Published online Aug 7, 2022. doi: 10.3748/wjg.v28.i29.3934
Peer-review started: March 17, 2022
First decision: April 11, 2022
Revised: April 25, 2022
Accepted: July 5, 2022
Article in press: July 5, 2022
Published online: August 7, 2022
Processing time: 138 Days and 21.7 Hours
Biliary decompression is well known to greatly decrease the risks of mortality in acute cholangitis (AC). Although early biliary drainage is recommended by the treatment guidelines for AC, the best time for performing this procedure is yet to be established. Furthermore, since the clinical outcomes of patients with severe AC vary dramatically, screening for patients that could benefit the most from early drainage would be more beneficial than the drainage performed based on the severity grade criteria.
To investigate the optimal drainage timing for AC patients with each disease severity grade and organ dysfunction.
In this retrospective monocenter cohort analysis, we reviewed 1305 patients who were diagnosed with AC according to the Tokyo guidelines 2018 at a Chinese tertiary hospital between July 2016 and December 2020. Demographic characteristics including age and sex, clinical and laboratory characteristics, and imaging findings of each patient were obtained from electronic medical records. We investigated the all-cause in-hospital mortality (IHM), hospital length of stay (LOS), and hospitalization costs associated with the timing of biliary drainage according to the severity grading and different dysfunctioning organs and predictors [age, white blood cell (WBC) count, total bilirubin, albumin, lactate, malignant obstruc
Biliary drainage within 24 or 48 h in Grade III AC patients could dramatically decrease IHM (3.9% vs 9.0%, P = 0.041; 4% vs 9.9%, P = 0.018, respectively), while increasing LOS and hospitalization costs. Multivariate logistic analysis revealed that neurological, respiratory, renal, and cardiovascular dysfunctions, hypoalbuminemia, and malignant obstruction were significantly associated with IHM (odds ratio = 5.32, 2.541, 6.356, 4.021, 5.655, and 7.522; P < 0.001, P = 0.016, P < 0.001, P = 0.012, P < 0.001, and P < 0.001; respectively). Biliary decompression performed within 12 h of admission significantly decreased the IHM in AC patients with neurological dysfunction (0% vs 17.3%, P = 0.041) or with serum lactate > 2 mmol/L (0% vs 5.4%, P = 0.016). In the subgroup of AC patients with renal dysfunction, abnormal WBC count, hyperbilirubinemia, or hypoalbuminemia, early drainage (< 24 h) reduced the IHM (3.6% vs 33.3%, P = 0.004; 1.9% vs 5.8%, P = 0.031; 1.7% vs 5.0%, P = 0.019; 0% vs 27%, P = 0.026; respectively). The IHM was lower in patients with AC combined with hepatic dysfunction, malignant obstruction, or a CCI > 3 who had undergone biliary drainage within 48 h (2.6% vs 20.5%, P = 0.016; 3.0% vs 13.5%, P = 0.006; 3.4% vs 9.6%, P = 0.021; respectively).
Biliary drainage within 12 h is beneficial for AC patients with neurological or cardiovascular dysfunction, while complete biliary decompression within 24 h of admission is recommended for treating patients with Grade III AC.
Core Tip: This study aimed to investigate the optimal timing of drainage for patients with acute cholangitis (AC) with each grade and organ dysfunction. We first attempted to study whether AC patients with different organ dysfunction should undergo biliary drainage at distinct times. We believe that our study makes a significant contribution to the literature because we found that patients with severe AC should complete biliary decompression within 24 h of admission, while biliary drainage within 12 h was beneficial for AC patients with neurological or cardiovascular dysfunction.
- Citation: Lu ZQ, Zhang HY, Su CF, Xing YY, Wang GX, Li CS. Optimal timing of biliary drainage based on the severity of acute cholangitis: A single-center retrospective cohort study. World J Gastroenterol 2022; 28(29): 3934-3945
- URL: https://www.wjgnet.com/1007-9327/full/v28/i29/3934.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i29.3934
Acute cholangitis (AC) is a life-threatening condition that occurs in the presence of biliary obstruction. Although growing evidence confirms that biliary decompression can dramatically decrease the mortality rates associated with AC, the optimal time for biliary drainage remains controversial[1-3]. Most experts agree that the timeframe for biliary decompression is distinct for different severity grades based on the Tokyo guidelines 2018/2013 (TG18/13), which recommend early biliary drainage for Grade II AC and urgent biliary drainage for Grade III AC; however, the exact timeframe is unclear[4]. Moreover, the 2019 European Society of Gastrointestinal Endoscopy guidelines recommend biliary drainage as soon as possible in patients with Grade III AC and within 12 h for patients with septic shock, while within 48–72 h for patients with Grade II AC[2]. Meanwhile, the 2021 American Society of Gastrointestinal Endoscopy (ASGE) guidelines suggest endoscopic retrograde cholangiopancreatography (ERCP) within 48 h in AC patients, regardless of severity[1]. Some studies have demonstrated a “the earlier, the better” approach for the management of AC cases[5-8]. They deemed urgent biliary decompression necessary in severe cases. However, other studies have shown that ERCP can be safely delayed to allow for sufficient resuscitation[9-11]. In our clinical experience, the severity of Grade III AC varies dramatically, and we have observed that the optimal timing of biliary decompression may vary for different organ injuries.
So far, no relevant study has determined whether the clinical outcomes of Grade III AC patients vary with different organ injuries and whether AC patients with different organ dysfunction should undergo biliary drainage at distinct times. Consequently, this single-center retrospective study aimed to investigate the relationship between drainage timing and in-hospital mortality (IHM) in patients with AC of different severities, and attempted to stratify patients with AC to identify the best decompression time.
Ethical compliance: This retrospective cohort study was conducted according to the tenets of the Declaration of Helsinki, and approved by the Bioethics Committee of Beijing Friendship Hospital, Capital Medical University (Certification No. 2020-P2-224-01). After the review conducted by the Ethics Committee, the need for informed consent was waived.
Sample size: Based on the pre-experimental results, which revealed a 0.87% and 3% mortality rates for patients who did and did not undergo biliary drainage, respectively, we calculated the sample size using PASS 15.0 with Power = 0.8, Alpha = 0.05, and N1 = N2. The resultant sample size was 1306. On this basis, we expanded the sample size by 15% to exclude the reduction caused by data deficiency or diagnostic errors.
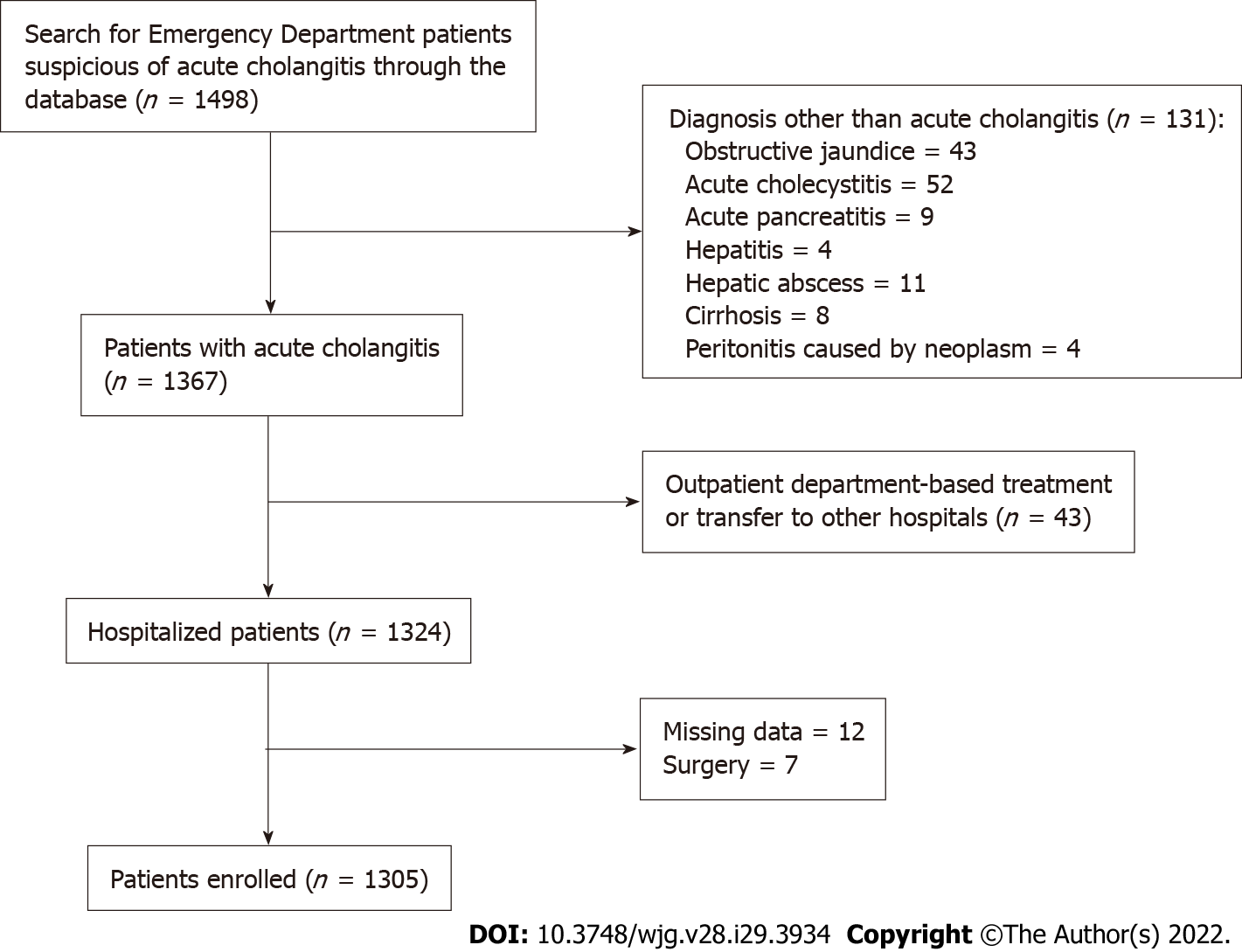
Enrollment: We searched the electronic medical record database of the Beijing Friendship Hospital for all adult (> 18 years) non-pregnant patients visiting the Emergency Department (ED) between July 2016 and December 2020 who were discharged with a diagnosis of AC. A total of 1498 patients were included in the study. All the medical records were reviewed and a diagnosis of AC was confirmed according to the TG18 diagnostic criteria[12]. Besides pregnant women and patients aged < 18 years, we also excluded patients transferred to other hospitals or outpatient departments for treatment and patients whose medical data were incomplete or missing. Finally, 1305 patients were enrolled (Figure 1).
Demographic data, including age and sex, were obtained for each patient. Clinical data, laboratory characteristics, and imaging findings were obtained from the electronic medical records. Clinical data included vital signs, fluid output, Glasgow coma score, the vasoactive drug dose, history of biliary disease, Charlton comorbidity index (CCI), etiology of AC, registration time at the ED, time and type of drainage, discharge time, complications of drainage, hospitalization cost, and IHM. Laboratory findings included white blood cell (WBC) count, platelet count, total bilirubin, albumin, aspartate transaminase, alanine transaminase, creatinine, amylase, prothrombin time-international normalized ratio, arterial blood oxygen pressure, and lactate. Computed tomography, magnetic resonance cholangiopancreatography, or ERCP findings were reviewed to determine the etiology of cholangitis. The time interval for biliary drainage was calculated as the difference between ED registration time and the time of ERCP or percutaneous transhepatic biliary drainage (PTBD). We used the TG18 severity criteria for grading the severity[12].
Benign stenosis was defined as stenosis in the biliary ducts without radiological findings of metastasis or malignant cells on histological examination. The indications of ERCP were AC combined with persistent extrahepatic biliary obstruction, and cases of anatomical derangement, failed ERCP, intrahepatic biliary obstruction underwent PTBD. The contraindications of ERCP included acute coronary syndrome, acute heart failure (New York Heart Association class III-IV), acute stroke occurring within 2 wk prior to enrollment, and acute pulmonary embolism complicated with the arterial PaO2 <60 mmHg, while the contraindications of PTBD were platelet count < 50000/mm3 or prothrombin activity < 60%. The adverse effects after drainage were based on the lexicon guidelines of the ASGE[13]. The second treatment included a second ERCP and a second PTBD for stone removal or stent placement. The need for a second therapeutic ERCP was assessed per the discretion of the experienced operators who performed the intervention and based on 2018 ERCP Guidelines for China[14]. All of the endoscopists had independently completed 300 ERCP interventions per year for 3 years.
Our primary outcome was IHM, and the secondary outcomes were hospital length of stay (LOS) and hospitalization costs. When analyzing the survivors’ LOS and entailed cost, we excluded patients who died or were transferred to other hospitals. We investigated the primary and secondary outcomes relevant to the timing of biliary drainage according to severity grading and some predictors based on TG18 and other previous studies.
Continuous variables were reported as medians with interquartile ranges (IQR) for not normally distributed; categorical variables were expressed as numbers and percentages. Comparisons between groups for continuous variables were evaluated using the Kruskal–Wallis test and Mann–Whitney U test, and for categorical variables, Fisher’s exact test was used. Univariate logistic regression analysis and multivariate logistic regression with stepwise variable selection were used to analyze the relationship between organ dysfunction or predictors and IHM. Odds ratios (ORs) and 95% confidence intervals were calculated. Statistical significance was set at P < 0.05. Statistical analyses were conducted using SPSS v22.
The characteristics of the study population are shown in Tables 1 and 2. This cohort included 1305 patients, the majority of whom were men (60%). The median age of the group was 74 years (IQR, 63-82 years), and patients with Grade I AC were significantly younger (P < 0.001). The CCI of individuals with Grade III cholangitis was significantly higher than that of patients with Grade I or II cholangitis (P < 0.001). Choledocholithiasis (69.4%) was the most common cause of cholangitis, followed by malignant obstruction (18.5%). Among patients with cholangitis caused by malignancy, the number of patients with Grade II cholangitis was higher than that of patients with Grade I or III cholangitis. More patients with Grade II AC underwent biliary decompression (P = 0.006), while the IHM and hospitalization costs were significantly higher in the Grade III AC group than in the Grade I and II AC groups (IHM: P < 0.001, hospitalization costs: P < 0.001). Deaths tended to occur earlier in the disease course in patients with Grade III AC (median time 6 d).
| Characteristics, n (%) | Total (n = 1305) | Grade I (n = 433) | Grade II (n = 405) | Grade III (n = 467) | P value |
| Age (yr)-median (IQR) | 74 (63-82) | 66 (59-72.5) | 79 (69-84) | 77 (66-83) | < 0.001 |
| Male, n (%) | 783 (60) | 276 (63.7) | 240 (59.3) | 267 (57.2) | 0.123 |
| CCI- median (IQR) | 2 (1-4) | 2 (1-3) | 2 (1-4) | 3 (1-5) | < 0.001 |
| Etiology, n (%) | < 0.001 | ||||
| Choledocholithiasis | 906 (69.4) | 315 (72.7) | 252 (62.2) | 339 (72.6) | |
| Malignant obstruction | 242 (18.5) | 73 (16.9) | 97 (24.0) | 72 (15.4) | |
| Benign stenosis | 94 (7.2) | 27 (6.2) | 42 (10.4) | 25 (5.4) | |
| Others | 63 (4.8) | 18 (4.2) | 14 (3.5) | 31 (6.6) | |
| Biliary drainage, n (%) | 915 (70.1) | 302 (69.7) | 306 (75.6) | 307 (65.7) | 0.006 |
| LOS (d)-median (IQR) | 11 (8-14) | 11 (8-14) | 11 (7.5-14) | 12 (7-15) | 0.110 |
| Hospitalization cost (CNY)-median (IQR) | 38784.37 (22744.31-53278.63) | 36536.36 (20851.37-47274.77) | 38308.33 (23452.14-52847.29) | 41832.19 (23355.98-58145.52) | < 0.001 |
| IHM, n (%) | 41 (3.1) | 1 (0.2) | 7 (1.7) | 33 (7.1) | < 0.001 |
| Survival time of dead (d)-median (IQR) | 8 (3-23.5) | 9 | 23 (13-46) | 6 (3-17) | 0.024 |
| Organ dysfunction | |||||
| Neurological dysfunction | 126 | 0 | 0 | 126 | < 0.001 |
| Respiratory dysfunction | 227 | 0 | 0 | 227 | < 0.001 |
| Renal dysfunction | 64 | 0 | 0 | 64 | < 0.001 |
| Cardiovascular dysfunction | 39 | 0 | 0 | 39 | < 0.001 |
| Hematological dysfunction | 149 | 0 | 0 | 149 | < 0.001 |
| Hepatic dysfunction | 83 | 0 | 0 | 83 | < 0.001 |
| Temperature (℃)-median (IQR) | 37.0 (36.6-38) | 36.8 (36.6-37.8) | 37 (36.6-38.25) | 37.2 (36.6-38.3) | 0.001 |
| Laboratory values | |||||
| WBC (/mm3)-median (IQR) | 10560 (7705-14305) | 9120 (7160-11165) | 12700 (8897-18441) | 11140 (7870-15810) | < 0.001 |
| T-Bil (mg/dL)-median (IQR) | 99.81 (62.43-155.76) | 69.28 (49.625-120.975) | 121.74 (88.97-184.41) | 1041.2 (67.74-156.31) | < 0.001 |
| Albumin (g/L)-median (IQR) | 35.4 (31.2-39.2) | 37.5 (34.2-40.4) | 34.9 (30.8-38.1) | 33.6 (29.2-37.8) | < 0.001 |
| Lactate (mmol/L)-median (IQR) | 2.15 (1.6-3.4) | 1.8 (1.4-2.7) | 2.1 (1.5-2.8) | 2.4 (1.7-4.1) | < 0.001 |
| Characteristics, n (%) | Total (n = 915) | Grade I (n = 302) | Grade II (n = 306) | Grade III (n = 307) | P value |
| Drainage method, n (%) | 0.001 | ||||
| ERCP | 830 (90.7) | 289 (95.7) | 269 (87.9) | 272 (88.6) | |
| PTBD | 85 (9.3) | 13 (4.3) | 37 (12.1) | 35 (11.4) | |
| Timing of drainage (hours)- median (IQR), n (%) | 24.0 (60.0) | 26.4 (62.4) | 26.4 (62.4) | 21.6 (45.6) | 0.001 |
| Biliary drainage within, n (%) | 0.001 | ||||
| 12 h | 212 (23.2) | 54 (17.9) | 69 (22.5) | 89 (29.0) | |
| 12-24 h | 233 (25.5) | 74 (24.5) | 70 (22.9) | 89 (29.0) | |
| 24-48 h | 172 (18.8) | 71 (23.5) | 54 (17.6) | 47 (15.3) | |
| > 48 h | 298 (32.6) | 103 (34.1) | 113 (36.9) | 82 (26.7) | |
| Second intervention, n (%) | 478 (52.2) | 159 (52.6) | 154 (50.3) | 165 (53.7) | 0.688 |
| Drainage outside working hours, n (%) | 207 (22.6) | 49 (16.2) | 60 (19.6) | 98 (31.9) | < 0.001 |
| Adverse events, n (%) | |||||
| Pancreatitis | 75 (8.2) | 23 (7.6) | 23 (7.5) | 29 (9.4) | 0.643 |
| Cholangitis | 8 (0.9) | 2 (0.7) | 2 (0.7) | 4 (1.3) | 0.742 |
| Perforation | 7 (0.8) | 1 (0.3) | 2 (0.7) | 0 (0) | 0.440 |
| Bile leak | 4 (0.4) | 2 (0.7) | 1 (0.3) | 1 (0.3) | 0.701 |
| Myocardial infarction | 5 (0.5) | 0 (0) | 3 (1.0) | 2 (0.7) | 0.339 |
A total of 915 patients in this cohort (70.1%) underwent biliary decompression, most of whom underwent endoscopic interventions (90.7%), while more patients underwent PTBD in the severe AC groups (Grade II: 37 cases, Grade III: 35 cases vs Grade I: 13 cases, P = 0.001). One hundred and sixty patients with Grade III were treated with antibiotics and fluid infusion only (disagreement about procedures = 35 cases, including two of mortality; with contraindications = 24 cases, including five of death; not tolerable conditions = 14 cases, including eight of death; obstruction spontaneous relief = 67 cases, including seven of mortality; not persistent biliary obstruction with high risk to stone removal by ERCP = 15 cases without death; not persistent biliary obstruction with selective cholecystectomy = five cases without death). The median drainage time was 24 h. Nearly half of the patients underwent biliary drainage within 24 h (445/915, 48%), while 89 patients with Grade III underwent drainage within 12 h (29%), which was significantly higher than that in Grades I and II (P = 0.04). Among the patients who underwent biliary drainage, more patients in Grade III underwent biliary drainage outside regular working hours (31.9%) and 478 patients (52.2%) required a second intervention for stone removal or stent placement, which exhibited no relationship with severity (P = 0.688). Post-ERCP pancreatitis was the major adverse event (8.2%), and the incidence of adverse events was not significantly different among the three severity grades.
The association of the IHM, LOS, and hospitalization costs with the timing of biliary drainage in each severity grade has been presented in Table 3. Biliary drainage significantly decreased the IHM in all AC patients (13/915 vs 28/390, P < 0.001). Among individuals with Grade III cholangitis, the IHM rate was significantly decreased in patients who had biliary drainage within 24 h or 48 h (P = 0.041, P = 0.018), while the LOS was significantly increased among those patients who underwent drainage within 12 h, 24 h, or 48 h (P < 0.001, P < 0.001, and P < 0.001, respectively). Hospitalization costs significantly increased for all patients with biliary drainage, regardless of severity criteria. For patients with Grade I AC, IHM was not affected by the timing of drainage and there was no relationship between LOS and the timing of biliary drainage for the survivors, but LOS was significantly extended in all the patients who underwent biliary drainage within 24 h or 48 h (P = 0.004, P = 0.002).
| Severity of AC | Characteristic-median (IQR) | Drainage | Absence of drainage | P value | Drainage < 12 h | Drainage > 12 h or absence | P value | Drainage < 24 h | Drainage > 24 h or absence | P value | Drainage < 48 h | Drainage > 48 h or absence | P value | |
| Grade I | IHM | 0/302 | 1/131 | 0.303 | 0/54 | 1/379 | 1.000 | 0/128 | 1/305 | 1.000 | 0/199 | 1/234 | 1.000 | |
| LOS (d) | 11 (9-15) | 7 (4-10) | < 0.001 | 11 (8-13.25) | 10 (8-14) | 0.778 | 11 (8-14) | 10 (7-14) | 0.004 | 11 (8-14) | 10 (6-14) | 0.002 | ||
| Survivors’ LOS (d) (n = 387) | 12 (9-15) | 8 (5-11) | < 0.001 | 11 (8-13.25) | 11 (8-14) | 0.794 | 11 (9-14) | 11 (8-14) | 0.065 | 11 (9-14) | 10 (8-14) | 0.101 | ||
| Hospitalization cost (CNY) | 42845.67 (33734.18-52209.23) | 15763.10 (7737.32-23680.31) | < 0.001 | 43328.59 (32863.61-49384.19) | 35317.71 (18848.59-46850.08 | 0.001 | 44154.19 (35638.76-52219.56) | 31292.68 (16269.75-44599.67) | < 0.001 | 42908.34 (33358.44-50564.68) | 25519.43 (12347.06-42424.96) | < 0.001 | ||
| Survivors’ hospitalization cost (CNY) (n = 387) | 42957.18 (33973.58-52224.73) | 16596.85 (9096.73-24755.65 | < 0.001 | 43462.72 (36174.00-49384.19) | 36604.86 (21962.98-47554.27) | 0.003 | 44443.3 (35988.02-52237.14) | 33492.6 (46019.17-18880.26) | < 0.001 | 43264.07 (34606.54-51093.62) | 29762.32 (16376.75-44463.21) | < 0.001 | ||
| Grade II | IHM | 2/306 | 5/99 | 0.011 | 0/69 | 7/336 | 0.608 | 0/139 | 7/266 | 0.101 | 1/193 | 6/212 | 0.125 | |
| LOS (d) | 11 (9-15) | 7 (4-12) | < 0.001 | 11 (8-14) | 11 (7-14) | 0.684 | 11 (9-14) | 10 (7-14) | 0.122 | 11 (8-14) | 10 (7-14.8) | 0.190 | ||
| Survivors’ LOS (d) (n = 349) | 12 (9-15) | 7.5 (4.75-11.25) | < 0.001 | 11.5 (9-14) | 11 (8-14) | 0.367 | 12 (10-14) | 11 (7-14) | 0.024 | 12 (9-14) | 11 (7-14) | 0.050 | ||
| Hospitalization cost (CNY) | 44033.13 (31071.05-56134.72) | 17626.20 (10037.69-25587.43) | < 0.001 | 45832.44 (36061.53-56949.37) | 36132.93 (21795.89-51453.62) | < 0.001 | 46789.09 (35989.59-57723.15) | 31505.72 (19948.31-47463.61) | < 0.001 | 45489.74 (33858.99-57600.43) | 29275.30 (16928.45-46255.47) | < 0.001 | ||
| Survivors’ hospitalization cost (CNY) (n = 349) | 45004.20 (32631.09-56660.62) | 16342.15 (10300.68-25017.80) | < 0.001 | 47938.00 (37937.29-58046.02) | 36629.15 (22828.93-51509.37) | < 0.001 | 48254.61 (37937.29-58929.51) | 31589.96 (20386.80-47062.76) | < 0.001 | 46564.37 (36191.07-57998.63) | 29338.38 (17687.02-45685.12) | < 0.001 | ||
| Grade III | IHM | 11/307 | 22/160 | < 0.001 | 3/89 | 30/378 | 0.168 | 7/178 | 26/289 | 0.041 | 9/225 | 24/242 | 0.018 | |
| LOS (d) | 13 (9-17) | 8 (3-12) | < 0.001 | 13 (11-19) | 11 (6-15) | < 0.001 | 13 (10-17) | 10 (6-14) | < 0.001 | 13 (9-17) | 9.5 (5-14) | < 0.001 | ||
| Survivors’ LOS (d) (n = 351) | 13 (11-18) | 9.5 (7-13.25) | <0.001 | 13 (12-19) | 12 (9-16) | 0.001 | 13 (11-17.75) | 12 (9-15) | < 0.001 | 13 (11-17.75) | 11 (8-15) | < 0.001 | ||
| Hospitalization cost | 51583.64 (38985.47-64886.01) | 20183.58 (11317.37-29525.99) | < 0.001 | 56599.94 (43260.73-70300.00) | 38527.58 (21034.79-55279.53) | < 0.001 | 55121.49 (40428.29-67707.01) | 31832.99 (17933.81-50037.89) | < 0.001 | 54295.52 (39252.57-65638.57) | 28165.23 (15708.29-45478.26) | < 0.001 | ||
| Survivors’ hospitalization cost (CNY) (n = 351) | 53507.33 (41027.94-65312.29) | 22909.77 (15594.93-31845.39) | < 0.001 | 57976.4 (50131.44-70333.71) | 43241.54 (28347.56-57860.29) | < 0.001 | 55873.84 (46654.40-69946.73) | 38973.06 (24292.41-53090.85) | < 0.001 | 55782.38 (43994.26-66493.67) | 34748.29 (21379.37-50147.24) | < 0.001 | ||
Univariate and multivariate analyses of predictors, including TG18 severity grading factors, lactate, CCI, and etiology of malignant obstruction, are shown in Table 4. In the univariate analysis, organ dysfunction, abnormal WBC count, hypoalbuminemia, CCI > 3, and etiology of malignancy were significantly associated with IHM. In a multivariate analysis of organ dysfunction, only neurological, respiratory, renal, and cardiovascular dysfunction, hypoalbuminemia, and malignant obstruction were significantly positively associated with IHM (OR = 5.32, 2.541, 6.356, 4.021, 5.655, and 7.522; P < 0.001, P = 0.016, P < 0.001, P = 0.012, P < 0.001, and P < 0.001, respectively).
| Predictors (n = 1305) | Univariate analysis | Multivariate analysis | Mortality to the timing of drainage | ||||||||||
| OR (95%CI) | P value | OR (95%CI) | P value | < 12 h | > 12 h or absence | P value | < 24 h | > 24 h or absence | P value | < 48 h | > 48 h or absence | P value | |
| Neurological dysfunction | 8.377 (4.384-16.007) | < 0.001 | 5.32 (2.373-11.931) | < 0.001 | 0/22 | 18/104 | 0.041 | 3/42 | 15/84 | 0.175 | 5/51 | 13/75 | 0.304 |
| Respiratory dysfunction | 2.886 (1.491-5.497) | 0.003 | 2.541 (1.189-5.43) | 0.016 | 1/44 | 14/183 | 0.314 | 4/91 | 11/136 | 0.414 | 6/117 | 9/110 | 0.428 |
| Renal dysfunction | 11.043 (5.402-22.573) | < 0.001 | 6.356 (2.623-15.397) | < 0.001 | 1/15 | 12/49 | 0.269 | 1/28 | 12/36 | 0.004 | 1/31 | 12/33 | 0.001 |
| Cardiovascular dysfunction | 11.569 (5.078-26.357) | < 0.001 | 4.021 (1.361-11.88) | 0.012 | 0/7 | 9/32 | 0.169 | 2/16 | 7/23 | 0.262 | 2/18 | 7/21 | 0.139 |
| Hematological dysfunction | 2.611 (1.253-5.441) | 0.02 | N/A | 2/37 | 8/104 | 1 | 3/61 | 7/88 | 0.527 | 3/74 | 7/75 | 0.327 | |
| Hepatic dysfunction | 5.263 (2.484-11.152) | < 0.001 | N/A | 0/15 | 10/68 | 0.196 | 1/30 | 9/53 | 0.086 | 1/39 | 9/44 | 0.016 | |
| Age (≥ 75 yr) | 1.432 (0.765-2.680) | 0.261 | N/A | 2/88 | 21/531 | 0.759 | 4/196 | 19/423 | 0.172 | 7/267 | 16/352 | 0.284 | |
| Temperature (≥ 39 ℃) | 0.390 (0.093-1.631) | 0.197 | N/A | 0/43 | 2/106 | 1 | 1/75 | 1/74 | 1 | 1/85 | 1/64 | 1 | |
| WBC (> 12000/mm3, < 4000/mm3) | 1.962 (1.043-3.688) | 0.036 | N/A | 1/107 | 23/445 | 0.063 | 4/207 | 20/342 | 0.031 | 6/278 | 18/275 | 0.012 | |
| T-Bil (≥ 5 mg/dL) | 1.711 (0.865-3.385) | 0.123 | N/A | 3/143 | 26/626 | 0.333 | 5/292 | 24/477 | 0.019 | 8/407 | 21/362 | 0.007 | |
| Albumin (< STD*0.7) | 10.715 (5.147-22.303) | < 0.001 | 5.655 (2.398-13.335) | < 0.001 | 0/8 | 12/51 | 0.188 | 0/15 | 12/44 | 0.026 | 1/24 | 11/35 | 0.018 |
| Lactate (≥ 2 mmol/L) | 1.450 (0.766-2.747) | 0.254 | N/A | 0/105 | 16/298 | 0.016 | 2/186 | 14/217 | 0.008 | 4/227 | 12/176 | 0.018 | |
| Malignant obstruction | 5.495 (2.924-10.325) | < 0.001 | 7.522 (3.504-16.149) | < 0.001 | 1/26 | 21/216 | 0.483 | 2/59 | 20/183 | 0.116 | 3/101 | 19/141 | 0.006 |
| CCI (> 3) | 4.080 (2.153-7.7340) | < 0.001 | N/A | 2/57 | 23/318 | 0.397 | 4/127 | 21/248 | 0.052 | 6/177 | 19/198 | 0.021 | |
From the data presented in Table 4, the association between IHM and the timing of biliary drainage for each clinical predictor is reflected. Among patients with AC complicated with neurological dysfunction or hyperlactatemia, the IHM rate was significantly decreased in individuals who underwent biliary decompression within 12 h (P = 0.041, P = 0.016), while those patients complicated with neurological dysfunction who had drainage within 24 h or 48 h could not improve prognosis compared with those who underwent drainage after 24 or 48 h, as well as those who did not undergo biliary drainage after admission (P = 0.175, P = 0.304). In patients with renal dysfunction, abnormal WBC count, hyperbilirubinemia, hypoalbuminemia, or hyperlactatemia, who had biliary decompression within 24 h or 48 h, there were significantly lower IHM rates than those of the remaining patients in each subgroup. Among patients with AC complicated with hepatic dysfunction, higher CCI (> 3), or malignancy, a lower IHM rate was significantly associated with early drainage (< 48 h) (P = 0.016, P = 0.006, P = 0.021).
In this retrospective monocenter cohort analysis including 1305 AC patients stratified according to TG18 severity criteria, early drainage (< 24 h) in Grade III AC patients had the greatest benefit, which could significantly reduce the all-cause IHM. It is worth noting that, in this subgroup, patients complicated with neurological dysfunction should be drained as early as possible (< 12 h). Moreover, early drainage was also required for AC patients with lactate more than 2 mmol/L, abnormal WBC count, hyperbilirubinemia, or hypoalbuminemia. Although these patients may have no severe cholangitis, early drainage could significantly reduce IHM and benefit the most. However, it should be noted that our results did not prove that drainage reduced hospitalization costs compared to conservative treatment. Furthermore, early drainage increased hospitalization costs and LOS.
AC is a clinically heterogeneous disease with recent mortality rates ranging from 2.7% to 10%, which is considered as an improvement since these rates were as high as 50%-60% in severe cases[15,16]. Although it is well-accepted that biliary decompression can significantly decrease the mortality of AC, it is highly debatable as to what the optimal strategy is for performing biliary drainage procedures. Should drainage occur as early as possible or should the procedure be delayed until stabilization after adequate resuscitation, especially for Grade III AC patients? Our study showed that biliary drainage could significantly decrease the IHM of AC patients (1.4% vs 7.2%, P < 0.001), and AC patients of Grade III underwent decompression within 24 h or 48 h had lower IHM (3.9% vs 9.0%, P = 0.041; 4% vs 9.9%, P = 0.018). These findings are in line with the results of a large sample size retrospective study, which showed that drainage within 48 h was associated with improved IHM (3.4% vs 10.2%, P = 0.019)[17], although it did not discuss drainage within 24 h. Another retrospective study of 6063 patients with AC conducted by Kiriyama et al[3] reported a distinct result: decompression within 24 h or 48 h improved the 30-d mortality rate only among Grade II patients (drainage within 24 h vs. after 24 h or no drainage: 1.7% vs 3.4%, P < 0.05; drainage within 48 h vs after 48 h or no drainage: 2.0% vs 3.7%, P < 0.05), and the drainage timing did not influence 30-d mortality in patients with Grade I and Grade III. This dissimilarity may be because we reviewed the all-cause IHM, while Kiriyama et al's study observed 30-d cholangitis-caused mortality, and the mortality rate of Grade III AC patients was lower than that in our study (5.1% vs 9.4%), especially for subgroups of delayed decompression in which more patients died from malignancy[3]. In addition, as the number and grade of patients without drainage were not shown in the results of Kiriyama et al[3], the proportion of patients without drainage in our study may be different from the group studied by Kiriyama et al[3]. Since then, few researchers have tried to examine the possibility of improving the prognosis of Grade III AC patients by undergoing biliary drainage more immediately[6,8]. Unfortunately, consistent with our results, there was no evidence that earlier decompression (within 12 h) benefited these severe patients.
Another multicenter retrospective net cohort study reported a novel finding in which delayed biliary decompression (> 12 h) was significantly associated with increased mortality in AC patients combined with septic shock [OR 3.40 (1.12-10.31)][7]. These results suggest that it may be necessary to approach each organ’s failure separately and that different types of organ dysfunction should be considered when determining the optimal drainage timing. This was verified by our multivariable analysis which showed that neurological, respiratory, renal, and cardiovascular dysfunction were significantly associated with IHM (OR = 5.32, 2.541, 6.356, 4.021, respectively), whereas hepatic and hematological dysfunction did not influence IHM. In addition to indicators affecting mortality recommended in TG18, we also analyzed CCI, malignancy, and lactate levels, which were previously reported to have an impact on the death rate[5,7,18]. Multivariate regression analysis showed that, in addition to organ dysfunction, hypoproteinemia and malignant obstruction significantly increased IHM. These outcomes were similar to those reported in a previous review[3].
In this study, we first attempted to stratify Grade III AC patients according to organ dysfunction to identify patients whose prognosis could most likely be improved by earlier decompression. According to our clinical experience, neurological dysfunction was the most severe complication and might affect drainage operation; therefore, AC patients with altered mental status require immediate biliary decompression. This was verified by our data that only undergoing drainage within 12 h could greatly improve IHM in this subgroup of individuals (0% vs 17.3%, P = 0.041). For AC patients with renal dysfunction, performing drainage within 24 h could decrease the IHM. As a result, the renal injury was not only caused by infection but also induced by hypovolemia, which was provoked by fever, decreased appetite, early initiation of antibiotics, and aggressive fluid resuscitation to improve renal flow were more valuable for these patients. Unlike previous studies[7], we did not observe an association between drainage and IHM in AC patients with cardiovascular dysfunction. This may be because only 39 patients were included in this subgroup. Drainage within 12 h significantly reduced mortality in AC patients with increased lactate levels (≥ 2 mmol/L), suggesting that decompression within 12 h might be beneficial for patients with cardiovascular dysfunction. Performing drainage within 48 h greatly reduced mortality in AC patients with hepatic dysfunction, because the amelioration of biliary stasis after drainage could directly rescue hepatic function and diminish inflammatory reaction, even if no significant association between hepatic injury and IHM was observed.
The influence of abnormal WBC count and hyperbilirubinemia on outcomes in AC has been previously described[9]. The underlying pathophysiologic mechanisms are known to result from sepsis; therefore, abnormal WBC count and hyperbilirubinemia are linked with an increased likelihood of poor prognosis. Hypoalbuminemia refers to malnutrition, which is linked to life-threatening infections and poor outcomes. For individuals in these subgroups, undergoing drainage within 24 h indicated a lower IHM.
Decompression within 12, 24, or 48 h in Grade III AC patients would extend the LOS, which was contrary to the findings of Aboelsoud et al[19] who demonstrated that drainage within 24 h or 48 h could decrease the LOS, compared with drainage after 24 h or 48 h (drainage within 24 h vs after 24 h: mean 7.71 vs 13.57 d, P = 0.001; drainage within 48 h vs after 48 h: mean 8.61 vs 14.24 d, P = 0.002). This was because their study only reviewed patients who underwent drainage, whereas our study included both patients who underwent drainage and those who did not. In addition, most of the Grade II and Grade III patients in this study received only endoscopic nasobliary drainage or endoscopic retrograde biliary drainage treatment at the first ERCP intervention because of their serious condition, and 52.2% of them received a second endoscopic intervention for biliary stone removal or stent placement when their condition stabilized, thus increasing the LOS. Drainage within 12, 24, or 48 h was associated with increased hospital costs despite the severity of AC since endoscopic operation itself was expensive, and the delayed-drainage group contained non-drainage ones who spent little.
Our analysis had certain limitations. First, it was retrospective in design, and as such, was susceptible to record bias and incomplete data. Second, because it is a single-center study, the study results only reflect the clinical status of our center and cannot represent the situation of all hospitals. Third, due to the limited sample size, especially the limited number of patients with cardiovascular dysfunction who underwent drainage within 48 h, some results were not statistically significant. In addition, the time from onset to initial treatment and the antibiotics and fluid resuscitation before admission to our hospital were not evaluated, which may have an impact on the outcome. A prospective multicenter study will be conducted to further explore a precise stratified model to guide drainage timing rather than TG18.
To our knowledge, this is the first study to stratify patients with Grade III AC according to different organ dysfunctions and to recommend the optimal timing of biliary drainage accordingly. Biliary decompression significantly decreases the all-cause IHM rates in AC, and early biliary drainage (< 24 h) was shown to be beneficial for AC patients with Grade III severity. Severe cases with different organ dysfunctions have distinct prognoses, and cases complicated with either neurological or cardiovascular dysfunction should undergo drainage within 12 h of admission. For patients with mild or moderate cholangitis, early drainage increases the probability of a second treatment and increases the patients' injury, hospitalization cost, and LOS. A further multicenter prospective cohort study will be conducted to verify the result and investigate whether the optimal timing of drainage based on different organ dysfunctions can increase the 30-d mortality rates and decrease the readmission rate.
Acute cholangitis (AC) is a life-threatening condition that occurs in the presence of biliary obstruction. Biliary decompression is well known to greatly decrease the risks of mortality in AC. Although early biliary drainage is recommended by the treatment guidelines for AC, the exact timeframe is yet to be established.
We have observed that the clinical outcomes of severe AC patients vary dramatically. So, we first attempted to study whether AC patients with different organ dysfunction should undergo biliary drainage at distinct times and try to screen out patients that could benefit the most from earlier drainage.
To investigate the optimal drainage timing for AC patients with each disease severity grade and organ dysfunction.
In this retrospective monocenter cohort analysis, we reviewed 1305 patients who were diagnosed with AC according to the Tokyo guidelines 2018 at a Chinese tertiary hospital for four years. We investigated the all-cause in-hospital mortality (IHM), hospital length of stay (LOS), and hospitalization costs associated with the timing of biliary drainage according to the severity grading and different dysfunctioning organs and critical predictors [age, white blood cell (WBC) count, total bilirubin, albumin, lactate, malignant obstruction, and Charlton comorbidity index (CCI)].
Biliary drainage within 24 h in Grade III AC patients had the greatest benefit, which could significantly reduce the all-cause IHM, while increasing LOS and hospitalization costs. Multivariate logistic analysis revealed that neurological, respiratory, renal, and cardiovascular dysfunctions, hypoalbuminemia, and malignant obstruction were significantly associated with IHM. Furthermore, AC patients complicated with neurological dysfunction or with serum lactate > 2 mmol/L should be drained as early as possible (< 12 h) for it could significantly decrease the IHM. In the subgroup of AC patients with renal dysfunction, abnormal WBC count, hyperbilirubinemia, or hypoalbuminemia, drainage within 24 h reduced the IHM, while in the subgroup of AC patients with hepatic dysfunction, malignant obstruction, or a CCI > 3, biliary drainage should be performed within 48 h.
Biliary drainage within 12 h is beneficial for AC patients with neurological or cardiovascular dysfunction, while complete biliary decompression within 24 h of admission is recommended for treating patients with Grade III AC.
A further multicenter prospective cohort study will be conducted to verify the result and investigate whether the optimal timing of drainage based on different organ dysfunctions can increase the 30-d mortality rates and decrease the readmission rate.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Badessi G, Italy; Emran TB, Bangladesh; Maieron A, Austria S-Editor: Yan JP L-Editor: A P-Editor: Yan JP
| 1. | Buxbaum JL, Buitrago C, Lee A, Elmunzer BJ, Riaz A, Ceppa EP, Al-Haddad M, Amateau SK, Calderwood AH, Fishman DS, Fujii-Lau LL, Jamil LH, Jue TL, Kwon RS, Law JK, Lee JK, Naveed M, Pawa S, Sawhney MS, Schilperoort H, Storm AC, Thosani NC, Qumseya BJ, Wani S. ASGE guideline on the management of cholangitis. Gastrointest Endosc. 2021;94:207-221.e14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 35] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 2. | Manes G, Paspatis G, Aabakken L, Anderloni A, Arvanitakis M, Ah-Soune P, Barthet M, Domagk D, Dumonceau JM, Gigot JF, Hritz I, Karamanolis G, Laghi A, Mariani A, Paraskeva K, Pohl J, Ponchon T, Swahn F, Ter Steege RWF, Tringali A, Vezakis A, Williams EJ, van Hooft JE. Endoscopic management of common bile duct stones: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2019;51:472-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 463] [Cited by in RCA: 373] [Article Influence: 62.2] [Reference Citation Analysis (0)] |
| 3. | Kiriyama S, Takada T, Hwang TL, Akazawa K, Miura F, Gomi H, Mori R, Endo I, Itoi T, Yokoe M, Chen MF, Jan YY, Ker CG, Wang HP, Wada K, Yamaue H, Miyazaki M, Yamamoto M. Clinical application and verification of the TG13 diagnostic and severity grading criteria for acute cholangitis: an international multicenter observational study. J Hepatobiliary Pancreat Sci. 2017;24:329-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 83] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 4. | Miura F, Okamoto K, Takada T, Strasberg SM, Asbun HJ, Pitt HA, Gomi H, Solomkin JS, Schlossberg D, Han HS, Kim MH, Hwang TL, Chen MF, Huang WS, Kiriyama S, Itoi T, Garden OJ, Liau KH, Horiguchi A, Liu KH, Su CH, Gouma DJ, Belli G, Dervenis C, Jagannath P, Chan ACW, Lau WY, Endo I, Suzuki K, Yoon YS, de Santibañes E, Giménez ME, Jonas E, Singh H, Honda G, Asai K, Mori Y, Wada K, Higuchi R, Watanabe M, Rikiyama T, Sata N, Kano N, Umezawa A, Mukai S, Tokumura H, Hata J, Kozaka K, Iwashita Y, Hibi T, Yokoe M, Kimura T, Kitano S, Inomata M, Hirata K, Sumiyama Y, Inui K, Yamamoto M. Tokyo Guidelines 2018: initial management of acute biliary infection and flowchart for acute cholangitis. J Hepatobiliary Pancreat Sci. 2018;25:31-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 174] [Article Influence: 24.9] [Reference Citation Analysis (0)] |
| 5. | Navaneethan U, Gutierrez NG, Jegadeesan R, Venkatesh PG, Butt M, Sanaka MR, Vargo JJ, Parsi MA. Delay in performing ERCP and adverse events increase the 30-day readmission risk in patients with acute cholangitis. Gastrointest Endosc. 2013;78:81-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 45] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 6. | Khamaysi I, Taha R. ERCP for severe acute cholangitis: The earlier, the better. Turk J Gastroenterol. 2020;31:78-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Karvellas CJ, Abraldes JG, Zepeda-Gomez S, Moffat DC, Mirzanejad Y, Vazquez-Grande G, Esfahani EK, Kumar A; Cooperative Antimicrobial Therapy of Septic Shock (CATSS) Database Research Group. The impact of delayed biliary decompression and anti-microbial therapy in 260 patients with cholangitis-associated septic shock. Aliment Pharmacol Ther. 2016;44:755-766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 56] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 8. | Becq A, Chandnani M, Bartley A, Nuzzo A, Bilal M, Bharadwaj S, Cohen J, Gabr M, Berzin TM, Pleskow DK, Sawhney MS. ERCP within 6 or 12 h for acute cholangitis: a propensity score-matched analysis. Surg Endosc. 2022;36:2418-2429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Schwed AC, Boggs MM, Pham XD, Watanabe DM, Bermudez MC, Kaji AH, Kim DY, Plurad DS, Saltzman DJ, de Virgilio C. Association of Admission Laboratory Values and the Timing of Endoscopic Retrograde Cholangiopancreatography With Clinical Outcomes in Acute Cholangitis. JAMA Surg. 2016;151:1039-1045. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 10. | Tabibian JH, Yang JD, Baron TH, Kane SV, Enders FB, Gostout CJ. Weekend Admission for Acute Cholangitis Does Not Adversely Impact Clinical or Endoscopic Outcomes. Dig Dis Sci. 2016;61:53-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Inamdar S, Sejpal DV, Ullah M, Trindade AJ. Weekend vs. Weekday Admissions for Cholangitis Requiring an ERCP: Comparison of Outcomes in a National Cohort. Am J Gastroenterol. 2016;111:405-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 12. | Kiriyama S, Kozaka K, Takada T, Strasberg SM, Pitt HA, Gabata T, Hata J, Liau KH, Miura F, Horiguchi A, Liu KH, Su CH, Wada K, Jagannath P, Itoi T, Gouma DJ, Mori Y, Mukai S, Giménez ME, Huang WS, Kim MH, Okamoto K, Belli G, Dervenis C, Chan ACW, Lau WY, Endo I, Gomi H, Yoshida M, Mayumi T, Baron TH, de Santibañes E, Teoh AYB, Hwang TL, Ker CG, Chen MF, Han HS, Yoon YS, Choi IS, Yoon DS, Higuchi R, Kitano S, Inomata M, Deziel DJ, Jonas E, Hirata K, Sumiyama Y, Inui K, Yamamoto M. Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholangitis (with videos). J Hepatobiliary Pancreat Sci. 2018;25:17-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 468] [Cited by in RCA: 424] [Article Influence: 60.6] [Reference Citation Analysis (0)] |
| 13. | Cotton PB, Eisen GM, Aabakken L, Baron TH, Hutter MM, Jacobson BC, Mergener K, Nemcek A Jr, Petersen BT, Petrini JL, Pike IM, Rabeneck L, Romagnuolo J, Vargo JJ. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc. 2010;71:446-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1238] [Cited by in RCA: 1842] [Article Influence: 122.8] [Reference Citation Analysis (1)] |
| 14. | ERCP group of Digestive Endoscopy Branch of Chinese Medical Association; Biliopancreology Group of Gastroenterologist Branch of Chinese Medical Association; National Clinical Research Center for Digestive Diseases. ERCP Guidelines for China (2018). Zhonghua Xiaohua Neijing Zazhi. 2018;35:777-813. |
| 15. | Andrew DJ, Johnson SE. Acute suppurative cholangitis, a medical and surgical emergency. A review of ten years experience emphasizing early recognition. Am J Gastroenterol. 1970;54:141-154. [PubMed] |
| 16. | Shimada H, Nakagawara G, Kobayashi M, Tsuchiya S, Kudo T, Morita S. Pathogenesis and clinical features of acute cholangitis accompanied by shock. Jpn J Surg. 1984;14:269-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Mulki R, Shah R, Qayed E. Early vs late endoscopic retrograde cholangiopancreatography in patients with acute cholangitis: A nationwide analysis. World J Gastrointest Endosc. 2019;11:41-53. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 27] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 18. | Lee F, Ohanian E, Rheem J, Laine L, Che K, Kim JJ. Delayed endoscopic retrograde cholangiopancreatography is associated with persistent organ failure in hospitalised patients with acute cholangitis. Aliment Pharmacol Ther. 2015;42:212-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 60] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 19. | Aboelsoud M, Siddique O, Morales A, Seol Y, Al-Qadi M. Early biliary drainage is associated with favourable outcomes in critically-ill patients with acute cholangitis. Prz Gastroenterol. 2018;13:16-21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |