Published online Apr 14, 2022. doi: 10.3748/wjg.v28.i14.1499
Peer-review started: October 20, 2021
First decision: December 27, 2021
Revised: January 13, 2022
Accepted: March 16, 2022
Article in press: March 16, 2022
Published online: April 14, 2022
Processing time: 167 Days and 22.6 Hours
A study addressing the influence of type 2 diabetes on the prognosis of acute-on-chronic liver failure patients was reviewed. Some statistical deficiencies were found in the reviewed article, and the sample size was too small to support the study. In addition, age should have been considered as one of the prognostic factors.
Core Tip: This is a comment on a study of the influence of type 2 diabetes on the prognosis of patients with acute-on-chronic liver failure. We believe that the conclusion of this study can provide more significant data.
- Citation: Wang W, Pan CC, Zhao WY, Sheng JY, Wu QQ, Chen SS. Comments on “Effect of type 2 diabetes mellitus in the prognosis of acute-on-chronic liver failure patients in China”. World J Gastroenterol 2022; 28(14): 1499-1502
- URL: https://www.wjgnet.com/1007-9327/full/v28/i14/1499.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i14.1499
We were pleased to read the high-level article published by Lai et al[1]. The results of their study showed a significant relationship between the prognosis of diabetes mellitus (DM) and acute-on-chronic liver failure (ACLF) patients. ACLF patients with DM have higher in-hospital mortality and infection rates than patients without DM. This is an important study that has made a significant contribution to the study of prognostic indicators for ACLF patients. However, there are still questionable issues in this study that we would like to discuss with the authors.
First, the Materials and Methods section needs to be more detailed and refined. The author should list the number of diabetic patients included and the number of people after grouping. The author should state the time for follow-up of the patients and redefine the concept of follow-up. If the author regards the discharge time as the end of the follow-up event, it may cause data loss. Therefore, another reference could be added for loss to follow-up. We notice that they performed multivariate analysis on parameters with P < 0.1 in univariate analysis, which is not convincing. A P value less than 0.05 would make the results more convincing. In addition, a sample of 200 for a study period of 7 years is small; the author should calculate the population size and analyze the sample size.
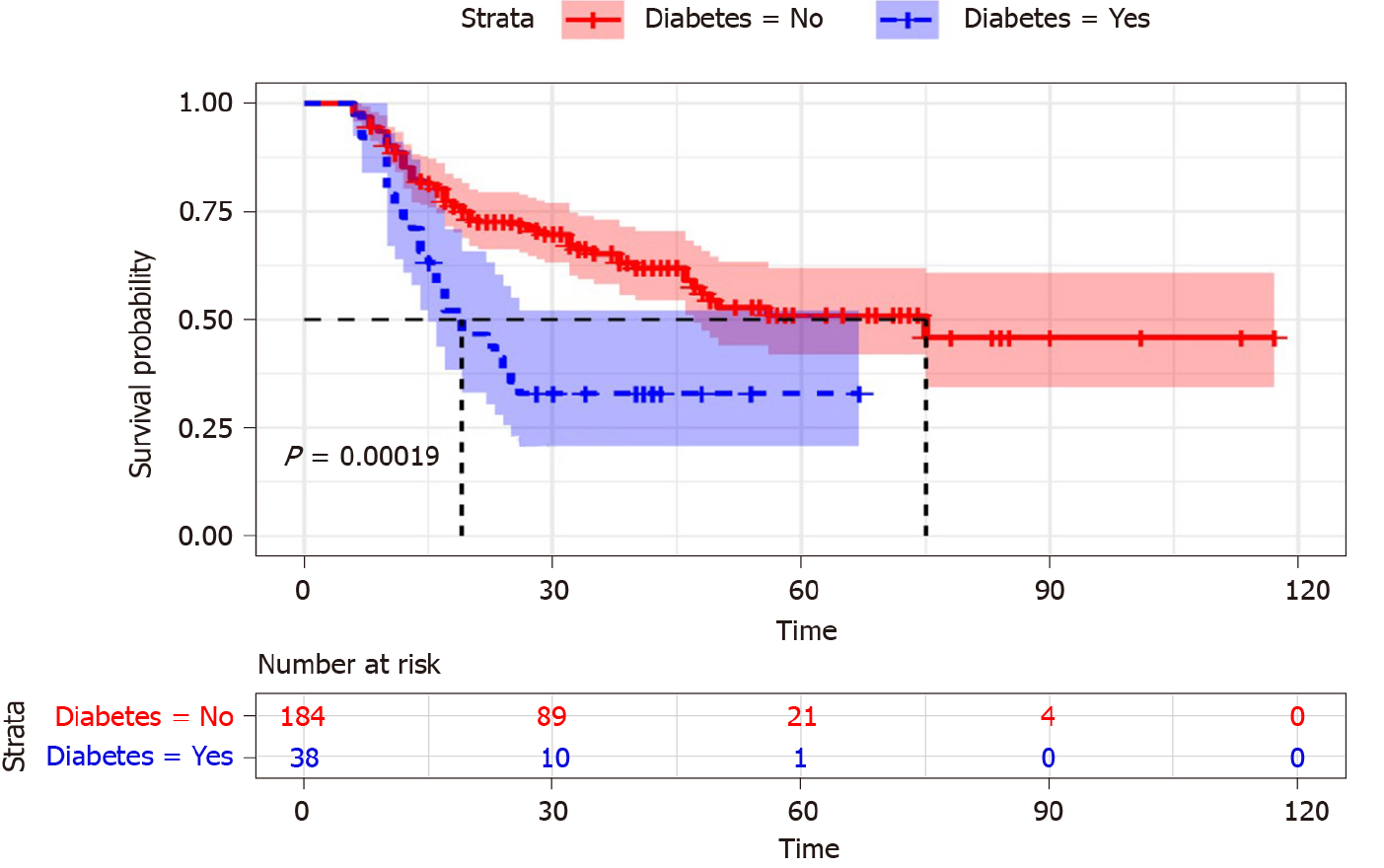
There are problems in the statistical analyses. Statistical analyses should be described in detail. In the table in the Results section, the author should provide more accurate statistical values, such as Student’s t-values or χ2 values. Table 1 shows that there are statistical differences in age between the DM group and non-DM group. Therefore, the author should describe the frequency and distribution of age in more detail and discuss the possible impact of age as a potential risk factor on the disease. For example, the author could divide the patients into different levels in the DM and non-DM groups according to age and statistically analyze the impact of different ages in each level on the mortality and infection rate of related diseases. According to the criteria of the World Health Organization in 2012[1,2], a younger age was defined as less than 45 years, and an older age was defined as greater or equal to 45 years. Therefore, the author could divide the original two groups into four groups. In Figure 1 (Figure in the manuscript "Effect of type 2 diabetes mellitus in the prognosis of acute-on-chronic liver failure patients in China"[1]), the author should indicate the time unit. We do not know how long the patients lived. In addition, we also noticed that the author did not indicate the corresponding P value when stating some conclusions.
| DM (yes) (n = 38) | DM (no) (n = 184) | P value | |
| Age (yr) | 56.32 ± 14.23 | 49.16 ± 12.84 | 0.002 |
| Gender, n (%) | 0.309 | ||
| Male | 28 (73.68) | 149 (80.98) | |
| Female | 10 (26.32) | 35 (19.02) | |
| Cause of disease, n (%) | 0.201 | ||
| Hepatitis B virus | 26 (68.42) | 139 (75.54) | |
| Hepatitis B virus + other | 5 (13.16) | 20 (10.87) | |
| Alcohol | 2 (5.26) | 15 (8.15) | |
| Others | 5 (13.16) | 10 (5.44) | |
| WBC (109/L) | 6.17 ± 4.03 | 7.35 ± 3.58 | 0.07 |
| RBC (1012/L) | 3.68 ± 0.87 | 3.94 ± 0.84 | 0.084 |
| Hb (g/L) | 117.21 ± 24.71 | 121.95 ± 23.13 | 0.257 |
| PLT (109/L) | 100.34 ± 42.20 | 118.79 ± 59.09 | 0.069 |
| PT (s) | 23.01 ± 5.38 | 24.45 ± 6.95 | 0.229 |
| INR | 1.97 ± 0.45 | 2.10 ± 0.59 | 0.229 |
| ALT (U/L) | 396.08 ± 448.56 | 560.36 ± 693.06 | 0.163 |
| AST (U/L) | 365.95 ± 391.18 | 419.99 ± 513.42 | 0.541 |
| γ-GGT (U/L) | 174.16 ± 305.61 | 137.57 ± 127.33 | 0.231 |
| TBIL (μmol/L) | 320.71 ± 141.31 | 309.56 ± 134.00 | 0.664 |
| ALB (g/L) | 29.25 ± 4.51 | 30.73 ± 4.03 | 0.045 |
| Scr (μmol/L) | 56.37 ± 22.00 | 63.45 ± 27.28 | 0.134 |
| BUN (mmol/L) | 3.94 ± 2.65 | 4.25 ± 2.98 | 0.56 |
| TCHO (mmol/L) | 2.67 ± 0.81 | 2.65 ± 1.05 | 0.919 |
| TG (mmol/L) | 1.45 ± 0.67 | 1.26 ± 0.70 | 0.124 |
| Na+ (mmol/L) | 136.98 ± 3.97 | 136.86 ± 4.43 | 0.878 |
| K+ (mmol/L) | 3.90 ± 0.46 | 4.08 ± 0.58 | 0.072 |
| AMON (μmol/L) | 3.90 ± 0.46 | 4.08 ± 0.58 | 0.332 |
| AFP (ng/mL) | 64.40 ± 40.39 | 128.19 ± 192.02 | 0.784 |
| BMI (kg/m2) | 24.99 ± 3.32 | 22.78 ± 3.03 | < 0.001 |
| FBG (mmol/L) | 5.34 ± 1.87 | 3.83 ± 1.07 | < 0.001 |
| Scoring systems | |||
| CTP | 10.79 ± 1.49 | 10.40 ± 1.35 | 0.115 |
| MELD | 19.38 ± 4.52 | 20.74 ± 5.06 | 0.128 |
| MELD-Na | 20.89 ± 5.00 | 22.27 ± 6.84 | 0.239 |
| Death, n (%) | 25 (65.79) | 69 (37.5) | 0.001 |
In the paper, the author repeatedly proposed that DM could predict ACLF. This is a confusing statement. The study only proves that DM has a certain influence on ACLF. To further predict ACLF through DM, a survival model would need to be established. The author should provide more detailed data, such as median follow-up and survival times, to build up the survival model.
In the Discussion section, the author explained that albumin (ALB) has nothing to do with the prognosis of liver failure in this study and believed that exogenous injection of ALB interfered with the experimental results. Inferring from this, we believe that the author neglected interference caused by the patients’ medications on the experimental results during treatment. ALB constitutes about half of serum proteins. ALB is involved in scavenging free radicals, maintaining colloidal osmotic pressure and protecting neuronal cells and is closely related to nutritional level[3] and systemic inflammatory response[4]. The author should describe in detail in the Methods section the type, dosage and method of drug injection during the treatment process. Actually, well-established indications for the use of human ALB in patients with cirrhosis pertain to conditions that are characterized by an acute deterioration of effective hypovolemia[5], such as renal dysfunction secondary to spontaneous bacterial peritonitis and hepatorenal syndrome, as shown by the international guidelines on the management of decompensated cirrhosis[6]. The current established indications for ALB use in patients with cirrhosis, such as preventing renal dysfunction induced by systolic blood pressure, suggest that patients should receive 1.5 g/kg body weight at diagnosis +1 g/kg body weight at day 3[7].
All in all, this is a high-level article in the field of diabetes and liver cirrhosis. Although there are some statistical deficiencies in the article, the author may be able to expand the sample and establish a multicenter prospective cohort study. For example, age factors could be considered for related diseases to evaluate the impact of DM on the prognosis in ACLF patients.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): E
P-Reviewer: Javed N, Pakistan; Saha S, India S-Editor: Fan JR L-Editor: Filipodia P-Editor: Fan JR
| 1. | Lai RM, Chen TB, Hu YH, Wu G, Zheng Q. Effect of type 2 diabetic mellitus in the prognosis of acute-on-chronic liver failure patients in China. World J Gastroenterol. 2021;27:3372-3385. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 2. | D'Angio RG. Is there a role for albumin administration in nutrition support? Ann Pharmacother. 1994;28:478-482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Zaccherini G, Bernardi M. The role and indications of albumin in advanced liver disease. Acta Gastroenterol Belg. 2019;82:301-308. [PubMed] |
| 4. | Garcia-Martinez R, Caraceni P, Bernardi M, Gines P, Arroyo V, Jalan R. Albumin: pathophysiologic basis of its role in the treatment of cirrhosis and its complications. Hepatology. 2013;58:1836-1846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 249] [Cited by in RCA: 308] [Article Influence: 25.7] [Reference Citation Analysis (0)] |
| 5. | European Association for the Study of the Liver. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis. J Hepatol. 2018;69:406-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1777] [Cited by in RCA: 1818] [Article Influence: 259.7] [Reference Citation Analysis (2)] |
| 6. | Margarson MP, Soni N. Serum albumin: touchstone or totem? Anaesthesia. 1998;53:789-803. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 217] [Cited by in RCA: 231] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 7. | World Health Day 2012 focuses on ageing and health. East Mediterr Health J. 2012;18:303. [PubMed] |