Published online Jul 21, 2022. doi: 10.3748/wjg.v28.i27.3514
Peer-review started: November 23, 2021
First decision: January 9, 2022
Revised: January 21, 2022
Accepted: June 23, 2022
Article in press: June 23, 2022
Published online: July 21, 2022
Processing time: 237 Days and 23.9 Hours
Percutaneous transhepatic cholangiography is a diagnostic and therapeutic procedure that involves inserting a needle into the biliary tree, followed by the immediate insertion of a catheter. Endoscopic ultrasound-guided biliary drainage (EUS-BD) is a novel technique that allows BD by echoendoscopy and fluoroscopy using a stent from the biliary tree to the gastrointestinal tract.
To compare the technical aspects and outcomes of percutaneous transhepatic BD (PTBD) and EUS-BD.
Different databases, including PubMed, Embase, clinicaltrials.gov, the Cochrane library, Scopus, and Google Scholar, were searched according to the guidelines for Preferred Reporting Items for Systematic reviews and Meta-Analyses to obtain studies comparing PTBD and EUS-BD.
Among the six studies that fulfilled the inclusion criteria, PTBD patients underwent significantly more reinterventions (4.9 vs 1.3), experienced more postprocedural pain (4.1 vs 1.9), and experienced more late adverse events (53.8% vs 6.6%) than EUS-BD patients. There was a significant reduction in the total bilirubin levels in both the groups (16.4-3.3 μmol/L and 17.2-3.8 μmol/L for EUS-BD and PTBD, respectively; P = 0.002) at the 7-d follow-up. There were no significant differences observed in the complication rates between PTBD and EUS-BD (3.3 vs 3.8). PTBD was associated with a higher adverse event rate than EUS-BD in all the procedures, including reinterventions (80.4% vs 15.7%, respectively) and a higher index procedure (39.2% vs 18.2%, respectively).
The findings of this systematic review revealed that EUS-BD is linked with a higher rate of effective BD and a more manageable procedure-related adverse event profile than PTBD. These findings highlight the evidence for successful EUS-BD implementation.
Core Tip: Endoscopic transpapillary biliary drainage (BD) is the preferred approach for biliary decompression in patients with unresectable pancreatic cancer and obstructive jaundice. We conducted a systematic review of studies comparing the technical aspects and outcomes of two distinct approaches for BD: Endoscopic ultrasound-guided BD (EUS-BD) and percutaneous transhepatic BD (PTBD). The evaluation of six studies that fulfilled the inclusion criteria revealed that PTBD was associated with more reinterventions, postprocedural pain, and late adverse events compared with EUS-BD. Both procedures were associated with a significant reduction in the total bilirubin levels at the 7-d follow-up, and there were no significant differences in the complication rates between the two procedures. In summary, EUS-BD was associated with a higher rate of effective BD and manageable procedure-related adverse events compared with PTBD, highlighting its utility in successful BD.
- Citation: Hassan Z, Gadour E. Percutaneous transhepatic cholangiography vs endoscopic ultrasound-guided biliary drainage: A systematic review. World J Gastroenterol 2022; 28(27): 3514-3523
- URL: https://www.wjgnet.com/1007-9327/full/v28/i27/3514.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i27.3514
Endoscopic transpapillary biliary drainage (BD) is the preferred approach for biliary decompression in patients with unresectable pancreatic cancer and obstructive jaundice[1]. Percutaneous transhepatic cholangiography (PTC) is a diagnostic and therapeutic procedure that involves inserting a needle into the biliary tree, followed by immediately inserting a catheter to achieve percutaneous BD. During the procedure, contrast is injected into one or more bile ducts (cholangiography) and sometimes into the duodenum. PTC can be performed using fluoroscopic guidance alone or using both fluoroscopic and ultrasound guidance[2,3].
In cases of suspected malignant biliary stricture, imaging alone may not be sufficient to provide a precise diagnosis. PTC was first introduced several decades ago to visualize biliary obstructions, treat malignant obstructive jaundice palliatively, and access BD[4]. Fine needle aspiration (FNA), brush cytology, and forceps biopsy have been performed using percutaneous biliary catheterization during PTC since the 1980s[5]. For biliary stenosis, endoscopic retrograde cholangiopancreatography (ERCP) has recently been recognized as a reliable diagnostic and therapeutic procedure.
Endoscopic retrograde BD (ERBD) is the most commonly used method of biliary decompression in patients with blockage of the distal central bile duct. This technique has a success rate of 90%-95% in the United States[6]. Altered anatomy, presenting pathology (tumor infiltration, impacted stone, and duodenal compression by a pancreatic pseudocyst), previous surgery, or variations in normal anatomy (periampullary diverticula and tortuous ducts) can contribute to the failure of ERBD. The failure rate of ERBD is 6%-7% in cases with obstructive jaundice caused by a blockage or altered anatomy[7]. Percutaneous transhepatic BD (PTBD) has a lower risk of complications than surgical decompression, but it is associated with complications such as fistula formation, repeat intervention, recurrent infection, and the requirement for long-term external catheter drainage, which contribute to a low quality of life[8]. Although PTBD is associated with severe morbidity and mortality, the only relative contraindication of PTBD is perihepatic ascites[6-9]. Furthermore, PTBD usually requires separate surgery after the failure of ERCP BD, thereby increasing the morbidity associated with biliary stasis.
Endoscopic ultrasound-guided BD (EUS-BD) has become more widely used as an alternative to PTBD in patients with anatomical abnormalities, which make endoscopic transpapillary insertion of a biliary stent difficult[10]. It offers advantages of being compatible with anatomic internal drainage, being more comfortable, and resulting in a recovery associated with fewer complications and reduced expenditure[11].
EUS is an extremely useful imaging method for examining the gastrointestinal luminal wall and surrounding tissues. The proximity of the EUS probe to the area of interest enables high-resolution imaging and EUS-guided FNA tissue collection in real time. EUS has become a crucial diagnostic technique due to its high-quality imaging and FNA capacity and is also used as a treatment tool. However, until recently, its use was limited to the introduction of various drugs[12,13]. The therapeutic uses of EUS have been expanded due to larger channel echoendoscopes, which combine the benefits of real-time ultrasound and fluoroscopy imaging with the use of ERCP-based devices and procedures, such as EUS-BD. In 1996, Wiersema et al[14] first reported EUS-guided diagnostic cholangiography and in 2001, Giovannini et al[10] first reported EUS-BD in a patient with pancreatic cancer, establishing a choledochoduodenal fistula with a needle knife followed by transduodenal stenting.
These early reports were followed by modified techniques and expanded indications, such as EUS-guided hepatic gastrostomy with stent placement[15], transduodenal EUS-rendezvous (EUS-RV) biliary access[16], and EUS-guided choledocholithiasis therapy with the creation of a neo papilla[17]. Since then, several studies have reported modifications to these techniques, including the use of a covered metal stent as a conduit for interventional endoscopic procedures in the bile duct[18,19]. Few studies have compared EUS-BD and PTBD in failed ERCP cases in terms of success rate and adverse event profile[20]; therefore, we performed a systematic review of the relevant literature to investigate the combined efficacy and adverse effects of EUS-BD and PTBD.
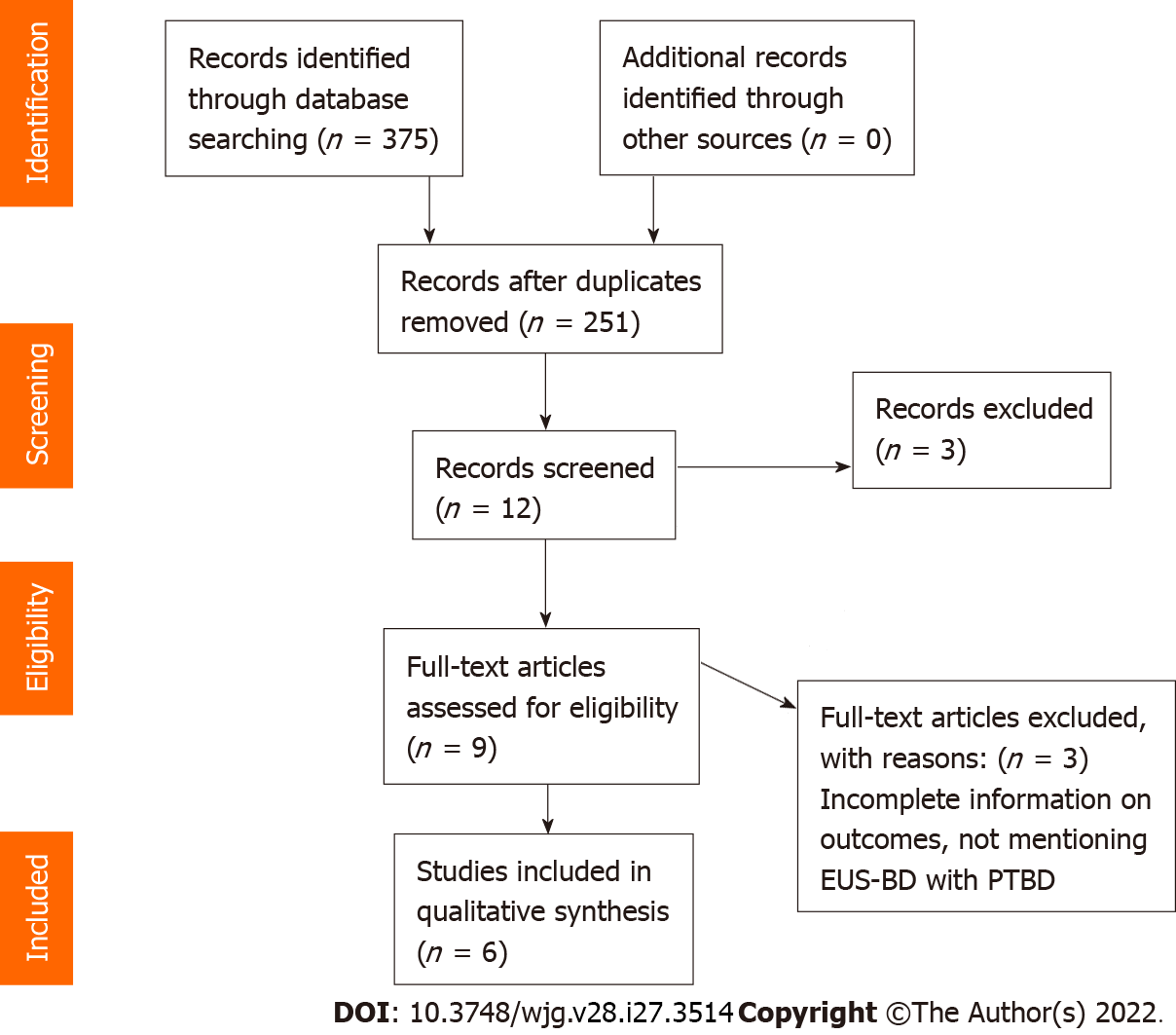
This systematic review was conducted using an electronic search of different databases, including PubMed, Embase, clinicaltrials.gov, the Cochrane library, Scopus, and Google Scholar using the guidelines for Preferred Reporting Items for Systematic reviews and Meta-Analyses[21]. Two investigators independently searched for the following key terms: all field “failed EUS”, all field “Percutaneous biliary drainage”, and all field “EUS-guided biliary drainage”. All the three search headings were connected using the Boolean operator “AND”. Studies published in English comparing PTBD with EUS-BD were chronologically limited to those published from their inception to October 2021. After completing the literature search, the references were imported to Endnote citation manager (Endnote X9) for removing any duplicates, following which the abstracts were screened for potential relevance by two independent investigators. This study included intervention studies, retrospective or prospective observational studies, case reports, randomized controlled trials, and published abstracts that reported at least some adverse events. And this study also cited high-quality articles in Reference Citation Analysis (https://www.referencecitationanalysis.com).
Letters, comments, seminar proceedings, and animal studies were excluded from our analysis. Moreover, only human studies were included and limited to the English language. Publications judged to be potentially relevant underwent a full text assessment by two independent investigators to determine their inclusion. Disagreements regarding study eligibility were resolved by consensus or adjudication between the investigators.
The baseline study details, including study identifiers, such as first author, publication year, title, and country, and study-specific methodological data, such as sample size, study design, single-center vs multicenter study types, and healthcare setting, are presented in Table 1. Technical and clinical success rates, including the total number of patients enrolled, number of patients in each arm, mean age, sex ratio, comorbidity index, mean preprocedural bilirubin, mean diameter of the bile duct, etiology of biliary obstruction, and reasons for EUS failure are shown in Table 2.
| Ref. | Artifon et al[23] | Bapaye et al[24] | Khashab et al[25] | Giovannini[26] | Jung et al[27] | Sharaiha et al[28] |
| Type of study (country) | Single-center, prospective, randomized, controlled trial(Brazil) | Single-center, retrospective, comparative study (India) | Single-center, retrospective, comparative, cohort study (United States) | Multicenter, randomized, phase II trial (France) | Multicenter, prospective, randomized, controlled trial (South Korea) | Single-center, retrospective, cohort review (United States) |
| Age [mean (SD)/median ± SD], yr | 63.4 (11.1) vs 71.0 (11.9) | 59.9 ± 13.3 vs 62.4 ± 10.2 | 64.9 ± 12.5 vs 66.9 ± 12.5 | N/A | 66.5 vs 68.4 | 68.7 ± 13.9 vs 58.8 ± 13.6 |
| Males/females | 2.25 vs 2.0 | 1.08 vs 1.6 | 1.2 vs 1.31 | 0.91 vs 9 | 3.25 vs 3 | 12 vs 1.47 |
| Comorbidity/quality index (mean) | 58.3 vs 57.8 (QoL sF 36) | N/A | N/A | N/A | 40.7 vs 40.5 (global health status/QoL) | 5.9 vs 6.4 (Charleston comorbidity index) |
| Total bilirubin (mean), mg/dL | 16.4 vs 17.2 | 7.11 ± 7.6 vs 9.41 ± 12.4 | 15.8 ± 11.3 vs 14.5 ± 8.8 | N/A | 10.4 vs 11.8 | N/A |
| Mean diameter of bile duct | 13.7 vs 11.9 | N/A | N/A | N/A | 11.22 vs 12.6 | N/A |
| Etiology of obstruction | ||||||
| Adenocarcinoma of the pancreatic | 10 vs 6 | 15 vs 18 | 43 | N/A | 12 vs 12 | 22 |
| Advanced lymphoma/liposarcoma | 0 vs 1 | 0 | 1 | N/A | 0 | 0 |
| Cholangiocarcinoma | 1 vs 1 | 2 vs 2 | 12 | N/A | 7 vs 14 | 9 |
| Duodenal carcinoma | 0 | 0 | 1 | N/A | 3 vs 0 | 5 |
| Gall bladder cancer | 0 | 0 | 0 | N/A | 5 vs 5 | 0 |
| Gastric carcinoma | 0 vs 1 | 0 | 1 | N/A | 3 vs 2 | 4 |
| Metastasis | 0 vs 3 | 0 | 12 | N/A | 3 vs 1 | 7 |
| Plasmacytoma | 1 vs 0 | 0 | 0 | N/A | 0 | 0 |
| Total malignancy | 0 | 37 | N/A | |||
| Reason for ERCP failure | ||||||
| Altered anatomy | 1 | 9 | 0 | N/A | 12 vs 10 | N/A |
| Duodenal/stomach invasion | 8 | 32 | 0 | N/A | 22 vs 22 | N/A |
| Indwelling duodenal stent | 0 | 16 | 0 | N/A | 0 | N/A |
| Unable to cannulate | 16 | 42 | 0 | N/A | 0 | N/A |
| Ref. | Technical success | Clinical success | ||
| EUS-guided Choledochoduodenostomy | Percutaneous transhepatic biliarydrainage | EUS-guided Choledochoduodenostomy | Percutaneous transhepatic biliarydrainage | |
| Artifon et al[23] | 13/13 | 12/12 | 13/13 | 12/12 |
| Bapaye et al[24] | 23/25 | 26/26 | 23/25 | 26/26 |
| Khashab et al[25] | 19/22 | 51/51 | 19/19 | 47/51 |
| Giovannini[26] | 19/20 | 17/17 | 18/19 | 17/17 |
| Jung et al[27] | 32/34 | 31/32 | 28/32 | 27/31 |
| Sharaiha et al[28] | 43/47 | 12/13 | 27/43 | 3/12 |
The GRADE checklist was used to evaluate the risk of bias in the included studies[22]. Table 3 shows a summary of the methodological qualities of studies reporting the prevalence data. Questions were answered as “yes”, “no”, “unclear”, or “not applicable”.
| Ref. | Criteria | Overall appraisal | ||||||||
| C1 | C2 | C3 | C4 | C5 | C6 | C7 | C8 | C9 | ||
| Artifon et al[23] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | Included |
| Bapaye et al[24] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Included |
| Khashab et al[25] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Included |
| Giovannini[26] | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Included |
| Jung et al[27] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | Included |
| Sharaiha et al[28] | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | Yes | Included |
Our literature search yielded 315 manuscripts, of which 132 studies remained after excluding duplicate studies. After reviewing the title and abstract, only nine articles were left for the thorough screening of data by reviewing the full text. Further, two studies were eliminated after reading the manuscripts because they included primary EUS-BD cases wherein EUS was not attempted as the primary procedure. The third study was excluded, as it did not contain full text. A total of six studies met the abovementioned inclusion criteria of the study[23-28] (Figure 1).
The most common method for gaining access to the biliary tree is ERCP. In patients with unmodified upper gastrointestinal anatomy, the success rate of bile duct cannulation using ERCP is > 90%[25]. Affected or variant anatomy, ampullary pathology (stones, stenosis, and tumor infiltration), periampullary diverticulum, gastric outlet obstruction, indwelling duodenal stent, and previous gastric bypass surgery are the prevalent causes of failed cannulation[29]. The rate of adverse outcomes associated with PTBD and surgery is extremely high, although these approaches are traditionally used to treat these clinical conditions[30]. The most prevalent issues related to long-term PTBD therapy are drain blockage, dislocation, and cholangitis, which require multiple interventions and longer hospital stays[31]. Moreover, patients are left with a permanent external drain, resulting in poor quality of life[32]. EUS-BD has emerged as a viable, extremely safe, effective, and minimally invasive approach[33]. Using echoendoscopy and fluoroscopy, the biliary tree is accessed from the gastrointestinal lumen, a fistulous tract is created, and a stent is deployed in a single step, eliminating the need for an external drain[34]. However, the rates of success and adverse events associated with EUS-BD remain unclear. The use of EUS-BD was first reported by Giovannini et al[10] in 2001. Subsequently, several studies reported the efficacy of EUS-BD as an alternative BD method after a failed ERCP. The EUS-BD procedures are divided into three techniques: (1) EUS-RV; (2) EUS-guided antegrade (EUS-AG); and (3) EUS-guided transluminal BD, including EUS-guided choledochoduodenostomy (EUS-CDS) and EUS-guided hepaticogastrostomy (EUS-HGS)[6]. In EUS-RV, the biliary duct is accessed using fluoroscopy and EUS, forming a temporary fistula, followed by guidewire placement into the duodenum via the biliary duct and ampulla. After guidewire placement, ERCP is performed using the EUS-placed guidewire, which is removed once biliary cannulation is obtained. Thus, EUS-RV should be performed in patients with an endoscopically accessible ampulla after unsuccessful biliary cannulation using conventional ERCP.
In EUS-AG, the intrahepatic biliary duct is accessed by creating a temporary fistula between the intestine and intrahepatic biliary duct from the upper intestine. Stent placement or balloon dilation is performed after the dilation of the fistula to achieve biliary obstruction through the fistula without reaching the ampulla using the endoscope. This technique is appropriate when reaching the biliary orifice using endoscopy is impossible or unmanageable, such as in biliary obstruction in patients with surgically altered anatomy or upper intestinal obstruction.
In EUS-guided transluminal BD, including EUS-CDS and EUS-HGS, the biliary duct is accessed followed by guidewire placement and fistula dilation under EUS guidance. For BD, a permanent fistula is created by inserting the stent between the biliary duct and the intestine. This procedure can be performed in cases where reaching the biliary orifice using endoscopy is possible or accessible; however, in patients with unresectable malignant biliary obstruction, its indication should be limited given the features of permanent fistula creation.
Recent studies have demonstrated that EUS-BD could be an alternative to PTBD in patients with inoperable malignant biliary blockage and failed ERCP. However, individual study outcomes show inconsistent results. We performed a systemic analysis to aggregate information from individual trials and examine the overall outcomes of EUS-BD compared with PTBD. EUS-BD was associated with a lower rate of adverse events compared with PTBD. The healthcare cost of PTBD was twice that of EUS-BD due to the high reintervention rate in the PTBD group. A retrospective study by Sharaiha et al[28] reported that the technical success rate was comparable between PTBD and EUS-BD in patients with inoperable malignant biliary obstruction and inaccessible papilla. In a retrospective study examining patients with incurable malignant biliary obstruction with failed ERCP due to an inaccessible papilla, Bapaye et al[24] found that the EUS-BD group had a higher success rate of BD (92% vs 46%, respectively, P > 0.05) and a lower rate of adverse events than the PTBD group (20% vs 46%, respectively, P = 0.05)[24]. These results were partially due to the use of EUS-BD in high-volume centers by experienced endoscopists. The rates of success and the complications of EUS-BD are expected to improve with technical advances.
In the present systematic review, the only randomized controlled study comparing EUS-BD and PTBD in patients with inoperable malignant biliary blockage was conducted by Artifon et al[8]. The study, which included 13 patients in the EUS-BD group and 12 patients in the PTBD group, reported that EUS-BD and PTBD were comparable in terms of cost, adverse events, and clinically meaningful improvements in bilirubin levels. The bilirubin levels in the EUS-BD group declined from 16.4 μmol/L to 3.3 μmol/L, whereas the bilirubin levels in the PTBD group declined from 17.2 μmol/L to 3.3 μmol/L[8]. The postprocedural follow-up period was 7 d in both the groups. Choi et al[32] reported a higher technical success rate in the PTBD group than in the EUS-BD group, although the functional success rate was comparable between the two groups[35].
In most facilities, PTBD is used as an alternative technique in cases of failed ERCP. In high-volume clinics, endoscopic ultrasound-guided gallbladder drainage has begun replacing PTBD, which was developed only a decade ago as the fourth approach for biliary decompression after surgical drainage, percutaneous transhepatic drainage, and endoscopic transpapillary drainage[36]. Although the type of BD approach used in cases of failed ERCP is currently determined by local competence, EUS-BD is a less intrusive and more physiologic technique. This approach improves nutrition absorption, prevents electrolyte loss, reduces reinterventions, and eliminates the stress of external drainage[37]. EUS-BD can also be performed in a single setting before ERCP if the patient agrees.
However, EUS-BD is associated with several specific issues. Only a small number of centers have the operational skills to perform EUS-BD, whereas most centers have extensive experience and skills to perform PTBD, and interventional radiologists are well-trained and equipped to perform PTBD[25]. The inherent risk of advanced endoscopy necessitates specialized training. Therefore, EUS-BD can only be performed in high-volume treatment institutions with adequate interventional radiology and surgical backup to prevent complications such as bile leak, pneumoperitoneum, hemorrhage, and stent migration[38,39].
The invasion of the sterile biliary tree by transmural puncture from the luminal side of the gastrointestinal tract poses a modest theoretical risk of infection in EUS-BD[40]. However, such negative events should improve with the further evolution of this technique. Despite its classification as a rescue treatment for failed ERCP, primary EUS-BD is currently compared with ERCP, and a recent study indicated similar short-term outcomes between EUS-BD and ERCP[41]. In addition, unlike ERCP, there is no risk of pancreatitis following EUS-BD. Furthermore, the clinical success rates and complications do not differ between EUS-BD and ERCP if performed by skilled endoscopists. The current systematic review revealed that EUS-BD was safe and effective when performed by skilled individuals, with a lower risk of adverse events and similar technical and clinical success rates.
Our analyses also indicated that: In patients with inoperable biliary blockage after a failed ERCP, EUS-BD was associated with a higher chance of successful BD and a lower risk of procedure-related adverse effects and infectious complications compared with PTBD. Furthermore, the number of patients with bile leaks was lower in the EUS-BD group than in the PTBD group.
Several case reports, series, and retrospective investigations regarding EUS-BD have been published to date. However, no prospective studies or comparisons of the various BD systems have been published; therefore, the technical success, functional success, adverse events, and stent patency of EUS-BD with long-term follow-up remain unknown. Prospective, randomized controlled studies are required to clarify these issues. However, it is clear that EUS-BD is clinically useful as a BD option. EUS-BD could become a first-line BD treatment instead of ERCP if the outcomes of clinical studies are positive and technologies are simplified.
Percutaneous transhepatic cholangiography is a diagnostic and therapeutic procedure. Endoscopic ultrasound-guided biliary drainage (EUS-BD) is a novel technique that allows BD whose technicality, success rate, and outcomes are not negligible.
We aimed to compare the technical details and outcomes of 132 studies concerning interventional BD procedures in patients with obstructive cholangiopathy. We conducted a systematic review of six studies that met the inclusion criteria.
To assess the suitability and appropriability of different clinical biliary interventions in achieving optimal BD for obstructive cholangiopathy.
An extensive systematic review was independently conducted by two investigators using an electronic search of different databases, including PubMed, Embase, clinicaltrials.gov, the Cochrane library, Scopus, and Google Scholar, using the guidelines for Preferred Reporting Items for Systematic reviews and Meta-Analyses to identify studies comparing percutaneous transhepatic BD (PTBD) and EUS-BD.
PTBD patients underwent significantly more reinterventions (4.9 vs 1.3), experienced more postprocedural pain (4.1 vs 1.9), and experienced more late adverse events (53.8% vs 6.6%) than EUS-BD patients. There was a significant reduction in the total bilirubin levels in both the groups (16.4-3.3 μmol/L and 17.2-3.8 μmol/L in the EUS-BD and PTBD groups, respectively; P = 0.002) at the postprocedural 7-d follow-up. There were no significant differences in the complication rates between the PTBD and EUS-BD groups (3.3 vs 3.8). PTBD was associated with a higher adverse event rate than EUS-BD in all the procedures, including reinterventions (80.4% vs 15.7%, respectively) and a higher rate of index procedure (39.2% vs 18.2%, respectively).
EUS-BD might be considered as a first-line BD treatment instead of PTBD if the outcomes of clinical studies are favorable and the technical approach is simplified.
EUS-BD following failed ERCP was superior to PTBD in patients with obstructive cholangiopathy.
Provenance and peer review: Unsolicited article; Externally peer reviewed
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: British Society of Gastroenterology, BSG64346.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United Kingdom
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Jin G, China; Villa E, United States S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Ang TL, Teo EK, Fock KM. EUS-guided transduodenal biliary drainage in unresectable pancreatic cancer with obstructive jaundice. JOP. 2007;8:438-443. [PubMed] |
| 2. | Mastier C, Valette PJ, Adham M, Mabrut JY, Glehen O, Ponchon T, Rousset P, Rode A. Complex Biliary Leaks: Effectiveness of Percutaneous Radiological Treatment Compared to Simple Leaks in 101 Patients. Cardiovasc Intervent Radiol. 2018;41:1566-1572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Azeemuddin M, Turab N Al Qamari, Chaudhry MBH, Hamid S, Hasan M, Sayani R. Percutaneous Management of Biliary Enteric Anastomotic Strictures: An Institutional Review. Cureus. 2018;10:e2228. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | DeMasi CJ, Akdamar K, Hunter FM, Sparks RD. Percutaneous transhepatic cholangiography in the diagnosis of jaundice. Am J Med Sci. 1967;254:316-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 5. | Voegeli DR, Crummy AB, Weese JL. Percutaneous transhepatic cholangiography, drainage, and biopsy in patients with malignant biliary obstruction. An alternative to surgery. Am J Surg. 1985;150:243-247. [RCA] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Komaki T, Kitano M, Sakamoto H, Kudo M. Endoscopic ultrasonography-guided biliary drainage: evaluation of a choledochoduodenostomy technique. Pancreatology. 2011;11 Suppl 2:47-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 41] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 7. | Enochsson L, Swahn F, Arnelo U, Nilsson M, Löhr M, Persson G. Nationwide, population-based data from 11,074 ERCP procedures from the Swedish Registry for Gallstone Surgery and ERCP. Gastrointest Endosc. 2010;72:1175-1184, 1184.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 145] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 8. | Artifon EL, Sakai P, Cunha JE, Dupont A, Filho FM, Hondo FY, Ishioka S, Raju GS. Surgery or endoscopy for palliation of biliary obstruction due to metastatic pancreatic cancer. Am J Gastroenterol. 2006;101:2031-2037. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 89] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 9. | Weber A, Gaa J, Rosca B, Born P, Neu B, Schmid RM, Prinz C. Complications of percutaneous transhepatic biliary drainage in patients with dilated and nondilated intrahepatic bile ducts. Eur J Radiol. 2009;72:412-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 96] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 10. | Giovannini M, Moutardier V, Pesenti C, Bories E, Lelong B, Delpero JR. Endoscopic ultrasound-guided bilioduodenal anastomosis: a new technique for biliary drainage. Endoscopy. 2001;33:898-900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 446] [Cited by in RCA: 480] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 11. | Lesmana CRA, Gani RA, Hasan I, Sulaiman AS, Ho KY, Dhir V, Lesmana LA. Palliative Endoscopic Ultrasound Biliary Drainage for Advanced Malignant Biliary Obstruction: Should It Replace the Percutaneous Approach? Case Rep Gastroenterol. 2019;13:385-397. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Kozarek RA. Malignant jaundice. Eur J Cancer Suppl. 2005;3:183-190. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Collins D, Penman I, Mishra G, Draganov P. EUS-guided celiac block and neurolysis. Endoscopy. 2006;38:935-939. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 46] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 14. | Wiersema MJ, Sandusky D, Carr R, Wiersema LM, Erdel WC, Frederick PK. Endosonography-guided cholangiopancreatography. Gastrointest Endosc. 1996;43:102-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 178] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 15. | Giovannini M, Dotti M, Bories E, Moutardier V, Pesenti C, Danisi C, Delpero JR. Hepaticogastrostomy by echo-endoscopy as a palliative treatment in a patient with metastatic biliary obstruction. Endoscopy. 2003;35:1076-1078. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 107] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 16. | Mallery S, Matlock J, Freeman ML. EUS-guided rendezvous drainage of obstructed biliary and pancreatic ducts: Report of 6 cases. Gastrointest Endosc. 2004;59:100-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 260] [Cited by in RCA: 259] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 17. | Itoi T, Itokawa F, Sofuni A, Kurihara T, Tsuchiya T, Ishii K, Tsuji S, Ikeuchi N, Moriyasu F. Endoscopic ultrasound-guided choledochoduodenostomy in patients with failed endoscopic retrograde cholangiopancreatography. World J Gastroenterol. 2008;14:6078-6082. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 86] [Cited by in RCA: 84] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 18. | Kahaleh M, Yoshida C, Kane L, Yeaton P. Interventional EUS cholangiography: A report of five cases. Gastrointest Endosc. 2004;60:138-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 68] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 19. | Chavalitdhamrong D, Draganov PV. Endoscopic ultrasound-guided biliary drainage. World J Gastroenterol. 2012;18:491-497. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 20. | Lee TH, Choi JH, Park do H, Song TJ, Kim DU, Paik WH, Hwangbo Y, Lee SS, Seo DW, Lee SK, Kim MH. Similar Efficacies of Endoscopic Ultrasound-guided Transmural and Percutaneous Drainage for Malignant Distal Biliary Obstruction. Clin Gastroenterol Hepatol. 2016;14:1011-1019.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 159] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 21. | Beller EM, Glasziou PP, Altman DG, Hopewell S, Bastian H, Chalmers I, Gøtzsche PC, Lasserson T, Tovey D; PRISMA for Abstracts Group. PRISMA for Abstracts: reporting systematic reviews in journal and conference abstracts. PLoS Med. 2013;10:e1001419. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 404] [Cited by in RCA: 499] [Article Influence: 41.6] [Reference Citation Analysis (0)] |
| 22. | Guyatt GH, Oxman AD, Schünemann HJ, Tugwell P, Knottnerus A. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol. 2011;64:380-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1540] [Cited by in RCA: 2092] [Article Influence: 139.5] [Reference Citation Analysis (0)] |
| 23. | Artifon EL, Aparicio D, Paione JB, Lo SK, Bordini A, Rabello C, Otoch JP, Gupta K. Biliary drainage in patients with unresectable, malignant obstruction where ERCP fails: endoscopic ultrasonography-guided choledochoduodenostomy versus percutaneous drainage. J Clin Gastroenterol. 2012;46:768-774. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 177] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 24. | Bapaye A, Dubale N, Aher A. Comparison of endosonography-guided vs. percutaneous biliary stenting when papilla is inaccessible for ERCP. United European Gastroenterol J. 2013;1:285-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 74] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 25. | Khashab MA, Valeshabad AK, Afghani E, Singh VK, Kumbhari V, Messallam A, Saxena P, El Zein M, Lennon AM, Canto MI, Kalloo AN. A comparative evaluation of EUS-guided biliary drainage and percutaneous drainage in patients with distal malignant biliary obstruction and failed ERCP. Dig Dis Sci. 2015;60:557-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 158] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 26. | Giovannini M. Learning in therapeutic EUS. Endosc Ultrasound. 2021;10:317-318. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 27. | Jung Y, Lee J, Cho JY, Kim YD, Park CG, Kim MW, Kim KJ, Kim SW. Comparison of efficacy and safety between endoscopic submucosal dissection and transanal endoscopic microsurgery for the treatment of rectal tumor. Saudi J Gastroenterol. 2018;24:115-121. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (1)] |
| 28. | Sharaiha RZ, Kumta NA, Desai AP, DeFilippis EM, Gabr M, Sarkisian AM, Salgado S, Millman J, Benvenuto A, Cohen M, Tyberg A, Gaidhane M, Kahaleh M. Endoscopic ultrasound-guided biliary drainage versus percutaneous transhepatic biliary drainage: predictors of successful outcome in patients who fail endoscopic retrograde cholangiopancreatography. Surg Endosc. 2016;30:5500-5505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 93] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 29. | Laméris JS, Stoker J, Nijs HG, Zonderland HM, Terpstra OT, van Blankenstein M, Schütte HE. Malignant biliary obstruction: percutaneous use of self-expandable stents. Radiology. 1991;179:703-707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 107] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 30. | Smith AC, Dowsett JF, Russell RC, Hatfield AR, Cotton PB. Randomised trial of endoscopic stenting versus surgical bypass in malignant low bileduct obstruction. Lancet. 1994;344:1655-1660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 603] [Cited by in RCA: 554] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 31. | Nennstiel S, Weber A, Frick G, Haller B, Meining A, Schmid RM, Neu B. Drainage-related Complications in Percutaneous Transhepatic Biliary Drainage: An Analysis Over 10 Years. J Clin Gastroenterol. 2015;49:764-770. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 137] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 32. | Choi JH, Kim HW, Lee JC, Paik KH, Seong NJ, Yoon CJ, Hwang JH, Kim J. Percutaneous transhepatic versus EUS-guided gallbladder drainage for malignant cystic duct obstruction. Gastrointest Endosc. 2017;85:357-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 45] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 33. | Irani S, Baron TH, Grimm IS, Khashab MA. EUS-guided gallbladder drainage with a lumen-apposing metal stent (with video). Gastrointest Endosc. 2015;82:1110-1115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 88] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 34. | Teoh AY, Binmoeller KF, Lau JY. Single-step EUS-guided puncture and delivery of a lumen-apposing stent for gallbladder drainage using a novel cautery-tipped stent delivery system. Gastrointest Endosc. 2014;80:1171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 85] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 35. | Caglar E, Atasoy D, Tozlu M, Altınkaya E, Dogan S, Senturk H. Experience of the Endoscopists Matters in Endoscopic Retrograde Cholangiopancreatography in Billroth II Gastrectomy Patients. Clin Endosc. 2020;53:82-89. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 36. | Baniya R, Upadhaya S, Madala S, Subedi SC, Shaik Mohammed T, Bachuwa G. Endoscopic ultrasound-guided biliary drainage versus percutaneous transhepatic biliary drainage after failed endoscopic retrograde cholangiopancreatography: a meta-analysis. Clin Exp Gastroenterol. 2017;10:67-74. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 37. | Holt BA, Hawes R, Hasan M, Canipe A, Tharian B, Navaneethan U, Varadarajulu S. Biliary drainage: role of EUS guidance. Gastrointest Endosc. 2016;83:160-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 70] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 38. | Kahaleh M, Artifon EL, Perez-Miranda M, Gupta K, Itoi T, Binmoeller KF, Giovannini M. Endoscopic ultrasonography guided biliary drainage: summary of consortium meeting, May 7th, 2011, Chicago. World J Gastroenterol. 2013;19:1372-1379. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 61] [Cited by in RCA: 63] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 39. | Kawakubo K, Isayama H, Kato H, Itoi T, Kawakami H, Hanada K, Ishiwatari H, Yasuda I, Kawamoto H, Itokawa F, Kuwatani M, Iiboshi T, Hayashi T, Doi S, Nakai Y. Multicenter retrospective study of endoscopic ultrasound-guided biliary drainage for malignant biliary obstruction in Japan. J Hepatobiliary Pancreat Sci. 2014;21:328-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 172] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 40. | Lakhtakia S. Complications of diagnostic and therapeutic Endoscopic Ultrasound. Best Pract Res Clin Gastroenterol. 2016;30:807-823. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 41. | Dhir V, Itoi T, Khashab MA, Park DH, Yuen Bun Teoh A, Attam R, Messallam A, Varadarajulu S, Maydeo A. Multicenter comparative evaluation of endoscopic placement of expandable metal stents for malignant distal common bile duct obstruction by ERCP or EUS-guided approach. Gastrointest Endosc. 2015;81:913-923. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 129] [Article Influence: 12.9] [Reference Citation Analysis (0)] |