Published online Oct 14, 2020. doi: 10.3748/wjg.v26.i38.5749
Peer-review started: April 28, 2020
First decision: May 15, 2020
Revised: May 27, 2020
Accepted: September 8, 2020
Article in press: September 8, 2020
Published online: October 14, 2020
Processing time: 168 Days and 17.1 Hours
Since the outbreak of the coronavirus disease 2019 (COVID-19), various measures have been taken to protect against the infection. As droplet and contact transmission are the main routes of COVID-19 infection, endoscopy centers are considered to be high-risk areas for exposure to COVID-19. We have undertaken several countermeasures in our endoscopic center during the pandemic, and have gained significant experience in terms of prevention and control of COVID-19. We here present our experience and strategies adopted for preventing hospital infection in our endoscopy center during the COVID-19 pandemic. We describe our management of the environment, endoscope, patients, and medical staff, and our self-made masks.
Core Tip: This opinion review presents our experience and strategies adopted for preventing hospital infection in an endoscopy center located in Western China during the coronavirus disease 2019 (COVID-19) pandemic. We describe our three-level screening strategy and an innovative self-made gastroscope isolated mask. We provide valuable information for China and other countries suffering from the COVID-19 pandemic.
- Citation: Gao Y, Ye LS, Du J, Zhang QY, Hu B. Management of an endoscopy center during the outbreak of COVID-19: Experience from West China Hospital. World J Gastroenterol 2020; 26(38): 5749-5758
- URL: https://www.wjgnet.com/1007-9327/full/v26/i38/5749.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i38.5749
Since the outbreak of coronavirus disease 2019 (COVID-19) in December 2019, China and many other countries have tried several measures to protect against the spread of infection[1-3]. Although the COVID-19 pandemic in China has been mostly under control[4,5], the number of infected people in European and American countries is noticeably increasing[5,6]. Due to the main routes of droplet and contact transmission[7], endoscopy centers have a high risk of exposure to COVID-19. As the most prestigious endoscopy center in western China, a total of 7135 diagnostic endoscopies and 643 therapeutic endoscopies were performed in West China Hospital from March 1 to April 10, 2020, which included 124 cases of endoscopic retrograde cholangiopan-creatography, 55 of endoscopic submucosal dissection, 207 of endoscopic mucosal resection, and 224 of endoscopic ultrasound. Compared with the same period last year, we reasonably arranged the endoscopy schedule and minimized unnecessary endoscopy (Table 1). There were no hospital infections in medical staff and patients. In the current review, we present our experience and strategies adopted for preventing hospital infection in our endoscopy center during the COVID-19 pandemic.
| March 1, 2019 –April 10, 2019 | March 1, 2020-April 10, 2020 | |
| Routine gastroscopy | 1414 | 616 |
| Routine colonoscopy | 903 | 438 |
| Painless gastroscopy | 4709 | 3325 |
| Painless colonoscopy | 3312 | 2462 |
| Enteroscopy | 24 | 30 |
| Capsule gastroscopy | 57 | 40 |
| EUS | 309 | 224 |
| Diagnostic endoscopy | 10728 | 7135 |
| Removal of foreign body in UGI tract | 109 | 70 |
| Hemostasis of varicose veins | 111 | 77 |
| Hemostasis of non-varicose veins | 25 | 19 |
| Stent placement in UGI tract | 1 | 4 |
| Stent placement in LGI tract | 2 | 6 |
| Esophageal EMR | 1 | 0 |
| Gastric EMR | 161 | 30 |
| Colorectal EMR | 569 | 177 |
| Esophageal ESD | 24 | 23 |
| Gastric ESD | 41 | 23 |
| Colorectal ESD | 14 | 9 |
| POEM | 5 | 0 |
| ERCP | 168 | 124 |
| EUS-FNA | 21 | 25 |
| EUS + stent drainage | 0 | 1 |
| STER | 8 | 7 |
| ESTD | 35 | 48 |
| Therapeutic endoscopy | 1295 | 643 |
Endoscopy centers generally have no rooms with negative-pressure laminar flow. Virus transmission might occur because patients undergoing upper gastrointestinal endoscopy cannot wear a mask, and fecal fluid might flow during lower gastrointestinal endoscopy[8]. Thus, disinfection of the environment and endoscopes is important.
Disinfection of the environment: In our center, 500 ppm chlorine-containing disinfectant was applied 1 or 2 times/d for disinfecting the surface of equipment and the ground. Doorknobs and chairs were wiped and disinfected with 1000 ppm chlorine-containing disinfectant for 2 or 3 times/d. Secretions were removed immediately, and the areas wiped with 2000 ppm chlorine-containing disinfectant. Natural ventilation was performed continuously.
Disinfection of the operation room: Here, 1000–2000 ppm chlorine-containing disinfectant was applied at least 2 times/d for ground disinfection. Disinfection with 75% alcohol was used for consoles and monitors. Electrosurgical workstations and treatment beds were wiped with 75% alcohol before and after each procedure. Disposable bedspread and pillowcases were used for each patient. An automatic air disinfection machine was applied in the operating room twice daily (05:00–7:00 and 19:00–21:00 h). Continuous ventilation was conducted using a fresh air ventilation system during working hours.
Disinfection of the resuscitation room: Surfaces of monitors and other instruments were wiped with 75% alcohol for disinfection. Additionally, sofas were wiped and disinfected with 1000–2000 ppm chlorine-containing disinfectant for 1 or 2 times/d. Floors were mopped with 1000–2000 ppm chlorine-containing disinfectant for 1 or 2 times/d. An automatic air disinfection machine was used for air disinfection in the operation room twice daily (05:00–7:00 and 19:00–21:00 h). Continuous ventilation was performed using a fresh air ventilation system during working hours.
Disinfection of the office area: The doorknobs in office areas were wiped and disinfected with 75% alcohol for 2–4 times/d. The desktops, chairs and cabinet surfaces were wiped and disinfected with 1000 ppm chlorine-containing disinfectant. The floor was mopped and disinfected with 1000 ppm chlorine-containing disinfectant. Continuous ventilation was carried out using a fresh air ventilation system during working hours.
Disinfection of the endoscopes: After preprocessing, the endoscope was immersed into a container with 0.2%–0.35% peracetic acid for predisinfection. Instruments should also be predisinfected using the solution with 0.2%–0.35% peracetic acid solution. Then, the endoscope was placed in a special container, sealed, and transferred to a clean and disinfected room. Standard cleaning and disinfection procedures were carried out after 10 min. Finally, total ethanol perfusion with 75% alcohol and full sterilization with 0.2%–0.35% peracetic acid were done before the application of endoscope to the next patient.
After daily cleaning and disinfection, the cleaning tank, rinsing tank, perfusion device, and cleaning brush were thoroughly cleaned and disinfected with 0.2%–0.35% peracetic acid.
Three special channels with eye-catching signs were set up, for entrance and exit of medical staff as well as patients. Dedicated staff were appointed for managing these channels and recording related information.
Entrance and exit channels for medical staff: Measurement of medical staff’s body temperature was undertaken before their entrance into a specific channel. In our center, staff without fever (< 37.3ºC) were allowed to enter the endoscopy center, and protective equipment, such as disposable mask, hat, and surgical gown were provided. The body temperature of the staff was measured again when they left work.
Entrance channel for patients: Patients who underwent secondary screening (see below) were allowed to enter our endoscopy center. Family members had no access to the endoscopy center. Entrance was permitted for one family member only if the patient was in serious condition.
Exit channel for patients: Patients who received endoscopic intervention had to leave the endoscopy center through an exit channel. Patients’ entrance was prohibited as well.
Appointment scheduling for patients: Personal mobility and gathering might increase the risk of coronavirus transmission. Diagnostic appointment scheduling for asymptomatic patients without warning signs (e.g., unexplained weight loss), and therapeutic plans for patients with mild illness (e.g., small colorectal polyps) should be delayed. The appointment should be arranged according to the potential severity of illness. Priority should be given to patients who are old, frail, children, have a history of taking immunosuppressants, have diabetes, or to other immunocompromised patients. In our center, all patients were informed about the risk of virus infection, if they would like to receive endoscopy during the outbreak.
Patient survey and preparation prior to endoscopy: Dedicated staff contacted patients via telephone within 2 wk before their scheduled appointment, and inquired about the presence of the following symptoms and epidemiological history. Symptoms mainly included new-onset fever, cough, loss of appetite, and diarrhea. Epidemiological histories included residency in high-risk areas within 2 wk, and history of contact with COVID-19 patients and suspected cases within 2 wk. Patients with any of these symptoms and epidemiological history were referred to the fever clinic, and endoscopy was performed only after ruling out COVID-19 infection. More than 30 patients reported fever during telephone consultation, and they were ruled out for COVID-19 infection before undergoing endoscopy. Patients without these suspicious symptoms or epidemiological history also have to undergo chest computed tomography (CT) 3–5 d prior to endoscopy. Study showed that chest CT had a low rate of missed diagnosis of COVID-19 (3.9%, 2/51) and thus it can be used as a standard method for diagnosis of COVID-19 based on CT features and transformation rules[9]. Rapid diagnosis can control the potential spread early and optimize patient management. During the outbreak, a male patient with history of contact with people from Hubei Province was confirmed with COVID-19 after undergoing chest CT and following virus detection, although he declared suspicious symptoms during telephone inquiry. Our strategy aimed to prevent the transmission of the virus from such atypical patients.
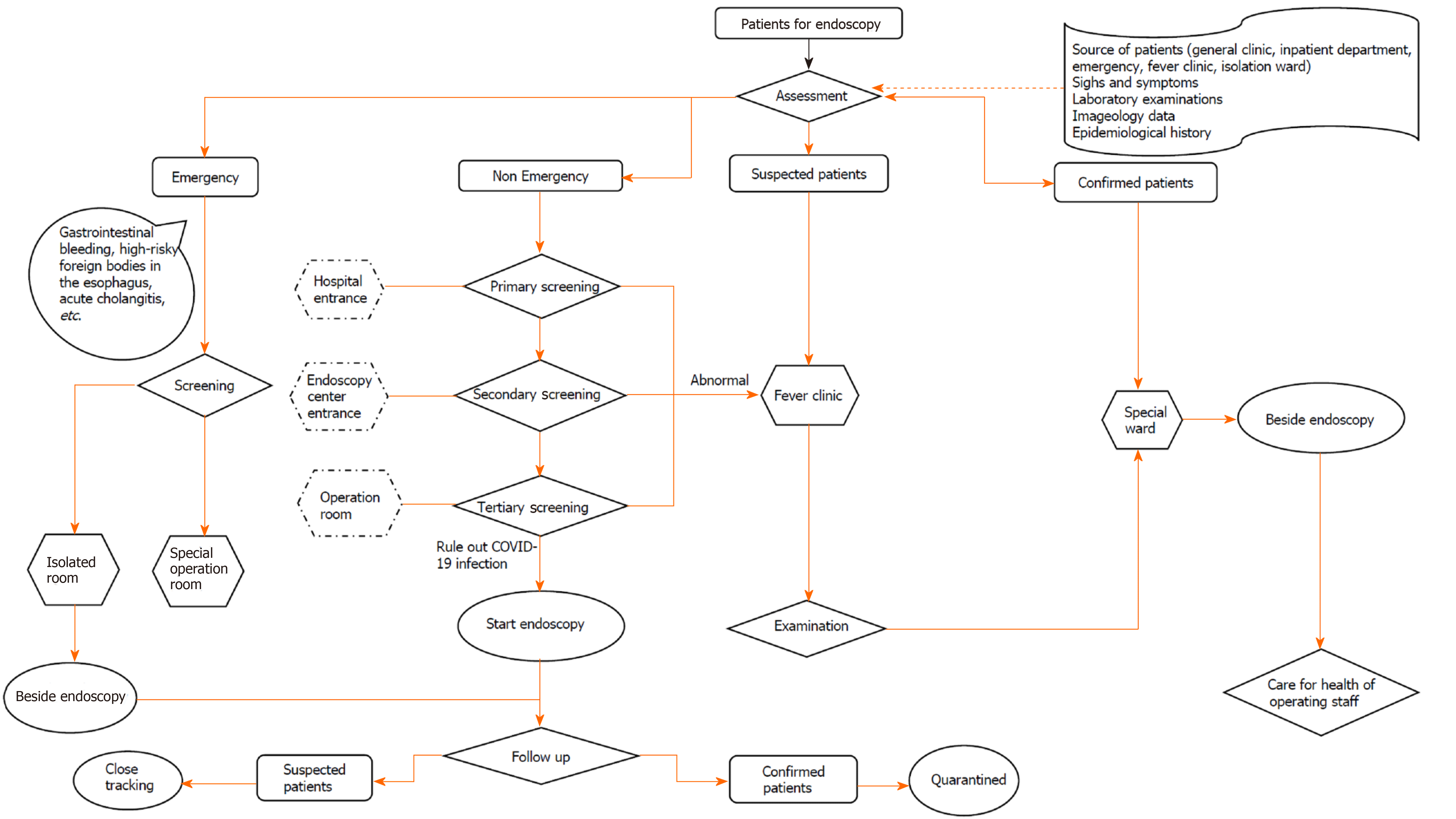
We implemented a three-level screening strategy for patients who received endoscopy during the COVID-19 pandemic (Figure 1).
Primary screening in the gate of the main building: All patients had to wear face masks, and only patients without fever were allowed to enter the building. Dedicated staff rechecked the body temperature and investigated the epidemiological history of patients with fever. These patients were sent to the fever clinic outside the building, and were guided by the staff.
Secondary screening in the gate of endoscopy center: The body temperature, symptoms, epidemiological history, and the results of chest CT of each patient were recorded and checked. Patients without fever and epidemiological history, and with normal chest CT findings within 3–5 d were allowed to enter the endoscopy center for endoscopic operation after disinfection of their hands using alcohol-based hand rubs. With the gradual easing of the pandemic, the time requirement for chest CT can be extended to 2 wk before examination. Suspected patients were sent to the fever clinic for further examination, and guided by staff, while confirmed patients were quarantined in a special isolated ward.
Tertiary screening in the operating room: When patients arrived at the operating room of the endoscopy center, an endoscopist and a nurse rechecked the information recorded by the secondary screening. Suspected patients were sent to the fever clinic, and guided by the staff, while confirmed patients were quarantined in a special isolated ward. The endoscopic operation was then carried out as usual for unsuspected patients.
Posthospital management: Follow-up was conducted when patients left our center. Dedicated staff contacted the patients via telephone and recorded any abnormalities. If a patient was diagnosed with COVID-19 during the follow-up period, all the related medical staff had to stop working, and be quarantined at their respective homes for at least 2 wk. Related patients would be contacted and quarantined as well.
The work plan was adjusted according to the number of appointed patients, and with minimized medical staff on duty. All endoscopists, nurses, and healthcare personnel were trained in terms of infection control, as well as utilizing personal protective equipment properly during endoscopy (Table 2). All staff had to daily report and record their symptoms and epidemiological history. Staff with fever or epidemiological history of exposure were referred to the fever clinic and were quarantined. Four medical staff of our endoscopy center were under home quarantine for 14 d due to confirmed cases in their community.
| Location | Occupational protection | Reserved supply | Environmental management | Screening and treatment | ||||
| No special pollution | Special pollution | Air disinfection | Screening method | No abnormalities | Suspected patients | |||
| Reservation office | Long sleeve overalls; medical surgical mask; disposable medical cap; plastic gloves/nitrile gloves | Infrared temperature measuring gun Thermometer; 75% alcohol. Free hand-washing disinfection | Surface disinfection: 75% alcohol Floor disinfection: 500 mg/L chlorine-containing disinfectant Frequency: 1-2 times/d | Secretion pollution: 2000 mg/L chlorine-containing disinfectant Frequency: immediate | Continuous fresh air exchange | Ask about symptoms and signs and epidemiological history Temperature measurement | Make an appointment | Stop appointment Send to fever clinic of emergency department |
| Reception and guidance area | Long sleeve overalls; medical surgical mask; disposable medical cap; plastic gloves /nitrile gloves | Infrared temperature measuring gun Thermometer; 75% alcohol Free hand-washing disinfection | Surface disinfection: 75% alcohol Floor disinfection: 500 mg/L chlorine-containing disinfectant Frequency: 1-2 times/d | Secretion pollution: 2000 mg/L chlorine-containing disinfectant Frequency: immediate | Continuous fresh air exchange | Ask about symptoms and signs and epidemiological history Temperature measurement Fill in the preliminary screening form | Lead to secondary waiting area | Stop appointment Send to fever clinic of emergency department |
| Secondary waiting area | Long sleeve overalls; medical surgical mask; disposable medical cap; Plastic gloves/nitrile gloves; Patients and families wear masks all the time | Infrared temperature measuring gun Thermometer; 75% alcohol Free hand-washing disinfection | Surface disinfection: 500 mg/L chlorine-containing disinfectant; Floor disinfection: 500 mg/L chlorine-containing disinfectant; Frequency: 1-2 times/d; Doorknob and chairs disinfection: 1000 ppm chlorine-containing disinfectant (2 or 3 times/d) | Secretion pollution: 2000 mg/L chlorine-containing disinfectant; Frequency: Immediate | Continuous fresh air exchange | Check the preliminary screening table, symptoms and signs, and epidemiological historyTake temperature if necessary | Prepare endoscopic diagnosis and treatment | Stop diagnosis and treatment Send to fever clinic of emergency department |
| Examination room | Long sleeve overalls; disposable waterproof isolated clothing; Medical surgical face mask and glasses; Disposable medical cap; latex gloves; special shoes; The assistant is the same as the reservation office | Free hand-washing disinfection (per room) | Surface disinfection: 75% alcohol Floor disinfection: 1000–2000 mg/L chlorine-containing disinfectant Frequency: 2 or 3 times/d | Secretion/blood pollution: 2000 mg/L chlorine-containing disinfectant Frequency: Immediate | Continuous fresh air exchange Automatic air disinfector Time: 2 h Frequency: 2 times/d | Check the preliminary screening table, symptoms and signs, and epidemiological historyTake temperature if necessary | Endoscopic diagnosis and treatment | Stop diagnosis and treatment; Send to fever clinic of emergency department |
| Resuscitation room | Long sleeve overalls; medical surgical mask; disposable medical cap; plastic gloves/nitrile gloves | Free hand-washing disinfection (per bed) | Surface disinfection: 75% alcohol Floor and sofa disinfection: 1000–2000 mg/L chlorine-containing disinfectant Frequency: 1 or 2 times/d | Secretion/blood pollution: 2000 mg/L chlorine-containing disinfectant Frequency: immediate | Continuous fresh air exchange Automatic air disinfector Time: 2 h Frequency: 2 times/d | Make sure they wear the mask when the patient leaves the resuscitation room; Publicity and education for family members | ||
| Disinfection room | Long sleeve overalls; Disposable waterproof isolated clothing; medical surgical face mask and glasses; disposable medical cap; latex gloves; special shoes | Free hand-washing disinfection | Surface disinfection: 500 mg/L chlorine-containing disinfectant Floor disinfection: 500 mg/L chlorine-containing disinfectant Frequency: 1 or 2 times/d | Secretion/blood pollution: 2000 mg/L chlorine-containing disinfectant Frequency: Immediate | Keep the storage cabinet ventilated, clean and dry | Suspend use of glutaraldehyde, and use peracetic acid for disinfection/sterilization | ||
| Office area | Personal clothes; Mask; All personnel are not allowed to come to the office with protective isolated clothing | Free hand-washing disinfection | Surface disinfection: 1000 mg/L chlorine-containing disinfectant Floor disinfection: 1000 mg/L chlorine-containing disinfectantFrequency: 2 or 3 times/d Doorknob disinfection: 75% alcohol (2–4 times/d) | Continuous fresh air exchange | Workers shall pack and seal the soiled bags in time | |||
| Staff for confirmed or suspected patients | Long sleeve overalls; disposable waterproof isolated clothing; medical protective clothing; protective face mask; protective glasses; N95 mask; protective shoe cover; double latex gloves | Free hand-washing disinfection; inside/outside the door of operation room | Surface disinfection: 2000 mg/L chlorine-containing disinfectant Floor disinfection: 2000 mg/L chlorine-containing disinfectant Frequency: Immediately after operation | Continuous fresh air exchange automatic air disinfector Time: 2 h/time Frequency: immediately after each operation | Operation room: Room 1; isolation corridor; staff: 2 doctors, 2 nurses and 2 anesthesiologists. All items prepared before operation, including environmental disinfection items. All remaining items shall be taken out after removing the outer package after the end of disinfection. All medical wastes shall be treated as hazardous wastes. After the final disinfection, the medical staff shall wait for 20 min for fresh air exchange, then remove the isolation protection facilities, turn on the sterilizer, after 30 min of disinfection, take off the mask and leave the inspection room. Disinfect the door handle again outside the door and have hand hygiene | |||
All medical staff had to change their personal clothes and wear a gown before entering the endoscopy center. They had to enter the main building through a channel different from patients after measuring their body temperature. Before meeting patients, medical staff had to perform hand hygiene, and wear a disposable surgical gown, with a face mask, hat, goggles, gloves, and protective shoe covers.
The symptoms and epidemiological history of patients were rechecked before further intervention. Staff had to maintain a distance from each patient in the explanation step before starting endoscopic intervention. Hands had to be washed before and after contact with each patient, after contact with a potential source of infection, and before and after wearing and removing personal protective equipment, including gloves[10]. Three levels of protection were required in case of exposure to respiratory secretions, such as tracheal intubation, airway care, and sputum aspiration for general patients, as well as during performing any endoscopic procedure on confirmed or suspected COVID-19 patients[11]. The tissue samples obtained during endoscopy were stored in a fixed area and the endoscopy report was provided to avoid cross-infection.
Medical staff took off their disposable items in the exit channel, and put them in the medical waste bin. To save materials, we did not discard all protective materials after each operation. We changed gloves and disinfected hands after each operation. Other protective equipment was not be replaced if there was no secretions or splashes. A seven-step hand-washing method was applied. Body temperature was recorded before leaving the endoscopy center. Staff changed from their gown to personal clothes, and put the gown in a specific tub. When off duty, staff stayed indoors and cooperated with the epidemic prevention management of the community. The manager of the endoscopy center communicated with the hospital management team closely and regularly, monitored the outbreak closely, and changed the plans quickly to deliver sustainable and effective endoscopy services.
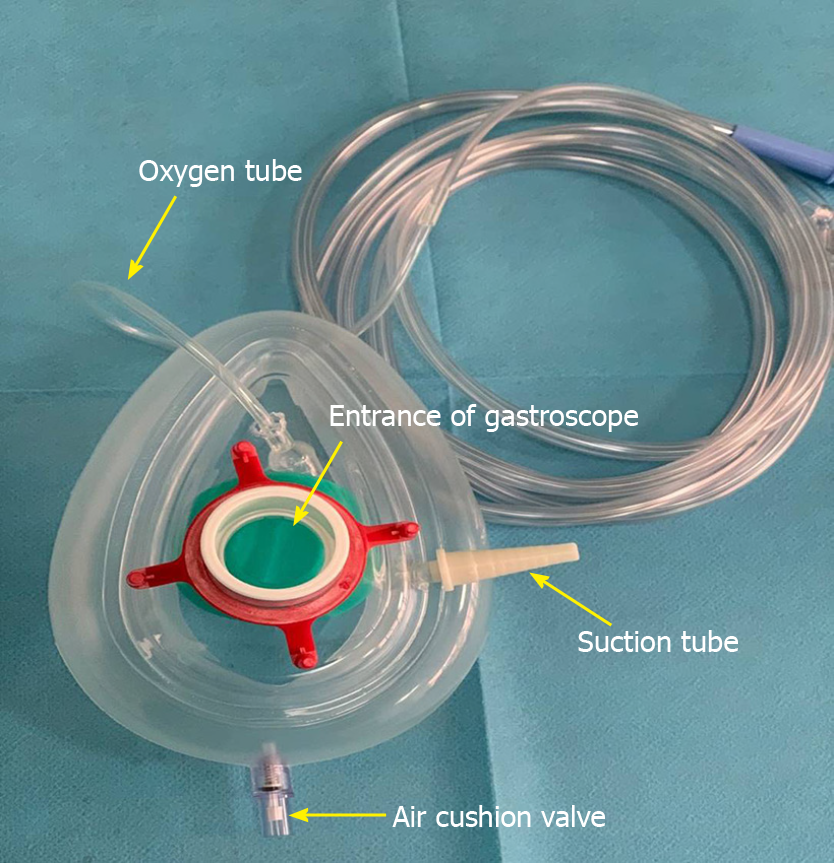
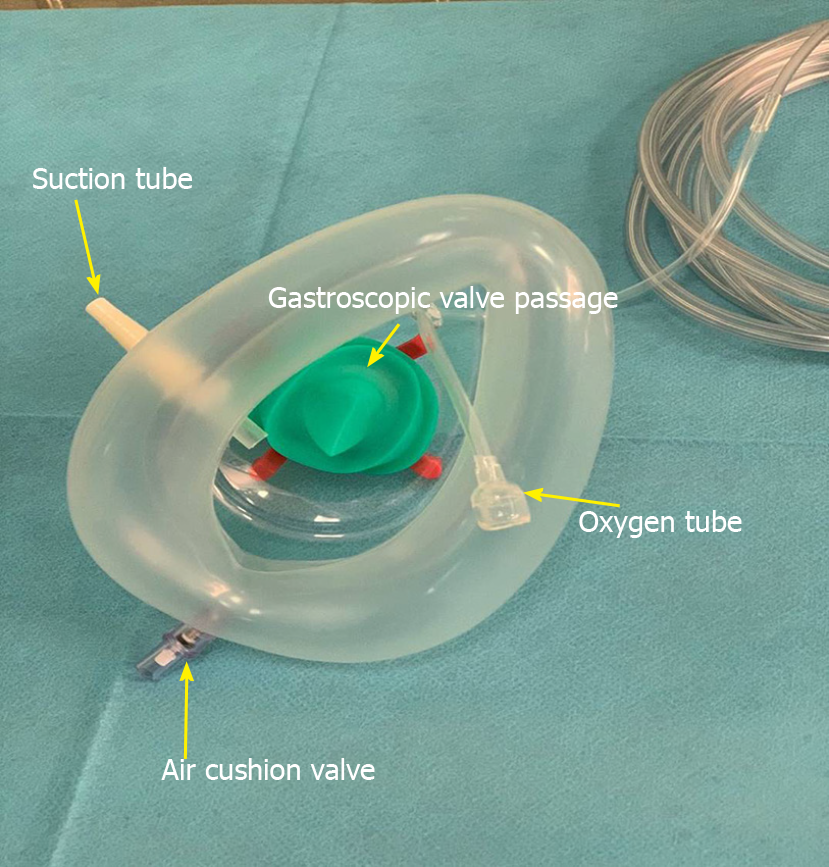
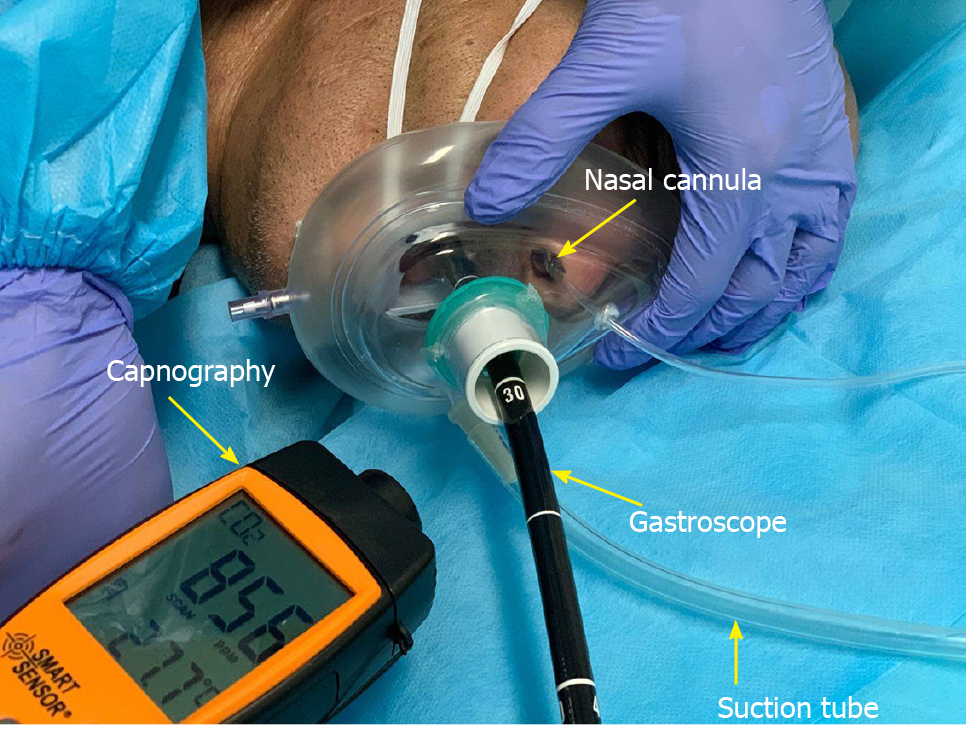
Based on the concept that patients with air-borne infectious disease should be isolated in negative pressure wards in order to prevent infection[8], a fully-enclosed “isolated mask” for patients undergoing upper gastrointestinal endoscopy was developed. The mask provided both oxygen inhalation and negative pressure (for suction of patients’ expulsion from mouth and nose) (Figures 2 and 3). The end of the mask cannula could be freely closed with a unidirectional flap at the entrance, which was fixed on the inside of the cannula to prevent patients’ expulsion from overflowing. There were two separate windows on the left and right sides of the mask bulge. One window was reserved for the oxygen tube, and the other was used for negative pressure suction.
The size of the window aperture was the same as the diameter of the tube, and it was sealed tightly. After the mask was inflated, it closely fitted the patient’s face to avoid expulsion leakage. The oxygen inhalation flow rate was adjusted to 6–8 L/min. The suction tube was connected to the central negative pressure system and the aspirated liquid (gas) was continuously removed to the hospital waste liquid (gas) treatment center. We have applied this isolated mask to 162 patients for respiratory isolation during upper gastrointestinal endoscopy (Figure 4). The gastroscopy process was smooth and the vital signs of the patients remained stable during and after the operation. No hospital infection occurred in our endoscopy center.
Our endoscopy center achieved effective epidemic prevention and undertook much diagnostic and therapeutic work during the COVID-19 pandemic. Several factors influenced the outcome of this management. First, experienced personnel led the overall situation and laid the foundation for success. We established a special prevention and control group at the beginning of the pandemic: The director as the team leader, the head nurse as the deputy team leader, and the infection control nurse and anesthetic medical team leader as the backbone. We quickly started our emergency procedures and adjusted the working mode in time: Delayed ordinary endoscopy, reduced the flow and aggregation of people, and kept special channels for patients with emergencies. In addition, we implemented a three-level screening mechanism and strengthened personnel access management. We improved the cleaning and disinfection of endoscopes and the environment. We formulated standards for pandemic protection in our endoscopy center, strictly implemented the health supervision of employees, and trained all staff in the use of personal protective equipment. Finally, although not used in large quantities, our innovative isolated mask played an important role. Our strategies may provide a comprehensive management for endoscopy centers during the COVID-19 pandemic.
As an infectious disease mainly transmitted by respiratory tract and contact, COVID-19 has its own special characters. The COVID-19 pandemic has attracted unprecedented global concern, which needs global unity. COVID-19 is transmitted from respiratory secretions, feces, and contaminated environmental surfaces. In addition, the virus is spread not only by patients with symptoms but also by asymptomatic individuals[9]. However, control of the pandemic can be realized through reasonable prevention and management. Other infectious diseases with the same or similar route of transmission can be managed by this method in medical environments with high risk of exposure, such as endoscopy centers. Some parts of this strategy (like three-level screening) can also be applied in community hospitals, which generally provide no endoscopic procedures for patients.
In conclusion, further protection of patients and medical staff is required during the outbreak of COVID-19 or other infectious diseases. We share our experience to provide valuable information for China and other countries that are suffering from the COVID-19 pandemic.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Ahmed M, Amornyotin S, Atogebania JW, Ribeiro IB S-Editor: Zhang L L-Editor: MedE-Ma JY P-Editor: Ma YJ
| 1. | Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS; China Medical Treatment Expert Group for Covid-19. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382:1708-1720. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19202] [Cited by in RCA: 18877] [Article Influence: 3775.4] [Reference Citation Analysis (7)] |
| 2. | Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, Ren R, Leung KSM, Lau EHY, Wong JY, Xing X, Xiang N, Wu Y, Li C, Chen Q, Li D, Liu T, Zhao J, Liu M, Tu W, Chen C, Jin L, Yang R, Wang Q, Zhou S, Wang R, Liu H, Luo Y, Liu Y, Shao G, Li H, Tao Z, Yang Y, Deng Z, Liu B, Ma Z, Zhang Y, Shi G, Lam TTY, Wu JT, Gao GF, Cowling BJ, Yang B, Leung GM, Feng Z. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N Engl J Med. 2020;382:1199-1207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11224] [Cited by in RCA: 9319] [Article Influence: 1863.8] [Reference Citation Analysis (0)] |
| 3. | Wang FS, Zhang C. What to do next to control the 2019-nCoV epidemic? Lancet. 2020;395:391-393. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 155] [Cited by in RCA: 148] [Article Influence: 29.6] [Reference Citation Analysis (0)] |
| 4. | Mahase E. China coronavirus: mild but infectious cases may make it hard to control outbreak, report warns. BMJ. 2020;368:m325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 5. | Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020;395:1225-1228. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1931] [Cited by in RCA: 1799] [Article Influence: 359.8] [Reference Citation Analysis (0)] |
| 6. | CDC COVID Data Tracker. United States COVID-19 Cases and Deaths by State. Available from: https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/summary.html. |
| 7. | Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054-1062. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17476] [Cited by in RCA: 18201] [Article Influence: 3640.2] [Reference Citation Analysis (0)] |
| 8. | Chiu PWY, Ng SC, Inoue H, Reddy DN, Ling Hu E, Cho JY, Ho LK, Hewett DG, Chiu HM, Rerknimitr R, Wang HP, Ho SH, Seo DW, Goh KL, Tajiri H, Kitano S, Chan FKL. Practice of endoscopy during COVID-19 pandemic: position statements of the Asian Pacific Society for Digestive Endoscopy (APSDE-COVID statements). Gut. 2020;69:991-996. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 256] [Cited by in RCA: 249] [Article Influence: 49.8] [Reference Citation Analysis (0)] |
| 9. | Li Y, Xia L. Coronavirus Disease 2019 (COVID-19): Role of Chest CT in Diagnosis and Management. AJR Am J Roentgenol. 2020;214:1280-1286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 662] [Cited by in RCA: 653] [Article Influence: 130.6] [Reference Citation Analysis (0)] |
| 10. | Repici A, Maselli R, Colombo M, Gabbiadini R, Spadaccini M, Anderloni A, Carrara S, Fugazza A, Di Leo M, Galtieri PA, Pellegatta G, Ferrara EC, Azzolini E, Lagioia M. Coronavirus (COVID-19) outbreak: what the department of endoscopy should know. Gastrointest Endosc. 2020;92:192-197. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 373] [Cited by in RCA: 380] [Article Influence: 76.0] [Reference Citation Analysis (0)] |
| 11. | Zhang Y, Zhang X, Liu L, Wang H, Zhao Q. Suggestions for infection prevention and control in digestive endoscopy during current 2019-nCoV pneumonia outbreak in Wuhan, Hubei province, China. Endoscopy. 2020;52:312-314. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 58] [Article Influence: 11.6] [Reference Citation Analysis (0)] |