Published online Sep 15, 1997. doi: 10.3748/wjg.v3.i3.185
Revised: December 22, 1996
Accepted: December 30, 1996
Published online: September 15, 1997
AIM: To demonstrate the relationship between the ultrastructural changes of the gastric mucosa and the syndrome differentiation in chronic gastritis.
METHODS: Sixteen chronic gastritis patients with Piweixuhan (PXG, the cold of insufficiency syndrome of the spleen and the stomach) and fifteen chronic gastritis patients with Ganweibuhe (GBG, incoordination syndrome of the liver and the stomach) were treated with Jianpiwenwei decoction (JWD, invigorating the spleen and warming the stomach) or Shuganhewei decoction (SHD, dispersing the stagnated Liver Qi and regulating the stomach), respectively for three months. Before and after treatment, a gastroscopy was performed and the gastric mucosa was collected from the lesser curvature of the antrum of each patient. The ultrasections were observed and photographed under the JEM-100C X electron microscope.
RESULTS: The common ultrastructural anomalies of the two types of chronic gastritis were the plasmacyte infiltration and the lesions of the mucosal epithelial cells, chief cells and antral mucous cells. There were obvious differences between the two types. In PXG, the predominant lesion of the chief cells was swelling of the mitochondria, while in GBG the rough endoplasmic reticulum was enlarged in the chief cells and the plasmacytes. After treatment, most cases of the ultrastructural lesions reverted to normal or improved.
CONCLUSION: There was a close relationship between the ultrastructural changes of gastric mucosa and the syndrome differentiation of chronic gastritis. JWD and SHD could significantly improve the ultrastructural lesions of the gastric mucosa.
- Citation: Zhang ZL, Bu JK, Zhao JX. Ultrastructural observation of the gastric mucosa in chronic gastritis patients treated by traditional Chinese medicine. World J Gastroenterol 1997; 3(3): 185-188
- URL: https://www.wjgnet.com/1007-9327/full/v3/i3/185.htm
- DOI: https://dx.doi.org/10.3748/wjg.v3.i3.185
Chronic gastritis is a common disease that is difficult to cure. Diagnosis and treatment of chronic gastritis by traditional Chinese medicine (TCM) has had a good therapeutic effect. In this study, we investigated the relationship between the ultrastructural changes of the gastric mucosa based on the TCM differentiation of chronic gastritis. The therapeutic effects of the TCM differentiation treatment on the gastric mucosa were also tested.
Sixteen patients with Piweixuhan (PXG, the cold of insufficiency syndrome of the spleen and the stomach) and fifteen patients with Ganweibuhe (GBG, incoordination syndrome of the liver and the stomach) were selected from the inpatients at the First Affiliated Hospital of Lanzhou Medical College. They were diagnosed according to the TCM differentiation standard of chronic gastritis in “Guiding Principle of Clinical Research of New Drugs” by the Chinese Ministry of Public Health.
The patients with PXG were treated with a Jianpiwenwei decoction (JWD, invigorating the spleen and warming the stomach). This decoction contained 10 g of Dangshen (Radix codonopsis pilosula e), 20 g of Fuling (Poria), 15 g of Baizhu (Rhizoma atractylodis macrocephalae), 5 g of Muxiang (Radix aucklandiae), 5 g of Shenggancao (Radix glycyrrhizae), 10 g of Zhibanxia (Rhizoma pinelliae preparata), 5 g of Sharen (Fructus amomi), 10 g of Gaoliangjiang (Rhizoma alpiniae officinarum), 10 g of Yanhusuo (Rhizoma corydalis), and 10 g of Chaomaiya (Fructus hordei germinatus).
The patients with GBG were treated with a Shuganhewei decoction (SHD, dispersing the stagnated Liver Qi and regulating the stomach). This decoction contained 10 g of Chaihu (Radix bupleuri), 15 g of Baishao (Radix paeoniae alba), 10 g of Zhiqiao (Fructus aurantii), 5 g of Muxiang (Radix aucklandiae), 10 g of Shenggancao (Radix glycyrrhizae), 10 g of Yujin (Radix curcumae), 15 g of Yanhusuo (Rhizoma corydalis), 10 g of Baizhi (Radix angelicae dahuricae), 10 g of Danggui (Radix angelicae sinensis), and 10 g of Jineijin (Endothelium corneum galli).
Patients were given 200 mL of the respective decoctions orally for three months, twice a day. The crude content of the two prescriptions was 500 g/L. Other related medications were not given during the observation period.
Gastroscopy was performed before and after the treatment. The gastric mucosa was collected from the lesser curvature of the antrum and immediately immersed in a cold 3% glutaraldehyde solution. The specimens were rinsed with phosphate buffer solution, post-fixed with 1% osmium tetroxide, dehydrated in graded steps with increasing percentages of ethanol, embedded with Epon 812, sectioned with an ultratome, and double stained with uranium acetate and lead citrate. The ultrasections were observed and photographed under the JEM 100CX transmission electron microscopy.
The main ultrastructural lesions were divided into three grades: severe, moderate and mild. After treatment, the therapeutic effects were determined according to the following assessment standard: recovery (the ultrastructural lesions disappeared completely), marked effectiveness (the ultrastructural lesions lightened by two grades), effective (the ultrastructural lesions lightened by one grade), ineffective (the ultrastructural lesions had no obvious changes). All data were analyzed statistically by the χ2 test, and significance was set at P < 0.05.
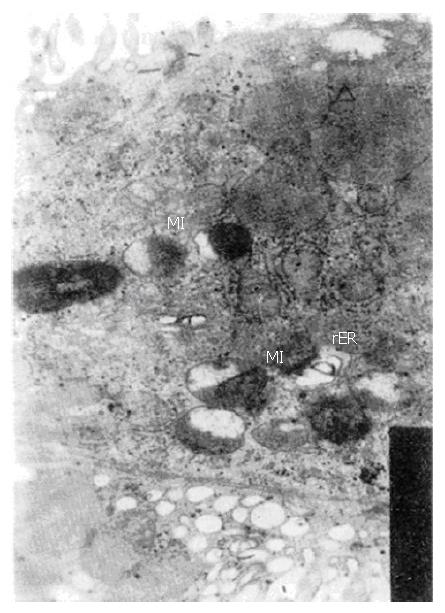
We observed that the mitochondria in the chief cells were swelled, its cristae were reduced and shortened, and some even displayed vacuolization. Some displayed pyknosis (Figure 1). The mitochondria lesions were classified into three grades: severe (the injured mitochondria exceeded 2/3 of all the mitochondria in the cytoplasm), moderate (the number of injured mitochondria was between 1/3 and 2/3 of all the mitochondria in cytoplasm), and mild (the injured mitochondria were less than 1/3 of all the mitochondria in cytoplasm).
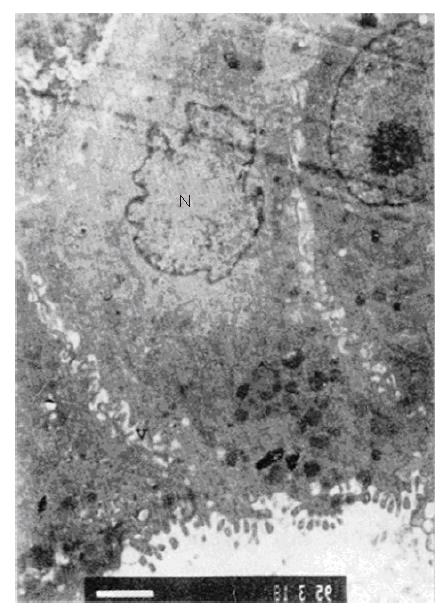
We observed that the rough endoplasmic reticulum (rER) in the chief cells were expanded, showed vesicles and vacuoles, and some even had intracisternal sequestration[1] (Figure 2). The rER enlargement was also graded into three degrees: mild (the rER enlargement was less than 1/3 of the cytoplasm or two times less than the area of the normal rER), moderate (the rER enlargement accounted for 1/3 to 2/3 of the cytoplasm or exceeded four times of the area of the normal rER), and severe (the rER enlargement was more than 2/3 of the cytoplasm or six times more than the area of the normal rER, or formed intracisternal sequestration).
We observed that the intercellular space in the mucosal epithelial and antral mucous was widened. This change was also graded into the following three degrees: severe (the intercellular space was significantly enlarged and exceeded the width of the cells, the cell processes became slight and dispersed, and lymphocytes appeared in some spaces), moderate (the width of the intercellular space was between the severe and mild degrees), and mild (the intercellular space was small, and the cell processes became shorter and smaller). In addition, we observed that the surface microvilli were short, small and sparse, the organelles were reduced, the mucous granules decreased, the cells atrophied, and the electron density increased. In a few patients, the mucous epithelial cells became stratified epithelium.
We observed heterotypical and deformed nuclei appeared in the mucosal epithelial cells and the antral mucous cells. Many nuclei were markedly enlarged and the nucleoli increased in number and size. The nuclear membrane folded and sank, which thereby led to nucleus deformation (Figure 3). This deformation was divided into three grades: severe (the sinking depth exceeded the short radius of the nucleus), moderate (the sinking depth or scope was between the mild and the severe grades), and mild (the sinking depth was less than 1/3 of the short radius of nucleus, or the sinking scope was less than 1/3 of the nuclear circumference).
We observed that the lymphocytes and plasmacytes infiltrated into the gastric mucosa. The lymphocytes were normal. Some appeared in the enlarged mucous intercellular space or between the glandular epithelial cells. In the plasmacytes, the rER enlarged to various degrees. We utilized the same grading method as that for the chief cells (Figure 4).
In addition, we found that the capillary endothelial cells in some patients were swelled or disappeared after treatment. There were a small number of G cells scattered in the antral mucosa. The rER was enlarged in some of these cells. In our study, the parietal cells, the zymogen granules in the chief cells, the stomach body’s mucous cells, and the mucigen granules were nearly normal.
The therapeutic effects on the ultrastructural lesions of the gastric mucosa are presented in Tables 1 and 2.
| Differentiation | Total cases | Organelle lesions | Injured cases (%) | Markedly effective | Effective | Ineffective | Total effective rate (%) |
| PXG | 16 | Mitochondriab | 13 (81.3) | 7 | 4 | 2 | 84.6 |
| rER6 | 3 (18.8) | 1 | 1 | 1 | 1.0 | ||
| GBG | 15 | Mitochondria | 3 (20.0) | 0 | 2 | 1 | 66.7 |
| rER | 12 (80.0) | 8 | 2 | 2 | 83.3 |
| Ultrastructural changes | Differentiation | Injured | Recovery | Markedly | Effective | Ineffective | Total effective |
| Cases (%) | effective | Rate (%) | |||||
| The intercellular space of mucosal epithelial cells widened | PXG | 14 (87.5) | 2 | 6 | 3 | 3 | 78.6 |
| GBG | 12 (80.0) | 2 | 5 | 3 | 2 | 83.3 | |
| The intercellular space of antral mucous cells widened | PXG | 13 (81.3) | 4 | 5 | 2 | 2 | 84.6 |
| GBG | 13 (86.7) | 3 | 6 | 3 | 1 | 92.3 | |
| The nuclear membrane of the mucosal epithelial cells and the antral mucous cells folded and sank in | PXG | 10 (62.5) | 3 | 3 | 2 | 2 | 80.0 |
| GBG | 10 (66.7) | 2 | 4 | 3 | 1 | 90.0 | |
| The rER in the plasmacyte enlarged | PXG | 6 (37.5)a | 1 | 3 | 0 | 2 | 66.7 |
| GBG | 12 (80.0) | 4 | 3 | 3 | 2 | 83.3 |
Optical microscopy is the primary means to diagnose the degree and the type of pathological changes in gastritis. However, it is difficult to detect the early stage lesions of organelles in the cells and to determine the nature of the lesions by optical microscopy because of its limited resolution. Moreover, the pathological grading under optical microscope is not very precise. In order to explore a more objective, reliable and precise method to determine therapeutic effects and pathological grading, we designed this study, which combined the TCM differentiation treatment and observation of the ultrastructure of the cells. Although there were some studies about the ultrastructural study of chronic gastritis[2-5], there were few studies about the relationship between the ultrastructural changes of the gastric mucosa and the TCM differentiation of chronic gastritis.
This study showed that the ultrastructural lesions in the chief cells were significantly different between the two types of gastritis. PXG was characterized by swelled mitochondria, while GBG was characterized by expanded rER. This morphological difference revealed that the TCM differentiation of chronic gastritis has a modern ultramicropathological basis. Ultrastructural research on chronic gastritis could greatly contribute to its treatment and differentiation.
This study also found that more than 80% of chronic gastritis patients had widened intercellular space of the mucosal epithelial and the antral mucous cells. This observation was consistent with the results of animal experiments reported in the literature[3,6]. On the other hand, more than 60% of the cases had deformed nuclei, the nuclear membrane was folded and sank in, and the nucleolus increased in number and size. This might be a compensated hyperfunction after the gastric mucosal barrier and the antral mucous cells were damaged. Liang et al[3] thought that the intercellular space enlargement was caused by mesenchyme edema. However, our results showed that the cell atrophy was a direct cause of intercellular space enlargement, which was consistent with our experimental results in a rat model[6].
The lymphocyte and plasmacyte infiltration into the gastric mucosa of chronic gastritis was reported previously, which indicated that chronic gastritis was closely related to the patient’s immunity. We observed plasmacyte infiltration in 58.1% of the patients with the rER enlarged to various degrees. Interestingly, the plasmacyte infiltration appeared in 80.0% of PXG patients, but only in 37.5% of GBG patients, which indicated that the GBG may be more closely related with immune functions. This has been confirmed by our experimental research[6] and helps to explain why the lesions of chief cells were significantly different between the two types of gastritis. We hypothesize that the rER enlargement in chief cells may be a result of immune damage. In PXG patients, the main changes of the chief cells were mitochondrial lesions. It is well known that the cAMP content in cells of PXG patients is reduced (and thus is ATP reduced), the mitochondrial permeability is increased, which causes swelling and vacuolization. As a result, energy is decreased, cell function is lowered, and cells are atrophied, which led to gastric mucosal atrophy. In this study, parietal cells were normal, which was not consistent with the literature[2-5]. This difference needs to be examined further.
We observed that the ultrastructural lesions in PXG and GBG patients were significantly improved after treatment with JWD and SHD. We hypothesized that JWD would improve the mitochondrial lesions by increasing the cAMP content in cells, while SHD would improve the rER enlargement by stabilizing the plasmacytes and inhibiting the excessive immune reaction. Both prescriptions could strengthen the resistance against diseases, regulate the patients’ immune function, and accelerate blood circulation of the gastric mucosa, thus promoting the recovery of the ultrastructural lesions of the gastric mucosa.
We also observed a few G cells in the antrum, in which some rER were enlarged. But we did not observe any other changes, such as secretory granules vacuolization and reduction reported by Ren et al[2]. The rER enlargement of G cells mainly appeared in GBG patients, which probably was caused by the neuroendocrine disorder of G cells. SHD could make the enlarged rER in G cells recover by regulating its neuroendocrine function.
In addition, in the mesenchyme of the gastric mucosa in a few patients, the capillary endothelium swelled and the capillary cavity narrowed leading to dysfunction of the microcirculation. After treatment, these changes disappeared, suggesting that the two decoctions could significantly improve the microcirculation of the gastric mucosa. Therefore, both recovery of the mucosal epithelium and gland and the improvement of the microcirculation of gastric mucosa should be emphasized in treating chronic gastritis so as to increase the therapeutic effects.
Zi-Li Zhang, male, was born on November 16, 1963 in Jingtai County, Gansu Province, and graduated from the Department of Medicine, Lanzhou Medical College in 1986. He is a Deputy chief physician, and has 31 papers published.
Original title:
S- Editor: Filipodia L- Editor: Jennifer E- Editor: Hu S
| 1. | Song SX, Be AH, Li JL, Bu JK, Wang YL, Sun SY. Electron microscopic basis for medicine. Beijing: Beijing Publishing House 1992; 183-227. |
| 2. | Ren HY, Chen GX, Nui LD, Lu GH, Hao WQ, et al. Observations of pathomorphologic changes on 150 chronic atrophic gastritis patients by treatment based on syndrome differentiation. Chinese Journal of Integrated Traditional and Western Medicine. 1993;13:144-146. |
| 3. | Liang P, Chen LY, Yang SM, Chen BF, Lin JX, Pan XZ, et al. A study of the ultramicroscopic structure of chronic atrophicgastritis with data of gastric mucosa biopsy in 20 cases. Chinese Journal of International Medicine. 1982;21:220-223. |
| 4. | Dong YM. [Scanning and transmission electron microscopy of chronic atrophic gastritis in 20 cases]. Zhonghua Binglixue Zazhi. 1987;16:50-53. [PubMed] |
| 5. | Li QM, Wu YF, Huang QH, Deng YF, Wu JL, et al. Ultrastructure of gastric mucosa and pathogenesis in spleen-energy deficiency. Chinese Journal of New Gastroenterology. 1994;2:156-157. |
| 6. | Bu JK, Zhang ZL, Zhao JX. Stereological and ultrastructural research on the rats with chronic gastritis treated based on the differential diagnosis of traditional Chinese medicine (TCM). China National Journal of New Gastroenterology. 1996;2:76-78. |