Published online Jun 14, 2021. doi: 10.3748/wjg.v27.i22.3073
Peer-review started: March 7, 2021
First decision: March 27, 2021
Revised: April 9, 2021
Accepted: April 28, 2021
Article in press: April 28, 2021
Published online: June 14, 2021
Processing time: 92 Days and 16.9 Hours
Inflammatory bowel disease (IBD) is a prevalent worldwide health problem featured by relapsing, chronic gastrointestinal inflammation. Enhancer of zeste homolog 2 (EZH2) is a critical epigenetic regulator in different pathological models, such as cancer and inflammation. However, the role of EZH2 in the IBD development is still obscure.
To explore the effect of EZH2 on IBD progression and the underlying mechanism.
The IBD mouse model was conducted by adding dextran sodium sulfate (DSS), and the effect of EZH2 on DSS-induced colitis was assessed in the model. The function of EZH2 in regulating apoptosis and permeability was evaluated by Annexin V-FITC Apoptosis Detection Kit, transepithelial electrical resistance analysis, and Western blot analysis of related markers, including Zona occludens 1, claudin-5, and occludin, in NCM460 and fetal human colon (FHC) cells. The mechanical investigation was performed by quantitative reverse transcription-polymerase chain reaction, Western blot analysis, and chromatin immunoprecipitation assays.
The colon length was inhibited in the DSS-treated mice and was enhanced by the EZH2 depletion in the system. DSS treatment caused a decreased histological score in the mice, which was reversed by EZH2 depletion. The inflammatory cytokines, such as tumor necrosis factor-α, interleukin-6, and interleukin-1β, were induced in the DSS-treated mice, in which the depletion of EZH2 could reverse this effect. Moreover, the tumor necrosis factor-α treatment induced the apoptosis of NCM460 and FHC cells, in which EZH2 depletion could reverse this effect in the cells. Moreover, the depletion of EZH2 attenuated permeability of colonic epithelial cells. Mechanically, the depletion of EZH2 or EZH2 inhibitor GSK343 was able to enhance the expression and the phosphorylation of janus kinase 2 (JK2) and signal transducer and activator of transcription in the NCM460 and FHC cells. Specifically, EZH2 inactivated JAK2 expression by regulating histone H3K27me3. JAK2 inhibitor TG101348 was able to reverse EZH2 knockdown-mediated colonic epithelial cell permeability and apoptosis.
Thus, we concluded that EZH2 contributed to apoptosis and inflammatory response by inactivating JAK2/ signal transducer and activator of transcription signaling in IBD. EZH2 may be applied as a potential target for IBD therapy.
Core Tip: In this study, we discovered that enhancer of zeste homolog 2 contributed to apoptosis and inflammatory response by inactivating janus kinase 2/signal transducer and activator of transcription signaling in inflammatory bowel disease (IBD). Enhancer of zeste homolog 2 may be applied as a potential target for IBD therapy.
- Citation: Zhou J, Yang Y, Wang YL, Zhao Y, Ye WJ, Deng SY, Lang JY, Lu S. Enhancer of zeste homolog 2 contributes to apoptosis by inactivating janus kinase 2/ signal transducer and activator of transcription signaling in inflammatory bowel disease. World J Gastroenterol 2021; 27(22): 3073-3084
- URL: https://www.wjgnet.com/1007-9327/full/v27/i22/3073.htm
- DOI: https://dx.doi.org/10.3748/wjg.v27.i22.3073
Inflammatory bowel disease (IBD) is a worldwide health problem with an increasing incidence. IBD, including Crohn’s disease and ulcerative colitis and IBD unclassified, is described as relapsing, chronic gastrointestinal inflammation[1,2]. IBD patients experience low life quality and a higher risk of colorectal cancer[3]. The critical feature of IBD is the unsolved inflammation of the intestinal field caused by a breakdown to shift from a pro-inflammatory situation to an anti-inflammatory situation[4]. Various immune cell populations, such as eosinophils, neutrophils, dendritic cells, and macrophages, are present in the intestinal mucosa, participating in inflammation during IBD[5,6]. These cells participate in inflammation by secreting chemokines, antimicrobial agents, and pro-inflammatory cytokines, such as tumor necrosis factor (TNF)-α, interleukin (IL)-6[3], and IL-1β[7]. Therefore, the understanding of the molecular mechanism underlying the inflammatory regulation during IBD progre
The fundamental function of epigenetic systems in determining T cell lineage fate decisions has been completely defined[8,9]. Nevertheless, the effect of the histone methyltransferase enhancer of zeste homolog 2 (EZH2) has been recently identified in the process[10,11]. EZH2 serves as a methylation of histone H3K27 to H3K27me3[12]. It has been found that targeting EZH2 is able to alleviate intestinal inflammation in IBD[11]. Moreover, janus kinase 2 (JK2)/ signal transducer and activator of transcription 3 (STAT3) signaling has been identified to alleviate inflammation response during IBD[13]. However, the correlation of EZH2 with JAK2/STAT3 signaling in the IBD development remains unclear. In this study, we were interested in the molecular mechanism of EZH2-mediated IBD progression.
The NCM460 and fetal human colon (FHC) cell lines were maintained in the lab and were incubated at 37 °C with 5% CO2 in Dulbecco’s Modified Eagle Medium (GE, United States) containing fetal bovine serum (15%; GE Healthcare, Chicago, IL, United States), streptomycin (0.1 mg/mL), and penicillin (100 units/mL). The lentiviral plasmids carrying EZH2 short hairpin ribonucleic acid (shRNA) and the corresponding control shRNA were obtained (GenScript, Nanjing, China). The transfection in the cells was performed by Liposome 3000 (Invitrogen, Carlsbad, CA, United States). The EZH2 inhibitor GSK343 (Sigma, St. Louis, MO, United States) and JAK2 inhibitor TG101348 (Selleck, Houston, TX, United States) were used at the dose of 5 μmol/L. The TNF-α (Sigma) was used at the dose of 50 ng/mL.
The clinical IBD samples (n = 50) and non-IBD control cases (n = 50) were collected from The Third People's Hospital of Chengdu. The diagnosis of IBD was consistent with the standard combination of radiologic, histological, endoscopic, and clinical criteria. The application of the samples was under the approval of the patients and proved by the Ethics Committee of Sichuan Cancer Hospital & Institute. The patients provided their written informed consent to participate in this study.
C57BL/6 mice (female, 6–8 wk) were obtained from the Chinese Academy of Medical Sciences (Beijing, China). The mice were randomly divided into three groups: Water group; dextran sodium sulfate (DSS) group; DSS + shEZH2 group. The mice in DSS and DSS + shEZH2 groups were constructed by adding DSS (2.5%, MP Biomedicals, Santa Ana, CA, United States) to drinking water for 7 d, followed by normal drinking water for the remaining days. The mice in DSS + shEZH2 groups were intraperitoneally injected with lentiviral plasmids carrying EZH2 shRNA (GenScript). The mice received DSS (3%) to induce intestinal inflammation, and the natural death time of mice in the indicated groups within 15 d was recorded. The body weight was recorded at the indicated time. The colon length was measured and calculated using a ruler. The tissues were treated with 4% paraformaldehyde, and the decalcification was conducted in 5% nitric acid, followed by cutting into 5 μm sections. A set of alcohols was applied for the dehydration of the samples. Afterward, hematoxylin and eosin staining was performed in the slice samples of femoral head and then observed by microscope (BX-42; Olympus, Tokyo, Japan). The histologic score used to quantify the effect of EZH2 depletion in the mouse model by the pathologist was according to the criteria: Crypt architecture (normal, 0–severe crypt distortion with loss of entire crypts, 3), degree of inflammatory cell infiltration (normal, 0–dense inflammatory infiltrate, 3), muscle thickening (base of crypt sits on the muscularis mucosae, 0–marked muscle thickening, 3), crypt abscess (absent, 0–present, 1), and goblet cell depletion (absent, 0–present, 1)[1,2]. The levels of cytokines were measured by enzyme-linked immunosorbent assays (Sigma). Animal care was authorized by the Animal Ethics Committee. All experimental procedures with mice were performed in accordance and compliance with the regulations of the Laboratory Animal Welfare and Ethics Committee of Sichuan Cancer Hospital & Institute.
About 2 × 105 NCM460 and FHC cells were plated on 6-well dishes. Cell apoptosis was assessed by employing the Annexin V-FITC Apoptosis Detection Kit (Sigma) using the manufacture’s instruction. Shortly, about 2 × 105 collected and washed cells collected by binding buffer and were dyed at 25 °C, followed by the flow cytometry analysis.
Total RNAs were extracted using TRIZOL (Invitrogen). The first-strand complementary (c)DNA was manufactured as the manufacturer's instruction (TaKaRa, Kyoto, Japan). The quantitative reverse transcription-polymerase chain reaction was carried out by applying SYBR-Green (TaKaRa). The primer sequences are as follows: EZH2 forward: 5′-AATCAGAGTACATGCGACTGAGA-3′, reverse: 5′-GCTGTATCCTTCGCTGTTTCC; JAK2 forward: 5′-GCCTTCTTTCAGAGCCATCAT-3′, reverse: 5′-GTGTAGGATCCCGGTCTTCAA-3′; Glyceraldehyde-3-phosphate dehydrogenase forward: 5′-AACGGATTTGGTCGTATTGGG-3′, reverse: 5′-CCTGGAAGATGGTGATGGGAT-3′.
Total proteins were extracted from the cells using radioimmunoprecipitation assay buffer (Cell Signaling Technology, Danvers, MA, United States) and quantified using the BCA Protein Quantification Kit (Abbkine, Wuhan, China). The proteins at same concentration were subjected to sodium dodecyl sulfate-polyacrylamide gel electrophoresis and transferred to poly(vinylidene fluoride) membranes (Millipore, Burlington, MA, United States), followed by the incubation with 5% milk and with the primary antibodies at 4 °C overnight. The corresponding secondary antibodies (Boster, Wuhan, China) were used for incubating the membranes 1 h at room temperature, followed visualization by using chemiluminescence detection kit (Beyotime, Beijing, China). The primary antibodies applied in this study comprised EZH2 (Abcam, Cambridge, United Kingdom), Zona occludens 1 (ZO-1) (Abcam), claudin-5 (Abcam), occludin (Abcam), H3K27me3 (Abcam), JAK2 (Abcam), STAT3 (Abcam), p-JAK2 (Abcam), p-STAT3 (Abcam), EZH2 (Abcam), caspase3, cleaved-caspase3 (Abcam), and β-actin (Abcam).
Chromatin immunoprecipitation (ChIP) was performed using a SimpleChIP Enzymatic ChIP Kit (Cell Signaling Technology) according to the manufacturer's instruction. Chromatin prepared from the cells in a 15 cm dish was used to determine total DNA input and was incubated overnight with specific antibodies or normal rabbit immunoglobulin G. Then, the binding DNA was analyzed by quantitative-polymerase chain reaction assays; the primer sequences were shown as above.
Transepithelial electrical resistance (TEER) measurement was used to analyze the barrier function of the intestine. About 2 × 105 cells/mL cells were layered on collagen-covered polycarbonate penetrable support supplements (Corning, Corning, NY, United States). The medium was replaced every 2 d. The production of the cells polarized monolayer at 3 wk was settled by monitoring and morphology of TEER by employing Millicell-ERS2 (Merck-Millipore). Delta-toxin was used to polarized monolayer cells at 37 °C.
The data were normally distributed. Data were expressed as mean ± SD, and the statistical analysis was conducted using GraphPad prism 7 (San Diego, CA, United States). The unpaired Student’s t-test was used to compare two groups, and the one-way analysis of variance was used to compare multiple groups. P < 0.05 was considered as statistically significant.
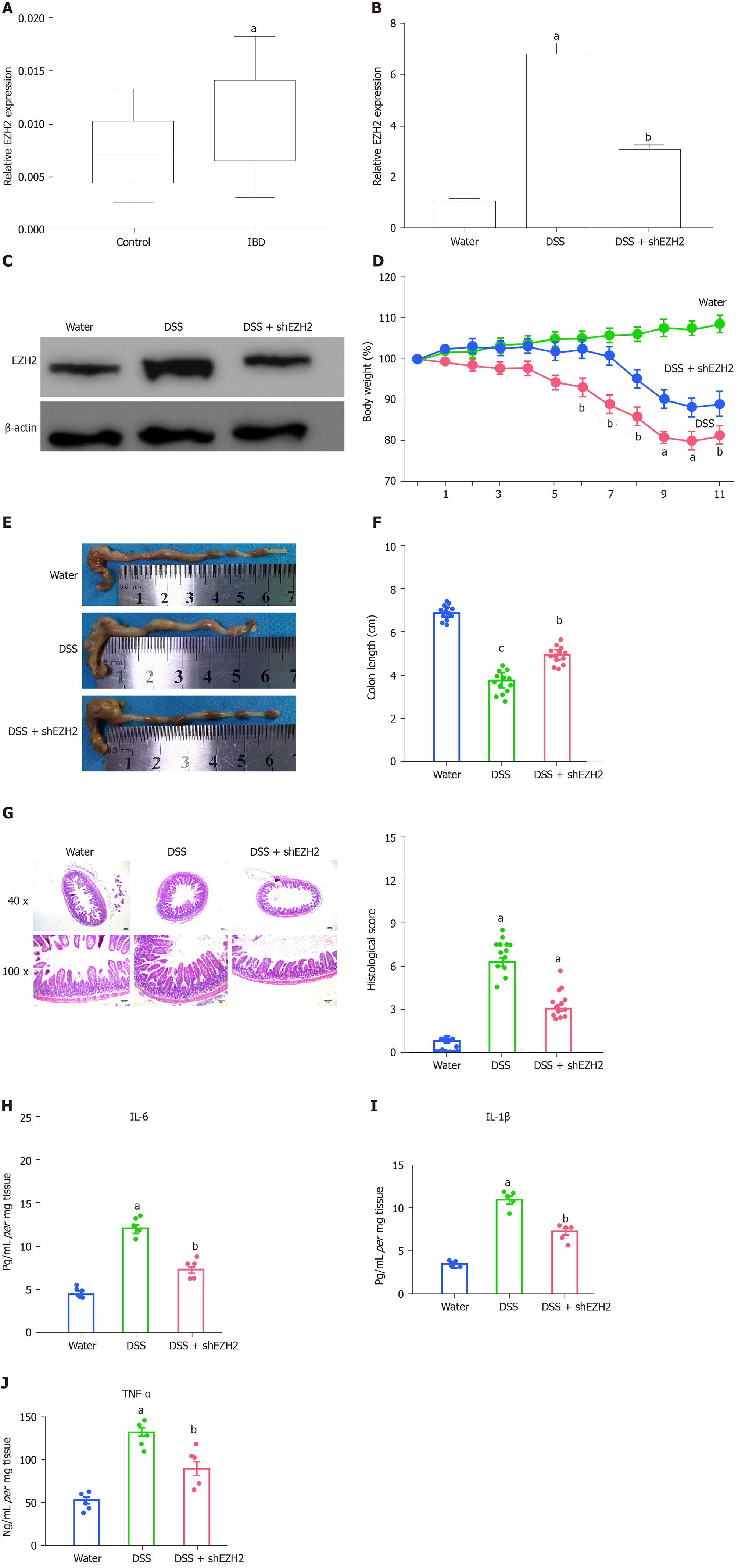
Firstly, we identified that the expression of EZH2 was enhanced in clinical IBD samples (n = 50) relative to healthy controls (n = 50) (Figure 1A). Meanwhile, we found that DSS enhanced EZH2 expression in mice, while the depletion of EZH2 by shRNA repressed the enhancement (Figure 1B and C). We then measured the effect of EZH2 on the DSS-induced colitis in vivo. We observed that the DSS treatment significantly resulted in a weight loss of the mice, which was attenuated by EZH2 depletion (Figure 1D). The colon length was reduced in the DSS-treated mice and was rescued by the EZH2 depletion in the system (Figure 1E and F). Meanwhile, the DSS treatment caused a decreased histological score in the mice, which was rescued by EZH2 depletion (Figure 1G). Moreover, the inflammatory cytokines, such as IL-6, IL-1β, and TNF-α, were enhanced in the DSS-treated mice, in which the depletion of EZH2 could reverse this effect (Figure 1H-J).
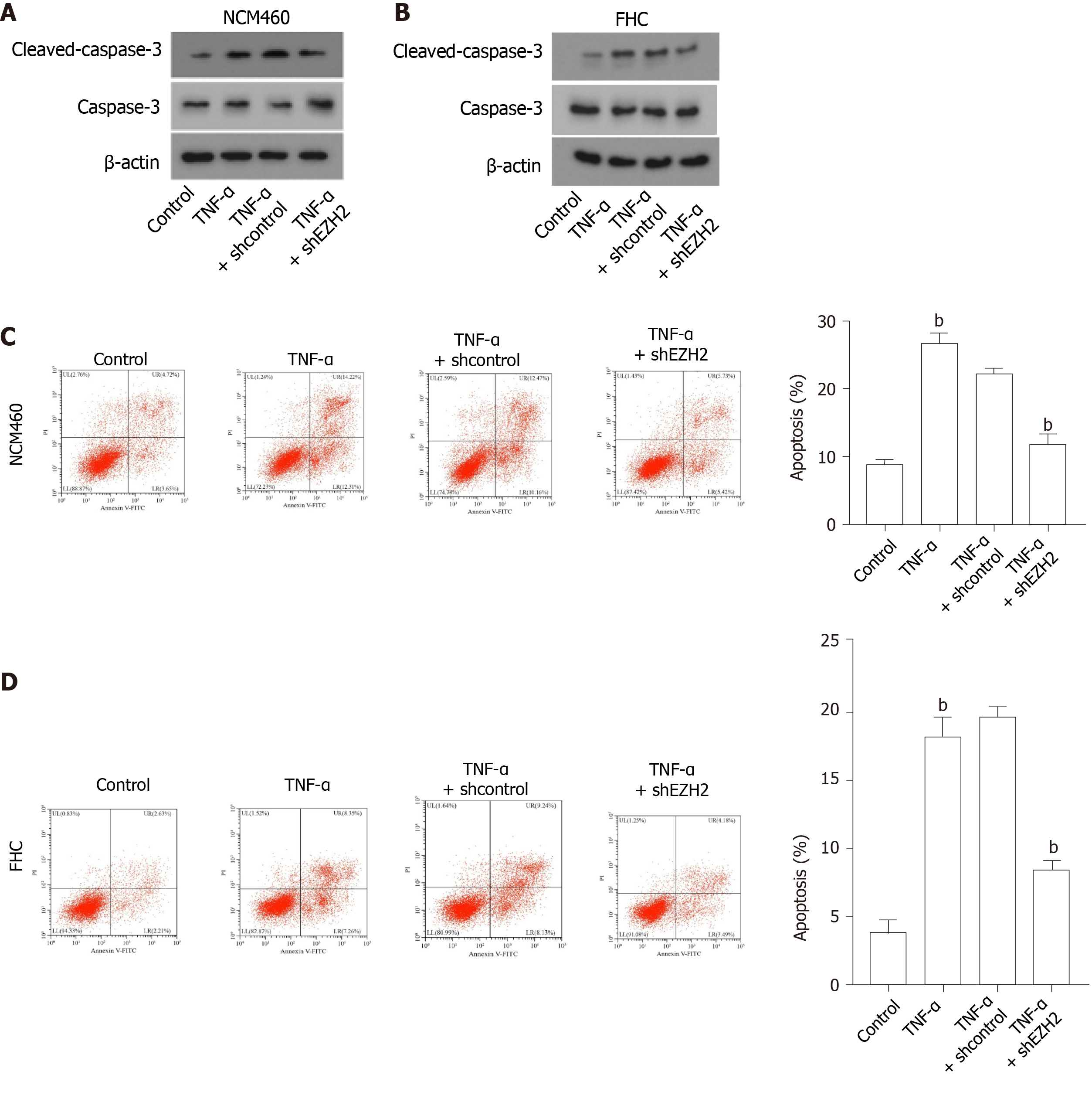
Then, the NCM460 and FHC colonic epithelial cells were treated with TNF-α or co-treated with TNF-α and EZH2 shRNA. We found that the expression of cleaved-caspase-3 was enhanced in the TNF-α-treated NCM460 and FHC cells, and the depletion of EZH2 was able to inhibit the enhancement in the cells (Figure 2A and B). Moreover, the TNF-α treatment induced the apoptosis of NCM460 and FHC cells, in which EZH2 knockdown could reverse this effect in the cells (Figure 2C and D).
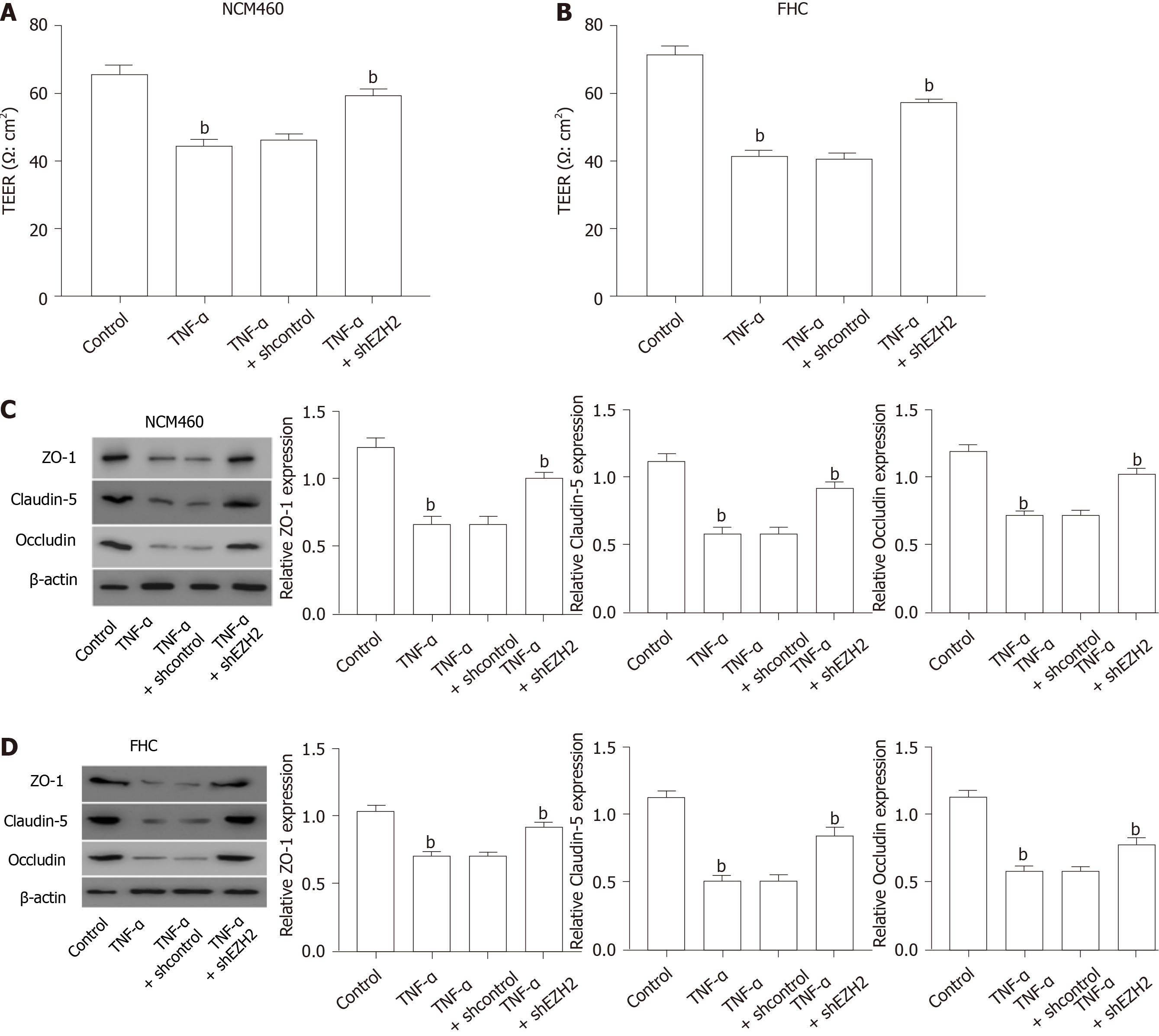
Next, we further identified that the TEER was reduced by TNF-α treatment in the NCM460 and FHC cells, which was rescued by the depletion of EZH2 in the cells (Figure 3A and B). Consistently, the expression of permeability markers, including ZO-1, claudin-5, and occludin, was inhibited in the TNF-α-treated NCM460 and FHC cells, but the EZH2 depletion could rescue this phenotype in the cells (Figure 3C and D).
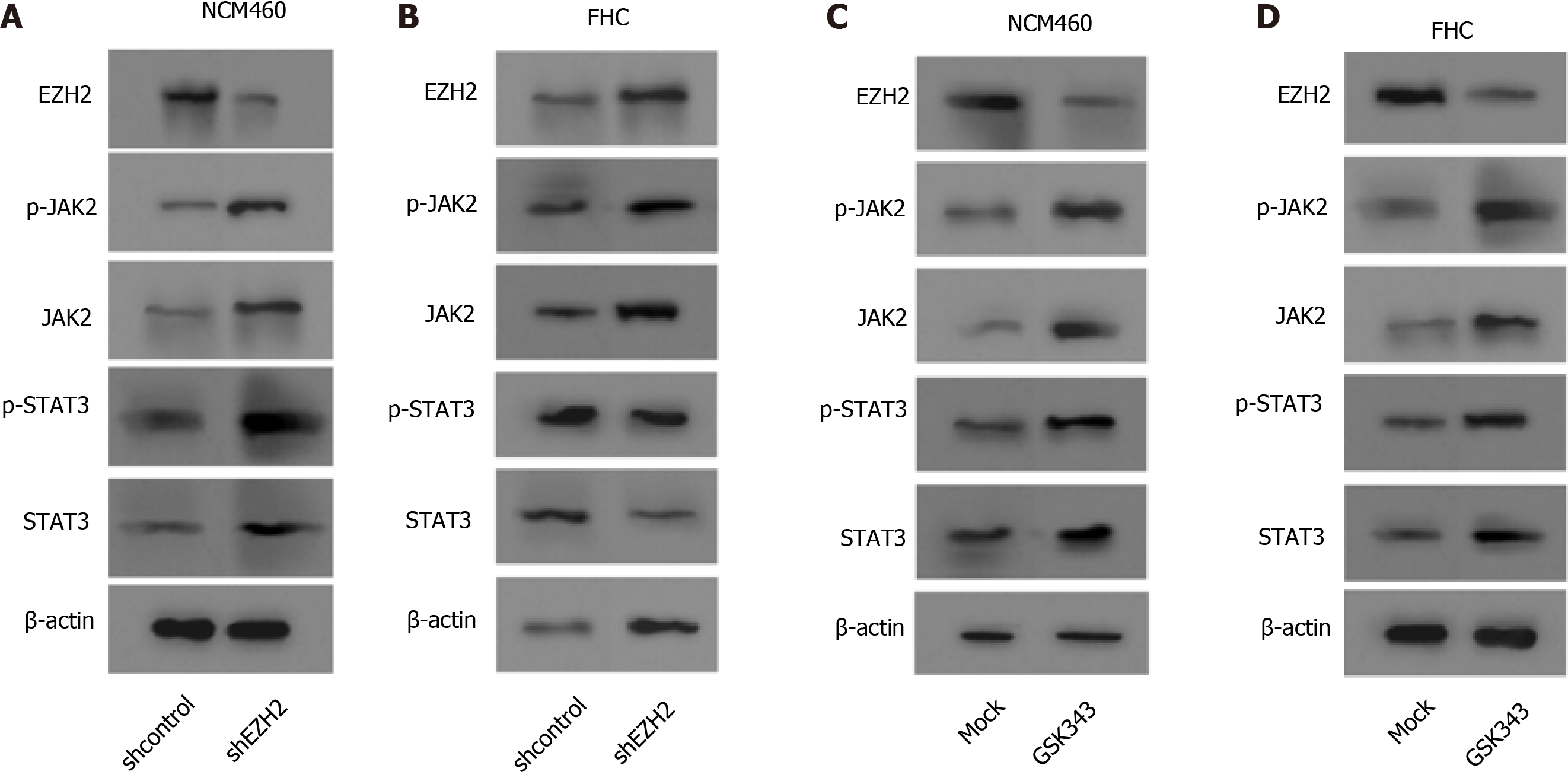
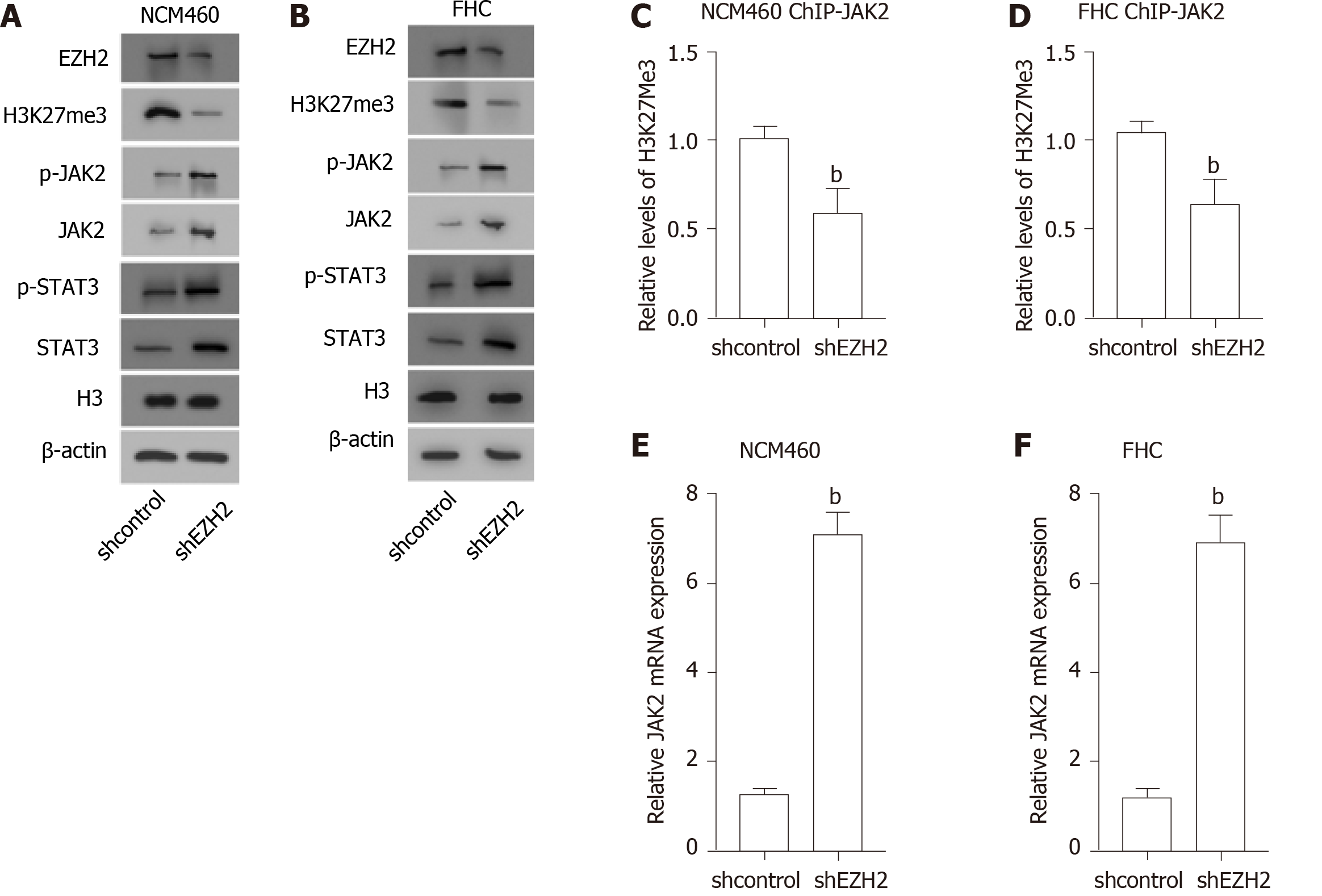
Significantly, Western blot analysis showed that the depletion of EZH2 enhanced the expression and the phosphorylation of JAK2 and STAT3 in the NCM460 and FHC cells (Figure 4A and B). Meanwhile, the expression and the phosphorylation of JAK2 and STAT3 EZH2 inhibitor were induced by the EZH2 inhibitor GSK343 in the cells (Figure 4C and D).
Furthermore, we observed that the H3K27me3 was reduced, along with the enhanced expression and the phosphorylation of JAK2 and STAT3, in the EZH2-knockdown NCM460 and FHC cells (Figure 5A and B). In addition, the depletion of EZH2 reduced the levels of H3K27me3 on the promoter of JAK2 in the cells (Figure 5C and D). Consistently, the mRNA expression of JAK2 was up-regulated by EZH2 depletion in the NCM460 and FHC cells (Figure 5E and F).
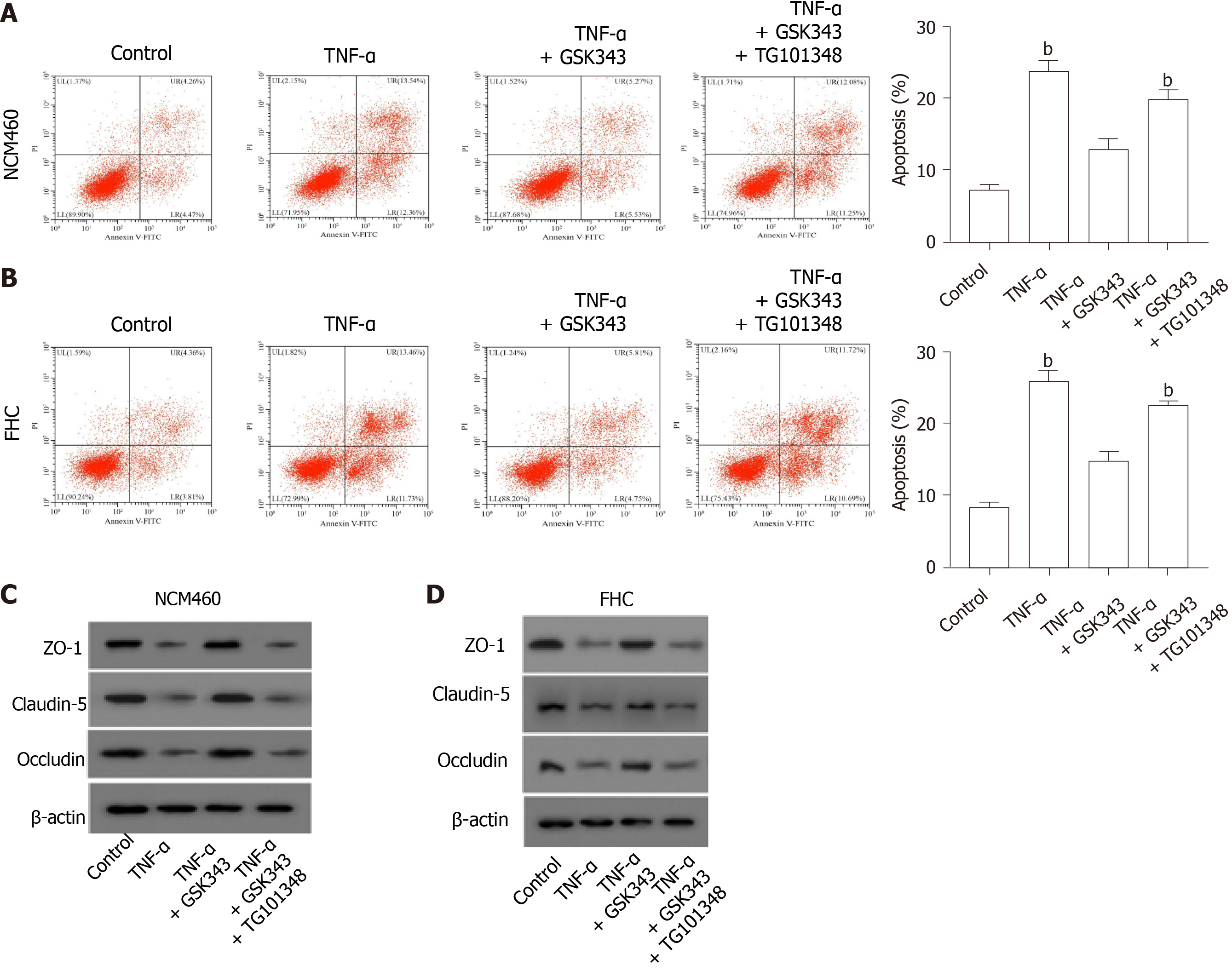
Next, we identified that EZH2 inhibitor GSK343 attenuated TNF-α-induced apoptosis of the NCM460 and FHC cells, and the JAK2 inhibitor TG101348 was able to rescue the phenotype in the cells (Figure 6A and B). Moreover, GSK343 rescued TNF-α-inhibited ZO-1, claudin-5, and occludin expression in the NCM460 and FHC cells, in which the co-treatment with TG101348 could reverse this effect in the system (Figure 6C and D).
IBD is a prevalent inflammatory gastrointestinal disease with high incidence. As a critical epigenetic regulator, EZH2 has been identified to contribute to IBD progression, but the mechanism remains unclear. In this study, we found that EZH2 promoted apoptosis and inflammatory response by inactivating JAK2/STAT signaling in IBD.
Several previous investigations have shown the function of EZH2 in the modulation of IBD. It has been reported that EZH2 is involved in the pathobiological mechanism of IBD progression[14]. Inhibiting EZH2 attenuates intestinal inflammation of IBD development[11]. EZH2 is an epigenetic regulator in colitis by inhibiting TNF-α-regulated apoptosis and inflammation in IBD[15]. EZH2 modulates intestinal necroptosis and inflammation in intestinal epithelial cells by c-jun N-terminal kinase signaling[16]. Targeting EZH2 enhances cAMP response element-binding protein to inhibit the ulcerative colitis progression[17]. It has been well-recognized that EZH2 presents a critical biological significance of in autoimmune disorders and cancer, and thereby targeting EZH2 is a promising therapeutic strategy in these diseases[18,19]. In this study, we demonstrated that the depletion of EZH2 inhibited DSS-induced colitis in vivo. EZH2 depletion attenuated apoptosis and permeability of colonic epithelial cells. Our data identified a critical role of EZH2 in the IBD progression, providing informative evidence of the function of EZH2 in modulating IBD development.
As essential cellular signaling in various pathological conditions, JAK2/STAT3 signaling plays critical role in IBD regulation. It has been found that V617F is able to up-regulate JAK2 expression in patients with IBD[20]. Sphk1 enhances ulcerative colitis by modulating JAK2/STAT3 signaling[21]. Renin-angiotensin system contributes to colonic inflammation by inducing helper T 17 activation through JAK2/STAT signaling[22]. A20 inhibits IBD via repressing nuclear factor-kappa B and STAT3 in mice[23]. Our mechanical studies showed that EZH2 inactivated JAK2 expression by regulating histone H3K27me3. EZH2 promoted apoptosis and permeability by inactivating JAK2/STAT signaling in colonic epithelial cells. These data discover an unreported association of EZH2 with JAK2/STAT signaling, elucidating a new mechanism involving EZH2 and JAK2/STAT in IBD pathogenesis.
In conclusion, we discovered that EZH2 contributed to apoptosis and inflammatory response by inactivating JAK2/STAT signaling in IBD. EZH2 is a promising target for treatment of IBD.
Inflammatory bowel disease (IBD) is a prevalent worldwide health problem featured by relapsing, chronic gastrointestinal inflammation. Enhancer of zeste homolog 2 (EZH2) is a critical epigenetic regulator in different pathological models, such as cancer and inflammation. However, the role of EZH2 in the IBD development is still obscure.
To identify the effect of EZH2 on the IBD progression and the underlying mechanism.
To explore the role of EZH2 in the IBD progression and the underlying mechanism.
The IBD mouse model was conducted by adding dextran sodium sulfate (DSS) and examining the effect of EZH2 on DSS-induced colitis in the model. The function of EZH2 in regulating apoptosis and permeability was evaluated by Annexin V-FITC Apoptosis Detection Kit, transepithelial electrical resistance analysis, and Western blot analysis of related markers, including Zona occludens 1, claudin-5, and occludin, in NCM460 and fetal human colon (FHC) cells. The mechanical investigation was performed by quantitative reverse transcription-polymerase chain reaction, Western blot analysis, and chromatin immunoprecipitation assays.
The colon length was inhibited in the DSS-treated mice and was enhanced by the EZH2 depletion in the system. DSS treatment caused a decreased histological score in the mice, which was reversed by EZH2 depletion. The inflammatory cytokines, such as tumor necrosis factor (TNF)-α, interleukin-6, and interleukin-1β, were induced in the DSS-treated mice, in which the depletion of EZH2 could reverse this effect. Moreover, the TNF-α treatment induced the apoptosis of NCM460 and FHC cells, in which EZH2 depletion could reverse this effect in the cells. Moreover, the depletion of EZH2 attenuated permeability of colonic epithelial cells. Mechanically, the depletion of EZH2 or EZH2 inhibitor GSK343 was able to enhance the expression and the phospho
EZH2 contributes to apoptosis and inflammatory response by inactivating JAK2/STAT signaling in IBD.
EZH2 may be applied as a potential target for IBD therapy.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chen P, Gatti S S-Editor: Fan JR L-Editor: Filipodia P-Editor: Wang LL
| 1. | Speca S, Dubuquoy L. Chronic bowel inflammation and inflammatory joint disease: Pathophysiology. Joint Bone Spine. 2017;84:417-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 2. | Sands BE. Biomarkers of Inflammation in Inflammatory Bowel Disease. Gastroenterology. 2015;149:1275-1285.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 213] [Cited by in RCA: 288] [Article Influence: 28.8] [Reference Citation Analysis (0)] |
| 3. | Franzosa EA, Sirota-Madi A, Avila-Pacheco J, Fornelos N, Haiser HJ, Reinker S, Vatanen T, Hall AB, Mallick H, McIver LJ, Sauk JS, Wilson RG, Stevens BW, Scott JM, Pierce K, Deik AA, Bullock K, Imhann F, Porter JA, Zhernakova A, Fu J, Weersma RK, Wijmenga C, Clish CB, Vlamakis H, Huttenhower C, Xavier RJ. Gut microbiome structure and metabolic activity in inflammatory bowel disease. Nat Microbiol. 2019;4:293-305. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 888] [Cited by in RCA: 1228] [Article Influence: 204.7] [Reference Citation Analysis (0)] |
| 4. | Shao BZ, Wang SL, Pan P, Yao J, Wu K, Li ZS, Bai Y, Linghu EQ. Targeting NLRP3 Inflammasome in Inflammatory Bowel Disease: Putting out the Fire of Inflammation. Inflammation. 2019;42:1147-1159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 81] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 5. | Graham DB, Xavier RJ. Pathway paradigms revealed from the genetics of inflammatory bowel disease. Nature. 2020;578:527-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 459] [Cited by in RCA: 469] [Article Influence: 93.8] [Reference Citation Analysis (0)] |
| 6. | Wright EK, Ding NS, Niewiadomski O. Management of inflammatory bowel disease. Med J Aust. 2018;209:318-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 74] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 7. | Halfvarson J, Brislawn CJ, Lamendella R, Vázquez-Baeza Y, Walters WA, Bramer LM, D'Amato M, Bonfiglio F, McDonald D, Gonzalez A, McClure EE, Dunklebarger MF, Knight R, Jansson JK. Dynamics of the human gut microbiome in inflammatory bowel disease. Nat Microbiol. 2017;2:17004. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 605] [Cited by in RCA: 820] [Article Influence: 102.5] [Reference Citation Analysis (0)] |
| 8. | Schmidl C, Delacher M, Huehn J, Feuerer M. Epigenetic mechanisms regulating T-cell responses. J Allergy Clin Immunol. 2018;142:728-743. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 98] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 9. | Henning AN, Roychoudhuri R, Restifo NP. Epigenetic control of CD8+ T cell differentiation. Nat Rev Immunol. 2018;18:340-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 341] [Cited by in RCA: 377] [Article Influence: 53.9] [Reference Citation Analysis (0)] |
| 10. | O'Meara MM, Simon JA. Inner workings and regulatory inputs that control Polycomb repressive complex 2. Chromosoma. 2012;121:221-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 62] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 11. | Zhou J, Huang S, Wang Z, Huang J, Xu L, Tang X, Wan YY, Li QJ, Symonds ALJ, Long H, Zhu B. Targeting EZH2 histone methyltransferase activity alleviates experimental intestinal inflammation. Nat Commun. 2019;10:2427. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 116] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 12. | Duan R, Du W, Guo W. EZH2: a novel target for cancer treatment. J Hematol Oncol. 2020;13:104. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 435] [Cited by in RCA: 597] [Article Influence: 119.4] [Reference Citation Analysis (0)] |
| 13. | Polgar N, Csongei V, Szabo M, Zambo V, Melegh BI, Sumegi K, Nagy G, Tulassay Z, Melegh B. Investigation of JAK2, STAT3 and CCR6 polymorphisms and their gene-gene interactions in inflammatory bowel disease. Int J Immunogenet. 2012;39:247-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 14. | Sarmento OF, Svingen PA, Xiong Y, Sun Z, Bamidele AO, Mathison AJ, Smyrk TC, Nair AA, Gonzalez MM, Sagstetter MR, Baheti S, McGovern DP, Friton JJ, Papadakis KA, Gautam G, Xavier RJ, Urrutia RA, Faubion WA. The Role of the Histone Methyltransferase Enhancer of Zeste Homolog 2 (EZH2) in the Pathobiological Mechanisms Underlying Inflammatory Bowel Disease (IBD). J Biol Chem. 2017;292:706-722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 56] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 15. | Liu Y, Peng J, Sun T, Li N, Zhang L, Ren J, Yuan H, Kan S, Pan Q, Li X, Ding Y, Jiang M, Cong X, Tan M, Ma Y, Fu D, Cai S, Xiao Y, Wang X, Qin J. Epithelial EZH2 serves as an epigenetic determinant in experimental colitis by inhibiting TNFα-mediated inflammation and apoptosis. Proc Natl Acad Sci USA. 2017;114:E3796-E3805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 75] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 16. | Lou X, Zhu H, Ning L, Li C, Li S, Du H, Zhou X, Xu G. EZH2 Regulates Intestinal Inflammation and Necroptosis Through the JNK Signaling Pathway in Intestinal Epithelial Cells. Dig Dis Sci. 2019;64:3518-3527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 17. | Li K, Yang J, Lei XF, Li SL, Yang HL, Xu CQ, Deng L. EZH2 inhibition promotes ANGPTL4/CREB1 to suppress the progression of ulcerative colitis. Life Sci. 2020;250:117553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 18. | Yang YX, Shen HH, Cao F, Xie LY, Zhu GL, Sam NB, Wang DG, Pan HF. Therapeutic potential of enhancer of zeste homolog 2 in autoimmune diseases. Expert Opin Ther Targets. 2019;23:1015-1030. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 19. | Stazi G, Zwergel C, Mai A, Valente S. EZH2 inhibitors: a patent review (2014-2016). Expert Opin Ther Pat. 2017;27:797-813. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 37] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 20. | Asadzadeh-Aghdaei H, Mashayekhi K, Koushki K, Azimzadeh P, Rostami-Nejad M, Amani D, Chaleshi V, Haftcheshmeh SM, Sahebkar A, Zali MR. V617F-independent upregulation of JAK2 gene expression in patients with inflammatory bowel disease. J Cell Biochem. 2019;120:15746-15755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 21. | Liu J, Jiang B. Sphk1 promotes ulcerative colitis via activating JAK2/STAT3 signaling pathway. Hum Cell. 2020;33:57-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 22. | He L, Du J, Chen Y, Liu C, Zhou M, Adhikari S, Rubin DT, Pekow J, Li YC. Renin-angiotensin system promotes colonic inflammation by inducing TH17 activation via JAK2/STAT pathway. Am J Physiol Gastrointest Liver Physiol. 2019;316:G774-G784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 23. | Lee SH, Lee HR, Kwon JY, Jung K, Kim SY, Cho KH, Choi J, Lee HH, Lee BI, Jue DM, Cho ML. A20 ameliorates inflammatory bowel disease in mice via inhibiting NF-κB and STAT3 activation. Immunol Lett. 2018;198:44-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |