Published online Sep 7, 2020. doi: 10.3748/wjg.v26.i33.5050
Peer-review started: May 20, 2020
First decision: July 29, 2020
Revised: August 3, 2020
Accepted: August 26, 2020
Article in press: August 26, 2020
Published online: September 7, 2020
Processing time: 106 Days and 18.7 Hours
Russell body gastritis (RBG) is very rare type of chronic inflammation of gastric mucosa. The pathologic hallmark of the disease is Russell bodies (RB) which represent accumulation of eosinophilic cytoplasmic inclusions in endoplasmic reticulum of mature plasma cells (Mott cells). Most published cases are associated with Helicobacter pylori (H. pylori) infection because of correlation between plasma cell activation and antigenic stimulation. There are insufficient data about H. pylori-negative RBG and very little is known about the natural course of the disease.
A 51-year-old male patient underwent endoscopic screening for mild iron deficiency anemia. Gastroscopy revealed diffuse hyperemia, edema and nodularity of the fundic and corpus mucosa. Due to non-specific endoscopic findings and iron-deficiency anemia our preliminary diagnosis was diffuse type of gastric carcinoma or gastric lymphoma. Biopsy specimens of gastric mucosa showed inflammatory infiltrate rich in Mott cells, consisting entirely of cytoplasmic RB. Absence of nuclear atypia and mitosis of the plasma cells, polyclonal pattern of the Mott cells and negative staining for cytokeratins favored diagnosis of RBG. The patient was treated with proton-pump inhibitor for 8 wk. Long-term clinical and endoscopic surveillance was scheduled. Albeit, there was no improvement in endoscopic features of the gastric mucosa in three consecutive gastroscopies, histopathological findings demonstrated that the chronic inflammatory infiltrate in the fundic mucosa is less pronounced, rich in plasma cells, with almost absent RB and Mott cells.
The prognosis of this entity is uncertain, that is why these patients are subjects of continuous follow up.
Core tip: We report a long-term follow up in a patient with Helicobacter pylori (H. pylori)-negative Russell body gastritis. Endoscopic findings include vast spectrum of nonspecific features without significant improvement in three consecutive gastroscopies. On the other hand, histology report showed tendency from decrease up to complete extinction of Russell bodies and Mott cells over time and under the influence of treatment. So far little is known about its etiology and pathogenesis, thus larger studies must be conducted. In this article, we summarize the most important clinical, endoscopic and histopathologic findings and associated conditions with H. pylori-negative Russell body gastritis, published in the literature so far.
- Citation: Peruhova M, Peshevska-Sekulovska M, Georgieva V, Panayotova G, Dikov D. Surveilling Russell body Helicobacter pylori-negative gastritis: A case report and review of literature. World J Gastroenterol 2020; 26(33): 5050-5059
- URL: https://www.wjgnet.com/1007-9327/full/v26/i33/5050.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i33.5050
The first case of Helicobacter pylori (H. pylori)-related Russell body gastritis (RBG) was announced in 1998 by Tazawa et al[1]. They described that H. pylori-positive gastritis is characterized by localized accumulation of plasma cells containing Russell bodies (RB) in gastric mucosa[1]. RB represent nondegradable, condensed immunoglobulin disposed in endoplasmic dilated rough reticulum cistern of plasma cells[2].
Most of the cases reported in the English literature so far are about H. pylori-positive RBG[3,4]. The main theory regarding the pathogenesis of RBG includes chronic infection with H. pylori leading to abnormal secretion of immunoglobulin or their derivates by plasma cells and subsequent formation of intracellular RB[5].
The few H. pylori-negative RBG cases that have been published were associated with HIV infection, alcohol and drug abuse, concomitant carcinoma and plasma cell neoplasms.
The clinical and endoscopic manifestation of RBG are variable and non-specific[6,7]. This rare type of chronic gastritis should be distinguished from other malignancies of the stomach such as carcinoma, lymphoma and plasmacytoma.
We present a case from our practice with H. pylori-negative RBG, who underwent endoscopic and histological surveillance three times over a period of one year.
We also made a review of twenty-one cases of H. pylori-negative RBG published in the literature up to now with their specific and unique clinical, endoscopic and histopathological features.
We present a case of a 51-year-old male who underwent endoscopic screening for mild iron deficiency anemia. The patient had no upper and lower gastrointestinal (GI) complaints.
The iron-deficiency anemia was diagnosed 2 mo before the admission to the hospital.
He was without other co-morbidities and past history for illness.
From the physical examination, he had pale skin and visible mucous membranes.
The laboratory work-up showed hemoglobin = 107 g/L, serum iron was 10.2 µmol/L (11.6-31.3 µmol/L), ferritin 18.43 ng/mL (30-400 ng/mL), total iron binding capacity 83.2 µmol/L (45-72 µmol/L). Inflammatory serological markers were within the normal limits–CRP was 0.30 ml/L (0-5 mg/L). Other biochemistry test results as well as carcinoembryonic antigen and carbohydrate antigen 19-9, were within the normal limits.
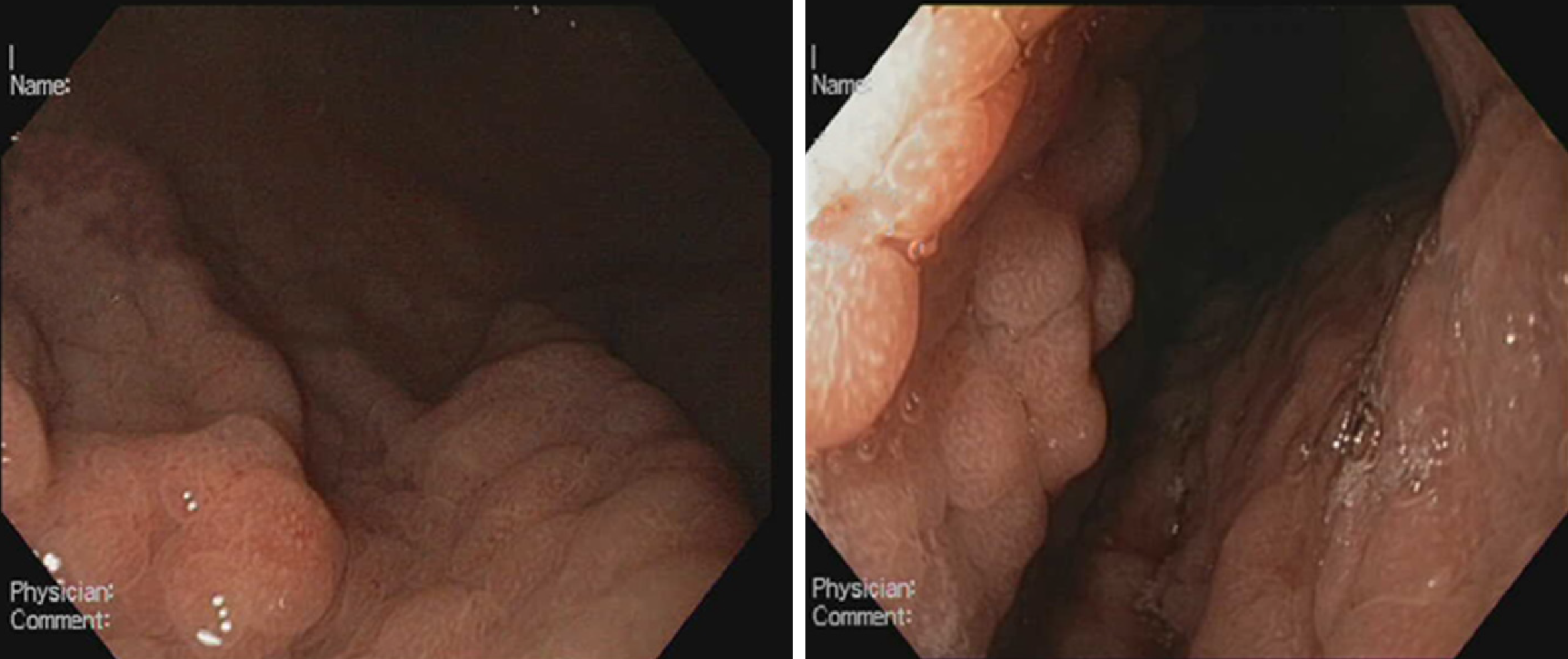
The colonoscopy was unremarkable. However, upper GI endoscopy revealed diffuse hyperemia, edema and nodularity of the gastric mucosa in the fundus and body, with a clear demarcation line between the body and the antrum. (Figure 1) The duodenal mucosa was intact. Due to non-specific endoscopic findings and iron-deficiency anemia our preliminary diagnoses were diffuse gastric carcinoma or gastric lymphoma. Therefore, multiple biopsies were taken from the stomach. We did not obtain duodenal, ileal and colonic biopsies, as there were no endoscopic abnormalities of the mucosa. We performed whole-body computed tomography with contrast enhancement. It showed neither pulmonary and abdominal space-occupying lesions, nor bone lytic lesions and enlarged lymph nodes.
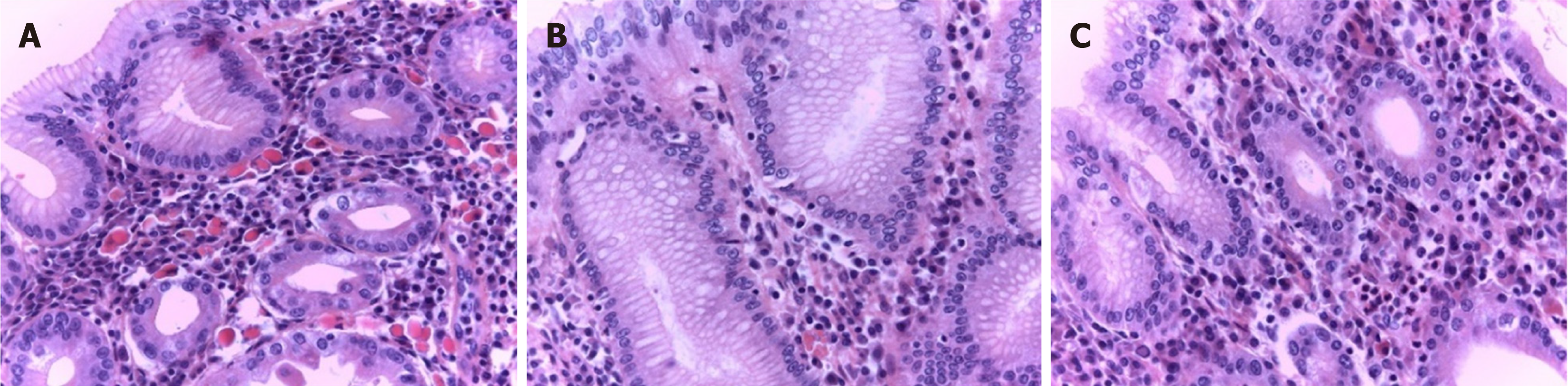
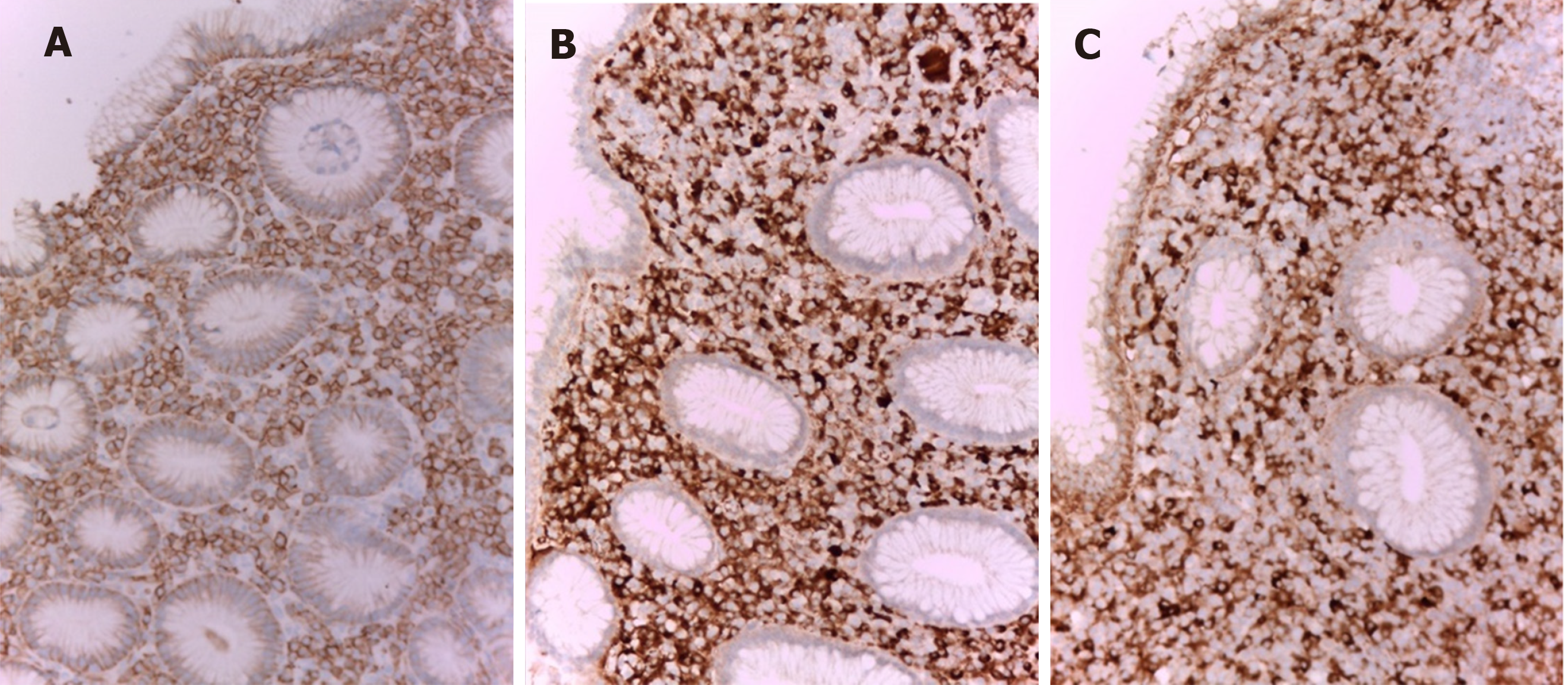
Histologically, in the biopsy of fundic mucosa, we observed inflammatory infiltrate rich in plasma cells with numerous eosinophilic hyaline bodies (RB) and so-called mature plasma cells (Mott cells), consisting entirely of cytoplasmic RB (Figure 2A). Several hyperplastic lymphoid follicles were also observed. The plasma cells expressed CD79a (Figure 3A), CD138 and they showed polyclonal pattern, both expressed kappa (Figure 3B) and lambda IgM light immunoglobulin chains (Figure 3C). А large number of eosinophils were seen and the neutrophilic leucocytes were rare.
There was no evidence of nuclear atypia and mitosis of the plasma cells, which ruled out lymphoma. Giemsa staining for H. pylori infection was negative, as well as immunohistochemical detection. Negative staining for cytokeratin AE1/AE3 excluded the signet-ring cell carcinoma. This microscopic finding corresponds to the so-called RBG.
We ruled out HIV, HCV and HBV infections, as well as autoimmune diseases, such as autoimmune thyroiditis and rheumatoid arthritis. However we did not check for M protein in the serum, we did not perform Bence-Jones protein urine test, TB-spot, EBER in situ hybridization or trephine biopsy of the bone marrow.
Histopathological findings confirmed H. pylori-negative RBG.
The patient was treated with proton-pump inhibitor (PPI) (Esomeprazole)-20 mg bid for 8 wk and intravenous iron medication.
Long-term clinical and endoscopic surveillance was scheduled. Three months later, he came for follow-up. His blood tests showed slight increase of his hemoglobin level (117 g/L). He underwent second gastroscopy with endoscopic findings identical to the previous one. Diathermic snare was used which allowed obtaining of larger and deeper tissue specimen of gastric mucosa. Histology report revealed dense accumulation of plasma cells in lamina propria, with decreased distribution of RB (Figure 2B). Intestinal metaplasia was observed in the areas with plasma cell infiltration but without dysplasia. Histopathological findings from third gastroscopy, performed twelve months after the initial diagnosis, demonstrated that the chronic inflammatory infiltrate in the fundic mucosa is less pronounced, rich in plasma cells, with almost absent RB and Mott cells (Figure 2C).
RBG is a rare form of chronic gastritis which mostly affects the antrum and has a male predominance[8,9]. The diagnosis is histologic, and it is characterized by accumulation of plasma cells containing RB and Mott cells in gastric mucosa. According to the literature, mucosal infiltration with RB and Mott cells may be associated with infectious or autoimmune processes[8,10-13]. The diagnostic and differential-diagnostic histological algorithm includes immunohistochemical detection of plasma cell nature of the inflammatory infiltrate (CD138 and CD79a positivity), as well as its polyclonality (both kappa and lambda light immunoglobulin M chains expression). These immunohistochemical profiles, as well as the absence of nuclear atypia, mitotic activity, lymphoepithelial lesions and monoclonal infiltrates are most in keeping with a benign process and not with a lymphoproliferative disease (lymphoma or myeloma).
Signet-ring stomach adenocarcinoma, where the cells resemble RB, but show nuclear atypia, mitotic activity and cytokeratin expression must also be excluded[14,15].
Once the histologic diagnosis and differential-diagnosis have been made, the pathologist must prove or rule out the association with H. pylori infection. This is done with Giemsa staining or immunohistochemical detection.
Literature data for RBG histologic follow up are scarce.
We have the opportunity to follow up in three consecutive biopsies the histological evolution of gastric mucosa in RBG. Our results showed a tendency from decrease up to complete extinction of RB and Mott cells in this chronic gastritis over time and under the influence of treatment. Our histologic follow up results indicate that RBG is probably an inconstant and dynamic morphological finding developing within a rich of plasma cells chronic gastritis. Like other authors we observe decreased number of RB and Mott cells in the time[8]. In contrast to this study, our results show that the reason for decreased number of RB in the stomach is not H. pylori eradication. Probably, the factor causing RB formation is not only H. pylori infection, other factors may also play role such as local degenerative or vascular-circulatory phenomena.
In one study, a total of 15 cases of RBG with polyclonal plasma cells, containing RB (Mott cells) have been described[8]. Our case also showed polyclonal proliferation of plasma cells with RB with uneventful clinical follow up. The decreased number of Mott cells in the stomach after H. pylori eradication shows that H. pylori is one of the factors causing RB formation. In practical terms, the latter can be used as an additional diagnostic sign in contrast to the increased follow up distribution of RB in the context of multiple myeloma-associated RBG[6].
Diffuse infiltration of plasma cells with RB in the gastric mucosa requires differential diagnosis with several diseases. Cytokeratin negativity and CD79a positivity exclude signet-ring cell carcinoma of the stomach. Kappa and lambda polyclonal immunoreactive pattern exclude lymphoplasmacytic lymphoma[1-3,5,7,16,17], plasmacytoma and monoclonal gammopathy of undetermined significance[4]. The lesion can be differentiated from MALT lymphoma by absence of nuclear atypia and lymphoepithelial lesions[8,18-20].
There are many unclear points about the etiology of RBG. According to Hasegawa[21], immunoglobulin accumulation could be in a result of an over or altered production as well as aberrant secretion and impaired excretion[21].
Most of the cases published in the literature have demonstrated a connection between H. pylori infection and antigenic stimulation of plasma cells[5,7]. On the other hand, H. pylori-negative RBG is rarely reported. To the best of our knowledge, only twenty-one cases are published in the literature so far. There are insufficient data about the etiology and progression of this entity. A possible relationship between H. pylori-negative RBG and the immune status has been proposed, with a number of cases reported in patients with HIV[10-12], alcohol[10,16,22] and drug abuse[10,13,16] and post-transplant patients[23].
Apart from chronic infections and immunosuppressive treatment, cancer could also be a trigger of immune dysregulation and RBC has been reported in patients with signet-ring cell carcinoma[14]. For this reason, it is of great importance to be able to discriminate between cancer-induced mucosal changes and RBG. During upper endoscopy this entity should be kept in mind because of the vast majority of differential diagnosis such as plasma cell neoplasms, signet-ring cell carcinoma and MALT lymphoma. It is also of great significance to obtain biopsies according to Sydney system.
Our case is about 51-year-old man with iron-deficiency anemia and H. pylori-negative RBG. We performed many diagnostic tests to rule out chronic infections, autoimmune diseases associated with B cell proliferation and different malignancies of gastric mucosa. We came to the conclusion that RBG in our patient is a benign process with uncertain prognosis and long-term clinical and endoscopic follow-up was scheduled. For a period of one year we observed histologic regression, most probably in a result of his 8-wk-treatment with PPI. Hence, PPI therapy could be considered as a feasible option of treatment for this rare type of gastritis.
In our article we present all published cases in English literature with H. pylori-negative RBG so far.
A summary of 22 reported H. pylori-negative RBG is described in Table 1.
| Cases | Ref. | Age/sex | History | Endoscopic findings | Symptoms | Histology | Immunology (Mott cells) | Follow up |
| 1 | Erbersdobler et al[16] | 80/Female | Alcohol and analgesic abuse, Candida esophagitis | Circumscribed, irregular mucosal swelling at the back side of the fundus (lesion up to 3 cm) | Epigastric pain and nausea | Confirmed candida and showed plasma cells with RBs | Poly | NR |
| 2 NR | Drut et al[10] | 34/Male | HIV+, Drug addict, Alcohol abuse | 2-cm-raised area located at the major curvature of the body of the stomach, presenting a central 1 cm rounded macule | Epigastric pain, acute diarrhoea, blood-stained stools | Moderate-to-severe gastritis with RBs | Poly | NR |
| 3 | Habib et al[22] | 75/Male | Alcohol use, Renal failure Dyslipidaemia, Rhabdomyolysis | Oesophagitis and nodular chronic active gastritis in the antrum | Reflux complaints, intermittent coffee-ground emesis | Regenerative changes and a dense chronic inflammatory infiltrate composed of numerous RBs | Poly | NR |
| 4 | Del Gobbo et al[7] | 78/Female | NR | Hyperaemia in the antral and GEJ mucosa | Epigastric pain | Moderate chronic inflammation in the mucosa of the cardia showed RBs | Poly | NR |
| 5 | Coyne et al[13] | 49/Male | Drug addict,HCV and Diabetes mellites | Severe erosive gastritis with oedematous mucosal folds | Nausea, epigastric pain, weight loss | RBG | Mono (κ chain, IgM) | NR |
| 6 | Bhalla et al[12] | 82/Male | HIV+ | Gastritis | Dyspepsia, loose stools, loss of appetite and weight | RBs present in gastric mucosa | Poly | NR |
| 7 | Klair et al[24] | 76/Female | Anemia,Multiple myeloma | Multiple small polyps in the fundus were seen on retroflexion, along with cobblestoned erythematous and irregular mucosa | Bone pains and adynamia | Oxyntic mucosa with chronic, inactive gastritis, with plasma cells | Poly | NR |
| 8 | Zhang et al[17] | 78/Male | NR | Gastritis with uneven mucosa in the antrum, corpus and incisura angularis | Heartburn | RBG with moderate chronic inflammation | Mono (κ chain) | Clinical follow-up evaluations were uneventful |
| 9 | Zhang et al[17] | 28/Male | NR | Erythema in antrum | Epigastric pain | RBG with mild chronic inflammation | Mono (κ chain) | NR |
| 10 | Zhang et al[17] | 24/Female | NR | Erythema in antrum | Abdominal discomfort | RBG with mild chronic inflammation | Mono (κ chain) | NR |
| 11 | Zhang et al[17] | 66/Male | NR | Ulceration stage A2 in Forrest classification in incisura angularis | Haematochezia | RBG with moderate glandular atrophy and mild chronic inflammation | NR | NR |
| 12 | Muthukumarana et al[23] | 44/M | Status post pancreatic and Kidney transplant Diabetes mellites | Diffuse mild erythematous gastric mucosa, non-cratered duodenal ulcer | Watery diarrhoea with abdominal pain, nausea and vomiting | Stomach, duodenum, terminal ileum, colon mucosa with RBs | Poly | NR |
| 13 | Saraggi et al[25] | 66/Male | NR | Los Angeles class A esophagitis. Multiple biopsy has been taken from GEJ and cardia | Heartburn | Mild lymphoplasmacytic inflammation in the mucosa of the cardia with RBs | Poly | NR |
| 14 | Antunes et al[26] | 79/Female | NR | 8 mm mucosal break in the lower oesophagus classified as grade B in the Los Angeles classification for oesophagitis, and a whitish and nodular area of mucosa in the incisura angularis | Hematemesis | RBG | NR | NR |
| 15 | Imai et al[27] | 64/Male | Chronic renal failure on dialysis | Flare, swollen mucous membrane and multiple verrucous erosion in gastric antrum | Poor appetite and blood eosinophilia | Infiltration of plasma cell containing RBs and eosinophils | IgA and kappa-light chain | NR |
| 16 | Trna et al[28] | 77/Male | NR | Several areas of different and mildly prominent mucosa in the GEJ and cardia | Non-cardiac chest pain and mild dysphagia | Nondysplastic intestinal metaplasia with mild chronic inflammatory infiltrate with RBs and plasma cells | NR | Follow-up endoscopy with biopsies– without any difference |
| 17 | Altindag et al[6] | 81/Female | Multiple myeloma (diagnosed from bone marrow 3years after endoscopy) | Gastritis in the antrum | Dyspepsia | Mild inflammation of gastric mucosa with RB | Poly | Histology report revealed increased distribution in RBs in follow-up endoscopy |
| 18 | Altindag et al[6] | 79/Female | NR | Gastritis in the antrum and gastric tubular adenoma with LGD | GI bleed | Mild glandular atrophy, moderate intestinal metaplasia, severe inflammation of gastric mucosa with RB | Poly | NR |
| 19 | Altindag et al[6] | 72/Male | NR | Gastritis in the antrum | Dyspepsia | Mild inflammation of gastric mucosa with RB and mild glandular atrophy | Poly | NR |
| 20 | Altindag et al[6] | 64/Male | Colonic tubular adenoma, HGD | Gastritis in the antrum | Epigastric pain, suspicion of gastric tumor | Moderate glandular atrophy, moderate intestinal metaplasia and moderate inflammation of gastric mucosa with RB | Poly | NR |
| 21 | Qiao et al[11] | 28/Male | HIV+, pancytopenia, splenomegaly, hepatomegaly | Erosions, erythematous mucosa, and vascular congestion in the gastric body and antrum | Abdominal pain, fatigue, rectal bleeding | Chronic inactive gastritis with RB infiltration in the mucosa | Poly | NR |
| 22 | Present study | 52/Male | Anemia | Diffuse hyperemia and edema of the gastric mucosa in the fundus and body | Iron-deficiency anemia | Abundant plasma cell inflammatory infiltrate, rich in RB and Mott cell | Poly | Without endoscopic improvement, histology report showed-decreased RB in second follow-up and almost absent RB in third follow-up |
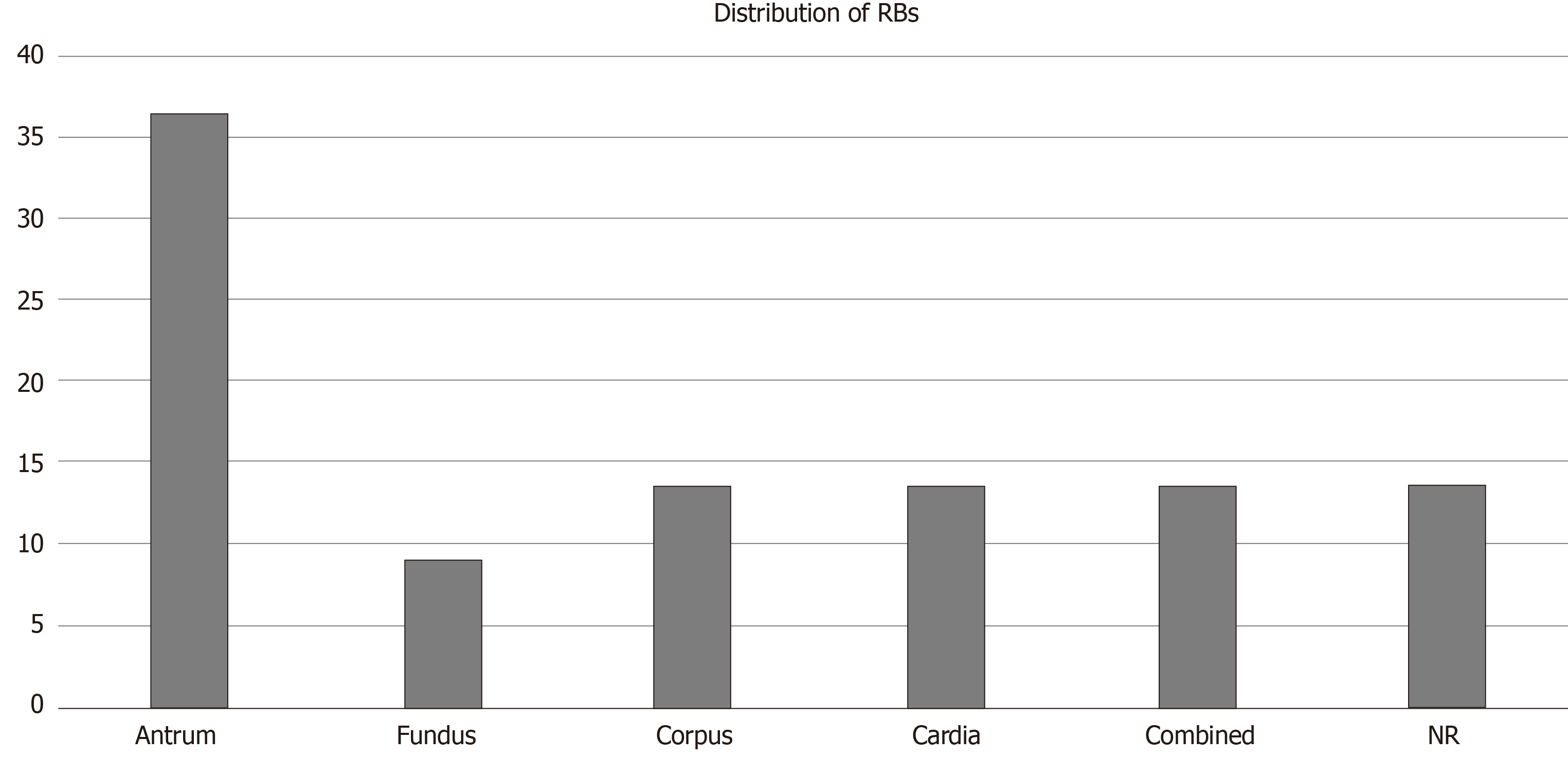
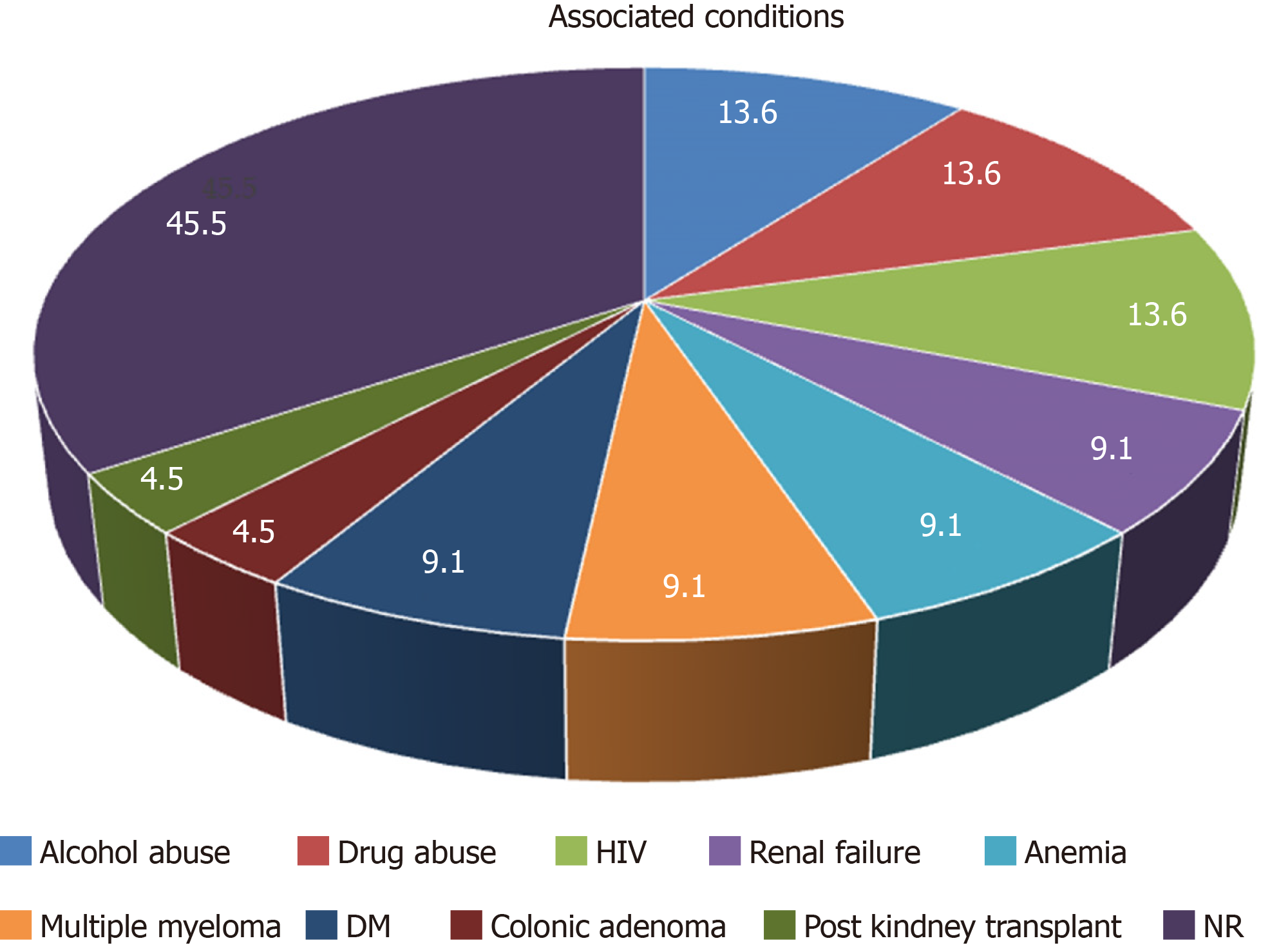
Aggregated data from all the reported cases show that patients are within the age range of 20 to 82 years with predominant age group between 70-80 years (40.9%). Male to female ratio was 2.14:1. Most of the patients had GI symptoms such as abdominal pain, dyspepsia and nausea. Endoscopic findings include vast spectrum of nonspecific features such as erythema, edema, erosions and ulcerations or well-formed nodular lesions. In eight of the patients H. pylori-negative RBG was localized in the gastric antrum (36.36%), in three of them it was in body of the stomach (13.63%), in the cardia (13.63%), in more than one region of the stomach (13.63%) and without specific localization in three of the patients (13.63%). According to our data, RBs distribution is the rarest in the fundus (9.09%) (Figure 4). Of all the twenty-two cases, two patients had anemia as concomitant disease[24], three reported alcohol abuse[10,16,22] and three with HIV infection[10-12] (Figure 5). Other associated conditions include multiple myeloma, chronic kidney failure, drug abuse, post kidney transplant, diabetes mellitus and colonic adenoma. Majority of the cases (ten) with H. pylori-negative RBG showed no evidence of concurrent medical conditions. In this literature review it is well visible that two of the cases of H. pylori-negative RBG are associated with lympho-proliferative disease (multiple myeloma)[6,24-28].
We would like to summarize that there are few cases of H. pylori-negative RBG described in the literature. This condition should be kept in mind during endoscopic surveillance and differentiated from other benign and malignant entities. To the best of our knowledge, our report is the first that present a long-term follow up in a patient H. pylori-negative RBG, treated with PPI. We came to conclusion that PPI therapy leads to significant reduction of RB and plasma cells in the gastric mucosa.
So far little is known about its etiology and pathogenesis, thus larger studies must be conducted. The outcome of chronic stimulation of the Mott cells is unknown, therefore it is of paramount importance to actively follow up these patients.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: United European Gastroenterology; ESGE, No. 56088243; Bulgarian Society of Gastroenterology.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Bulgaria
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Farhat S, Neri V, Serban ED, Sergi C S-Editor: Zhang L L-Editor: A P-Editor: Ma YJ
| 1. | Tazawa K, Tsutsumi Y. Localized accumulation of Russell body-containing plasma cells in gastric mucosa with Helicobacter pylori infection: 'Russell body gastritis'. Pathol Int. 1998;48:242-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 56] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 2. | Bhaijee F, Brown KA, Long BW, Brown AS. Russell body gastroenteritis: an aberrant manifestation of chronic inflammation in gastrointestinal mucosa. Case Rep Med. 2013;2013:797264. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 3. | Ensari A, Savas B, Okcu Heper A, Kuzu I, Idilman R. An unusual presentation of Helicobacter pylori infection: so-called "Russell body gastritis". Virchows Arch. 2005;446:463-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Wolkersdörfer GW, Haase M, Morgner A, Baretton G, Miehlke S. Monoclonal gammopathy of undetermined significance and Russell body formation in Helicobacter pylori gastritis. Helicobacter. 2006;11:506-510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Paik S, Kim SH, Kim JH, Yang WI, Lee YC. Russell body gastritis associated with Helicobacter pylori infection: a case report. J Clin Pathol. 2006;59:1316-1319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 40] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 6. | Altindag SD, Cakir E, Ekinci N, Avci A, Dilek FH. Analysis of clinical and histopathological findings in Russell body gastritis and duodenitis. Ann Diagn Pathol. 2019;40:66-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 7. | Del Gobbo A, Elli L, Braidotti P, Di Nuovo F, Bosari S, Romagnoli S. Helicobacter pylori-negative Russell body gastritis: case report. World J Gastroenterol. 2011;17:1234-1236. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 20] [Cited by in RCA: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Yorita K, Iwasaki T, Uchita K, Kuroda N, Kojima K, Iwamura S, Tsutsumi Y, Ohno A, Kataoka H. Russell body gastritis with Dutcher bodies evaluated using magnification endoscopy. World J Gastrointest Endosc. 2017;9:417-424. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Pizzolitto S, Camilot D, DeMaglio G, Falconieri G. Russell body gastritis: expanding the spectrum of Helicobacter pylori - related diseases? Pathol Res Pract. 2007;203:457-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Drut R, Olenchuk AB. Images in pathology. Russell body gastritis in an HIV-positive patient. Int J Surg Pathol. 2006;14:141-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Qiao J, Dudrey E, Gilani S. Russell body gastritis. Pathologica. 2019;111:76-78. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Bhalla A, Mosteanu D, Gorelick S, Hani-el-Fanek. Russell body gastritis in an HIV positive patient: case report and review of literature. Conn Med. 2012;76:261-265. [PubMed] |
| 13. | Coyne JD, Azadeh B. Russell body gastritis: a case report. Int J Surg Pathol. 2012;20:69-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Wolf EM, Mrak K, Tschmelitsch J, Langner C. Signet ring cell cancer in a patient with Russell body gastritis--a possible diagnostic pitfall. Histopathology. 2011;58:1178-1180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Bozhkova DM, Dikov D. Should we perform cytokeratin immunostaining in cases of Russell body gastritis? Ann Diagn Pathol. 2020;46:151524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Erbersdobler A, Petri S, Lock G. Russell body gastritis: an unusual, tumor-like lesion of the gastric mucosa. Arch Pathol Lab Med. 2004;128:915-917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 17. | Zhang H, Jin Z, Cui R. Russell body gastritis/duodenitis: a case series and description of immunoglobulin light chain restriction. Clin Res Hepatol Gastroenterol. 2014;38:e89-e97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 18. | Joo M. Gastric mucosa-associated lymphoid tissue lymphoma masquerading as Russell body gastritis. Pathol Int. 2015;65:396-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Kai K, Miyahara M, Tokuda Y, Kido S, Masuda M, Takase Y, Tokunaga O. A case of mucosa-associated lymphoid tissue lymphoma of the gastrointestinal tract showing extensive plasma cell differentiation with prominent Russell bodies. World J Clin Cases. 2013;1:176-180. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (2)] |
| 20. | Fujiyoshi Y, lnagaki H, Tateyama H, Murase T, Eimoto T. Mott cell tumor of the stomach with Helicobacter pylori infection. Pathol Int. 2001;51:43-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Hasegawa H. Aggregates, crystals, gels, and amyloids: intracellular and extracellular phenotypes at the crossroads of immunoglobulin physicochemical property and cell physiology. Int J Cell Biol. 2013;2013:604867. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 22. | Habib C, Gang DL, Ghaoui R, Pantanowitz L. Russell body gastritis. Am J Hematol. 2010;85:951-952. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 23. | Muthukumarana V, Segura S, O'Brien M, Siddiqui R, El-Fanek H. "Russell Body Gastroenterocolitis" in a Posttransplant Patient: A Case Report and Review of Literature. Int J Surg Pathol. 2015;23:667-672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 24. | Klair JS, Girotra M, Kaur A, Aduli F. Helicobacter pylori-negative Russell body gastritis: does the diagnosis call for screening for plasmacytic malignancies, especially multiple myeloma? BMJ Case Rep. 2014;2014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 25. | Saraggi D, Battaglia G, Guido M. Russell body carditis. Dig Liver Dis. 2015;47:526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 26. | Antunes AG, Cadillá J, Velasco F. Russell body gastritis in an Hp-negative patient. BMJ Case Rep. 2016;2016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 27. | Imai T, Sentani K, Yamashita K, Oue N, Yoshida K, Yasui W. Russell Body Gastritis Concurrent with Eosinophilia: a case report. Hiroshima J Med Sci. 2016;65:69-72. [PubMed] |
| 28. | Trna J, Horáková I. Gastrointestinal tract and Russell bodies - a case report of Russell body carditis and review of the literature. Acta Gastroenterol Belg. 2017;80:551-552. [PubMed] |