Published online Jan 28, 2020. doi: 10.3748/wjg.v26.i4.375
Peer-review started: Otober 11, 2019
First decision: December 5, 2019
Revised: January 2, 2020
Accepted: January 11, 2020
Article in press: January 11, 2020
Published online: January 28, 2020
Processing time: 98 Days and 10.2 Hours
Pancreatic ductal adenocarcinoma is an aggressive cancer with high recurrence rates following surgical resection. While adjuvant chemotherapy improves survival, a significant proportion of patients are unable to initiate or complete all intended therapy following pancreatectomy due to postoperative complications or poor performance status. The administration of chemotherapy prior to surgical resection is an alternative strategy that ensures its early and near universal delivery as well as improves margin-negative resection rates and potentially improves long-term survival outcomes. Neoadjuvant therapy is increasingly being recommended to patients with pancreatic ductal adenocarcinoma, however, patient-centered research on its use is lacking. In this review, we highlight opportunities to focus research efforts in the domains of patient preferences, patient-reported outcomes, patient experience, and survivorship. Novel research in these areas may identify relevant barriers and facilitators to the use of neoadjuvant therapy thereby increasing its utilization, improve shared-decision making for patients and providers, and optimize the experience of those undergoing neoadjuvant therapy.
Core tip: Neoadjuvant therapy is increasingly being recommended to patients with pancreatic ductal adenocarcinoma, however, patient-centered research on its use is lacking. In this review, we highlight opportunities to focus research efforts in the domains of patient preferences, patient-reported outcomes, patient experience, and survivorship. Novel research in these areas may identify relevant barriers and facilitators to the use of neoadjuvant therapy thereby increasing its utilization, improving shared-decision making for patients and providers, and optimizing the experience of those undergoing neoadjuvant therapy.
- Citation: Cloyd JM, Tsung A, Hays J, Wills CE, Bridges JF. Neoadjuvant therapy for resectable pancreatic ductal adenocarcinoma: The need for patient-centered research. World J Gastroenterol 2020; 26(4): 375-382
- URL: https://www.wjgnet.com/1007-9327/full/v26/i4/375.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i4.375
Pancreatic ductal adenocarcinoma (PDAC) is a leading cause of cancer-related mortality worldwide with a 5-year overall survival rate of only 9%[1]. Although the majority of patients with PDAC present with locally advanced or metastatic disease, even those with resectable cancers who undergo potentially curative surgery are likely to experience cancer recurrence. For all patients with resectable cancers, adjuvant chemotherapy after surgery improves overall survival[2-4]. However, up to 50% of patients who undergo pancreatectomy fail to initiate adjuvant chemotherapy typically due to postoperative complications or poor performance status[5] and a greater number of patients fail to complete the intended course of adjuvant therapy for similar reasons[6].
The administration of chemotherapy prior to surgical resection is an alternative strategy that ensures its early and near universal delivery. Neoadjuvant therapy (NT) offers several other theoretical benefits including improved margin-negative resection rates, decreased lymph node positivity, early treatment of presumed micro-metastatic disease, and the ability to measure in vivo response to therapy histologically after resection[7,8]. Evidence of improved survival with this approach has been supported by results from large cancer databases[9], meta-analyses of non-randomized trials[10,11], Markov decision analysis models[2], and several small randomized controlled trials[3-15] (Table 1).
| Ref. | Setting | Neoadjuvant type | Neoadjuvant therapy | Upfront surgery | Comments | ||
| Sample size | Overall survival | Sample size | Overall survival | ||||
| Population-based analyses | |||||||
| Mokdad et al[9], 2016 | NCDB | Mixed | 2005 | 26 mo | 6015 | 21 mo | NT: ↓LN, ↓R1/R2 margins |
| Retrospective institutional analyses | |||||||
| Michelakos et al[46], 2019 | United States | Chemo | 110 | 38 mo | 155 | 21 mo | |
| Sugimoto et al[47], 2019 | United States | Mixed | 911 | 23 mo1 | 911 | 19 mo1 | Resected patients: 29 mo vs 21 mo |
| Meta-analyses of retrospective studies | |||||||
| Versteijne et al[10], 2018 | N/A | Mixed | 17381 | 19 mo1 | 17461 | 15 mo1 | NT: ↓resected rate, ↑R0 rate, ↓LN |
| Prospective randomized trials | |||||||
| Casadei et al[44], 2015 | Italy | CRT | 181 | 22 mo1 | 201 | 19 mo1 | Did not complete accrual |
| Golcher et al[43], 2015 | Germany | CRT | 331 | 17 mo1 | 331 | 14 mo1 | Did not complete accrual |
| Jang et al[14], 2018 | South Korea | CRT | 271 | 21 mo1 | 231 | 12 mo1 | Terminated early (improved survival in NT group) |
| Van Tienhoven et al[13], 2018 | Netherlands | CRT | 1191 | 17 mo1 | 1271 | 13 mo1 | Presented in abstract only |
| Resected patients: 30 mo vs 17 mo | |||||||
| Unno et al[15], 2019 | Japan | Chemo | 1821 | 37 mo1 | 180 | 27 mo1 | Presented in abstract only |
Current guidelines state that either immediate surgical resection or NT followed by surgical resection can be considered[6] but utilization of NT for PDAC in the United States remains low despite the theoretical and empiric advantages of NT[7,18]. This is in stark contrast to the routine use of NT in other cancers to improve overall survival[9], margin-negative resection rates[20], local recurrence[21], or to facilitate less invasive surgery[22]. The reasons for this discrepancy are unclear but we hypothesize, in part, that it is related to a lack of patient-centered research on the use of NT for PDAC. In this article, we describe specific evidence gaps in patient-centered research that should be addressed and the significance these findings could have on improving the outcomes of patients with PDAC.
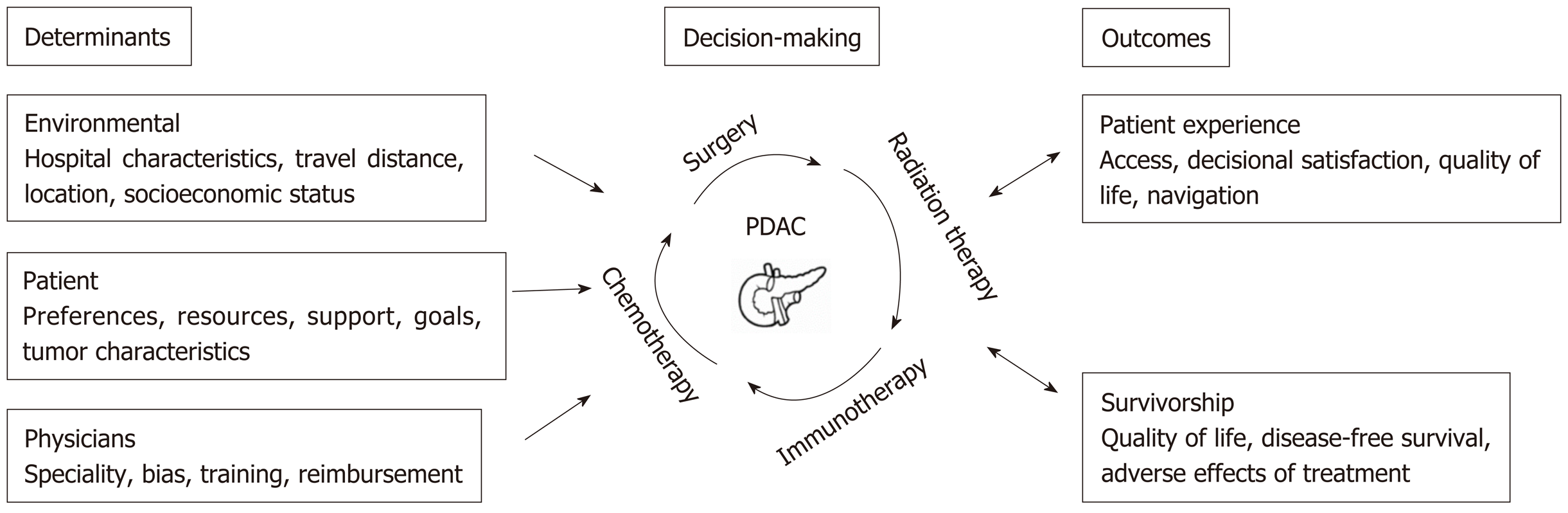
Scant research is available on how decisions are made with regards to treatment sequencing for PDAC. The relative importance of institutional-, patient-, and physician-related factors to decision making is unknown. A novel conceptual model (Figure 1) can define the probable determinants and outcomes of treatment sequence decision making for PDAC. Since the optimal treatment sequencing for PDAC has not been established, decisions are typically made on an individual basis. Decision making may be influenced not only by patient demographic or tumor-related factors and physician preferences, but also patient perceptions, preferences, values, or expectations. The sequencing of treatment for PDAC directly impacts, and conversely is impacted by, the patient experience and survivorship.
Previous research on NT for PDAC has focused on its safety[23] efficacy[7], and cost-effectiveness[24]; missing from prior studies has been an evaluation of patient preferences regarding its use. Cancer-related treatment decisions are complex and require consideration of multiple competing factors such as efficacy, toxicity, costs, and psychosocial well-being, each of which may be valued differently by patients. Such preference sensitive decisions are often made in the context of shared decision making (SDM), a model in which informed and engaged patients make health-care decisions in conjunction with their providers[25]. The degree to which patients are involved in the SDM process of choosing NT or immediate surgery is unclear. Moreover, whether patients have strong preferences for their cancer treatment sequencing is unknown. However, most patients with cancer desire an active role in making decisions about their care[26] and such patient-centered decision making has been shown to improve patients’ understanding of their treatment options, satisfaction with their health care, and overall quality of life (QOL)[27-29].
Previous research in breast and rectal cancer suggest patient-centered approaches to SDM regarding NT are lacking in clinical practice[30-32]. Indeed, SDM is under-utilized by surgeons in general[33]. Other qualitative research among patients with PDAC has highlighted that patient expectations often differ from that of their health-care providers and that SDM is infrequently used[34]. Eliciting and understanding patient opinions, values, and preferences regarding NT will help facilitate SDM which will not only improve patient-centered care but also may increase NT utilization.
Little research has been conducted on patient opinions regarding neoadjuvant approaches to solid tumor malignancies or their preferences towards treatment sequencing. In practice, multiple barriers to the receipt of NT are often expressed by patients. Some patients may have financial concerns secondary to missing work by “delaying” surgery. Others worry about arranging and/or affording transportation for NT due to long travel distances. Frequently, patients state their desire to “just get the cancer out” even if this emotional response does not align with one’s values and priorities (e.g., maximizing survival, avoiding unnecessary treatment, not becoming a burden on caregivers).
While clinical trials have traditionally focused on efficacy, the importance of patient-reported outcomes (PRO) is increasingly recognized[35,36]. Still, little research has been performed on PROs in PDAC despite its relative importance given the short survival durations experienced by most patients. Recently, an international collaboration of both health care providers and patients identified 8 key PROs for PDAC utilizing a Delphi method[37]. Interestingly, the authors found similarity in the core PROs identified among patients treated with curative- and palliative-intent. Whether patients who are receiving NT prioritize the same PROs, due to uncertainty about the prospects of curative surgery, symptoms of the primary tumor, or effects of treatment, is unknown. Interestingly, a recent randomized controlled trial of patients with advanced ovarian cancer actually found improved QOL among patients who received NT compared to those who underwent immediate surgery followed by adjuvant chemotherapy[38].
Equally important, and even less well studied, is the experience of patients undergoing NT for PDAC. The neoadjuvant period is particularly complex and potentially distressing to patients given the need for numerous tests, consultations, and care from multiple providers. Patient assessment of the coordination and communication among their care providers during this time is also unknown. Furthermore, patient perception of provider attentiveness to their physical and psychosocial symptoms as well as their awareness of resources to address them has not been studied. As patient experience is a key domain of health care delivery, further research in this area is needed.
While interest in NT for PDAC has increased considerably over the past decade, significant gaps exist in patient-centered outcomes research. Therefore, resources and efforts should be directed towards addressing unanswered questions in several domains: Patient preferences, SDM, the patient experience, PROs, and survivorship, among others (Table 2).
| Patient preferences |
| What are patient perceptions and opinions regarding NT? |
| What are the barriers and facilitators to NT? |
| What sources of information inform decision making for NT? |
| The patient experience |
| How does shared decision making occur regarding NT? |
| How do patients perceive communication, coordination, and the health care experience during NT? |
| What resources are needed by patients undergoing NT? |
| Patient-reported outcomes (PROs) |
| Are PROs for pancreatic cancer similar or unique during NT? |
| How is patient quality of life affected by NT? |
| Survivorship |
| Does receipt of NT influence survivorship during and following treatment? |
| Do patients experience decisional regret/satisfaction? |
Changing decision-making paradigms in PDAC could have profound significance. First, an understanding of patient opinions and preferences may help explain why utilization rates of NT are especially low. Indeed, a clearer understanding of the relevant barriers and facilitators to the use of NT may identify opportunities to increase its utilization. Since completion of multimodality therapy is one of the strongest determinants of long-term survival, increasing utilization of NT represents an immediate opportunity to improve the outcomes of patients with PDAC while novel systemic therapies are being developed. Furthermore, participation in clinical trials is low. While multiple trials are currently under investigation[39-42], at least two prior randomized controlled trials evaluating NT were closed early, primarily due to low accrual[43,44]. Second, a better understanding of patient preferences and priorities will improve the SDM process when making decisions about NT or immediate surgery. Such information could enable the creation of educational tools or decision aids. Similar decision aids have been shown to be helpful in the decision making process regarding NT for breast cancer[45]. Finally, an enhanced focus on the patient experience, PROs, and survivorship should improve patient QOL both during and following treatment.
PDAC is an aggressive malignancy with a high rate of recurrence even among patients who undergo curative-intent surgery. While NT is a novel and increasingly utilized approach to treatment, patient-centered research, particularly within the domains of patient preferences, patient experience, PROs, and survivorship, are lacking. Studies that address these evidence gaps are expected to improve the delivery of patient-centered care and ultimately outcomes of patients with PDAC.
Manuscript source: Invited Manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gabriel S, Ridola L S-Editor: Gong ZM L-Editor: A E-Editor: Zhang YL
| 1. | Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68:7-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11573] [Cited by in RCA: 13167] [Article Influence: 1881.0] [Reference Citation Analysis (4)] |
| 2. | Neoptolemos JP, Stocken DD, Friess H, Bassi C, Dunn JA, Hickey H, Beger H, Fernandez-Cruz L, Dervenis C, Lacaine F, Falconi M, Pederzoli P, Pap A, Spooner D, Kerr DJ, Büchler MW; European Study Group for Pancreatic Cancer. A randomized trial of chemoradiotherapy and chemotherapy after resection of pancreatic cancer. N Engl J Med. 2004;350:1200-1210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1945] [Cited by in RCA: 1909] [Article Influence: 90.9] [Reference Citation Analysis (0)] |
| 3. | Oettle H, Post S, Neuhaus P, Gellert K, Langrehr J, Ridwelski K, Schramm H, Fahlke J, Zuelke C, Burkart C, Gutberlet K, Kettner E, Schmalenberg H, Weigang-Koehler K, Bechstein WO, Niedergethmann M, Schmidt-Wolf I, Roll L, Doerken B, Riess H. Adjuvant chemotherapy with gemcitabine vs observation in patients undergoing curative-intent resection of pancreatic cancer: a randomized controlled trial. JAMA. 2007;297:267-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1779] [Cited by in RCA: 1764] [Article Influence: 98.0] [Reference Citation Analysis (0)] |
| 4. | Conroy T, Hammel P, Hebbar M, Ben Abdelghani M, Wei AC, Raoul JL, Choné L, Francois E, Artru P, Biagi JJ, Lecomte T, Assenat E, Faroux R, Ychou M, Volet J, Sauvanet A, Breysacher G, Di Fiore F, Cripps C, Kavan P, Texereau P, Bouhier-Leporrier K, Khemissa-Akouz F, Legoux JL, Juzyna B, Gourgou S, O'Callaghan CJ, Jouffroy-Zeller C, Rat P, Malka D, Castan F, Bachet JB; Canadian Cancer Trials Group and the Unicancer-GI–PRODIGE Group. FOLFIRINOX or Gemcitabine as Adjuvant Therapy for Pancreatic Cancer. N Engl J Med. 2018;379:2395-2406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1427] [Cited by in RCA: 1945] [Article Influence: 277.9] [Reference Citation Analysis (0)] |
| 5. | Bilimoria KY, Bentrem DJ, Ko CY, Tomlinson JS, Stewart AK, Winchester DP, Talamonti MS. Multimodality therapy for pancreatic cancer in the U.S. : utilization, outcomes, and the effect of hospital volume. Cancer. 2007;110:1227-1234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 182] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 6. | Altman AM, Wirth K, Marmor S, Lou E, Chang K, Hui JYC, Tuttle TM, Jensen EH, Denbo JW. Completion of Adjuvant Chemotherapy After Upfront Surgical Resection for Pancreatic Cancer Is Uncommon Yet Associated With Improved Survival. Ann Surg Oncol. 2019;26:4108-4116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 91] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 7. | Cloyd JM, Katz MH, Prakash L, Varadhachary GR, Wolff RA, Shroff RT, Javle M, Fogelman D, Overman M, Crane CH, Koay EJ, Das P, Krishnan S, Minsky BD, Lee JH, Bhutani MS, Weston B, Ross W, Bhosale P, Tamm EP, Wang H, Maitra A, Kim MP, Aloia TA, Vauthey JN, Fleming JB, Abbruzzese JL, Pisters PW, Evans DB, Lee JE. Preoperative Therapy and Pancreatoduodenectomy for Pancreatic Ductal Adenocarcinoma: a 25-Year Single-Institution Experience. J Gastrointest Surg. 2017;21:164-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 113] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 8. | Cloyd JM, Wang H, Egger ME, Tzeng CD, Prakash LR, Maitra A, Varadhachary GR, Shroff R, Javle M, Fogelman D, Wolff RA, Overman MJ, Koay EJ, Das P, Herman JM, Kim MP, Vauthey JN, Aloia TA, Fleming JB, Lee JE, Katz MHG. Association of Clinical Factors With a Major Pathologic Response Following Preoperative Therapy for Pancreatic Ductal Adenocarcinoma. JAMA Surg. 2017;152:1048-1056. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 93] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 9. | Mokdad AA, Minter RM, Zhu H, Augustine MM, Porembka MR, Wang SC, Yopp AC, Mansour JC, Choti MA, Polanco PM. Neoadjuvant Therapy Followed by Resection Versus Upfront Resection for Resectable Pancreatic Cancer: A Propensity Score Matched Analysis. J Clin Oncol. 2017;35:515-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 307] [Article Influence: 34.1] [Reference Citation Analysis (0)] |
| 10. | Versteijne E, Vogel JA, Besselink MG, Busch ORC, Wilmink JW, Daams JG, van Eijck CHJ, Groot Koerkamp B, Rasch CRN, van Tienhoven G; Dutch Pancreatic Cancer Group. Meta-analysis comparing upfront surgery with neoadjuvant treatment in patients with resectable or borderline resectable pancreatic cancer. Br J Surg. 2018;105:946-958. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 251] [Cited by in RCA: 389] [Article Influence: 55.6] [Reference Citation Analysis (1)] |
| 11. | Unno M, Hata T, Motoi F. Long-term outcome following neoadjuvant therapy for resectable and borderline resectable pancreatic cancer compared to upfront surgery: a meta-analysis of comparative studies by intention-to-treat analysis. Surg Today. 2019;49:295-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 12. | de Geus SW, Evans DB, Bliss LA, Eskander MF, Smith JK, Wolff RA, Miksad RA, Weinstein MC, Tseng JF. Neoadjuvant therapy versus upfront surgical strategies in resectable pancreatic cancer: A Markov decision analysis. Eur J Surg Oncol. 2016;42:1552-1560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 43] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 13. | Van Tienhoven G, Versteijne E, Suker M, Groothuis KBC, Busch OR, Bonsing BA, de Hingh IHJT, Festen S, Patijn GA, de Vos-Geelen J, Zwinderman AH, Punt CJA, van Eijck CH. Preoperative chemoradiotherapy versus immediate surgery for resectable and borderline resectable pancreatic cancer (PREOPANC-1): A randomized, controlled, multicenter phase III trial. J Clin Oncol. 2018;36:LBA4002. [RCA] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 108] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 14. | Jang JY, Han Y, Lee H, Kim SW, Kwon W, Lee KH, Oh DY, Chie EK, Lee JM, Heo JS, Park JO, Lim DH, Kim SH, Park SJ, Lee WJ, Koh YH, Park JS, Yoon DS, Lee IJ, Choi SH. Oncological Benefits of Neoadjuvant Chemoradiation With Gemcitabine Versus Upfront Surgery in Patients With Borderline Resectable Pancreatic Cancer: A Prospective, Randomized, Open-label, Multicenter Phase 2/3 Trial. Ann Surg. 2018;268:215-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 310] [Cited by in RCA: 511] [Article Influence: 73.0] [Reference Citation Analysis (0)] |
| 15. | Unno M, Motoi F, Matsuyama Y, Satoi S, Matsumoto I, Aosasa S, Shirakawa H, Wada K, Fujii T, Yoshitomi H, Takahashi S, Sho M, Ueno H, Kosuge T. Randomized phase II/III trial of neoadjuvant chemotherapy with gemcitabine and S-1 versus upfront surgery for resectable pancreatic cancer (Prep-02/JSAP-05). J Clin Oncol. 2019;37:189-189. [RCA] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 130] [Article Influence: 21.7] [Reference Citation Analysis (0)] |
| 16. | Khorana AA, Mangu PB, Berlin J, Engebretson A, Hong TS, Maitra A, Mohile SG, Mumber M, Schulick R, Shapiro M, Urba S, Zeh HJ, Katz MH. Potentially Curable Pancreatic Cancer: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol. 2016;34:2541-2556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 238] [Cited by in RCA: 283] [Article Influence: 31.4] [Reference Citation Analysis (0)] |
| 17. | Youngwirth LM, Nussbaum DP, Thomas S, Adam MA, Blazer DG, Roman SA, Sosa JA. Nationwide trends and outcomes associated with neoadjuvant therapy in pancreatic cancer: An analysis of 18 243 patients. J Surg Oncol. 2017;116:127-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 71] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 18. | Hashmi A, Kozick Z, Fluck M, Hunsinger MA, Wild J, Arora TK, Shabahang MM, Blansfield JA. Neoadjuvant versus Adjuvant Chemotherapy for Resectable Pancreatic Adenocarcinoma: A National Cancer Database Analysis. Am Surg. 2018;84:1439-1445. [PubMed] |
| 19. | Cunningham D, Allum WH, Stenning SP, Thompson JN, Van de Velde CJ, Nicolson M, Scarffe JH, Lofts FJ, Falk SJ, Iveson TJ, Smith DB, Langley RE, Verma M, Weeden S, Chua YJ, MAGIC Trial Participants. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006;355:11-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4899] [Cited by in RCA: 4609] [Article Influence: 242.6] [Reference Citation Analysis (0)] |
| 20. | van Hagen P, Hulshof MC, van Lanschot JJ, Steyerberg EW, van Berge Henegouwen MI, Wijnhoven BP, Richel DJ, Nieuwenhuijzen GA, Hospers GA, Bonenkamp JJ, Cuesta MA, Blaisse RJ, Busch OR, ten Kate FJ, Creemers GJ, Punt CJ, Plukker JT, Verheul HM, Spillenaar Bilgen EJ, van Dekken H, van der Sangen MJ, Rozema T, Biermann K, Beukema JC, Piet AH, van Rij CM, Reinders JG, Tilanus HW, van der Gaast A; CROSS Group. Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med. 2012;366:2074-2084. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3288] [Cited by in RCA: 4080] [Article Influence: 313.8] [Reference Citation Analysis (0)] |
| 21. | Kapiteijn E, Marijnen CA, Nagtegaal ID, Putter H, Steup WH, Wiggers T, Rutten HJ, Pahlman L, Glimelius B, van Krieken JH, Leer JW, van de Velde CJ; Dutch Colorectal Cancer Group. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med. 2001;345:638-646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3104] [Cited by in RCA: 3120] [Article Influence: 130.0] [Reference Citation Analysis (0)] |
| 22. | van der Hage JA, van de Velde CJ, Julien JP, Tubiana-Hulin M, Vandervelden C, Duchateau L. Preoperative chemotherapy in primary operable breast cancer: results from the European Organization for Research and Treatment of Cancer trial 10902. J Clin Oncol. 2001;19:4224-4237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 803] [Cited by in RCA: 774] [Article Influence: 32.3] [Reference Citation Analysis (0)] |
| 23. | Verma V, Li J, Lin C. Neoadjuvant Therapy for Pancreatic Cancer: Systematic Review of Postoperative Morbidity, Mortality, and Complications. Am J Clin Oncol. 2016;39:302-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 80] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 24. | Abbott DE, Tzeng CW, Merkow RP, Cantor SB, Chang GJ, Katz MH, Bentrem DJ, Bilimoria KY, Crane CH, Varadhachary GR, Abbruzzese JL, Wolff RA, Lee JE, Evans DB, Fleming JB. The cost-effectiveness of neoadjuvant chemoradiation is superior to a surgery-first approach in the treatment of pancreatic head adenocarcinoma. Ann Surg Oncol. 2013;20 Suppl 3:S500-S508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 56] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 25. | Légaré F, Witteman HO. Shared decision making: examining key elements and barriers to adoption into routine clinical practice. Health Aff (Millwood). 2013;32:276-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 449] [Cited by in RCA: 552] [Article Influence: 46.0] [Reference Citation Analysis (0)] |
| 26. | Tariman JD, Berry DL, Cochrane B, Doorenbos A, Schepp K. Preferred and actual participation roles during health care decision making in persons with cancer: a systematic review. Ann Oncol. 2010;21:1145-1151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 210] [Cited by in RCA: 243] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 27. | Hack TF, Degner LF, Watson P, Sinha L. Do patients benefit from participating in medical decision making? Longitudinal follow-up of women with breast cancer. Psychooncology. 2006;15:9-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 265] [Cited by in RCA: 282] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 28. | Gattellari M, Butow PN, Tattersall MH. Sharing decisions in cancer care. Soc Sci Med. 2001;52:1865-1878. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 369] [Cited by in RCA: 365] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 29. | Kehl KL, Landrum MB, Arora NK, Ganz PA, van Ryn M, Mack JW, Keating NL. Association of Actual and Preferred Decision Roles With Patient-Reported Quality of Care: Shared Decision Making in Cancer Care. JAMA Oncol. 2015;1:50-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 173] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 30. | Herrmann A, Hall A, Zdenkowski N. Women's Experiences with Deciding on Neoadjuvant Systemic Therapy for Operable Breast Cancer: A Qualitative Study. Asia-Pac J Oncol Nurs. 2018;5:68-76. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 31. | Kunneman M, Engelhardt EG, Ten Hove FL, Marijnen CA, Portielje JE, Smets EM, de Haes HJ, Stiggelbout AM, Pieterse AH. Deciding about (neo-)adjuvant rectal and breast cancer treatment: Missed opportunities for shared decision making. Acta Oncol. 2016;55:134-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 70] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 32. | de Ligt KM, Spronk PER, van Bommel ACM, Vrancken Peeters MTFD, Siesling S, Smorenburg CH; Nabon Breast Cancer Audit group. Patients' experiences with decisions on timing of chemotherapy for breast cancer. Breast. 2018;37:99-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 33. | de Mik SML, Stubenrouch FE, Balm R, Ubbink DT. Systematic review of shared decision-making in surgery. Br J Surg. 2018;105:1721-1730. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 118] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 34. | Ziebland S, Chapple A, Evans J. Barriers to shared decisions in the most serious of cancers: a qualitative study of patients with pancreatic cancer treated in the UK. Health Expect. 2015;18:3302-3312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 38] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 35. | Kotronoulas G, Kearney N, Maguire R, Harrow A, Di Domenico D, Croy S, MacGillivray S. What is the value of the routine use of patient-reported outcome measures toward improvement of patient outcomes, processes of care, and health service outcomes in cancer care? A systematic review of controlled trials. J Clin Oncol. 2014;32:1480-1501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 789] [Cited by in RCA: 715] [Article Influence: 65.0] [Reference Citation Analysis (0)] |
| 36. | Porter ME, Larsson S, Lee TH. Standardizing Patient Outcomes Measurement. N Engl J Med. 2016;374:504-506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 408] [Cited by in RCA: 456] [Article Influence: 50.7] [Reference Citation Analysis (0)] |
| 37. | van Rijssen LB, Gerritsen A, Henselmans I, Sprangers MA, Jacobs M, Bassi C, Busch OR, Fernández-Del Castillo C, Fong ZV, He J, Jang JY, Javed AA, Kim SW, Maggino L, Mitra A, Ostwal V, Pellegrini S, Shrikhande SV, Wilmink JW, Wolfgang CL, van Laarhoven HW, Besselink MG; COPRAC study group. Core Set of Patient-reported Outcomes in Pancreatic Cancer (COPRAC): An International Delphi Study Among Patients and Health Care Providers. Ann Surg. 2019;270:158-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 38. | Fagotti A, Ferrandina G, Vizzielli G, Fanfani F, Gallotta V, Chiantera V, Costantini B, Margariti PA, Gueli Alletti S, Cosentino F, Tortorella L, Scambia G. Phase III randomised clinical trial comparing primary surgery versus neoadjuvant chemotherapy in advanced epithelial ovarian cancer with high tumour load (SCORPION trial): Final analysis of peri-operative outcome. Eur J Cancer. 2016;59:22-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 288] [Article Influence: 32.0] [Reference Citation Analysis (0)] |
| 39. | Motoi F, Ishida K, Fujishima F, Ottomo S, Oikawa M, Okada T, Shimamura H, Takemura S, Ono F, Akada M, Nakagawa K, Katayose Y, Egawa S, Unno M. Neoadjuvant chemotherapy with gemcitabine and S-1 for resectable and borderline pancreatic ductal adenocarcinoma: results from a prospective multi-institutional phase 2 trial. Ann Surg Oncol. 2013;20:3794-3801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 105] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 40. | Tachezy M, Gebauer F, Petersen C, Arnold D, Trepel M, Wegscheider K, Schafhausen P, Bockhorn M, Izbicki JR, Yekebas E. Sequential neoadjuvant chemoradiotherapy (CRT) followed by curative surgery vs. primary surgery alone for resectable, non-metastasized pancreatic adenocarcinoma: NEOPA- a randomized multicenter phase III study (NCT01900327, DRKS00003893, ISRCTN82191749). BMC Cancer. 2014;14:411. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 63] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 41. | Ettrich TJ, Berger AW, Perkhofer L, Daum S, König A, Dickhut A, Wittel U, Wille K, Geissler M, Algül H, Gallmeier E, Atzpodien J, Kornmann M, Muche R, Prasnikar N, Tannapfel A, Reinacher-Schick A, Uhl W, Seufferlein T. Neoadjuvant plus adjuvant or only adjuvant nab-paclitaxel plus gemcitabine for resectable pancreatic cancer - the NEONAX trial (AIO-PAK-0313), a prospective, randomized, controlled, phase II study of the AIO pancreatic cancer group. BMC Cancer. 2018;18:1298. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 56] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 42. | Labori KJ, Lassen K, Hoem D, Grønbech JE, Søreide JA, Mortensen K, Smaaland R, Sorbye H, Verbeke C, Dueland S. Neoadjuvant chemotherapy versus surgery first for resectable pancreatic cancer (Norwegian Pancreatic Cancer Trial - 1 (NorPACT-1)) - study protocol for a national multicentre randomized controlled trial. BMC Surg. 2017;17:94. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 82] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 43. | Golcher H, Brunner TB, Witzigmann H, Marti L, Bechstein WO, Bruns C, Jungnickel H, Schreiber S, Grabenbauer GG, Meyer T, Merkel S, Fietkau R, Hohenberger W. Neoadjuvant chemoradiation therapy with gemcitabine/cisplatin and surgery versus immediate surgery in resectable pancreatic cancer: results of the first prospective randomized phase II trial. Strahlenther Onkol. 2015;191:7-16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 197] [Cited by in RCA: 238] [Article Influence: 21.6] [Reference Citation Analysis (0)] |
| 44. | Casadei R, Di Marco M, Ricci C, Santini D, Serra C, Calculli L, D'Ambra M, Guido A, Morselli-Labate AM, Minni F. Neoadjuvant Chemoradiotherapy and Surgery Versus Surgery Alone in Resectable Pancreatic Cancer: A Single-Center Prospective, Randomized, Controlled Trial Which Failed to Achieve Accrual Targets. J Gastrointest Surg. 2015;19:1802-1812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 161] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 45. | Herrmann A, Boyle F, Butow P, Hall AE, Zdenkowski N. Exploring women's experiences with a decision aid for neoadjuvant systemic therapy for operable breast cancer. Health Sci Rep. 2018;1:e13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 46. | Michelakos T, Pergolini I, Castillo CF, Honselmann KC, Cai L, Deshpande V, Wo JY, Ryan DP, Allen JN, Blaszkowsky LS, Clark JW, Murphy JE, Nipp RD, Parikh A, Qadan M, Warshaw AL, Hong TS, Lillemoe KD, Ferrone CR. Predictors of Resectability and Survival in Patients With Borderline and Locally Advanced Pancreatic Cancer who Underwent Neoadjuvant Treatment With FOLFIRINOX. Ann Surg. 2019;269:733-740. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 242] [Article Influence: 48.4] [Reference Citation Analysis (0)] |
| 47. | Sugimoto M, Takahashi N, Farnell MB, Smyrk TC, Truty MJ, Nagorney DM, Smoot RL, Chari ST, Carter RE, Kendrick ML. Survival benefit of neoadjuvant therapy in patients with non-metastatic pancreatic ductal adenocarcinoma: A propensity matching and intention-to-treat analysis. J Surg Oncol. 2019;120:976-984. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |