Published online Nov 28, 2023. doi: 10.3748/wjg.v29.i44.5882
Peer-review started: June 5, 2023
First decision: August 26, 2023
Revised: September 30, 2023
Accepted: November 14, 2023
Article in press: November 14, 2023
Published online: November 28, 2023
Processing time: 175 Days and 8.3 Hours
The clinical trend and characteristics of peptic ulcer disease (PUD) have not fully been investigated in the past decade.
To evaluate the changing trends and characteristics of PUD according to age and etiology.
We analyzed seven hospital databases converted into the Observational Medical Outcomes Partnership-Common Data Model between 2010 and 2019. We classified patients with PUD who underwent rapid urease tests or Helicobacter pylori (H. pylori) serology into three groups: H. pylori-related, drug [nonsteroidal anti-inflammatory drugs (NSAIDs) or aspirin]-related, and idiopathic (H. pylori/NSAID/aspirin-negative) PUD and compared the yearly trends and characteristics among the three groups.
We included 26785 patients in 7 databases, and the proportion of old age (≥ 65 years) was 38.8%. The overall number of PUD exhibited no decrease, whereas PUD in old age revealed an increasing trend (P = 0.01 for trend). Of the 19601 patients, 41.8% had H. pylori-related, 36.1% had drug-related, and 22.1% had idiopathic PUD. H. pylori-related PUD exhibited a decreasing trend after 2014 (P = 0.01), drug-related PUD demonstrated an increasing trend (P = 0.04), and idiopathic PUD showed an increasing trend in the old-age group (P = 0.01) during 10 years. Patients with drug-related PUD had significantly more comorbidities and concomitant ulcerogenic drugs. The idiopathic PUD group had a significantly higher number of patients with chronic liver disease.
With the aging population increase, the effects of concomitant ulcerogenic drugs and preventive strategies should be investigated in drug-induced PUD. Further studies are required to clarify the relationship between idiopathic PUD and chronic liver disease.
Core Tip: In the multicenter study including 26785 peptic ulcer disease (PUD) patients from 7 databases, the overall number of PUD exhibited no decrease, whereas PUD in old age revealed an increasing trend from 2010 to 2019 in Korea. According to etiology, decreasing trend of Helicobacter pylori-related PUD after year 2014, and increasing trend of drug-related PUD were observed in the past decade. Drug-related PUD showed significantly more comorbidities and exposure to concomitant ulcerogenic drugs, and the idiopathic PUD group had a significantly higher proportion in the chronic liver disease. Further studies are required to clarify the relationship between idiopathic PUD and chronic liver disease.
- Citation: Choi YJ, Kim TJ, Bang CS, Lee YK, Lee MW, Nam SY, Shin WG, Seo SI. Changing trends and characteristics of peptic ulcer disease: A multicenter study from 2010 to 2019 in Korea. World J Gastroenterol 2023; 29(44): 5882-5893
- URL: https://www.wjgnet.com/1007-9327/full/v29/i44/5882.htm
- DOI: https://dx.doi.org/10.3748/wjg.v29.i44.5882
Peptic ulcer disease (PUD) remains a critical cause of hospitalization, particularly when complicated by hemorrhage, perforation, or obstruction[1]. The main etiologies of PUD include Helicobacter pylori (H. pylori) infection and the use of aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs)[1]. The overall decline of H. pylori infection in the general population and advances in the management of H. pylori infection have led to a decline in the PUD incidence over the past two decades, however, prescriptions of aspirin and NSAIDs have increased over the same period owing to the rising number of older patients and patients with comorbidities[2]. Furthermore, direct oral anticoagulants (DOAC), newer NSAIDs, and antiplatelet agents continue to be used in chronic disease, and public awareness of H. pylori eradication has improved. Consequently, trends of PUD have demonstrated inconsistent results among regions[2-7]. A recent popu-lation-based study reported that morbidity and mortality due to PUD decreased significantly from 1990 to 2019, while a gradual upward trend has been observed in the recent 15 years, which might be associated with changes in risk factors[2]. Meanwhile, the incidence of non-H. pylori, non-NSAIDs/aspirin PUD, also termed idiopathic PUD, has increased in recent years, particularly in Asian countries[8]. The clinical outcomes of idiopathic PUD revealed recurrent ulcer bleeding and higher mortality in previous studies[9-14]; however, characteristics of idiopathic PUD remain poorly understood and warrant further investigation.
To date, few large-scale studies have comprehensively investigated the recent changing trends and clinical characteristics of PUD, including the multiple risk factors. Therefore, we investigated the trends and characteristics of PUD according to age and etiology in Korea between 2010 and 2019.
We analyzed seven hospital databases converted into the Observational Medical Outcomes Partnership-Common Data Model (OMOP-CDM) using the FEEDER-NET platform, which is a coordinating platform that enables data user and supplier connections and multi-institution analyses, with the anonymity of patients’ personal information, as applied in previous studies[15-17]. The included institutions were Ajou University Medical Center (AUMC), Daegu Catholic Medical Center (DCMC), Ewha Womans University Medical Center (EUMC), Gyeongsang National University Hospital (GNUH), Kangdong Sacred Heart Hospital (KDH), Kangwon National University Hospital (KNUH), and Wonkwang University Hospital (WKUH). The detailed characteristics of each database are presented in Supplementary Table 1.
The characteristics of PUD were analyzed using the characterization tab on ATLAS, which is a web-based open platform developed by the Observational Health Data Sciences and Informatics community[18]. We analyzed basic demographic information, prescriptions, and comorbidities during the year before entering the cohort. We evaluated for exposure to aspirin and other antiplatelet agents, NSAIDs, anticoagulants, and potential ulcerogenic drugs (steroids, antidepressants, bisphosphonates, and immunosuppressive agents). Further, the mean Charlson Comorbidity Index (CCI) was calculated for each database. The same analytic codes were applied to seven hospital databases, and the results of each database were combined as proportions without extracting the raw data. The combined results were analyzed yearly for trend analysis and compared according to age group and etiology of PUD. This study was approved by the Institutional Review Board (IRB) of Kangdong Sacred Hospital (IRB number: 2021-11-001). The other six hospitals were affiliated with the Research Border Free Zone, which recognizes IRB approval of the research organizing center and waives individual IRB approval.
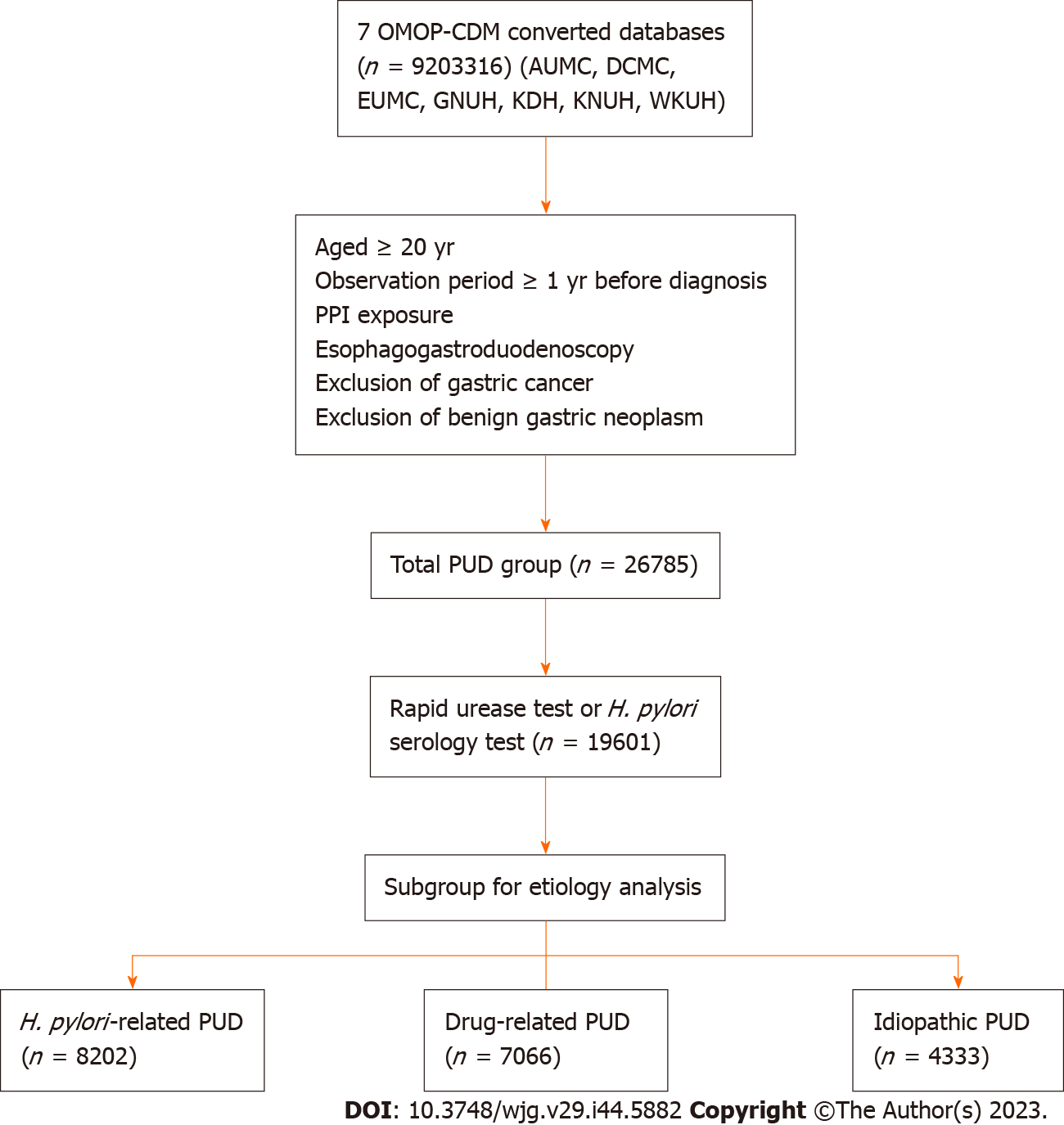
We defined a newly diagnosed PUD as having a 1-year observation period between January 1, 2010, and December 31, 2019, combining diagnostic codes for PUD, esophagogastroduodenoscopy, and exposure to proton pump inhibitors (PPIs). This operational definition was based on previous reports[3,19]. The index date was defined as the initial diagnosis of PUD. Exclusion criteria were as follows: (1) Age < 20 years; (2) Observation period < 1 year before the index date; (3) No exposure to PPIs 30 d before or after the index date; (4) No exposure to esophagogastroduodenoscopy 30 d before or after the index date; (5) Gastric cancer before the index date; and (6) Benign gastric neoplasm before the index date. Each concept name and identifier included in the OMOP-CDM databases matched to diagnostic codes or drugs are listed in Supplementary Table 2.
We classified PUD patients who underwent rapid urease tests or H. pylori serology tests according to etiology into the following three groups: (1) H. pylori-related; (2) Drug-related (H. pylori-negative and NSAIDs/aspirin-related); and (3) Idiopathic (H. pylori/NSAID/aspirin-negative) PUD. H. pylori-related PUD included patients who were concomitantly prescribed H. pylori eradication therapy (PPI, amoxicillin, clarithromycin, bismuth, tetracycline, and metronidazole) for 7-14 d. Drug-related PUD included patients who were not exposed to H. pylori eradication therapy and were exposed to aspirin or NSAIDs before the index date. Idiopathic PUD included patients without exposure to aspirin, NSAIDs, or H. pylori eradication therapy. We further performed a subgroup analysis according to age and sex. We defined the old age group as ≥ 65 years, and the young age group as < 65 years.
Categorical variables were compared using the χ2 or Fisher’s exact test based on the results from the ATLAS version 2.7.6. Continuous variables were expressed as means with standard deviations. The yearly trend was analyzed with simple linear regression, and the yearly trend for each group was compared using the Cochran Armitage test for trends. Statistical significance was set at P < 0.05. Statistical analyses were performed using R version 4.2.1 (R Foundation for Statistical Computing).
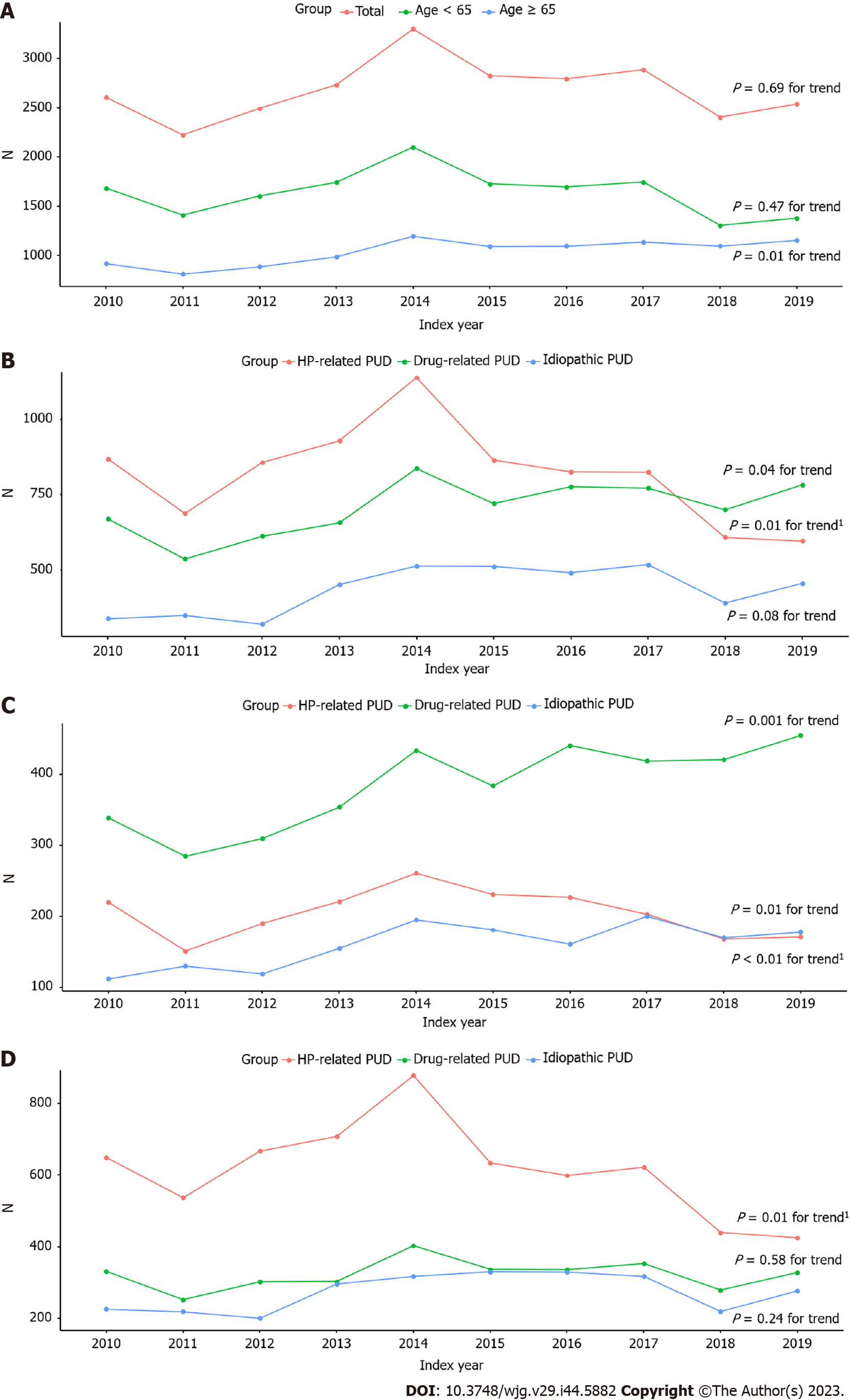
The flowchart of the study is presented in Figure 1. A total of 26785 patients (AUMC, n = 4629; DCMC, n = 4690; EUMC, n = 3118; GNUH, n = 2998; KDH, n = 6320; KNUH, n = 1854; and WKUH, n = 3176) were included between 2010 and 2019. Finally, 15544 (58%) were men, and 11241 (42%) were women. The yearly trend of PUD exhibited no declining pattern in the total patients (P = 0.69 for trend) (Figure 2A). The yearly PUD trend in each database is presented in Supple
The baseline demographics are presented in Table 1. The proportion of gastric ulcers (69.2%) was over twofold that of duodenal ulcers (31.3%). The most prevalent comorbidity was hypertensive disorder, followed by diabetes mellitus. The proportions of exposure to NSAIDs, aspirin, and antiplatelet agents were 19.9%, 15.2%, and 11.4%, respectively. Regarding anticoagulants, warfarin and DOAC were prescribed in 2.2% and 1.1% of total patients, respectively. The proportion of exposure to steroids was 12.7%. Detailed information for each database is presented in Supple
| Total (n = 26785) | |
| Age ≥ 65 yr | 10392 (38.8) |
| Men | 15544 (58.0) |
| RUT or serology | 19601 (73.2) |
| Gastric ulcer | 18527 (69.2) |
| Duodenal ulcer | 8377 (31.3) |
| Diagnosis | |
| Hypertensive disorder | 4773 (17.8) |
| Diabetes mellitus | 2239 (8.4) |
| Hyperlipidemia | 2038 (7.6) |
| Chronic kidney disease | 1282 (4.8) |
| Ischemic heart disease | 2221 (8.3) |
| Cerebrovascular disease | 812 (3.0) |
| Chronic liver disease | 1436 (5.4) |
| Osteoarthritis | 425 (1.6) |
| Chronic obstructive lung disease | 515 (1.9) |
| Medication | |
| Aspirin | 4068 (15.2) |
| Other antiplatelet agent1 | 3065 (11.4) |
| Clopidogrel | 2386 (8.9) |
| Cilostazole | 691 (2.6) |
| NSAID | 5342 (19.9) |
| Warfarin | 579 (2.2) |
| DOAC | 297 (1.1) |
| Steroid | 3404 (12.7) |
| Antidepressant | 6308 (23.6) |
| Bisphosphonate | 488 (1.8) |
| Immunosuppressant | 578 (2.2) |
The proportion of patients with old age (≥ 65 years) was 38.8% (10392/26785). The PUD with the old-age group demonstrated an increasing annual trend (P = 0.01 for trend), whereas the young age group (< 65 years) showed no specific trend overall (P = 0.47 for trend) (Figure 2A). The mean CCI in old age was higher than that in total patients (old-age group vs total group; 3.18 ± 2.6 vs 2.58 ± 2.4 in AUMC; 2.94 ± 2.2 vs 2.30 ± 1.9 in DCMC; 2.37 ± 1.9 vs 1.77 ± 1.5 in EUMC; 2.61 ± 2.0 vs 2.19 ± 1.8 in GNUH; 2.58 ± 2.0 vs 2.05 ± 1.7 in KDH; 2.78 ± 2.1 vs 2.36 ± 1.9 in KNUH; and 3.21 ± 2.4 vs 2.66 ± 2.2 in WKUH).
Of the total patients, 19601 underwent rapid urease or H. pylori serology tests. The number of H. pylori-related, drug-related, and idiopathic PUD patients was 8202 (41.8%); 7066 (36.1%); and 4333 (22.1%), respectively. The proportions according to etiology in each hospital are presented in Supplementary Table 3. H. pylori-related PUD exhibited a decreasing trend after 2014 (P = 0.01 for trend), and drug-related PUD showed a slightly increasing trend in the past 10 years (P = 0.04 for trend). In contrast, idiopathic PUD revealed no statistically increasing trend in the past 10 years (P = 0.08 for trend) (Figure 2B).
The comparison of characteristics among the three groups is presented in Table 2. The H. pylori-related PUD group showed the lowest proportion of old age among the three groups. The proportion of duodenal ulcers was significantly higher in the H. pylori-related PUD than in the other groups. The drug-related PUD group had significantly more elderly patients, less predominance of men, more gastric ulcers, comorbidities except for chronic liver disease, exposure to concomitant potential ulcerogenic drugs than the other groups (Table 2). Notably, there were more patients with chronic liver disease in the idiopathic PUD group than in the other groups. In addition, there were significantly more patients with alcoholic liver damage and cirrhosis in the idiopathic PUD group (Table 2).
| H. pylori-related PUD (n = 8202) | Drug-related PUD (n = 7066) | Idiopathic PUD (n = 4333) | P value | All (n = 19601) | |
| Age ≥ 65 | 2043 (24.9) | 3842 (54.4) | 1601 (36.9) | < 0.001 | 7486 (38.2) |
| Men, n (%) | 5268 (64.2) | 3774 (53.4) | 2747 (63.4) | < 0.001 | 11789 (60.1) |
| Gastric ulcer | 5062 (61.7) | 5052 (71.5) | 2758 (63.7) | < 0.001 | 12872 (65.7) |
| Duodenal ulcer | 3272 (39.9) | 2171 (30.7) | 1574 (36.3) | < 0.001 | 7017 (35.8) |
| Diagnosis, n (%) | |||||
| Hypertensive disorder | 928 (11.3) | 2036 (28.8) | 529 (12.2) | < 0.001 | 3493 (17.8) |
| Diabetes mellitus | 438 (5.3) | 954 (13.5) | 256 (5.9) | < 0.001 | 1648 (8.4) |
| Hyperlipidemia | 587 (7.2) | 829 (11.7) | 129 (3.0) | < 0.001 | 1545 (7.9) |
| Chronic kidney disease | 173 (2.1) | 604 (8.5) | 123 (2.8) | < 0.001 | 900 (4.6) |
| Ischemic heart disease | 483 (5.9) | 1098 (15.5) | 49 (1.1) | < 0.001 | 1630 (8.3) |
| Cerebrovascular disease | 161 (2.0) | 372 (5.3) | 35 (0.8) | < 0.001 | 568 (2.9) |
| Chronic liver disease | 224 (2.7) | 447 (6.3) | 349 (8.1) | < 0.001 | 1020 (5.2) |
| Alcoholic liver damage | 164 (2.0) | 253 (3.6) | 234 (5.4) | < 0.001 | 651 (3.3) |
| Liver cirrhosis | 175 (2.1) | 381 (5.4) | 325 (7.5) | < 0.001 | 881 (4.5) |
| Osteoarthritis | 84 (1.0) | 191 (2.7) | 13 (0.4) | < 0.001 | 288 (1.5) |
| Chronic obstructive lung disease | 76 (0.9) | 209 (3.0) | 74 (1.7) | < 0.001 | 359 (1.8) |
| Medication, n (%) | |||||
| Antiplatelet agent1 | 634 (7.7) | 1514 (21.4) | 77 (1.8) | < 0.001 | 2225 (11.4) |
| Warfarin | 84 (1.0) | 258 (3.7) | 34 (0.8) | < 0.001 | 376 (1.9) |
| DOAC | 33 (0.4) | 129 (1.8) | 20 (0.5) | < 0.001 | 182 (0.9) |
| Steroid | 690 (8.4) | 1423 (20.1) | 227 (5.2) | < 0.001 | 2340 (11.9) |
| Antidepressant | 1188 (14.5) | 2408 (34.1) | 868 (20.0) | < 0.001 | 4464 (22.8) |
| Bisphosphonate | 94 (1.1) | 223 (3.2) | 18 (0.4) | < 0.001 | 335 (1.7) |
| Immunosuppressant | 125 (1.5) | 275 (3.9) | 35 (0.8) | < 0.001 | 435 (2.2) |
Of 19601 patients, we conducted a subgroup analysis according to age group and sex. In the old-age (≥ 65 years) group (n = 7486), H. pylori-related PUD was 2043 (27.3%); drug-related was 3842 (51.3%); and idiopathic was 1601 (21.4%). In the young age (< 65 years) group (n = 12115), H. pylori-related PUD was 6159 (50.8%); drug-related was 3224 (26.6%); and idiopathic was 2732 (22.6%). In the old-age group, H. pylori-related PUD exhibited a decreasing trend after 2014 (P < 0.01 for trend), whereas drug-related and idiopathic PUD showed an overall increasing trend (drug-related, P = 0.001 for trend; idiopathic, P = 0.01 for trend) (Figure 2C). In the young age group, there was only a decreasing trend for H. pylori-related PUD after 2014 (P = 0.01 for trend) (Figure 2D). The yearly trend did not differ according to sex.
In the old-age group, more women had drug-related PUD than total patients (Table 3). The proportion of gastric ulcers was highest in drug-related PUD, regardless of age, whereas the proportion of duodenal ulcers showed different patterns according to age. In the old-age group, the proportion of duodenal ulcer was highest in the idiopathic PUD, and it was highest in H. pylori-related PUD in the young age group (Table 3). Other comorbidities or exposure to concomitant drugs did not differ according to age (Table 3). Supplementary Table 4 lists the subgroup analysis according to sex. No significant difference was found according to sex.
| Age (yr) | H. pylori-related PUD (n = 8202) | Drug-related PUD (n = 7066) | Idiopathic PUD (n = 4333) | P value | |
| Men | ≥ 65 | 1161/2043 (56.8) | 1869/3842 (48.6) | 934/1601 (58.3) | < 0.001 |
| < 65 | 4107/6159 (66.7) | 1905/3224 (59.1) | 1813/2732 (66.4) | < 0.001 | |
| Gastric ulcer | ≥ 65 | 1481/2043 (72.5) | 2855/3842 (74.3) | 1093/1601 (68.3) | < 0.001 |
| < 65 | 3581/6159 (58.1) | 2197/3224 (68.1) | 1665/2732 (60.9) | < 0.001 | |
| Duodenal ulcer | ≥ 65 | 612/2043 (30.0) | 1117/3842 (29.1) | 561/1601 (35.0) | < 0.001 |
| < 65 | 2660/6159 (43.2) | 1054/3224 (32.7) | 1013/2732 (37.1) | < 0.001 | |
| Diagnosis | |||||
| Hypertensive disorder | ≥ 65 | 452/2043 (22.1) | 1431/3842 (37.2) | 321/1601 (20.0) | < 0.001 |
| < 65 | 476/6159 (7.7) | 605/3224 (18.8) | 208/2732 (7.6) | < 0.001 | |
| Diabetes mellitus | ≥ 65 | 194/2043 (9.5) | 610/3842 (15.9) | 148/1601 (9.2) | < 0.001 |
| < 65 | 244/6159 (4.0) | 344/3224 (10.7) | 108/2732 (4.0) | < 0.001 | |
| Hyperlipidemia | ≥ 65 | 201/2043 (9.8) | 533/3842 (13.9) | 53/1601 (3.3) | < 0.001 |
| < 65 | 386/6159 (6.3) | 296/3224 (9.2) | 76/2732 (2.8) | < 0.001 | |
| Chronic kidney disease | ≥ 65 | 76/2043 (3.7) | 382/3842 (9.9) | 64/1601 (4.0) | < 0.001 |
| < 65 | 97/6159 (1.6) | 222/3224 (6.9) | 59/2732 (2.3) | < 0.001 | |
| Ischemic heart disease | ≥ 65 | 247/2043 (12.1) | 794/3842 (20.7) | 35/1601 (2.6) | < 0.001 |
| < 65 | 236/6159 (3.8) | 304/3224 (9.4) | 14/2732 (0.6) | < 0.001 | |
| Cerebrovascular disease | ≥ 65 | 92/2043 (4.5) | 288/3842 (7.5) | 25/1601 (1.6) | < 0.001 |
| < 65 | 69/6159 (1.1) | 84/3224 (2.7) | 10/2732 (0.5) | < 0.001 | |
| Chronic liver disease | ≥ 65 | 42/2043 (2.3) | 202/3842 (5.3) | 120/1601 (7.5) | < 0.001 |
| < 65 | 182/6159 (3.0) | 245/3224 (7.6) | 229/2732 (8.4) | < 0.001 | |
| Alcoholic liver damage | ≥ 65 | 20/2043 (1.1) | 85/3842 (2.2) | 64/1601 (4.0) | < 0.001 |
| < 65 | 144/6159 (2.3) | 168/3224 (5.2) | 170/2732 (6.2) | < 0.001 | |
| Liver cirrhosis | ≥ 65 | 29/2043 (1.6) | 161/3842 (4.2) | 113/1601 (7.1) | < 0.001 |
| < 65 | 146/6159 (2.4) | 220/3224 (6.8) | 212/2732 (7.8) | < 0.001 | |
| Osteoarthritis | ≥ 65 | 56/2043 (2.7) | 145/3842 (3.8) | 10/1601 (1.1) | < 0.001 |
| < 65 | 28/6159 (0.5) | 46/3224 (1.6) | 3/2732 (0.2) | < 0.001 | |
| Chronic obstructive lung disease | ≥ 65 | 53/2043 (2.6) | 176/3842 (4.6) | 57/1601 (3.6) | 0.001 |
| < 65 | 23/6159 (0.4) | 33/3224 (1.0) | 17/2732 (0.6) | 0.001 | |
| Medication | |||||
| Antiplatelet agent | ≥ 65 | 324/2043 (15.9) | 1058/3842 (27.5) | 51/1601 (3.2) | < 0.001 |
| < 65 | 310/6159 (5.0) | 456/3224 (14.1) | 26/2732 (1.0) | < 0.001 | |
| Warfarin | ≥ 65 | 49/2043 (2.4) | 190/3842 (4.9) | 28/1601 (1.9) | < 0.001 |
| < 65 | 35/6159 (0.6) | 68/3224 (2.1) | 6/2732 (0.3) | < 0.001 | |
| DOAC | ≥ 65 | 23/2043 (1.2) | 112/3842 (2.9) | 19/1601 (1.2) | < 0.001 |
| < 65 | 10/6159 (0.2) | 17/3224 (0.6) | 1/2732 (0.1) | 0.015 | |
| Steroid | ≥ 65 | 237/2043 (11.6) | 807/3842 (21.0) | 111/1601 (6.9) | < 0.001 |
| < 65 | 453/6159 (7.4) | 616/3224 (19.1) | 116/2732 (4.2) | < 0.001 | |
| Antidepressant | ≥ 65 | 456/2043 (22.3) | 1568/3842 (40.8) | 435/1601 (27.2) | < 0.001 |
| < 65 | 732/6159 (11.9) | 840/3224 (26.1) | 433/2732 (15.8) | < 0.001 | |
| Bisphosphonate | ≥ 65 | 54/2043 (2.6) | 174/3842 (4.5) | 11/1601 (0.7) | < 0.001 |
| < 65 | 40/6159 (0.6) | 49/3224 (1.5) | 7/2732 (0.4) | < 0.001 | |
| Immunosuppressant | ≥ 65 | 49/2043 (2.4) | 108/3842 (2.8) | 13/1601 (0.9) | < 0.001 |
| < 65 | 76/6159 (1.2) | 167/3224 (5.2) | 22/2732 (1.0) | < 0.001 | |
The findings of this multicenter OMOP-CDM-based study revealed that the total number of PUD patients demonstrated no decreasing trend, whereas newly diagnosed PUD in the old-age group showed an increasing trend in the past 10 years. We classified PUD patients who underwent H. pylori serology or rapid urease tests into H. pylori-related, drug-related, and idiopathic PUD to clarify the characteristics and changing trends of PUD according to etiology. H. pylori-related PUD showed a decreasing trend after 2014; drug-related PUD, an increasing trend; and idiopathic PUD, an increasing trend only in the old-age group. Drug-related PUD revealed significantly more comorbidities and exposure to concomitant ulcerogenic drugs. Notably, the proportion of patients with chronic liver disease was significantly higher in idiopathic PUD.
Several studies have investigated the trends of PUD, and the overall prevalence has exhibited a decreasing trend in the past few decades; however, the trend differed according to region or sex owing to changes in the distribution of the etiologies of PUD[2,3]. A recent global study has reported that the age-standardized incidence rate exhibited an increasing annual trend with increasing age[2], and our results showed an increasing trend of PUD in the old-age group. A recent Korean nationwide cohort study conducted in 2006-2015 showed a decreasing trend in the H. pylori infection rate and no change in drug exposure that increases the risk of peptic ulcer bleeding (PUB)[3]. Furthermore, the H. pylori infection rate was 34.4% in that study when it was defined by including patients who received H. pylori eradication therapy out of the patients who underwent rapid urease tests, H. pylori cultures, urea breath tests, Warthin-Starry silver stains, and H. pylori stool antigen tests[3]. The lower H. pylori infection rate than that in our study may be attributed to the lack of H. pylori serology testing and false-negative results in the PUB setting in that study. H. pylori-related PUD was 41.8% in our study, which was consistent with a recent Korean nationwide multicenter study that reported 43.9% H. pylori seropositivity from 2016 to 2017[20]. Our proportion of H. pylori-related PUD also included patients who had H. pylori eradication therapy, which suggests that the knowledge and awareness of the public was improved in the past decade. A recent meta-analysis also revealed that technology-enhanced communication initiatives effectively improve compliance to the H. pylori eradication regimen and increase the eradication rate[21].
The use of NSAIDs or aspirin has increased dramatically in recent decades, and the prevalence of NSAID use in patients aged ≥ 65 years is reported to be as high as 96%[22,23]. The proportion of drug-related PUD revealed an increasing trend, and it was prominent in the old-age group. The drug-related PUD group included more elderly patients and showed comorbidities and exposure to concomitant ulcerogenic drugs compared with the other groups, consistent with previous reports[24]. Drug-related PUD may cause serious complications, including bleeding or perforation[25]. Clinical practice guidelines for the appropriate treatment and prevention of drug-related PUD have been recently developed[26,27]. The guidelines recommend high-risk patients who are on long-term NSAID medications receive low-dose PPIs to prevent PUD and its complications; however, evidence in patients who take multiple ulcerogenic drugs remains lacking[26]. In a previous case series analysis from seven population-based healthcare databases, concomitant use of NSAIDs or aspirin with selective serotonin reuptake inhibitors, aldosterone antagonists, corticosteroids, or anticoagulants significantly increased the risk of upper gastrointestinal bleeding[28]. Our results suggest that drug-induced PUD may have more severe clinical outcomes; therefore, further strategies should be investigated to prevent complications in elderly patients.
The proportion of idiopathic PUD was 22.1% in our study, which is consistent with the proportion in the previous multicenter prospective study in 2008[9] and higher than that in the study by Chung et al[8] (8.6%) of patients with PUB in Korea[12]. Idiopathic PUD can be defined after excluding the missed diagnosis of H. pylori infection and undocumented use of NSAIDs or aspirin; therefore, the definition and diagnosis of H. pylori infection differed among the previous studies. Epidemiological studies have consistently reported an increasing proportion of H. pylori-negative PUD, particularly in Asian countries[8]; however, most of these studies were conducted before 2014, and few large-scale studies have investigated the changing trends or characteristics of idiopathic PUD in recent years. Our idiopathic PUD group included patients who had no exposure to aspirin, NSAIDs, or H. pylori eradication therapy before the index date. In our study, the exact results of the H. pylori tests could not be obtained, and patients with idiopathic PUD may overlap with those with drug-induced PUD. Despite these limitations, our study was the first to demonstrate the increasing trend of idiopathic PUD in old age in the past decade. In addition, we confirmed that the proportion of idiopathic PUD may differ regionally depending on the regional H. pylori prevalence.
The proportions of most of the comorbidities and drug exposures were higher in drug-induced PUD in our study, and only chronic liver disease was significantly higher in patients with idiopathic PUD among the three groups. Previous studies have compared the characteristics of idiopathic PUD with those of H. pylori-related PUD. The risks for idiopathic PUD included older age, smoking, alcohol, comorbid diseases, and higher psychological stress[8]. In our study, among three PUD groups, only the proportion of chronic liver disease was significantly higher in the idiopathic PUD; therefore, it may be a distinct characteristic compared with drug-induced PUD. The relationship between idiopathic PUD and liver disease has been suggested in several studies. Kim et al[29] have reported that despite the decreased H. pylori infection in patients with severe liver cirrhosis, PUD was increased in 288 patients with liver cirrhosis. Therefore, factors other than H. pylori infection may be involved in the pathogenesis of PUD in patients with cirrhosis[29,30]. A proposed patho-physiological mechanism is that portal hypertension induces splanchnic vascular congestion followed by gastrointestinal mucosal changes involving impaired mucosal secretion and microvascular flow, leading to peptic ulcer formation[31]. Moreover, we demonstrated that alcoholic liver disease was more prevalent in idiopathic PUD, suggesting that alcohol may be another risk factor for idiopathic PUD, although the causal relationship is uncertain.
Our study had several limitations. First, the proportion of idiopathic PUD may have been overestimated since we could not identify the exact H. pylori infection or confirmation after H. pylori eradication using an administrative database. However, this limitation may be overcome by converting text data to CDM in future studies. Second, our study was not conducted nationwide; therefore, we could not demonstrate the PUD trend as a proportion of the total patients. However, we observed that the pattern or severity of PUD may vary according to the scale of each hospital. Third, patients may overlap across hospital databases. Patients may be diagnosed with PUD in one hospital and treated in another. Fourth, the claims data-based research design may include misclassification bias or inaccurate data. Lastly, we could not include data on smoking or alcohol consumption; therefore, it could not be evaluated as a cause of idiopathic PUD.
Despite these limitations, our study had the following strengths. The main strength is that the analysis was performed using the OMOP-CDM database, which can be applied to other databases worldwide with the same analytic code. Second, our study used the operational definition of PUD based on a previous validation study, which showed high sensitivity and specificity[19]. Lastly, our study confirmed the changing trends and characteristics of PUD according to etiology and age group in the past 10 years using a large-scale multicenter design.
In conclusion, PUD exhibited an increasing trend in the old-age group in the past decade. Regarding etiology, H. pylori-related PUD decreased, whereas drug-related and idiopathic PUD increased, particularly in the old-age group. With the rising number of older patients, the effects of concomitant ulcerogenic drugs on PUD should be investigated, and preventive strategies for drug-induced PUD should be developed. Further studies are required to clarify the relationship between idiopathic PUD and chronic liver disease.
To date, few large-scale studies have comprehensively investigated the recent changing trends and clinical characteristics of peptic ulcer disease (PUD), including the multiple risk factors.
The incidence of idiopathic PUD, has increased in recent years, particularly in Asian countries. The clinical outcomes of idiopathic PUD revealed recurrent ulcer bleeding and higher mortality in previous studies; however, characteristics of idiopathic PUD remain poorly understood and warrant further investigation.
We aimed to evaluate the changing trends and characteristics of PUD according to age and etiology.
We analyzed seven hospital databases that were converted to a common data model between 2010 and 2019. We classified PUD patients who underwent rapid urease testing or Helicobacter pylori (H. pylori) serology testing into the following three groups according to etiology: (1) H. pylori-related; (2) drug-related [H. pylori-negative and nonsteroidal anti-inflammatory drugs (NSAIDs)/aspirin-related]; and (3) Idiopathic (H. pylori/NSAID/aspirin-negative) PUD.
The overall number of PUD exhibited no decrease, whereas PUD in old age revealed an increasing trend. H. pylori-related PUD exhibited a decreasing trend after 2014, drug-related PUD demonstrated an increasing trend, and idiopathic PUD showed an increasing trend in the old-age group during 10 years. The idiopathic PUD group had a significantly higher number of patients with chronic liver disease.
There was an increase in the incidence of PUD in the older age group during the last decade. There was a decrease in H. pylori-related PUD and an increase in drug-related and idiopathic PUD, especially in the elderly group.
Further preventive strategies for drug-induced PUD should be developed. Further studies are required to clarify the relationship between idiopathic PUD and chronic liver disease.
We acknowledge to Dr. Kee Myung Lee (Department of Gastroenterology, Ajou University School of Medicine, Suwon, Korea), Dr. Ji Min Han (Department of Internal Medicine, Daegu Catholic University Medical Center, Daegu, Korea), Dr. Ki-Nam Shim (Department of Internal Medicine, Ewha Womans University College of Medicine, Seoul, Korea), Dr. Chang Min Lee (Department of Internal Medicine, Gyeongsang National University Hospital, Gyeongsang National University, College of Medicine, Jinju, Korea), Dr. Sung Chul Park (Department of Internal Medicine, Kangwon National University School of Medicine, Chuncheon, Korea), and Dr. Suck Chei Choi (Department of Internal Medicine, Digestive Disease Research Institute, Wonkwang University College of Medicine, Iksan, Korea) for supplying the CDM data. We thank Jinseob Kim, MD (CEO, Zarathu), for his statistical advice.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C, C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Shelat VG, Singapore; Shiryajev YN, Russia; Skrypnyk I, Ukraine; Sugimoto M, Japan S-Editor: Wang JJ L-Editor: A P-Editor: Yu HG
| 1. | Lanas A, Chan FKL. Peptic ulcer disease. Lancet. 2017;390:613-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 399] [Cited by in RCA: 561] [Article Influence: 70.1] [Reference Citation Analysis (37)] |
| 2. | Xie X, Ren K, Zhou Z, Dang C, Zhang H. The global, regional and national burden of peptic ulcer disease from 1990 to 2019: a population-based study. BMC Gastroenterol. 2022;22:58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 101] [Article Influence: 33.7] [Reference Citation Analysis (0)] |
| 3. | Kim YS, Lee J, Shin A, Lee JM, Park JH, Jung HY. A Nationwide Cohort Study Shows a Sex-Dependent Change in the Trend of Peptic Ulcer Bleeding Incidence in Korea between 2006 and 2015. Gut Liver. 2021;15:537-545. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 4. | Sung JJ, Kuipers EJ, El-Serag HB. Systematic review: the global incidence and prevalence of peptic ulcer disease. Aliment Pharmacol Ther. 2009;29:938-946. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 263] [Cited by in RCA: 271] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 5. | Lanas A, García-Rodríguez LA, Polo-Tomás M, Ponce M, Quintero E, Perez-Aisa MA, Gisbert JP, Bujanda L, Castro M, Muñoz M, Del-Pino MD, Garcia S, Calvet X. The changing face of hospitalisation due to gastrointestinal bleeding and perforation. Aliment Pharmacol Ther. 2011;33:585-591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 125] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 6. | Malmi H, Kautiainen H, Virta LJ, Färkkilä N, Koskenpato J, Färkkilä MA. Incidence and complications of peptic ulcer disease requiring hospitalisation have markedly decreased in Finland. Aliment Pharmacol Ther. 2014;39:496-506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 7. | Leow AH, Lim YY, Liew WC, Goh KL. Time trends in upper gastrointestinal diseases and Helicobacter pylori infection in a multiracial Asian population--a 20-year experience over three time periods. Aliment Pharmacol Ther. 2016;43:831-837. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 52] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 8. | Chung CS, Chiang TH, Lee YC. A systematic approach for the diagnosis and treatment of idiopathic peptic ulcers. Korean J Intern Med. 2015;30:559-570. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 34] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 9. | Jang HJ, Choi MH, Shin WG, Kim KH, Chung YW, Kim KO, Park CH, Baek IH, Baik KH, Kae SH, Kim HY. Has peptic ulcer disease changed during the past ten years in Korea? A prospective multi-center study. Dig Dis Sci. 2008;53:1527-1531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 53] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 10. | McColl KE. Helicobacter pylori-negative nonsteroidal anti-inflammatory drug-negative ulcer. Gastroenterol Clin North Am. 2009;38:353-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Wong GL, Wong VW, Chan Y, Ching JY, Au K, Hui AJ, Lai LH, Chow DK, Siu DK, Lui YN, Wu JC, To KF, Hung LC, Chan HL, Sung JJ, Chan FK. High incidence of mortality and recurrent bleeding in patients with Helicobacter pylori-negative idiopathic bleeding ulcers. Gastroenterology. 2009;137:525-531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 92] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 12. | Chung WC, Jeon EJ, Kim DB, Sung HJ, Kim YJ, Lim ES, Kim MA, Oh JH. Clinical characteristics of Helicobacter pylori-negative drug-negative peptic ulcer bleeding. World J Gastroenterol. 2015;21:8636-8643. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 11] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 13. | Wong GLH, Lau LHS, Ching JYL, Tse YK, Ling RHY, Wong VWS, Chiu PWY, Lau JYW, Chan FKL. Prevention of recurrent idiopathic gastroduodenal ulcer bleeding: a double-blind, randomised trial. Gut. 2020;69:652-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (1)] |
| 14. | Hung LC, Ching JY, Sung JJ, To KF, Hui AJ, Wong VW, Leong RW, Chan HL, Wu JC, Leung WK, Lee YT, Chung SC, Chan FK. Long-term outcome of Helicobacter pylori-negative idiopathic bleeding ulcers: a prospective cohort study. Gastroenterology. 2005;128:1845-1850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 75] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 15. | Kim Y, Seo SI, Lee KJ, Kim J, Yoo JJ, Seo WW, Shin WG. Risks of long-term use of proton pump inhibitor on ischemic vascular events: A distributed network analysis of 5 real-world observational Korean databases using a common data model. Int J Stroke. 2023;18:590-598. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (1)] |
| 16. | Park DH, Seo SI, Lee KJ, Kim J, Kim Y, Seo WW, Lee HS, Shin WG, Yoo JJ. Long-term proton pump inhibitor use and risk of osteoporosis and hip fractures: A nationwide population-based and multicenter cohort study using a common data model. J Gastroenterol Hepatol. 2022;37:1534-1543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 17. | Seo WW, Seo SI, Kim Y, Yoo JJ, Shin WG, Kim J, You SC, Park RW, Park YM, Kim KJ, Rhee SY, Park M, Jin ES, Kim SE. Impact of pitavastatin on new-onset diabetes mellitus compared to atorvastatin and rosuvastatin: a distributed network analysis of 10 real-world databases. Cardiovasc Diabetol. 2022;21:82. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 29] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 18. | Hripcsak G, Duke JD, Shah NH, Reich CG, Huser V, Schuemie MJ, Suchard MA, Park RW, Wong IC, Rijnbeek PR, van der Lei J, Pratt N, Norén GN, Li YC, Stang PE, Madigan D, Ryan PB. Observational Health Data Sciences and Informatics (OHDSI): Opportunities for Observational Researchers. Stud Health Technol Inform. 2015;216:574-578. [PubMed] |
| 19. | Lee JW, Kim HK, Woo YS, Jahng J, Jin YR, Park JH, Kim YS, Jung HY. [Optimal Operational Definition of Patient with Peptic Ulcer Bleeding for Big Data Analysis Using Combination of Clinical Characteristics in a Secondary General Hospital]. Korean J Gastroenterol. 2016;68:77-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Lim SH, Kim N, Kwon JW, Kim SE, Baik GH, Lee JY, Park KS, Shin JE, Song HJ, Myung DS, Choi SC, Kim HJ, Yim JY, Kim JS. Trends in the seroprevalence of Helicobacter pylori infection and its putative eradication rate over 18 years in Korea: A cross-sectional nationwide multicenter study. PLoS One. 2018;13:e0204762. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 66] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 21. | Chua BQY, Chong VWS, Teng TZJ, Chia CTW, Aung MO, Shelat VG. Does technology-enhanced communication improve Helicobacter pylori eradication outcomes?-A meta-analysis. Helicobacter. 2022;27:e12890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 22. | Pilotto A, Franceschi M, Leandro G, Di Mario F; Geriatric Gastroenterology Study Group (Societè Italiana Gerontologie Geriatria). NSAID and aspirin use by the elderly in general practice: effect on gastrointestinal symptoms and therapies. Drugs Aging. 2003;20:701-710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 73] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 23. | Wongrakpanich S, Wongrakpanich A, Melhado K, Rangaswami J. A Comprehensive Review of Non-Steroidal Anti-Inflammatory Drug Use in The Elderly. Aging Dis. 2018;9:143-150. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 564] [Cited by in RCA: 512] [Article Influence: 73.1] [Reference Citation Analysis (0)] |
| 24. | Zullo A, Hassan C, Campo SM, Morini S. Bleeding peptic ulcer in the elderly: risk factors and prevention strategies. Drugs Aging. 2007;24:815-828. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 53] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 25. | Yang YJ, Bang CS, Shin SP, Park TY, Suk KT, Baik GH, Kim DJ. Clinical characteristics of peptic ulcer perforation in Korea. World J Gastroenterol. 2017;23:2566-2574. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 26. | Joo MK, Park CH, Kim JS, Park JM, Ahn JY, Lee BE, Lee JH, Yang HJ, Cho YK, Bang CS, Kim BJ, Jung HK, Kim BW, Lee YC; Korean College of Helicobacter Upper Gastrointestinal Research. Clinical Guidelines for Drug-Related Peptic Ulcer, 2020 Revised Edition. Gut Liver. 2020;14:707-726. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 27. | Kamada T, Satoh K, Itoh T, Ito M, Iwamoto J, Okimoto T, Kanno T, Sugimoto M, Chiba T, Nomura S, Mieda M, Hiraishi H, Yoshino J, Takagi A, Watanabe S, Koike K. Evidence-based clinical practice guidelines for peptic ulcer disease 2020. J Gastroenterol. 2021;56:303-322. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 149] [Cited by in RCA: 141] [Article Influence: 35.3] [Reference Citation Analysis (0)] |
| 28. | Masclee GM, Valkhoff VE, Coloma PM, de Ridder M, Romio S, Schuemie MJ, Herings R, Gini R, Mazzaglia G, Picelli G, Scotti L, Pedersen L, Kuipers EJ, van der Lei J, Sturkenboom MC. Risk of upper gastrointestinal bleeding from different drug combinations. Gastroenterology. 2014;147:784-792.e9; quiz e13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 107] [Article Influence: 9.7] [Reference Citation Analysis (35)] |
| 29. | Kim DJ, Kim HY, Kim SJ, Hahn TH, Jang MK, Baik GH, Kim JB, Park SH, Lee MS, Park CK. Helicobacter pylori infection and peptic ulcer disease in patients with liver cirrhosis. Korean J Intern Med. 2008;23:16-21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 30. | Kirk AP, Dooley JS, Hunt RH. Peptic ulceration in patients with chronic liver disease. Dig Dis Sci. 1980;25:756-760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 51] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 31. | Bang CS, Baik GH, Kim JH, Kim JB, Suk KT, Yoon JH, Kim YS, Kim DJ. Peptic ulcer disease in liver cirrhosis and chronic hepatitis: impact of portal hypertension. Scand J Gastroenterol. 2014;49:1051-1057. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |