Published online Sep 7, 2020. doi: 10.3748/wjg.v26.i33.4972
Peer-review started: March 27, 2020
First decision: May 21, 2020
Revised: May 29, 2020
Accepted: June 17, 2020
Article in press: June 17, 2020
Published online: September 7, 2020
Processing time: 160 Days and 14.7 Hours
Changes in bowel function after right-sided colectomy are not well understood compared to those associated with left-sided colectomy or rectal resection. In particular, there are concerns about bowel function after right-sided colectomy with complete mesocolic excision, which has become popular in the West.
To evaluate the functional outcomes of patients who underwent right-sided colectomy with D3 lymphadenectomy for colon cancer.
Functional data from patients who underwent minimally invasive right-sided colectomy for colon cancer from October 2017 to September 2018 were prospectively collected. Functional outcomes were evaluated preoperatively and at 3, 6, 12, and 18 mo postoperatively.
Prior to surgery, 57 patients answered the questionnaire, and 47 responded at three months, 52 at 6 mo, 52 at 12 mo, and 25 at 18 mo postoperatively. Most scales of quality of life and bowel function improved significantly over time. Urgency persisted to a high degree throughout the period without a significant change over time. The use of medications for defecation was about 10% over the entire period. Gas (P = 0.023) and fecal frequency (P < 0.001) increased, and bowel dysfunction group (P = 0.028) was more common among patients taking medication. At six months, resected bowel and colon lengths were significantly different as a risk factor between the dysfunction group and the no dysfunction group [odd ratio (OR): 1.095, P = 0.026; OR: 1.147, P = 0.031, respectively] in univariate analysis, but not in multivariate analysis.
Despite D3 lymphadenectomy, most bowel symptoms improved over time after right-sided colectomy using a minimally invasive approach, and continuous medication was needed in only approximately 10% of patients.
Core tip: In patients who underwent right-sided colectomy, bowel function and quality of life are mostly well preserved. Although concerns about functional outcomes have been raised since complete mesocolic excision has been widely applied, no significant problems have been experienced by patients. Approximately 10% of patients continue to need medication, and we need to pay attention to these patients.
- Citation: Lee KM, Baek SJ, Kwak JM, Kim J, Kim SH. Bowel function and quality of life after minimally invasive colectomy with D3 lymphadenectomy for right-sided colon adenocarcinoma. World J Gastroenterol 2020; 26(33): 4972-4982
- URL: https://www.wjgnet.com/1007-9327/full/v26/i33/4972.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i33.4972
As the incidence of colorectal cancer increases, problems that occur after treatment in colorectal cancer survivors are also becoming important social issues. As is true in other cancers, the issues that may arise in patients with colorectal cancer who are undergoing surgery vary. For patients and surgeons, short-term surgical complications are important immediately after surgery, and oncologic outcomes become important later on. In many cases, bowel habit changes, voiding, and sexual dysfunctions occur after surgery, and these functional problems are easily overlooked. Many patients experience poor quality of life (QOL) due to these functional problems[1-3]. In particular, multiple studies have demonstrated that the dysfunctions that follow rectal resection or left-sided colectomy are more severe[4-7]. Low anterior resection syndrome (LARS) is a generic term for bowel habit changes that occur after anterior or low anterior resection, including symptoms such as urgency, frequent defecation, stool fragmentation, fecal incontinence, difficult evacuation, and increased gas[8-11]. In general, LARS is caused by colonic dysmotility, neorectal reservoir dysfunction, and anal sphincter or pelvic nerve damage, but these causes may be combined, and the degree of symptoms among patients varies greatly[12].
Compared with bowel habit changes that occur after rectal resection or left-sided colectomy, bowel dysfunctions seen after right-sided colectomy are relatively mild and temporary and have not traditionally been considered a significant issue. Since the proximal colon and terminal ileum are mainly responsible for the absorption of water, there may be temporary postoperative symptoms such as diarrhea. Over time, the water absorption of the small bowel increases, and diarrhea mostly improves[13,14]. However, some patients have very severe, consistent bowel symptoms and sometimes do not get better even with medication[15-17]. Since the concept of complete mesocolic excision (CME) has been introduced, the range of right-sided colectomy has become more extensive, suggesting that the risk of bowel dysfunction due to superior mesenteric nerve plexus transection has increased[18-21]. Unlike left-sided colectomy, however, not many studies have been published on the topic of bowel dysfunction after right-sided colectomy. We therefore planned the present study to investigate changes in bowel function and associated alterations in QOL after right-sided colectomy with D3 lymphadenectomy.
In our institution, most colorectal surgeries are performed using a minimally invasive approach. This study included patients who underwent laparoscopic or robotic-assisted right hemicolectomy or extended right hemicolectomy for colon cancer at Korea University ANAM Hospital between October 2017 and September 2018. Patients identified as having adenocarcinoma of the appendix, cecum, ascending colon, hepatic flexure, or proximal transverse colon were included. Patients of all disease stages were eligible; however, patients who did not respond to the questionnaire were excluded from the study. This study was approved by the Institutional Review Board (IRB) of Korea University ANAM Hospital (IRB No. 2020AN0004), and all participants provided informed consent.
All included patients underwent right hemicolectomy or extended right hemicolectomy with D3 lymph node dissection. Bowel resections were performed from the terminal ileum to the transverse colon. In both surgeries, the ileocolic and right colic arteries were divided at their origin of the superior mesenteric artery, while the right branch or the root of the middle colic artery was further divided. In our institution, a soft diet is allowed on the second day after surgery if there are no specific problems observed. Antidiarrheal or constipation medications were prescribed as needed depending on the patient's symptoms. In cases of postoperative stage 2 disease with risk factors or stage 3 disease, oxaliplatin-based adjuvant chemotherapy (FOLFOX4 regimen) for 8-12 cycles or 5-fluorouracil with leucovorin (FL regimen) for 6 cycles was performed.
In our hospital, functional surveys are not routine. We prospectively collected questionnaires about QOL and symptoms, as well as bowel and urogenital function, in patients undergoing surgery for colorectal cancer between October 2017 and September 2018, and followed them up. Questionnaire responses were conducted preoperatively and 3, 6, 12, 18, and 24 mo after the operation; however, patients in the study were surveyed for up to 18 mo. The assessment of QOL used version 3 of the European Organization for Research and Treatment of Cancer (EORTC) Core QOL Questionnaire (QLQ) C30[22]. Bowel function was evaluated for the items of gas, stool leakage, frequency, fragmentation, and urgency[8]. Patients with responses of zero to 20 points were classified as the no bowel dysfunction group, those with 21 to 29 points were the minor dysfunction group, and those with 20 to 42 points were the major dysfunction group. Patients who received right-sided colectomy did not undergo the assessment for voiding or sexual function.
Continuous data are presented as mean values and categorical data are presented as numbers (percentages). Changes in the EORTC QLQ-C30 and bowel dysfunction scales were analyzed with the Wilcoxon single-rank test, comparing follow-up scores to the preoperative baseline. Correlations between EORTC QLQ-C30 and chemotherapy, between the scales and medication use, and between EORTC QLQ-C30 and the scales were analyzed by linear regression. Univariate and multivariate analyses of clinicopathologic factors were performed using Cox regression analysis in order to determine risk factors in the bowel dysfunction group (composed of both the minor and major dysfunction groups) as compared to the no bowel dysfunction group. Statistical analyses were performed using the Statistical Package for the Social Sciences version 20.0 (IBM Corp., Armonk, NY, United States), and P values less than 0.05 were accepted as statistically significant.
A total of 336 patients participated in the questionnaire during this study. Of these, 57 patients underwent right or extended right hemicolectomy with a minimally invasive approach. Forty-seven patients at three months, 52 at 6 mo, 52 at 12 mo, and 25 at 18 mo postoperatively participated in the questionnaire. The clinical characteristics of the patients who participated in the survey are described in Table 1. More than half of the participants had ascending colon cancer, and most underwent laparoscopic surgery and right hemicolectomy. The mean resected bowel length was 36.3 cm, the mean colon length was 26.7 cm, and the mean ileal length was 9.9 cm. No patients received chemotherapy before surgery, and 18 patients received chemotherapy after surgery (31.6%).
| n = 57 | |
| Age (yr) | 63.8 (36-80) |
| Male/female | 30 (52.6)/27 (47.4) |
| Body mass index (kg/m2) | 23.7 (18.6-33.9) |
| Location of lesion | |
| Appendix | 3 (5.3) |
| Cecum | 9 (15.8) |
| Ascending colon | 33 (57.9) |
| Hepatic flexure colon | 7 (12.3) |
| Transverse colon | 5 (8.8) |
| Operation type | |
| Laparoscopy | 56 (98.2) |
| Robot | 1 (1.8) |
| Procedure | |
| Right hemicolectomy | 47 (82.5) |
| Extended right hemicolectomy | 10 (17.5) |
| Resected bowel length (cm) | 36.3 (19.0-69.5) |
| Colon | 26.7 (9.5-56.0) |
| Ileum | 9.9 (3.2-35.5) |
| Preoperative obstruction | 10 (17.5) |
| Stage | |
| 0 | 8 (14.0) |
| 1 | 11 (19.3) |
| 2 | 19 (33.3) |
| 3 | 14 (24.6) |
| 4 | 5 (8.8) |
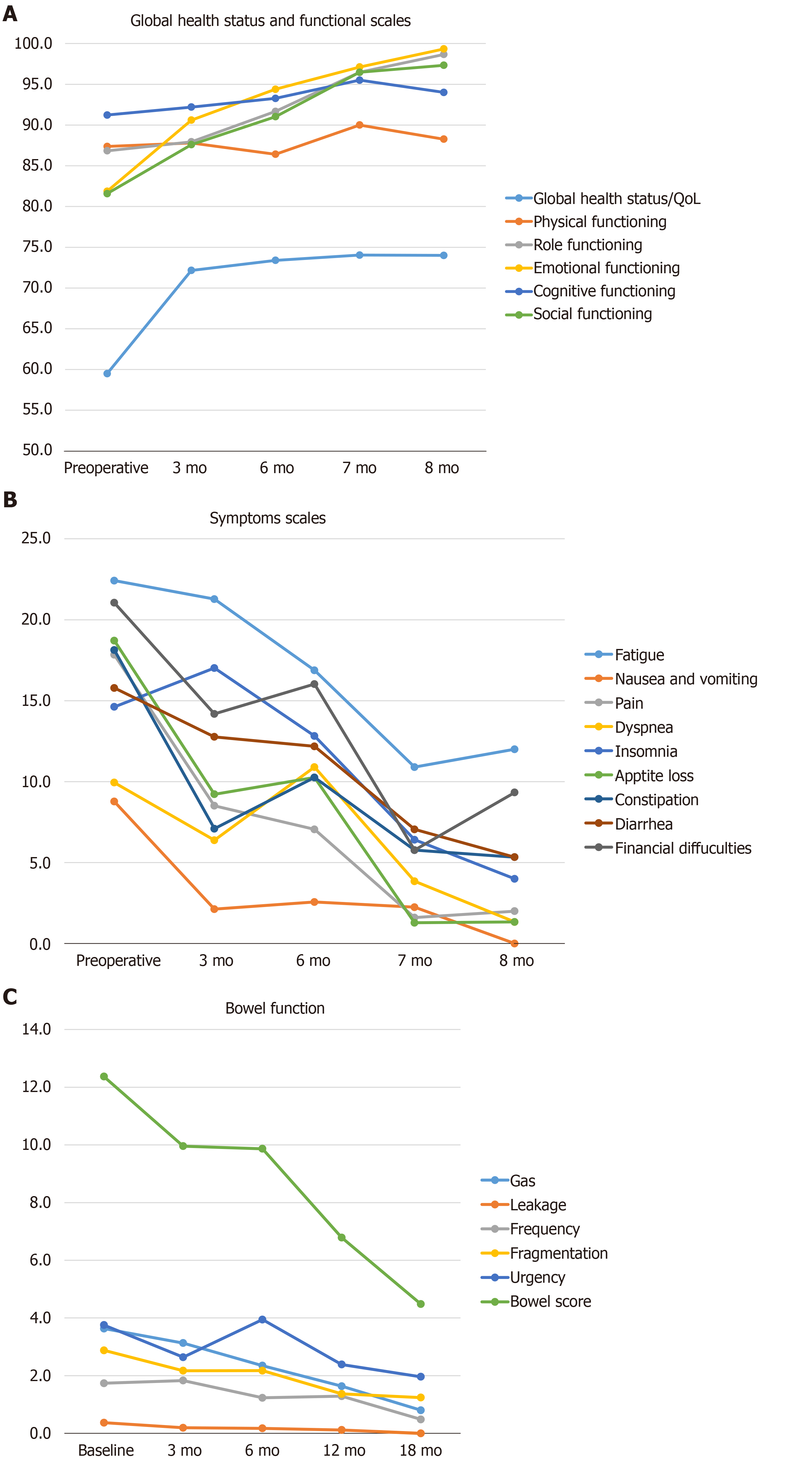
Most of the scales in the global health status, functional, and symptoms categories showed significant improvement over time (Table 2, Figure 1A and B). Most functional scales tended to consistently improve up to 18 mo. Many symptoms, on the other hand, showed a temporary deterioration at six months, then improved at 12 mo, and then had worsened again by 18 mo. There was a high burden of fatigue and financial difficulties reported throughout the study period. At three and six months after surgery, about 35%-40% of the patients received chemotherapy. Analyzing the correlation between chemotherapy and QOL, insomnia (P = 0.005) and total symptoms scales (P = 0.017) were significantly worse among patients who received chemotherapy. There was no difference in results according to chemotherapy regimen.
| Preoperative (n = 57) | 3 mo (n = 47) | 6 mo (n = 52) | 12 mo (n = 52) | 18 mo (n = 25) | P value1 | P value2 | |
| Global health status/QOL | |||||||
| Global health status/QOL | 59.5 | 72.2 | 73.4 | 74.0 | 74.0 | 0.001 | 0.145 |
| Functional scales | |||||||
| Physical functioning | 87.4 | 87.8 | 86.4 | 90.0 | 88.3 | 0.530 | 0.591 |
| Role functioning | 86.8 | 87.9 | 91.7 | 96.5 | 98.7 | 0.001 | 0.716 |
| Emotional functioning | 81.9 | 90.6 | 94.4 | 97.1 | 99.3 | < 0.001 | 0.795 |
| Cognitive functioning | 91.2 | 92.2 | 93.3 | 95.5 | 94.0 | 0.104 | 0.291 |
| Social functioning | 81.6 | 87.6 | 91.0 | 96.5 | 97.3 | < 0.001 | 0.135 |
| Sum | 428.9 | 446.1 | 456.8 | 475.6 | 477.6 | < 0.001 | 0.568 |
| Symptom scales/items | |||||||
| Fatigue | 22.4 | 21.3 | 16.9 | 10.9 | 12.0 | 0.001 | 0.207 |
| Nausea and vomiting | 8.8 | 2.1 | 2.6 | 2.2 | 0.0 | 0.001 | 0.470 |
| Pain | 17.8 | 8.5 | 7.1 | 1.6 | 2.0 | < 0.001 | 0.278 |
| Dyspnea | 9.9 | 6.4 | 10.9 | 3.8 | 1.3 | 0.021 | 0.059 |
| Insomnia | 14.6 | 17.0 | 12.8 | 6.4 | 4.0 | 0.009 | 0.005 |
| Appetite loss | 18.7 | 9.2 | 10.3 | 1.3 | 1.3 | < 0.001 | 0.285 |
| Constipation | 18.1 | 7.1 | 10.3 | 5.8 | 5.3 | 0.006 | 0.066 |
| Diarrhea | 15.8 | 12.8 | 12.2 | 7.1 | 5.3 | 0.010 | 0.909 |
| Financial difficulties | 21.1 | 14.2 | 16.0 | 5.8 | 9.3 | < 0.001 | 0.115 |
| Sum | 147.3 | 98.6 | 98.9 | 44.9 | 40.7 | < 0.001 | 0.017 |
| Chemotherapy | 0 | 18 (38.3) | 18 (34.6) | 1 (1.9) | 0 | NA | NA |
| FOLFOX | 0 | 17 (36.2) | 17 (32.7) | 1 (1.9) | 0 | NA | NA |
| FL | 0 | 1 (2.1) | 1 (1.9) | 0 | 0 | NA | NA |
Most of the bowel functions showed statistically significant improvement over time, while urgency persisted into the late period without significant change (Table 3 and Figure 1C). On the other hand, leakage was very rare throughout the study period. Furthermore, the use of defecation medications remained at a rate of around 10% for the entire period, and there was no significant difference between the follow-up time points. Analyzing the correlation between medication and bowel function, gas (P = 0.023) and fecal frequency (P < 0.001) were significantly increased in, and the bowel dysfunction group (P = 0.028) was more likely to have, patients taking medication.
| Preoperative (n = 57) | 3 mo (n = 47) | 6 mo (n = 52) | 12 mo (n = 52) | 18 mo (n = 25) | P value1 | P value2 | |
| Gas | 3.6 | 3.1 | 2.3 | 1.6 | 0.8 | < 0.001 | 0.023 |
| Leakage | 0.4 | 0.2 | 0.2 | 0.1 | 0 | 0.025 | 0.691 |
| Frequency | 1.7 | 1.8 | 1.2 | 1.3 | 0.5 | 0.014 | < 0.001 |
| Fragmentation | 2.9 | 2.2 | 2.2 | 1.4 | 1.2 | 0.037 | 0.858 |
| Urgency | 3.8 | 2.6 | 3.9 | 2.4 | 2.0 | 0.217 | 0.532 |
| Score | 12.4 | 10.0 | 9.9 | 6.8 | 4.5 | < 0.001 | 0.053 |
| Dysfunction group | 0.014 | 0.028 | |||||
| No | 44 (77.2) | 41 (87.2) | 43 (82.7) | 47 (90.4) | 24 (96.0) | ||
| Minor | 5 (8.8) | 4 (8.5) | 4 (7.7) | 3 (5.8) | 1 (4.0) | ||
| Major | 8 (14.0) | 2 (4.3) | 5 (9.6) | 2 (3.8) | 0 | ||
| Medicine | 5 (8.8) | 6 (12.8) | 6 (11.5) | 5 (9.6) | 2 (8.0) | 0.882 | |
| Antidiarrheal agent | 1 (1.8) | 2 (4.3) | 1 (1.9) | 1 (1.9) | 0 | 0.558 | |
| Bulking agent | 0 | 2 (4.3) | 1 (1.9) | 1 (1.9) | 2 (8.0) | 0.161 | |
| Stool softener | 3 (5.3) | 4 (8.5) | 4 (7.7) | 1 (1.9) | 2 (8.0) | 0.764 | |
| Other | 1 (1.8) | 0 | 0 | 3 (5.8) | 0 | 0.447 |
When analyzing the correlation between QOL and bowel function, most bowel symptoms except leakage adversely affected most functional and symptom scales (Table 4). Meanwhile, emotional and social functions were found to be associated with most bowel symptoms. In analyzing the factors relating to bowel function, gas was associated with resected colon length (P = 0.032) and disease stage (P = 0.013). In addition, leakage was related to body mass index (P = 0.005) and colon length (P = 0.011). Frequency was related to sex (P = 0.002), and the bowel score was related to disease stage (P = 0.020).
| Gas | Leakage | Frequency | Fragmentation | Urgency | Bowel score | Dysfunction group | ||||||||
| CC | P value | CC | P value | CC | P value | CC | P value | CC | P value | CC | P value | CC | P value | |
| Global health status/QOL | ||||||||||||||
| -0.138 | 0.035 | -0.091 | 0.165 | -0.129 | 0.049 | -0.090 | 0.170 | -0.095 | 0.150 | -0.166 | 0.011 | -0.145 | 0.027 | |
| Functional scales | ||||||||||||||
| Physical | -0.048 | 0.464 | 0.010 | 0.883 | -0.155 | 0.018 | -0.023 | 0.728 | -0.087 | 0.186 | -0.107 | 0.104 | -0.103 | 0.118 |
| Role | -0.027 | 0.679 | -0.052 | 0.433 | -0.197 | 0.003 | -0.011 | 0.870 | -0.085 | 0.195 | -0.108 | 0.099 | -0.067 | 0.306 |
| Emotional | -0.145 | 0.027 | -0.199 | 0.002 | -0.249 | < 0.001 | -0.194 | 0.003 | -0.193 | 0.003 | -0.301 | < 0.001 | -0.242 | < 0.001 |
| Cognitive | -0.067 | 0.306 | -0.041 | 0.529 | -0.193 | 0.003 | -0.168 | 0.010 | -0.176 | 0.007 | -0.234 | < 0.001 | -0.186 | 0.004 |
| Social | -0.220 | 0.001 | -0.170 | 0.009 | -0.026 | 0.695 | -0.150 | 0.022 | -0.156 | 0.017 | -0.233 | < 0.001 | -0.179 | 0.006 |
| Sum | -0.137 | 0.037 | -0.123 | 0.062 | -0.217 | 0.001 | -0.139 | 0.034 | -0.183 | 0.005 | -0.258 | < 0.001 | -0.203 | 0.002 |
| Symptom scales/items | ||||||||||||||
| FA | 0.025 | 0.704 | 0.007 | 0.918 | 0.138 | 0.035 | 0.194 | 0.003 | 0.261 | < 0.001 | 0.268 | < 0.001 | 0.213 | 0.001 |
| NV | 0.108 | 0.101 | -0.056 | 0.394 | 0.137 | 0.036 | 0.154 | 0.018 | 0.232 | < 0.001 | 0.254 | < 0.001 | 0.255 | < 0 .001 |
| PA | 0.159 | 0.015 | 0.090 | 0.172 | 0.133 | 0.042 | 0.056 | 0.396 | 0.118 | 0.073 | 0.173 | 0.008 | 0.138 | 0.036 |
| DY | 0.044 | 0.502 | -0.007 | 0.913 | -0.014 | 0.832 | -0.007 | 0.915 | 0.192 | 0.003 | 0.118 | 0.073 | 0.065 | 0.322 |
| SL | 0.096 | 0.143 | -0.007 | 0.915 | 0.117 | 0.074 | 0.152 | 0.021 | 0.308 | < 0.001 | 0.293 | < 0.001 | 0.207 | 0.002 |
| AP | 0.140 | 0.033 | -0.003 | 0.960 | 0.088 | 0.183 | -0.003 | 0.958 | 0.090 | 0.172 | 0.110 | 0.094 | 0.083 | 0.204 |
| CO | 0.098 | 0.135 | -0.605 | 0.325 | 0.404 | < 0.001 | 0.034 | 0.609 | 0.016 | 0.806 | 0.134 | 0.040 | 0.087 | 0.184 |
| DI | 0.048 | 0.463 | 0.356 | < 0.001 | -0.055 | 0.401 | 0.311 | < 0.001 | 0.355 | < 0.001 | 0.360 | < 0.001 | 0.368 | < 0.001 |
| FI | 0.168 | 0.010 | 0.076 | 0.247 | 0.070 | 0.291 | 0.089 | 0.173 | 0.095 | 0.148 | 0.161 | 0.014 | 0.118 | 0.073 |
| Sum | 0.165 | 0.011 | 0.080 | 0.224 | 0.196 | 0.003 | 0.184 | 0.005 | 0.306 | < 0.001 | 0.349 | < 0.001 | 0.282 | < 0.001 |
When we analyzed the risk factors affecting the bowel dysfunction group, while there was no significant effect noted at other times, univariate analysis at six months showed that the resected bowel length [odd ratio (OR): 1.095, P = 0.026] and colon length (OR: 1.147, P = 0.031) were significantly different between the bowel dysfunction group (both minor and major) and the no bowel dysfunction group (Table 5). Multivariate analysis failed to identify any significant risk factors.
| Reference | Univariate | Multivariate | ||
| P value | OR | P value | OR | |
| Age (yr) | 0.826 | 1.008 | ||
| Sex (male) | 0.229 | 0.396 | ||
| Body mass index (kg/m2) | 0.325 | 1.108 | ||
| Lesion | 0.769 | - | ||
| Operation type (laparoscopy) | 1.000 | 3.462 | ||
| Operation name (right hemicolectomy) | 0.536 | 0.568 | ||
| Resected bowel length (cm) | 0.026 | 1.095 | 0.297 | 1.093 |
| Colon | 0.031 | 1.147 | 0.415 | 1.048 |
| Ileum | 0.386 | 1.048 | ||
| Preoperative obstruction (no) | 0.938 | - | ||
| Stage | 0.980 | - | ||
In our study, the scores for most QOL scales and bowel functions tended to improve over time after surgery. There were many relationships noted between QOL and bowel functions, and it was found that various factors such as resected bowel length and colon length influence bowel function. Despite D3 lymphadenectomy for right-sided colon adenocarcinoma, bowel function did not seem to be a big problem in most patients who underwent right-sided colectomy using a minimally invasive approach.
Unlike in the East, especially South Korea and Japan, which routinely perform D3 lymphadenectomy during colectomy, extensive mesocolic dissection has been increasing in the West only since Hohenberger et al[18] introduced the concept of CME. At the same time, concerns about bowel dysfunction caused by nerve injury have also increased in the West. According to Thorsen et al[20], when performing right colectomy with D3 lymphadenectomy, small bowel denervation may occur due to superior mesenteric nerve plexus transection, which may result in increased bowel frequency. However, bowel dysfunction was not an important issue after colonic surgery in the East, especially right-side colectomy. Bertelsen et al[21] also noted that CME did not increase the degree of bowel dysfunction when compared to conventional surgery.
In our study, most of the bowel functions gradually improved over time, but differences in symptoms were observed. Leakage rarely appeared in the period, probably due to the use of right-sided colectomy. In general, leakage symptoms are more problematic in patients undergoing rectal surgery or left-sided colectomy. Theodoropoulos et al[23] reported that uncontrolled stool was more severe in patients who underwent left colectomy or low anterior resection than in patients who underwent right colectomy. In our study, on the other hand, urgency was high throughout the period and did not improve significantly over time. In addition, the symptom of urgency adversely affected most functional and symptom scores in the QOL evaluation. Bertelsen et al[21] also reported an urgency of 35.3% to 37.4% in patients who received right-sided colectomy; however, there have been no reports on how the severity or nature of this symptom changes over time.
When we surveyed patients about their use of medication for defecation problems, approximately 10% of all study participants were taking medications. Very few studies have reported the use of medications in patients who have undergone right-sided colectomy[14,20,21]. As shown in our study, medication rates were not high. However, since the ratio remained constant over the entire period, it is worth noting the fact that 10% of patients experienced bowel function that was consistently poor after right-sided colectomy. According to the results in our study, bowel function has a significant effect on the QOL of patients, especially emotional and social functions. Therefore, the active management of bowel function may help improve patient QOL scores.
Upon comparing the bowel dysfunction group to the no bowel dysfunction group, it was found that the resected bowel and colon lengths were significantly different between these two populations only at six months. In general, the resected colonic length has not been considered to have a significant effect on bowel function, but it may have some effect on bowel function at a relatively early point during the postoperative period[13]. The overall analysis of factors affecting bowel symptoms showed that resected bowel length, especially colonic length, was also associated with leakage. This colon length is thought to reduce the bowel capacity.
To date, the best tool for evaluating bowel function after right-sided colectomy has not been established. Other previous studies used Wexner scores, the Bristol stool scale, or some of the symptom items in EORTC QLQ-C30[3,21,23]. However, because the Wexner score is based on fecal incontinence and frequency only, and the Bristol stool scale evaluates only the hardness of the stool, their use is limited in fully representing all symptoms that the patient may report. The bowel score that we used is primarily a tool for measuring bowel habit changes after low anterior resection, and we also questioned whether it could be used to measure bowel function after right-sided colectomy. However, this approach seems to have more advantages in expressing a function, and it can be applied to right-sided colectomy. In addition to the score, our study supplemented the examination of the stool status with the symptom scale of the EORTC QLQ-C30, which evaluates factors such as constipation and diarrhea.
Our study has some limitations that should be considered. First, the maximum number of patients was 57, and follow-up for more than 18 mo was performed in only about half of this population. This is because our institution does not routinely distribute a questionnaire on functions, and we enrolled patients for a limited period of time and only followed up after that. In our study, many QOL scores tended to worsen again in the analysis performed at 18 mo, possibly due to the small number of patients who were followed up to this time point. If the follow-up period were longer, reanalysis may yield new long-term results. In addition, there was no survey immediately after surgery, so comparisons based on that time point were not possible. A second disadvantage of this study is that there was no comparison group, because of course, D3 lymphadenectomy has been conducted in Korea. Furthermore, only patients who had minimally invasive surgery were included in our study, because our institution is a very specialized hospital for laparoscopic and robotic colorectal surgery. Third, the bowel score as the tool to measure bowel function is not commonly used after right colectomy, and other scores such as the Bristol stool scale have not been measured together. Finally, medication use was not controlled due to the fact that this was a cohort study, so that potentially confounding effect could not be entirely eliminated. However, given the situation of there being very few studies on bowel functions after right-sided colectomy with D3 lymphadenectomy, our study may be of importance with many implications that could be incorporated into or considered in future investigations.
In conclusion, about 10% of patients were in constant need of medication after right-sided colectomy, and most bowel symptoms improved over time. Even with D3 lymphadenectomy for right-sided colon adenocarcinoma, patients receiving right-sided colectomy using a minimally invasive approach should not experience major bowel dysfunction.
Compared with bowel habit changes that occur after rectal resection or left-sided colectomy, bowel dysfunctions seen after right-sided colectomy are relatively mild and temporary and have not traditionally been considered a significant issue.
Since the concept of complete mesocolic excision has been introduced, suggesting that the risk of bowel dysfunction due to superior mesenteric nerve plexus transection has increased. But not many studies have been published on the topic of bowel dysfunction after right-sided colectomy.
The main aim of this study was to evaluate the functional outcomes of patients who underwent right-sided colectomy with D3 lymphadenectomy for colon cancer.
Functional data from patients who underwent minimally invasive right-sided colectomy with D3 lymph node dissection for colon cancer were prospectively collected. Questionnaire responses were conducted preoperatively and 3, 6, 12, and 18 mo after the operation. The assessment of quality of life (QOL) used version 3 of the European Organization for Research and Treatment of Cancer Core QOL Questionnaire C30. Bowel function was evaluated for the items of gas, stool leakage, frequency, fragmentation, and urgency.
Most scales of quality of life and bowel function improved significantly over time. Urgency persisted to a high degree throughout the period without a significant change over time. The use of medications for defecation was about 10% over the entire period. In patients taking medication, gas and fecal frequency increased, and bowel dysfunction group was more common. At six months, resected bowel and colon lengths were significant risk factor for bowel dysfunction.
Even with D3 lymphadenectomy for right-sided colon adenocarcinoma, patients receiving right-sided colectomy using a minimally invasive approach should not experience major bowel dysfunction, and most bowel symptoms improved over time. About 10% of patients were in constant need of medication after right-sided colectomy continuously.
Larger samples, long-term follow-up study including comparison group is needed to complement our findings. It is also better to use a more suitable bowel score as the tool to measure bowel function after right colectomy.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Gao F, Milone M, Yu B S-Editor: Yan YP L-Editor: A P-Editor: Li JH
| 1. | Ho YH, Low D, Goh HS. Bowel function survey after segmental colorectal resections. Dis Colon Rectum. 1996;39:307-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 55] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 2. | Papa MZ, Karni T, Koller M, Klein E, Scott D, Bersuk D, Sareli M, Ben Ari G. Avoiding diarrhea after subtotal colectomy with primary anastomosis in the treatment of colon cancer. J Am Coll Surg. 1997;184:269-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 3. | Magdeburg J, Glatz N, Post S, Kienle P, Rickert A. Long-term functional outcome of colonic resections: how much does faecal impairment influence quality of life? Colorectal Dis. 2016;18:O405-O413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (1)] |
| 4. | Hinojosa MW, Konyalian VR, Murrell ZA, Varela JE, Stamos MJ, Nguyen NT. Outcomes of right and left colectomy at academic centers. Am Surg. 2007;73:945-948. [PubMed] |
| 5. | Masoomi H, Buchberg B, Dang P, Carmichael JC, Mills S, Stamos MJ. Outcomes of right vs. left colectomy for colon cancer. J Gastrointest Surg. 2011;15:2023-2028. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 50] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 6. | Kwaan MR, Al-Refaie WB, Parsons HM, Chow CJ, Rothenberger DA, Habermann EB. Are right-sided colectomy outcomes different from left-sided colectomy outcomes?: study of patients with colon cancer in the ACS NSQIP database. JAMA Surg. 2013;148:504-510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 79] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 7. | Kummer A, Slieker J, Grass F, Hahnloser D, Demartines N, Hübner M. Enhanced Recovery Pathway for Right and Left Colectomy: Comparison of Functional Recovery. World J Surg. 2016;40:2519-2527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 8. | Emmertsen KJ, Laurberg S. Low anterior resection syndrome score: development and validation of a symptom-based scoring system for bowel dysfunction after low anterior resection for rectal cancer. Ann Surg. 2012;255:922-928. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 549] [Cited by in RCA: 745] [Article Influence: 57.3] [Reference Citation Analysis (0)] |
| 9. | Bryant CL, Lunniss PJ, Knowles CH, Thaha MA, Chan CL. Anterior resection syndrome. Lancet Oncol. 2012;13:e403-e408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 344] [Cited by in RCA: 433] [Article Influence: 33.3] [Reference Citation Analysis (1)] |
| 10. | Levack MM, Savitt LR, Berger DL, Shellito PC, Hodin RA, Rattner DW, Goldberg SM, Bordeianou L. Sigmoidectomy syndrome? Patients' perspectives on the functional outcomes following surgery for diverticulitis. Dis Colon Rectum. 2012;55:10-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 62] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 11. | Martellucci J. Low Anterior Resection Syndrome: A Treatment Algorithm. Dis Colon Rectum. 2016;59:79-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 90] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 12. | Koda K, Yamazaki M, Shuto K, Kosugi C, Mori M, Narushima K, Hosokawa I, Shimizu H. Etiology and management of low anterior resection syndrome based on the normal defecation mechanism. Surg Today. 2019;49:803-808. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 13. | Luboshits J, Goldberg G, Chubadi R, Achiron A, Atsmon J, Hayslett JP, Lumbroso R, Povsner E, Halevy J. Functional adaptation of rat remnant colon after proximal hemicolectomy. Dig Dis Sci. 1992;37:175-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Yuan L, O'Grady G, Milne T, Jaung R, Vather R, Bissett IP. Prospective comparison of return of bowel function after left versus right colectomy. ANZ J Surg. 2018;88:E242-E247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 15. | Rees H, Markley MA, Kiely EM, Pierro A, Pritchard J. Diarrhea after resection of advanced abdominal neuroblastoma: a common management problem. Surgery. 1998;123:568-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Hirano S, Kondo S, Hara T, Ambo Y, Tanaka E, Shichinohe T, Suzuki O, Hazama K. Distal pancreatectomy with en bloc celiac axis resection for locally advanced pancreatic body cancer: long-term results. Ann Surg. 2007;246:46-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 255] [Cited by in RCA: 240] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 17. | Hirano S, Kondo S, Tanaka E, Shichinohe T, Tsuchikawa T, Kato K, Matsumoto J. Postoperative bowel function and nutritional status following distal pancreatectomy with en-bloc celiac axis resection. Dig Surg. 2010;27:212-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 18. | Hohenberger W, Weber K, Matzel K, Papadopoulos T, Merkel S. Standardized surgery for colonic cancer: complete mesocolic excision and central ligation--technical notes and outcome. Colorectal Dis. 2009;11:354-64; discussion 364-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 990] [Cited by in RCA: 1104] [Article Influence: 69.0] [Reference Citation Analysis (0)] |
| 19. | Fatima J, Houghton SG, Sarr MG. Development of a simple model of extrinsic denervation of the small bowel in mouse. J Gastrointest Surg. 2007;11:1052-1056. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 20. | Thorsen Y, Stimec B, Andersen SN, Lindstrom JC, Pfeffer F, Oresland T, Ignjatovic D; RCC study group. Bowel function and quality of life after superior mesenteric nerve plexus transection in right colectomy with D3 extended mesenterectomy. Tech Coloproctol. 2016;20:445-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 37] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 21. | Bertelsen CA, Larsen HM, Neuenschwander AU, Laurberg S, Kristensen B, Emmertsen KJ. Long-term Functional Outcome After Right-Sided Complete Mesocolic Excision Compared With Conventional Colon Cancer Surgery: A Population-Based Questionnaire Study. Dis Colon Rectum. 2018;61:1063-1072. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 22. | Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, Filiberti A, Flechtner H, Fleishman SB, de Haes JC. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9802] [Cited by in RCA: 11453] [Article Influence: 357.9] [Reference Citation Analysis (0)] |
| 23. | Theodoropoulos GE, Papanikolaou IG, Karantanos T, Zografos G. Post-colectomy assessment of gastrointestinal function: a prospective study on colorectal cancer patients. Tech Coloproctol. 2013;17:525-536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |