Published online May 21, 2022. doi: 10.3748/wjg.v28.i19.2112
Peer-review started: December 19, 2021
First decision: March 10, 2022
Revised: March 23, 2022
Accepted: April 15, 2022
Article in press: April 15, 2022
Published online: May 21, 2022
Processing time: 148 Days and 20.8 Hours
Natural orifice transluminal endoscopic surgery (NOTES) gallbladder-preserving surgery by flexible endoscopy is an emerging technology. However, the gallbladder fails to obtain traction and positioning functions during the operation.
To evaluate the feasibility and safety of a new surgical method, “snare-assisted pure NOTES gallbladder-preserving surgery”.
Eight miniature pigs were randomly divided into the experimental group [NOTES gallbladder-preserving surgery using the snare device, snare assisted (SA)] and the control group (NOTES gallbladder-preserving surgery without using the snare device, NC), with four cases in each group. The differences between the two groups of animals in operating time, operating workload, complications, adverse events, white blood cells, and liver function were determined.
No differences were found in the surgical success rate, gallbladder incision closure, white blood cell count, or liver function between the two groups. The total operating time, gallbladder incision blood loss, gallbladder disorientation time, gallbladder incision closure time, and workload scores on the National Aeronautics and Space Administration-Task Load Index were significantly reduced in the SA group (P < 0.05).
These results indicated that snare-assisted pure NOTES gallbladder-preservation surgery using standard endoscopic instruments reduced the difficulty of operation, shortened operation time, and did not increase complications in pigs. A new method for pure NOTES gallbladder-preservation surgery was provided.
Core Tip: This study aimed to evaluate the feasibility and safety of a new surgical method, “snare-assisted pure natural orifice transluminal endoscopic surgery (NOTES) gallbladder-preserving surgery”. Eight miniature pigs were randomly divided into an experimental group [snare assisted (SA)] and a control group. The total operating time, gallbladder incision blood loss, gallbladder disorientation time, gallbladder incision closure time, and workload scores on the National Aeronautics and Space Administration-Task Load Index were significantly reduced in the SA group. These results indicated that snare-assisted pure NOTES gallbladder-preservation surgery reduced the difficulty of the operation, shortened the operation time, and did not increase complications.
- Citation: Guo XW, Liang YX, Huang PY, Liang LX, Zeng YQ, Ding Z. Snare-assisted flexible endoscope in trans-gastric endoscopic gallbladder-preserving surgery: A pilot animal study. World J Gastroenterol 2022; 28(19): 2112-2122
- URL: https://www.wjgnet.com/1007-9327/full/v28/i19/2112.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i19.2112
The incidence of benign gallbladder diseases, such as gallbladder stones and gallbladder polyps, has been increasing yearly[1], and the total prevalence of gallbladder stones in adults worldwide has reached 10%–20%[2]. Currently, cholecystectomy is still the main method used for the treatment of gallbladder stones and polyps. However, many complications occur after the patient loses the gallbladder[3,4]; moreover, gallbladder loss leads to an increased incidence of colorectal, pancreatic, esophageal, and liver cancers[5-8]. With the development of medicine, some doctors have realized that gallbladder removal may not be suitable for all patients with benign gallbladder diseases. The operation and concept of preserving the gallbladder and curing benign gallbladder diseases are now widely supported. In addition, some patients refuse open or laparoscopic cholecystectomy because it can cause surgical scars on the abdominal wall. They believe that these scars have a negative impact on their physical and mental health[9]. As an emerging technology, gallbladder-preservation surgery via natural orifice transluminal endoscopic surgery (NOTES) has obvious advantages in the complete resection of gallbladder polyps, removal of gallbladder stones, and preservation of gallbladder function. It is minimally invasive, painless, and scar-free. However, there are some technical obstacles to the clinical application of this operation. For example, the gallbladder bed is close to the liver, is obscured by fatty tissue, and has a poor field of vision; therefore, it can be difficult to locate the gallbladder[10]. In addition, the gallbladder collapses and shrinks quickly after incision, and the instruments used for gallbladder operation lose their focus, thereby making the operation very difficult[11]. The single-channel flexible endoscope for gallbladder-preservation surgery via NOTES requires additional navigation and traction.
Our inspiration came from the use of snares to assist in traction and exposure of lesions during endoscopic submucosal dissection. We tried a similar surgical method, which involved using a snare to assist in the traction and positioning of the gallbladder. The aim of this study was to evaluate the feasibility and safety of a newly proposed operative method, “a snare-assisted pure NOTES gallbladder-preserving surgery by a single-channel flexible endoscope”.
Eight Bama mini pigs weighing 15–20 kg that were in good health (with qualified certification) were chosen. The eight animals were randomly divided into two groups: The experimental group [NOTES gallbladder-preserving surgery using the snare device, snare assisted (SA)] and the control group (NOTES gallbladder-preserving surgery without using the snare device, NC). Each group had four animals. This study was conducted in the Experimental Center of the People's Hospital of Guangxi Zhuang Autonomous Region. The study was reviewed and approved by the Ethics Committee of the People's Hospital of Guangxi Zhuang Autonomous Region and the Ethics Committee of the Tongji Medical College, No. KY-LW-2019-4, [2020]-S322.
A single-channel flexible endoscope (GIF-Q260J, Olympus, Tokyo, Japan) and an electrosurgical generator (Endocut ICC200; Erbe, Tubingen, Germany) were used. Other equipment included a snare (Boston Scientific, Ref; M00562650), a transparent cap (Olympus), an insulated IT-knife (model KD-610L, Olympus), a hook knife (model KD-620LR, Olympus), an injection needle (model 19G, Olympus), hemostatic clips and a release device (Olympus), and hot hemostatic forceps (KD610, Olympus). All endoscopes and accessories were sterilized prior to use.
The medications used in the study included xylazine hydrochloride injection, propofol injection, diazepam, 2% pentobarbital sodium, atropine, cimetidine, and ceftiofur sodium for injection (Chengdu Zhongmu Biological Pharmaceutical Co., Ltd.).
The pigs fasted for 48–72 h. They were given 200 mL of milk and 500 mL of 50% glucose for their daily drink. Preoperative intramuscular injection of xylazine hydrochloride (2 mL) was completed, after which blood was immediately collected from the anterior vena cava of the neck. Then, an intravenous injection needle was placed in the dorsal ear vein, and intravenous infusion of propofol injection (4 mg/kg/h) was completed to maintain anesthesia. Endotracheal intubation was not performed. The ECG oxygen saturation meter was connected to monitor vital signs, and electrode pads were pasted on the abdominal skin after shaving. Preoperative intramuscular injection of ceftiofur sodium (5 mg/kg) was performed to prevent infection.
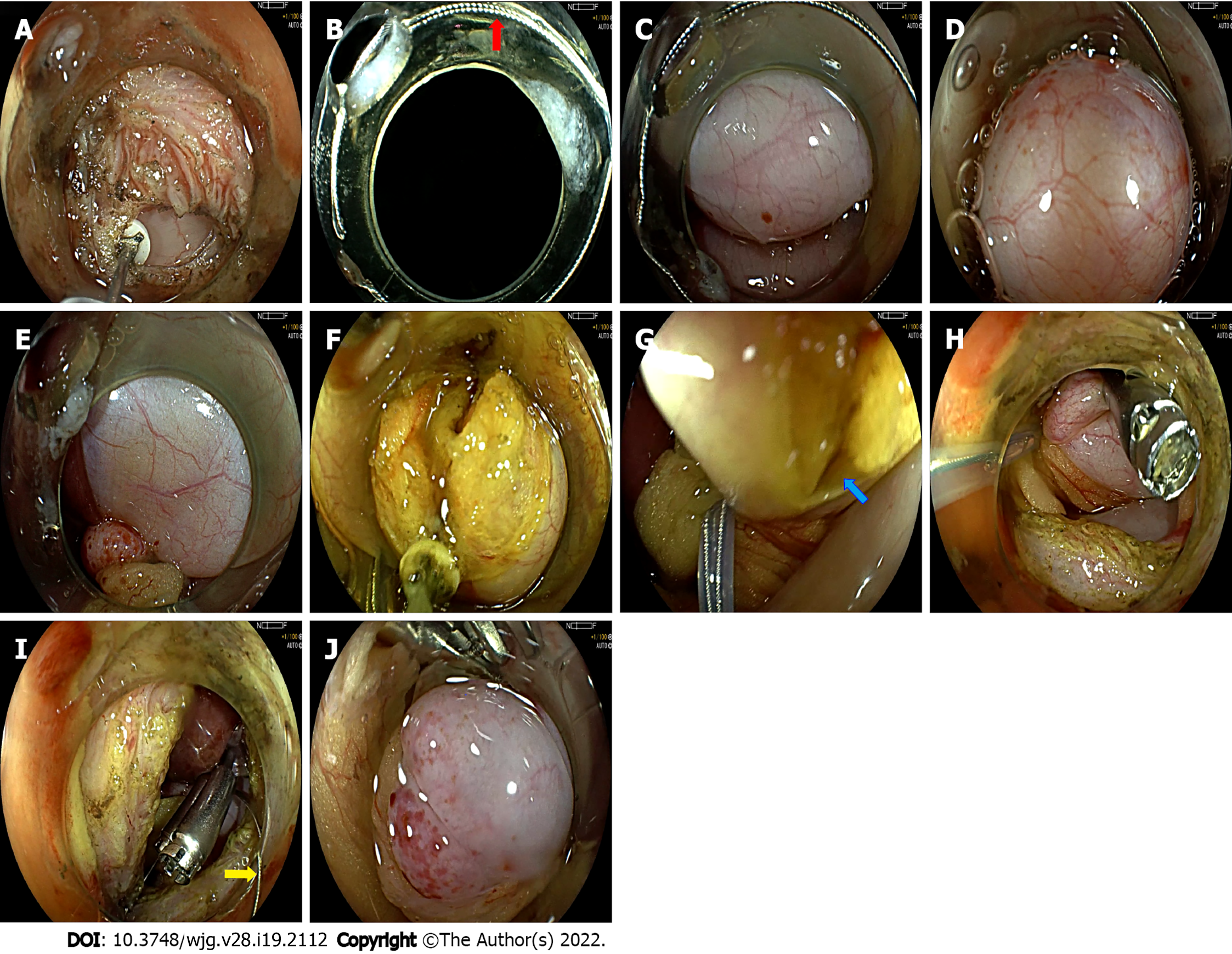
SA group: Each generally anesthetized pig was placed on its left side on the operating table. Each one wore a sterile mouth ring and was covered with sterile towels. An ordinary gastroscope was preinserted into the stomach. The stomach, esophagus, and duodenum were flushed with normal saline (> 1000 mL). A transparent cap was placed on the front end of the sterile gastroscope, and the anterior wall of the gastric antrum was incised using a hook knife and IT knife (Figure 1A). The snare was placed on the transparent cap and inserted into the abdominal cavity along with the endoscope (Figure 1B). The liver and gallbladder were examined (Figure 1C). The transparent cap clung to the gallbladder wall, and the gallbladder wall was sucked in it. The snare was released, and the gallbladder wall was ligated (Figure 1D). Under this ligation state (Figure 1E), a hook knife and IT knife were used to make an incision of approximately 13 mm in the gallbladder wall (Figure 1F and G). The endoscope entered the gallbladder and was used to observe and flush the gallbladder mucosa. Metal clips were employed to close the gallbladder incision (Figure 1H). The snare was loosened (Figure 1I and J). The abdominal cavity was flushed with normal saline (> 2000 mL). Further observation was performed to ensure that there was no bleeding or bile leakage at the gallbladder incision. Then, the gastric wall incision was closed with clips.
NC group: Except for the fact that the snare was not used, the operating procedures performed for this group were the same as those mentioned above.
During the operation, the intra-abdominal pressure was not measured. The anesthesiologist monitored the abdominal wall pressure and the oxygenation index of the ear skin, which prompted the endoscopist to suck the gas from the abdominal cavity with an endoscope in time to reduce the intra-abdominal pressure.
The video came from a single surgical procedure in the SA group. A pig model was used to demonstrate snare-assisted pure NOTES gallbladder-preserving surgery by a single-channel flexible endoscope (Videos 1 and 2).
All pigs were given liquid food after fasting for 24 h. All animals received ceftiofur sodium via injection (5 mg/kg, qd, 3 d) to prevent infection. An experienced physician conducted extensive monitoring of these animals daily to observe whether complications or adverse events occurred. Blood was collected at 24 h and 28 d after the operation. Gastroscopy was performed 28 d after the operation.
The animal protocol was designed to minimize pain or discomfort to the animals. All animals were killed by barbiturate overdose (intravenous injection, 150 mg/kg pentobarbital sodium) for autopsy.
Changes in the number of white blood cells, blood amylase, and liver function were observed before and after the operation. The operation success rate, operation time, intraoperative and postoperative complications, and animal survival rate were recorded. The National Aeronautics and Space Administration-Task Load Index (NASA-TLX)[12] was used to assess the difficulty of the operation. The conditions of the abdominal cavity, stomach wall, and gallbladder were observed by autopsy.
Quantitative data are expressed as the mean ± SD. The results were analyzed by SPSS 23.0 statistical software. The significance of the data was determined by Student’s t-test. P value < 0.05 was considered statistically significant.
The operation was completed on all animals, and a success rate of 100% was achieved. It took 10.9 ± 4.3 min to cut the stomach wall, and the bleeding volume was 12.4 ± 6.6 mL. Although entry into the abdominal cavity occurred through the anterior wall of the gastric antrum, which was close to the gallbladder, the mirror body had no bending and showed good mobility. The operation space and visual field were small, and it took 11.0 ± 3.6 min to locate the gallbladder. Fortunately, under the assisted traction and navigation positioning of the snare, blood loss during gallbladder incision was reduced (P < 0.05). The total operating time, gallbladder disorientation time during the operation, and gallbladder incision closure time were significantly reduced in the SA group (P < 0.05) (Table 1). No differences were found between the two groups in the time involved in gallbladder incision and the number of clips required to close the gallbladder incision (P > 0.05), as shown in Table 1. However, removal of the clip was needed in 50% (2/4) of the animals in the NC group due to the incorrect placement of the clip; this situation did not occur in the SA group. The inside of the gallbladder of all animals was fully explored and flushed. None of the animals had bile leakage from the gallbladder incision.
| Content | NC group | SA group | t value | P value |
| Time required for gallbladder incision (min) | 18.5 ± 7.0 | 10.0 ± 1.8 | 2.335 | 0.058 |
| Bleeding volume of gallbladder incision (mL) | 7.5 ± 2.9 | 2.0 ± 2.2 | 3.051 | 0.022 |
| Number of gallbladder disorientations | 2.0 ± 0.8 | 1.3 ± 0.5 | 1.567 | 0.168 |
| Longest time of gallbladder disorientation (min) | 11.5 ± 4.7 | 2.0 ± 0.8 | 4.020 | 0.007 |
| Time involved in closing the gallbladder (min) | 18.3 ± 1.7 | 12.5 ± 2.1 | 4.271 | 0.005 |
| Number of clamps used to close the gallbladder (pieces) | 6.3 ± 0.5 | 6.5 ± 1.0 | -0.447 | 0.670 |
| Total operation time (min) | 142.3 ± 10.2 | 102.5 ± 5.5 | 6.853 | 0.000 |
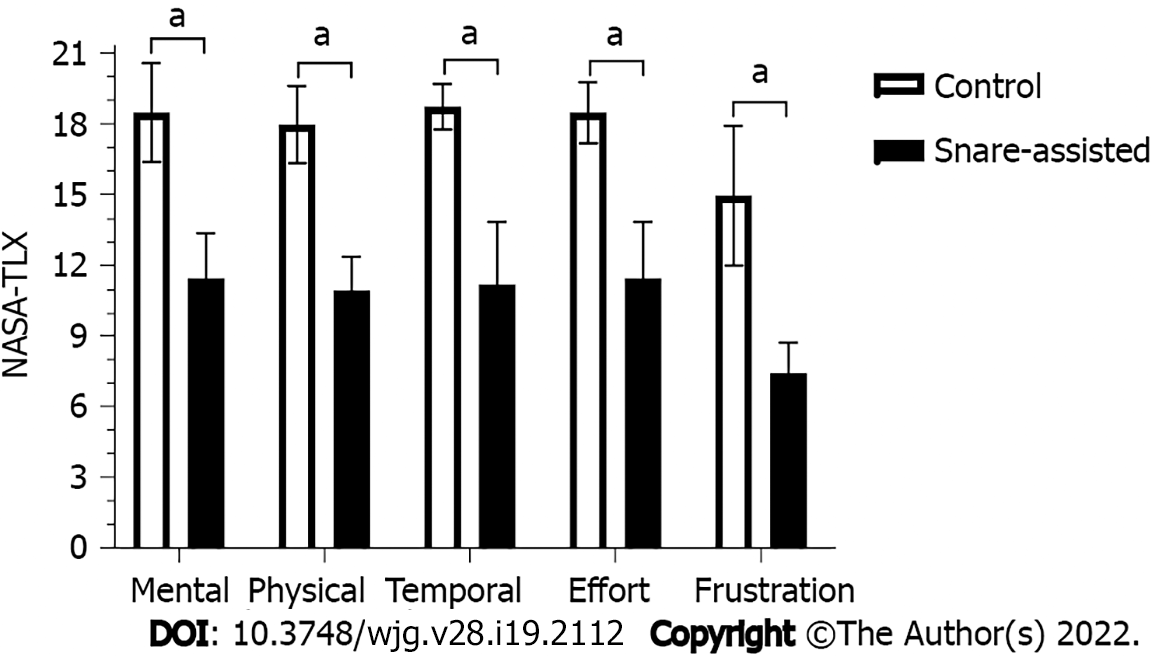
| NASA-TLX mental demand | 18.5 ± 2.1 | 11.5 ± 1.9 | 4.950 | 0.003 |
| NASA-TLX physical | 18.0 ± 1.6 | 11.0 ± 1.4 | 6.481 | 0.001 |
| NASA-TLX temporal demand | 18.8 ± 1.0 | 11.3 ± 2.6 | 5.359 | 0.002 |
| NASA-TLX effort | 18.5 ± 1.3 | 11.5 ± 2.4 | 5.170 | 0.004 |
| NASA-TLX frustration | 15.0 ± 2.9 | 7.5 ± 1.3 | 4.666 | 0.003 |
Using the NASA-TLX to evaluate the difficulty of operation, the results showed that under the auxiliary traction and positioning of the snare, the mental demand, physical burden, temporal demand, effort, and frustration of the endoscopist were significantly reduced (P < 0.05), as shown in Table 1 and Figure 2.
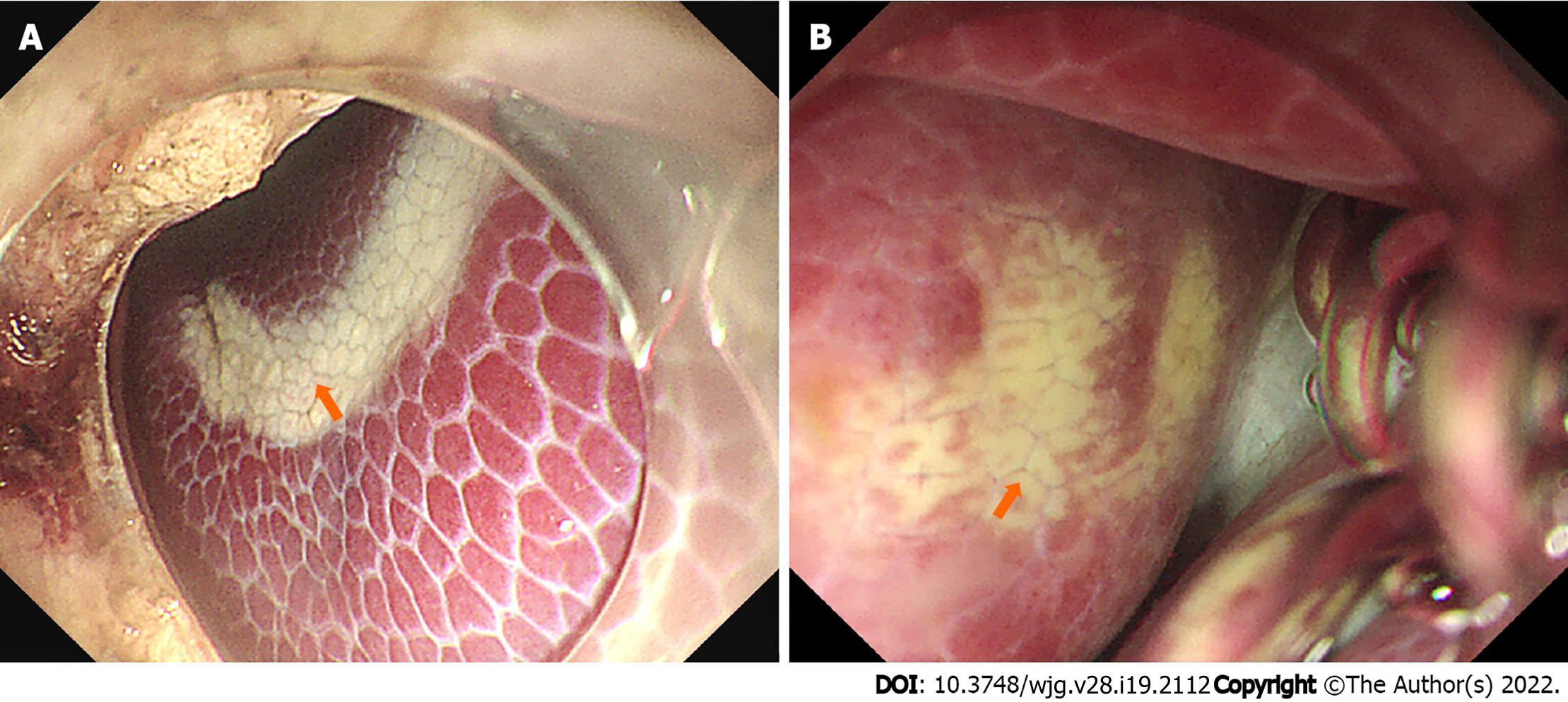
During the operation, 75% (3/4) of the animals in the NC group showed a significant decrease in the “blood oxygen index” of the ear skin, which returned to normal after the gas in the abdominal cavity was sucked through an endoscope. However, the animals in the SA group did not show these adverse events. In addition, 100% (4/4) of the animals in the NC group had electric burn scars on their livers (Figure 3), whereas only 25% (1/4) of the animals in the SA group showed a similar condition.
All animals survived, and their body weight increased appropriately (an increase of 1.88 ± 0.69 kg) until euthanasia on Day 28. The follow-up found that the animals in the SA group were normal after the operation, and no complications occurred. In addition, no significant differences were found between the groups in the number of white blood cells and neutrophils, liver function, or the amount of amylase in the blood at 24 h and 28 d after surgery (P > 0.05) (Table 2).
| Blood | 24 h after operation | 28 d after operation | ||||||
| NC group | SA group | t value | P value | NC group | SA group | t value | P value | |
| Number of white blood cells (× 109/L) | 28.83 ± 3.43 | 30.10 ± 3.47 | -0.521 | 0.621 | 26.16 ± 3.64 | 25.59 ± 4.40 | 0.201 | 0.847 |
| Number of neutrophils (× 109/L) | 18.39 ± 1.67 | 19.76 ± 3.65 | -0.682 | 0.521 | 16.03 ± 1.31 | 16.67 ± 2.39 | -0.472 | 0.654 |
| Number of lymphocytes (× 109/L) | 8.63 ± 3.71 | 9.35 ± 1.30 | -0.368 | 0.732 | 8.79 ± 2.68 | 7.95 ± 2.34 | 0.472 | 0.654 |
| Number of red blood cells (× 1012/L) | 7.12 ± 0.92 | 6.23 ± 0.41 | 1.763 | 0.128 | 6.27 ± 0.26 | 5.79 ± 0.43 | 1.909 | 0.105 |
| Hemoglobin (g/L) | 129.3 ± 8.5 | 115.8 ± 6.9 | 2.466 | 0.049 | 120.50 ± 3.42 | 111.50 ± 5.69 | 2.714 | 0.035 |
| Total bilirubin (μmol/L) | 1.85 ± 0.98 | 2.73 ± 0.74 | -1.426 | 0.204 | 2.30 ± 0.96 | 2.73 ± 0.62 | -0.743 | 0.486 |
| Direct bilirubin (μmol/L) | 1.28 ± 0.99 | 2.15 ± 0.66 | -1.469 | 0.192 | 1.58 ± 0.87 | 2.05 ± 0.59 | -0.901 | 0.402 |
| ALT (U/L) | 58.3 ± 22.9 | 41.5 ± 3.7 | 1.446 | 0.198 | 49.75 ± 11.32 | 40.50 ± 2.08 | 1.607 | 0.201 |
| AST (U/L) | 78.3 ± 66.3 | 50.8 ± 12.7 | 0.815 | 0.446 | 61.25 ± 19.36 | 49.75 ± 8.26 | 1.093 | 0.317 |
| Alkaline phosphatase (U/L) | 183.5 ± 35.9 | 189.8 ± 57.3 | -0.185 | 0.859 | 178.75 ± 36.29 | 176.00 ± 38.40 | 0.104 | 0.920 |
| γ-GT (U/L) | 73.8 ± 32.9 | 77.8 ± 20.3 | -0.207 | 0.843 | 72.50 ± 16.76 | 64.25 ± 12.31 | 0.793 | 0.458 |
| Amylase (U/L) | 2684.8 ± 465.9 | 2829.5 ± 170.6 | -0.584 | 0.581 | 2583.25 ± 130.31 | 2770.00 ± 102.56 | -2.252 | 0.065 |
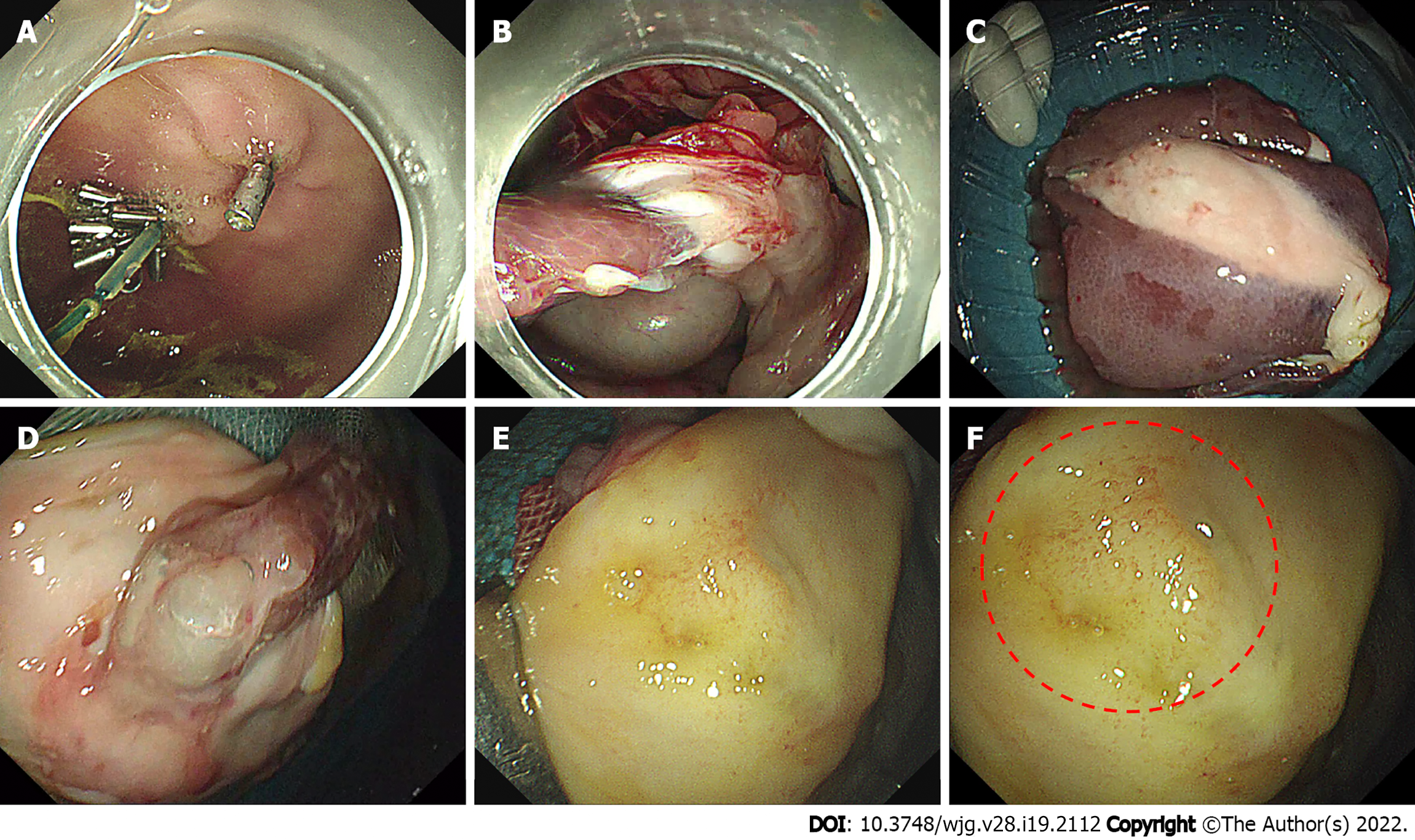
The gastric wall incisions of all animals healed without ulcers and incision fistulas (Figure 4A). A small number of omental adhesions existed on the gastric serosal surface of all animals. After the adhesions were released, the gastric wall incisions healed well. The gallbladder incisions of all animals were closed well, and no biliary fistulas, peritoneal effusions, abdominal hematomas, or abdominal abscesses were found. However, there were some adhesions around the gallbladder incisions, and the metal clip was wrapped in it (Figure 4B-D). The gallbladder was opened, and the gallbladder mucosa was smooth, with no formation of stones or polyps. The mucosa at the original incision healed well (Figure 4E), and the local mucosa was slightly edematous (Figure 4F), with an average thickness of 4.2 ± 0.7 mm. However, there was no difference in the thickness of the gallbladder mucosa between the two groups (P > 0.05).
At present, cholecystectomy is still the gold standard for the treatment of gallbladder stones and polyps. However, the gallbladder has an irreplaceable role in the digestion process of the human body. Many complications and adverse reactions can occur after gallbladder resection[5-8]. Therefore, both physicians and patients expect to find a better treatment that will preserve the gallbladder and cure gallbladder stones and polyps. This paper reports the successful application of flexible endoscopy via NOTES gallbladder-preservation surgery. This seems to be a promising new surgery for patients who wish to preserve the gallbladder without scarring of the abdominal wall.
In previous single-channel flexible endoscopy via NOTES gallbladder-preservation surgery, the gallbladder was not effectively tracted and navigated, and the gallbladder and gallbladder incision were often lost during the operation, thereby significantly prolonging the operation time and increasing the damage to the surrounding organs[13]. These disadvantages make it extremely difficult to promote this kind of surgery. If the gallbladder and gallbladder incision can be positioned quickly and accurately during the operation and the gallbladder can be pulled safely and effectively, then the difficulty and risk of the operation will be greatly reduced, and the operation time will be shortened. Both physicians and the patients will benefit.
In recent years, snares have been used in endoscopic submucosal dissection to assist in traction and exposure of lesions[14]. Inspired by this use, we applied the snare device to gallbladder-preserving surgery, which is called “snare-assisted pure NOTES gallbladder-preserving surgery by flexible endoscope”. Compared with the non-snare group, the use of the snare significantly reduced the duration and difficulty of the operation. Moreover, the NASA-TLX workload score was significantly reduced, and no adverse reactions or complications occurred.
Although the endoscope enters the abdominal cavity through the stomach, the organs and structures in the four quadrants of the abdominal cavity can be clearly observed[15]. However, this study found that the gallbladder of pigs is deeply buried in the liver lobe and is mostly covered by the surrounding omentum. This affected the surgical vision and caused the disorientation of the gallbladder during the operation. This increased the difficulty of locating the gallbladder and gallbladder incision again and significantly prolonged the operation time. Given the navigation guidance of the snare during the operation, the endoscopist quickly found the gallbladder and gallbladder incision again. Thus, the duration of gallbladder disorientation during the operation and the total operation time were significantly shortened.
This study found that after the incision of the gallbladder, the bile flowed out, the gallbladder collapsed and shrank, and the surgical instruments lost their focus, thereby increasing the difficulty of the operation. The use of a snare to pull or drag the gallbladder can significantly reduce the difficulty of operation, shorten the time of gallbladder exploration, and reduce electrical coagulation damage to the nearby liver. Particularly in the case of massive hemorrhage from the gallbladder incision, blood obstructs the vision of the endoscope. The gallbladder is raised or pulled into the stomach by the snare, which can better expose the bleeding point. This is conducive to the electrocoagulation and hemostasis of the hot hemostatic forceps. This study showed that the blood loss from the gallbladder incision in the SA group was smaller than that in the NC group. Another issue is the poor closure of the gallbladder incision, which can lead to a bile fistula[10]. Although metal clips were used in this study to close the gallbladder incision, no complications, such as biliary fistula or peritonitis, occurred after the operation. However, the time involved in closing the gallbladder incision in the SA group was significantly shortened, and there were no adverse events that required the removal of the metal clip due to its incorrect placement.
This study found that 75% of the animals in the NC group experienced a significant drop in the blood oxygen index of the ears during the operation. The abdominal gas was sucked through the endoscope, and the operation was suspended to return to normal. It is possible that the abdominal pressure was too high, which inhibited the animals’ breathing and heartbeats[16]. However, the blood oxygen index of the ear skin of the animals in the SA group remained normal. Given the traction and positioning of the snare, it can assist the surgical operation and expose the surgical field without blowing excess air into the abdominal cavity.
Although there are many microorganisms in the digestive tract, the strong acidity of gastric juice makes it difficult for most microorganisms to survive. Therefore, transgastric NOTES gallbladder-preserving surgery might not increase the risk of infection. A study showed that there was no significant difference in C-reactive protein and tumor necrosis factor-α levels after open surgery, laparoscopic surgery, and pure NOTES[17]. The present study found that although the leukocytes and neutrophils in the blood of all animals increased 24 h after the operation, they quickly returned to normal, and no difference was found between the two groups of animals at 24 h and 28 d after surgery. Therefore, using the snare did not increase the risk of infection during surgery.
The gallbladders of all animals were opened, and their gallbladder mucosae were smooth without the formation of stones and polyps. The mucosal surface at the original incision healed well, and no difference was found in the thickness of the gallbladder healing area between the two groups. The snare did not affect the healing of gallbladder mucosa or gallbladder incision. Moreover, some adhesions appeared around the gallbladder incision in all animals, and the metal clip was wrapped in it. This finding may be due to the body's response to abdominal organ damage and foreign bodies[10]. However, the snare did not aggravate this reaction.
To the best of our knowledge, this is the first experimental study of snare-assisted pure NOTES gallbladder-preserving surgery. However, several limitations of this study bear consideration. First, we only applied snare assistance for endoscopic trans-gastric gallbladder-preserving surgery. Thus, we cannot generalize the efficacy of snare assistance with other surgical paths, such as endoscopic transrectal gallbladder-preserving surgery and endoscopic transvaginal gallbladder-preserving surgery. Studies with other surgery paths are necessary in the future for a complete evaluation of the efficacy and safety of snare-assisted pure NOTES gallbladder-preserving surgery. Second, the number of animals used was small, and more studies with larger sample sizes are needed to confirm these findings. Third, it was undertaken on animals; thus, clinical trials are needed to demonstrate the effectiveness of snare-assisted pure NOTES gallbladder-preserving surgery in humans.
In summary, we successfully performed a flexible endoscopic gallbladder-preserving operation on pigs through pure NOTES. The use of a snare to assist the operation can reduce the difficulty of the operation and shorten the operation time; it does not increase the risk of the operation. Translating this new technology to human subjects seems straightforward and has great practical value in the clinic. However, further studies with large sample sizes are needed to confirm its clinical benefits, especially in humans.
With the development of medicine, the operation and concept of preserving the gallbladder and curing benign gallbladder diseases are now widely supported. As an emerging technology, gallbladder-preservation surgery via natural orifice transluminal endoscopic surgery (NOTES) has obvious advantages in the complete resection of gallbladder polyps, removal of gallbladder stones, improvement of gallbladder inflammation, and preservation of gallbladder function. However, there are some technical obstacles to the clinical application of this operation. For example, the gallbladder bed is close to the liver, is obscured by fatty tissue, and has a poor field of vision, indicating that it can be difficult to locate the gallbladder. In addition, the gallbladder collapses and shrinks quickly after incision, and the instruments used for gallbladder operation lose their focus, thereby making the operation very difficult.
The single-channel flexible endoscope for gallbladder-preservation surgery via NOTES requires additional navigation and traction. We proposed a new operative method that involved using a snare to assist in the traction and positioning of the gallbladder.
This study aimed to evaluate the feasibility and safety of a new surgical method, “snare-assisted pure NOTES gallbladder-preserving surgery”.
Eight miniature pigs were randomly divided into the experimental group [NOTES gallbladder-preserving surgery using the snare device, snare assisted (SA)] and the control group (NOTES gallbladder-preserving surgery without using the snare device, NC), with four cases in each group. The differences between the two groups of animals in operating time, operating workload, complications, adverse events, white blood cells, and liver function were determined.
No differences were found in the surgical success rate, gallbladder incision closure, white blood cell count, or liver function between the two groups. The total operating time, gallbladder incision blood loss, gallbladder disorientation time, gallbladder incision closure time, and workload scores of the National Aeronautics and Space Administration-Task Load Index were significantly reduced in the SA group (P < 0.05).
These results indicated that snare-assisted pure NOTES gallbladder-preservation surgery using standard endoscopic instruments reduced the difficulty of the operation, shortened operation time, and did not increase complications in pigs.
A new method for pure NOTES gallbladder-preservation surgery was provided. Translating this new technology to human subjects seems straightforward and has great practical value in the clinic.
The authors thank Dr Jiao Lan, Dr Fei Liu and Rui-Ping Xiao from Scientific Research Center of the People’s Hospital of Guangxi Zhuang Autonomous Region for their valuable technological assistance on our projects.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Badessi G, Italy; Wang S, China S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
| 1. | Jian W, Song YZ, Xiang QF, Tian HY, Xie ZZ, Yang JB, Zhang YM, Zhang RK, Liu JL. Application of Transparent Cap-assisted Choledochoscopy in Endoscopic Gallbladder-preserving Surgery. Surg Laparosc Endosc Percutan Tech. 2020;30:317-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Lammert F, Gurusamy K, Ko CW, Miquel JF, Méndez-Sánchez N, Portincasa P, van Erpecum KJ, van Laarhoven CJ, Wang DQ. Gallstones. Nat Rev Dis Primers. 2016;2:16024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 590] [Cited by in RCA: 516] [Article Influence: 57.3] [Reference Citation Analysis (0)] |
| 3. | Stewart L. Iatrogenic biliary injuries: identification, classification, and management. Surg Clin North Am. 2014;94:297-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 52] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 4. | Saxena P, Khashab MA. New NOTES Clinical Training and Program Development. Gastrointest Endosc Clin N Am. 2016;26:385-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Shao T, Yang YX. Cholecystectomy and the risk of colorectal cancer. Am J Gastroenterol. 2005;100:1813-1820. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 75] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 6. | Fan Y, Hu J, Feng B, Wang W, Yao G, Zhai J, Li X. Increased Risk of Pancreatic Cancer Related to Gallstones and Cholecystectomy: A Systematic Review and Meta-Analysis. Pancreas. 2016;45:503-509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 7. | Lagergren J, Mattsson F. Cholecystectomy as a risk factor for oesophageal adenocarcinoma. Br J Surg. 2011;98:1133-1137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Lagergren J, Mattsson F, El-Serag H, Nordenstedt H. Increased risk of hepatocellular carcinoma after cholecystectomy. Br J Cancer. 2011;105:154-156. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Yasuda K, Shiroshita H, Inomata M, Kitano S. [Natural orifice translumenal endoscopic surgery: historical and future perspectives]. Nihon Geka Gakkai Zasshi. 2013;114:298-302. [PubMed] |
| 10. | Liu BR, Kong LJ, Song JT, Liu W, Yu H, Dou QF. Feasibility and safety of functional cholecystectomy by pure NOTES: a pilot animal study. J Laparoendosc Adv Surg Tech A. 2012;22:740-745. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Liu BR, Ullah S, Li DL, Liu D, Zhao LX, Yang W, Kong LJ, Zhang JY. A snare-assisted pure NOTES retrograde cholecystectomy using a single channel flexible endoscope: a pilot experiment in a porcine model. Surg Endosc. 2020;34:3706-3710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Lowndes BR, Forsyth KL, Blocker RC, Dean PG, Truty MJ, Heller SF, Blackmon S, Hallbeck MS, Nelson H. NASA-TLX Assessment of Surgeon Workload Variation Across Specialties. Ann Surg. 2020;271:686-692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 92] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 13. | Soltes M, Radoňak J. A risk score to predict the difficulty of elective laparoscopic cholecystectomy. Wideochir Inne Tech Maloinwazyjne. 2014;9:608-612. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Zhang Q, Cai JQ, Wang Z, Xiao B, Bai Y. Snare combined with endoscopic clips in endoscopic resection of gastric submucosal tumor: a method of tumor traction. Endosc Int Open. 2019;7:E1150-E1162. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 15. | Li Y, Han S. Transgastric endoscopic gallbladder polypectomy and cholecystolithiasis: A case report. Exp Ther Med. 2020;19:95-98. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Adelsdorfer C, Taura P, Ibarzabal A, Vendrell M, Delitala A, Deulofeu R, Adelsdorfer W, Delgado S, Lacy AM. Effect of transgastric natural orifice transluminal endoscopic surgery peritoneoscopy on abdominal organ microcirculation: an experimental controlled study. Gastrointest Endosc. 2016;83:427-433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (1)] |
| 17. | Arroyo Vázquez J, Bergström M, Dot J, Abu-Suboh-Abadia M, Fonseca C, Esteves M, Azadani A, Armengol J, Masachs M, Armengol-Miró JR, Park PO. Surgical Trauma Caused by Different Abdominal Access Routes-Comparison of Open Surgical, Laparoscopic, and NOTES Transgastric Techniques in a Porcine Model. J Laparoendosc Adv Surg Tech A. 2016;26:511-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |