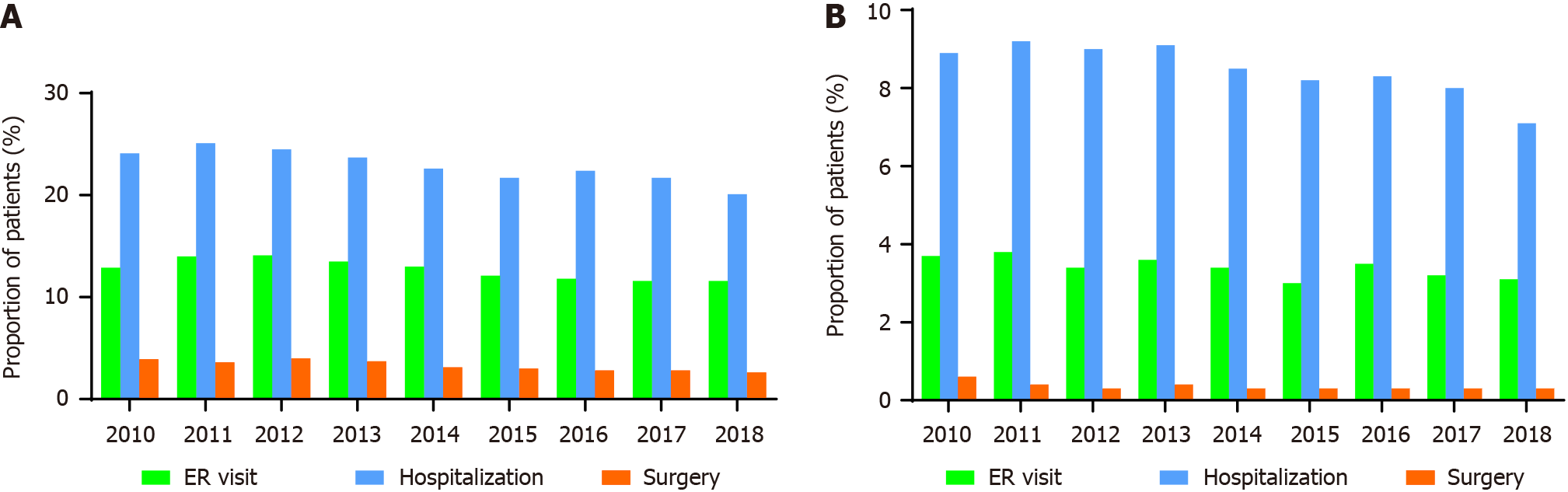
Figure 6 shows the trend in IBD outcomes, including IBD-related ER visits, hospitalizations, and surgeries, between 2010 and 2018. In 2018, 1991 (11.6%) and 1081 (3.1%) patients with CD and UC, respectively, visited the ER at least once with a diagnosis of IBD. The rate of ER visits did not change significantly during the study period.
A total of 3448 (20.1%) and 2440 (7.1%) patients with CD and UC, respectively, were hospitalized in 2018. The hospitalization rates for CD and UC showed a decreasing trend during the study period, from 24.1% in 2010 to 20.1% in 2018 for CD and from 8.9% in 2010 to 7.1% in 2018 for UC.
Regarding surgery, 399 patients with CD (2.3%) and 42 patients with UC (0.1%) underwent bowel resection for complications related to IBD in 2018. The surgery rate for patients with CD decreased from 3.4% in 2010 to 2.3% in 2018. Regarding UC, there was a decreasing trend in the surgery rate, from 0.4% in 2010 to 0.2% in 2014; however, it remained relatively unchanged thereafter.
This nationwide population-based study investigated the comprehensive epidemiological data on IBD in South Korea from 2010 to 2018. To the best of our knowledge, this was the first study to analyze the epidemiology of IBD in an Asian population, considering medication use and IBD-related clinical outcomes, such as ER visits, hospitalizations, and surgeries. Throughout the study period, the incidence of UC increased continuously, with a shift towards the younger age group, whereas that of CD plateaued from 2014 onwards. Furthermore, patients with more recently diagnosed IBD showed higher use rates of immunomodulators and biologics and lower rates of hospitalization and surgery.
The average annual incidence rates of IBD in this study from 2010 to 2018 were 3.1 per 105 for CD and 6.7 per 105 for UC, comparable to the findings of previous studies conducted in Korea using the nationwide HIRA database. In such studies, the incidence of CD and UC ranged from 2.6 to 3.2 per 105 people and from 4.3 to 5.3 per 105 people, respectively, during 2005-2016[3,5,6,8]. The incidence of IBD in the present study was lower than that in North America (Olmsted County, Minnesota; the incidence of CD was 10.7 per 105 people and that of UC was 12.2 per 105 people) and Europe (Denmark; incidence of CD was 9.1 per 105 people and that of UC was 18.6 per 105 people)[9,10]. However, this was the highest estimate among Asian countries, representing the economic advancement and Westernization of society with rapid industrialization in Korea[11,12].
Remarkably, the incidence of UC increased continuously over the entire study period, whereas that of CD plateaued from 2014 onwards. Although the SK cohort study showed an increased incidence of IBD, the increase has slowed down recently[4]. Moreover, recent studies using a nationwide database have reported the incidence of IBD to have plateaued or even decreased[3,5,6]. The global evolution of IBD could explain this trend; IBD in Korea has recently accelerated through the incidence stage to the stage of compounding prevalence[2]. Unlike other industrialized countries in Asia that experienced a rising incidence of IBD in the 2020s, Korea and Japan transitioned into an accelerated incidence stage earlier owing to rapid industrialization[6,13]. Studies with more recent data may show a trend toward a decrease or plateau in incidence. Importantly, our study included the most recent data from previous epidemiological studies in Korea and confirmed a stabilizing incidence and an increasing trend in the prevalence of IBD. Longitudinal studies with long-term follow-ups would be necessary to evaluate the transition of this epidemiological stage accurately.
One of the interesting findings of this study was the shift in the peak age of UC incidence to a younger age, which changed from individuals in their 50 s to those in their 20 s, during the study period. This trend has also been observed in several previous studies in Korea[6,8,14]. Although the exact reason for this shift is still unclear, changes in dietary habits and lifestyle factors may be linked. Furthermore, the increased frequency of eating out and using delivered food, especially among young people, and the rise in coffee and sugar-sweetened beverage consumption, could play a role[15,16]. Moreover, reduced exposure to green areas and increased time spent in urban living and working environments may have contributed to this trend[17,18]. Finally, with improved access to healthcare over the past few decades, the rate of endoscopic examinations among young people may have increased, leading to a higher rate of early diagnosis of UC[19]. Further studies are recommended to elucidate the underlying reasons for this trend.
Another interesting finding of this study was that the rates of hospitalization and surgery in patients with IBD decreased over the study period, in line with the increased use of immunomodulators and biologics. Temporal changes in IBD outcomes following the use of new therapeutic agents have been addressed in previous studies. In a hospital-based cohort study of patients with UC, conducted in Korea between 1986 and 2015, the rates of hospitalization and surgery decreased over time; in particular, the rate of surgery significantly decreased after the introduction of anti-tumor necrosis factor agents[20]. A meta-analysis of 44 population-based cohort studies revealed a decreasing trend in the risk of surgery, which was significantly lower in patients diagnosed in the 21st century than in those diagnosed in the 20th century for both CD and UC[21].
The ER visits and hospitalization rates in this study were comparable to those reported in previous Korean studies[3,20]. However, the surgery rate was much lower than that in previous studies[7,21,22]. This discrepancy could be attributed to differences in the methods used to calculate the surgery rate. Two Western studies have reported that the risk of surgery is highest within the first 1 or 2 years after the diagnosis of UC, and one South Korean study has reported that the rate of surgery is low between 5 and 10 years after the diagnosis of UC, increasing slightly thereafter[20,23,24]. Our current study analyzed the rate of surgery in patients with IBD each year, irrespective of the time of diagnosis, so it did not reflect the cumulative probabilities of surgery after IBD diagnosis. Furthermore, considering that previous studies reported a gradual decrease in the surgery rate over time, the lower rate in this study could have been due to our consideration of a more recent time period[21,25].
This study had some limitations. First, the certainty of the IBD diagnosis was limited owing to the nature of the claims data. To overcome this concern, we defined patients with IBD more accurately using both ICD-10 codes and V-codes rather than relying only on ICD-10 codes based on a comparative analysis of patients with IBD in the SK-IBD study. Our definition was further validated internally at a tertiary referral hospital in Korea (Seoul National University Hospital), demonstrating sensitivity rates of 94.5% and 96.4% for CD and UC, respectively. Second, since we used claims data, we could not obtain detailed clinical information, such as symptoms, disease phenotype, or severity, which may have influenced the clinical outcomes of IBD. Thus, we could not establish a causal relationship between using immunomodulators and biologics and IBD-related clinical outcomes. Third, the present study included a study cohort that was retrospectively enrolled with a diagnostic code for IBD during the study period from 2010 to 2018 and was followed up until 2018. Therefore, the duration of the disease and follow-up within the cohort showed heterogeneity; moreover, the follow-up duration may be too short to reflect the entire clinical course of IBD, particularly among subjects diagnosed recently. Finally, although we carefully devised an operational definition of clinical outcomes to encompass IBD-related results, inherent uncertainty remained since the NHIS does not provide detailed clinical data of individual patients or information on individual identifiers.
In conclusion, our study indicated a distinct shift in the epidemiology of the Korean population with IBD towards a stabilizing incidence and a younger age at diagnosis. The incidence of CD has been stable since 2014, whereas that of UC has continuously increased, peaking at a younger age. Moreover, the use of immunomodulators and biologics increased notably, aligning with a reduction in the rates of hospitalization and surgery during the study period. Our findings shed light on the evolving landscape of IBD in Korea and reveal changes in its incidence, treatment patterns, and clinical outcomes.
Over time, inflammatory bowel disease (IBD) has become a global disease with changing epidemiological patterns. Traditionally, IBD has been considered a Western disease; however, its incidence has increased in newly industrialized countries, including Asia, since the turn of the twenty-first century.
Although the epidemiology of IBD differs between the Western and Eastern worlds, and understanding the epidemiology of IBD is crucial for better management of patients and healthcare resources, data on IBD epidemiology in Asia remain limited.
We aimed to evaluate the incidence and prevalence of IBD using a nationwide population-based cohort in South Korea. Additionally, we sought to investigate the temporal changes in the medications and clinical outcomes of IBD.
This study used claims data from the National Health Insurance Service of South Korea. We identified IBD patients using the International Classification of Diseases, Tenth Revision, and Rare and Intractable Disease diagnostic codes for Crohn’s disease (CD) and ulcerative colitis (UC). The incidence, prevalence, medication use, and clinical outcomes of IBD were assessed from 2010 to 2018.
Over the study period, from 2010 to 2018, 14498 and 31409 patients were newly diagnosed with CD and UC, respectively. The incidence of CD has stabilized in South Korea, while that of UCD has steadily increased with a shifted peak age from the 50-s to the 20-s since 2014. The prevalence rates of both CD and UC increased consistently. Over the study period, the use of immunomodulators and biologics increased, but that of 5-aminosalicylates and steroids decreased in both CD and UC patients, which was accompanied by decreased IBD-related hospitalizations and surgeries.
The nationwide study revealed the recent epidemiology of IBD in South Korea. The incidence of CD has been stable since 2014, but that of UC has increased with a shift to a younger age at peak incidence between 2010 and 2018. Additionally, the clinical outcomes of IBD improved over the study period, in parallel with the increased use of immunomodulators and biologics.
Future studies are required to evaluate the long-term prognosis of IBD according to changes in IBD treatment medications, including indicators such as disease activity and quality of life.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Coelho-Prabhu N, United States; Xiao Y, China S-Editor: Qu XL L-Editor: A P-Editor: Yuan YY
| 1. | Ng SC, Shi HY, Hamidi N, Underwood FE, Tang W, Benchimol EI, Panaccione R, Ghosh S, Wu JCY, Chan FKL, Sung JJY, Kaplan GG. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2017;390:2769-2778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2677] [Cited by in RCA: 4109] [Article Influence: 513.6] [Reference Citation Analysis (110)] |
| 2. | Kaplan GG, Windsor JW. The four epidemiological stages in the global evolution of inflammatory bowel disease. Nat Rev Gastroenterol Hepatol. 2021;18:56-66. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 187] [Cited by in RCA: 767] [Article Influence: 191.8] [Reference Citation Analysis (0)] |
| 3. | Jung YS, Han M, Kim WH, Park S, Cheon JH. Incidence and Clinical Outcomes of Inflammatory Bowel Disease in South Korea, 2011-2014: A Nationwide Population-Based Study. Dig Dis Sci. 2017;62:2102-2112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 58] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 4. | Park SH, Kim YJ, Rhee KH, Kim YH, Hong SN, Kim KH, Seo SI, Cha JM, Park SY, Jeong SK, Lee JH, Park H, Kim JS, Im JP, Yoon H, Kim SH, Jang J, Kim JH, Suh SO, Kim YK, Ye BD, Yang SK; Songpa-Kangdong Inflammatory Bowel Disease [SK-IBD] Study Group. A 30-year Trend Analysis in the Epidemiology of Inflammatory Bowel Disease in the Songpa-Kangdong District of Seoul, Korea in 1986-2015. J Crohns Colitis. 2019;13:1410-1417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 127] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 5. | Kim HJ, Hann HJ, Hong SN, Kim KH, Ahn IM, Song JY, Lee SH, Ahn HS. Incidence and natural course of inflammatory bowel disease in Korea, 2006-2012: a nationwide population-based study. Inflamm Bowel Dis. 2015;21:623-630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 149] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 6. | Kwak MS, Cha JM, Lee HH, Choi YS, Seo SI, Ko KJ, Park DI, Kim SH, Kim TJ. Emerging trends of inflammatory bowel disease in South Korea: A nationwide population-based study. J Gastroenterol Hepatol. 2019;34:1018-1026. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 63] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 7. | Kim JA, Yoon S, Kim LY, Kim DS. Towards Actualizing the Value Potential of Korea Health Insurance Review and Assessment (HIRA) Data as a Resource for Health Research: Strengths, Limitations, Applications, and Strategies for Optimal Use of HIRA Data. J Korean Med Sci. 2017;32:718-728. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 349] [Cited by in RCA: 532] [Article Influence: 66.5] [Reference Citation Analysis (0)] |
| 8. | Kim SH, Park Y, Kim SP, Lee SH, Oh SH, Yang SK, Yoon HJ, Kim KM. Shift to a Younger Age and Regional Differences in Inflammatory Bowel Disease in Korea: Using Healthcare Administrative Data. Dig Dis Sci. 2022;67:5079-5089. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 9. | Shivashankar R, Tremaine WJ, Harmsen WS, Loftus EV Jr. Incidence and Prevalence of Crohn's Disease and Ulcerative Colitis in Olmsted County, Minnesota From 1970 Through 2010. Clin Gastroenterol Hepatol. 2017;15:857-863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 346] [Article Influence: 43.3] [Reference Citation Analysis (0)] |
| 10. | Lophaven SN, Lynge E, Burisch J. The incidence of inflammatory bowel disease in Denmark 1980-2013: a nationwide cohort study. Aliment Pharmacol Ther. 2017;45:961-972. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 123] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 11. | Park J, Cheon JH. Incidence and Prevalence of Inflammatory Bowel Disease across Asia. Yonsei Med J. 2021;62:99-108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 119] [Cited by in RCA: 114] [Article Influence: 28.5] [Reference Citation Analysis (0)] |
| 12. | Park SH. Update on the epidemiology of inflammatory bowel disease in Asia: where are we now? Intest Res. 2022;20:159-164. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 55] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 13. | Murakami Y, Nishiwaki Y, Oba MS, Asakura K, Ohfuji S, Fukushima W, Suzuki Y, Nakamura Y. Estimated prevalence of ulcerative colitis and Crohn's disease in Japan in 2014: an analysis of a nationwide survey. J Gastroenterol. 2019;54:1070-1077. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 114] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 14. | Lee JW, Eun CS. Inflammatory bowel disease in Korea: epidemiology and pathophysiology. Korean J Intern Med. 2022;37:885-894. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 18] [Reference Citation Analysis (0)] |
| 15. | Narula N, Wong ECL, Dehghan M, Mente A, Rangarajan S, Lanas F, Lopez-Jaramillo P, Rohatgi P, Lakshmi PVM, Varma RP, Orlandini A, Avezum A, Wielgosz A, Poirier P, Almadi MA, Altuntas Y, Ng KK, Chifamba J, Yeates K, Puoane T, Khatib R, Yusuf R, Boström KB, Zatonska K, Iqbal R, Weida L, Yibing Z, Sidong L, Dans A, Yusufali A, Mohammadifard N, Marshall JK, Moayyedi P, Reinisch W, Yusuf S. Association of ultra-processed food intake with risk of inflammatory bowel disease: prospective cohort study. BMJ. 2021;374:n1554. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 70] [Cited by in RCA: 196] [Article Influence: 49.0] [Reference Citation Analysis (0)] |
| 16. | Lee D, Albenberg L, Compher C, Baldassano R, Piccoli D, Lewis JD, Wu GD. Diet in the pathogenesis and treatment of inflammatory bowel diseases. Gastroenterology. 2015;148:1087-1106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 246] [Cited by in RCA: 286] [Article Influence: 28.6] [Reference Citation Analysis (0)] |
| 17. | Elten M, Benchimol EI, Fell DB, Kuenzig ME, Smith G, Kaplan GG, Chen H, Crouse D, Lavigne E. Residential Greenspace in Childhood Reduces Risk of Pediatric Inflammatory Bowel Disease: A Population-Based Cohort Study. Am J Gastroenterol. 2021;116:347-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 36] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 18. | Benchimol EI, Kaplan GG, Otley AR, Nguyen GC, Underwood FE, Guttmann A, Jones JL, Potter BK, Catley CA, Nugent ZJ, Cui Y, Tanyingoh D, Mojaverian N, Bitton A, Carroll MW, deBruyn J, Dummer TJB, El-Matary W, Griffiths AM, Jacobson K, Kuenzig ME, Leddin D, Lix LM, Mack DR, Murthy SK, Sánchez JNP, Singh H, Targownik LE, Vutcovici M, Bernstein CN. Rural and Urban Residence During Early Life is Associated with Risk of Inflammatory Bowel Disease: A Population-Based Inception and Birth Cohort Study. Am J Gastroenterol. 2017;112:1412-1422. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 63] [Cited by in RCA: 91] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 19. | Passos MAT, Chaves FC, Chaves-Junior N. THE IMPORTANCE OF COLONOSCOPY IN INFLAMMATORY BOWEL DISEASES. Arq Bras Cir Dig. 2018;31:e1374. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 20. | Cha JM, Park SH, Rhee KH, Hong SN, Kim YH, Seo SI, Kim KH, Jeong SK, Lee JH, Park SY, Park H, Kim JS, Im JP, Yoon H, Kim SH, Jang J, Kim JH, Suh SO, Kim YK, Ye BD, Yang SK. Long-term prognosis of ulcerative colitis and its temporal changes between 1986 and 2015 in a population-based cohort in the Songpa-Kangdong district of Seoul, Korea. Gut. 2020;69:1432-1440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 40] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 21. | Tsai L, Ma C, Dulai PS, Prokop LJ, Eisenstein S, Ramamoorthy SL, Feagan BG, Jairath V, Sandborn WJ, Singh S. Contemporary Risk of Surgery in Patients With Ulcerative Colitis and Crohn's Disease: A Meta-Analysis of Population-Based Cohorts. Clin Gastroenterol Hepatol. 2021;19:2031-2045.e11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 191] [Article Influence: 47.8] [Reference Citation Analysis (0)] |
| 22. | Hong SW, Ye BD, Cheon JH, Lee JH, Koo JS, Jang BI, Lee KM, Kim YS, Kim TO, Im JP, Song GA, Jung SA, Kim HS, Park DI, Huh KC, Kim YH, Cha JM, Seo GS, Choi CH, Song HJ, Baik GH, Kim JW, Shin SJ, Park YS, Lee CK, Lee J, Jung SH, Jung Y, Park SC, Joo YE, Jeen YT, Han DS, Yang SK, Kim HJ, Kim WH, Kim JS. Clinical Features and Long-term Prognosis of Crohn's Disease in Korea: Results from the Prospective CONNECT Study. Gut Liver. 2022;16:907-920. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 23. | Fumery M, Singh S, Dulai PS, Gower-Rousseau C, Peyrin-Biroulet L, Sandborn WJ. Natural History of Adult Ulcerative Colitis in Population-based Cohorts: A Systematic Review. Clin Gastroenterol Hepatol. 2018;16:343-356.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 210] [Cited by in RCA: 327] [Article Influence: 46.7] [Reference Citation Analysis (1)] |
| 24. | Rungoe C, Langholz E, Andersson M, Basit S, Nielsen NM, Wohlfahrt J, Jess T. Changes in medical treatment and surgery rates in inflammatory bowel disease: a nationwide cohort study 1979-2011. Gut. 2014;63:1607-1616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 236] [Cited by in RCA: 263] [Article Influence: 23.9] [Reference Citation Analysis (0)] |
| 25. | Dittrich AE, Sutton RT, Haynes K, Wang H, Fedorak RN, Kroeker KI. Incidence Rates for Surgery in Crohn's Disease Have Decreased: A Population-based Time-trend Analysis. Inflamm Bowel Dis. 2020;26:1909-1916. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (0)] |