Published online Jun 28, 2020. doi: 10.3748/wjg.v26.i24.3421
Peer-review started: March 11, 2020
First decision: April 25, 2020
Revised: May 6, 2020
Accepted: May 29, 2020
Article in press: May 29, 2020
Published online: June 28, 2020
Processing time: 108 Days and 19.7 Hours
The number of liver cancer patients is likely to continue to increase in the coming decades due to the aging of the population and changing risk factors. Traditional treatments cannot meet the needs of all patients. New treatment methods evolved from pulsed electric field ablation are expected to lead to breakthroughs in the treatment of liver cancer. This paper reviews the safety and efficacy of irreversible electroporation in clinical studies, the methods to detect and evaluate its ablation effect, the improvements in equipment and its antitumor effect, and animal and clinical trials on electrochemotherapy. We also summarize studies on the most novel nanosecond pulsed electric field ablation techniques in vitro and in vivo. These research results are certain to promote the progress of pulsed electric field in the treatment of liver cancer.
Core tip: The economic burden of liver cancer worldwide remains great. As a new therapeutic method, pulsed electric field ablation has revolutionized the treatment of liver cancer since this method is different from traditional thermal ablation. We focus on the safety of irreversible electroporation in the clinical treatment of liver cancer and the evaluation of imaging technology. We also review preclinical studies of electrochemotherapy and nanosecond pulsed electric field for liver cancer.
- Citation: Liu ZG, Chen XH, Yu ZJ, Lv J, Ren ZG. Recent progress in pulsed electric field ablation for liver cancer. World J Gastroenterol 2020; 26(24): 3421-3431
- URL: https://www.wjgnet.com/1007-9327/full/v26/i24/3421.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i24.3421
Over the last couple of decades, the total number of liver cancer cases has been increasing as the population ages and grows[1]. During the next decade, further increases in the number of new cases of primary liver cancer is predicted each year in most studied countries as a result of changes in risk factors[2]. However, the global hepatocellular carcinoma (HCC) burden can be reduced by administering universal hepatitis B virus vaccinations, avoiding environmental and lifestyle risk factors, and broadly implementing HCC surveillance in high-risk patients[3]. Biannual liver ultrasonography (US) is recommended for patients with cirrhosis because these examinations increase the detection rate of very early HCCs for which effective therapies are feasible[4].
On account of involving a complex decision-making process, HCC management requires a multidisciplinary approach to achieve the best outcome[5]. Patients with early-stage HCC may be treated by surgical resection, liver transplantation, and percutaneous ablation[6]. Surgical resection was previously recommended as the first-line choice for radical treatment, but almost 70% of patients who underwent surgical resection developed recurrent HCC[7]. Although liver transplantation is the best treatment option for HCC, the shortage of available organ donors is the main limiting factor[8]. Percutaneous ablation includes radiofrequency ablation, microwave ablation, cryoablation, and percutaneous ethanol injection, which have evolved considerably over the past 20 years, enabling treatment of an increasing number of patients[6]. Classical monopolar radiofrequency ablation (RFA) possibly has the same therapeutic effect as surgical resection for HCC tumors less than 2–3 cm developing on cirrhotic liver, but the outcomes are still affected by local and distant tumor recurrence[9]. The therapeutic response to RFA is limited for tumors larger than 2 to 3 cm, as well as for tumors located near a major vessel[10]. Since microwave ablation heats up more rapidly and reaches a higher temperature than RFA, this method seems to be an alternative to monopolar RFA for HCC tumors less than 3 cm, especially for multiple HCC tumors[9]. In first-generation cryoablation devices, there is an increased rate of adverse events after ablation compared to that after RFA[11]. Ethanol injection still has a role in high-resource countries for tumor nodules less than 2 cm adjacent to large intrahepatic vessels or bile ducts[12].
Pulsed electric field ablation for liver cancer is a novel ablation modality based on short electric pulses inducing important nonthermal changes in cell physiology. Pulsed electric field ablation for liver cancer mainly encompasses three techniques, including electrochemotherapy (ECT), nanosecond pulsed electric fields (nsPEFs), and irreversible electroporation (IRE). By summarizing the latest advances in different types of pulsed electric field ablation, we hope to promote the study of pulsed electric fields for the treatment of liver cancer.
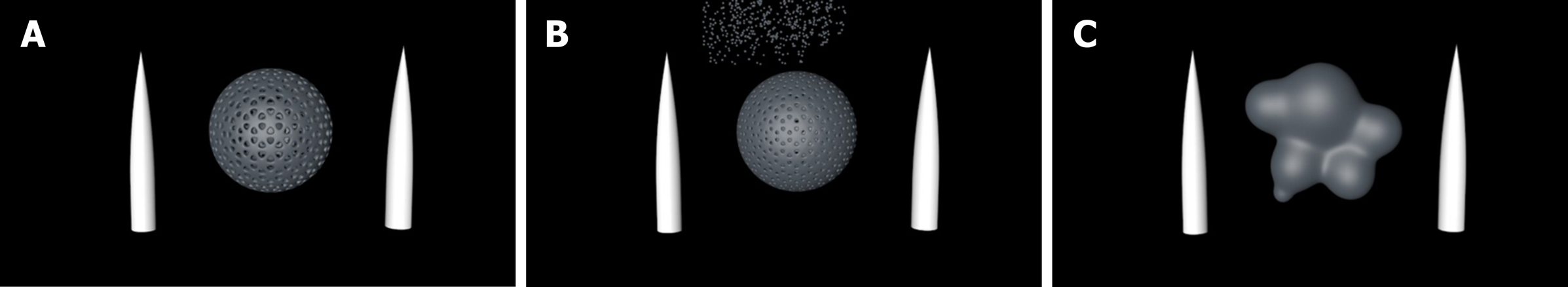
IRE is a nonthermal ablative method that delivers 1-3 kV/cm electric pulses with a pulse width of a millisecond between two electrodes and causes irreversible damage to cells by inducing definitive pores across the cellular membrane[13], while sparing the tissue scaffold, large blood vessels, and other tissue structures (Figure 1A)[14]. Thus, IRE has been used as an adequate method for the treatment of HCC in cases where traditional methods are unsuitable or deemed to have a high risk for complications[15].
During the last decade, an increasing number of clinical studies from different countries and regions have evaluated the safety and efficacy of IRE ablation for liver tumors (Table 1). A recent study from Southeast Asia was conducted by Kalra et al[16] on 21 patients with unresectable HCC. Although the study reported a higher incidence of complications (42.9%), they were mostly mild and did not require additional treatment. Moreover, the investigators found that nodule size (< 25 mm, P = 0.045) was the only factor that significantly affected local tumor progression-free survival[16]. However, Sutter et al[17] found that only the serum α-fetoprotein level (200 ng/mL) (P = 0.0004) was correlated with overall tumor progression-free survival. The authors believe that this finding highlights the impact of aggressive growth on cancer treatment[17]. As the largest United Kingdom series on IRE, a bi-institutional review suggests that IRE can be a useful tool for lesions < 2 cm in size, especially HCC. However, the main limitations of the study include its retrospective design, insufficient sample size, and heterogeneous group of patients with multiple pathologies[18]. Similarly, a study designed in a prospective setting in Japan suggested that after image-guided percutaneous IRE treatment, patients with small HCCs can achieve good local disease control. The reason for the presence of a residual tumor in one (17%) of the six patients with HCCs may be the anatomically unfavorable location of the lesion, inaccurate evaluation performed immediately postoperatively, and strict needle placement requirements[19].
| Ref. | Design | Number of patients (lesions) | Tumor type | Tumor size (mm) | Primary efficacy % | Complications | Local recurrence |
| Kalra et al[16] | Retrospective study | 21 (21) | 21 HCC | 26 (14-40) | 100% | 42.9% No major complications | 24% |
| Mafeld et al[18] | Bi-institutional retrospective study | 52 (59) | 20 HCC; 3 cholangiocellular carcinoma; 33 metastatic disease | 24 (7-52) | 75% | 17% | Not reported |
| Sugimoto et al[19] | Prospective study | 5 (6) | 6 HCC | 17.5 (11.2-23.8) | 83% | No serious complications | Not reported |
| Distelmaier et al[24] | Longitudinal observational diagnostic study | 29 (43) | 4 HCC; 39 others | 6.4 (mL) | 93% | Needle tract seeding in 26%, local heating to bile ducts in 24% | 5% |
| Sutter et al[17] | Retrospective single-center study | 58 (75) | 75 HCC | 24 (6-90) | 77.3% (the first time); 89.35 (the second time); 92% (the third time) | 19% | Not reported |
| Frühling et al[20] | Single-center nonrandomized clinical study | 30 (38) | 23 CRLM; 8 HCC; 7 others | 24 (0.8–4.0) | 78.9% at 3 mo; 65.8% at 6 mo | 20.0% minor, 3.3% major complications | 21.1% at 3 mo; 34.2% at 6 mo |
| Niessen et al[88] | Prospective, single-center study | 34 (65) | 33 HCC; 22 CRLM; 10 others | 24 ± 14 (2-71) | 94.5% | 15.71% minor, 11.79% major complication | 13.84% |
| Eller et al[89] | Prospective study | 14 (18) | 5 HCC; 11 CRLM; 2 others | 20 (11-37) | 86% | 29% | 17% |
| Cannon et al[90] | Prospective study | 44 (48) | 14 HCC; 20 CRLM; 10 others | HCC 2.1 (1.3–4.5); CRLM 2.7 (1.2–11); other 2.5 (1.1–5.0) | 100% | 11.36% (with all complications resolving within 30 d) | Not reported |
Likewise, in a single-center nonrandomized clinical trial, HCC was most controlled at 3 mo (0% recurrence) compared to colorectal liver metastasis (26.1% recurrence) and other metastases (28.6% recurrence), and smaller tumors can have a lower risk of recurrence[20]. A study by Alnaggar et al[21] pointed out that hepatic injury caused by IRE is transient and self-limiting in patients with HCC and can be monitored by serum transaminases and bilirubin values. Analogously, Froud et al[22] found that although there is a marked increase in liver enzymes after IRE ablation, most of the elevations were safe and self-limiting[22]. In a study evaluating the effect of IRE on vascular patency, only seven (4.4%) of 158 vessels showed abnormal changes. Statistical analysis showed that the presence or absence of vascular abnormalities may not be related to the distance to the ablation site[23]. Unfortunately, in a prospective multi-institution study by Distelmaier et al[24], although local recurrence was found in only two (5%) of the 40 patients with target tumors, needle tract seeding was observed in 27% of patients, and sufficient local heating to the bile ducts was discovered in 22% of patients[24].
A systematic evaluation showed that IRE had a complete response rate of 93% to 100% at 3 mo for HCCs less than 3 cm, with only minor complications during this period[25]. The relevant minor IRE-associated hepatic complications included arrhythmia, portal vein thrombosis, bile duct dilatation, and hepatic abscesses. Fortunately, the majority of these complications did not require further treatment[26]. For instance, vessel narrowing may occur acutely but without long-term sequelae[27]. In general, IRE is a safe and effective method for local ablation. As IRE has become increasingly and widely used in clinical practice, its effect will be further verified.
There have been many studies on the examination and evaluation of ablation effects in animal models. A study of a rodent hepatoma model confirmed that grayscale US, computed tomography (CT), and magnetic resonance imaging (MRI) can be used to distinguish the ablation area from the nonablated area after IRE[28]. All of these modalities, including contrast-enhanced ultrasound (CEUS), CT, and MRI, were able to accurately characterize the ablation effect over a follow-up period of several months[29]. In a study of Yorkshire pigs that compared the results of gross and histopathologic examinations and US, evaluating the hyperechoic rim that appeared 90–120 min after IRE ablation had the best accuracy (± 2 mm)[30]. Another study suggested that 60 to 120 min after IRE ablation would be a suitable time to evaluate the ablation area by US, and this study showed that the appropriate time for CEUS was 10 min after ablation[31]. Nonetheless, in a study on the ablation of normal porcine livers, Schmidt et al[32] found that changes detected by US within minutes of IRE (median, 20 min) were consistent with the area of eventual cellular necrosis[32]. In addition, since the hardness of liver tissue increases after IRE ablation, elastography can be used as an auxiliary means to B-mode US to further detect the ablation effect[33]. CEUS (r2 = 0.923, P < 0.0001) showed a better correlation with gross pathologic findings than B-mode US (r2 = 0.905, P < 0.0001)[34].
Although there is a good correlation between contrast-enhanced CT images and histopathology in pig liver models[35], a clinical study found that the normal appearance of enhanced CT images after IRE ablation may be confused with the typical characteristics of potential complications[36]. In a recent porcine liver model study, the three histopathological areas in the ablated area showed different MRI characteristics, and the hepatobiliary phase MRI scans showed the best evaluation ability[37]. Some clinical studies have found that after IRE ablation, MRI scans show large ablation areas that decrease with time[38] and can reflect the morphological and functional changes of the ablation areas[39]. One study suggested that the observation time after ablation should be delayed in the future because the pathological response after ablation in pig liver models lasted for at least 24 h[40]. There are also more novel detection methods that are expected to better reflect the ablation effect of IRE, such as fluorine 18 fluorodeoxyglucose positron emission tomography[41], diffusion-weighted imaging[42], and transcatheter intra-arterial perfusion-MRI[43].
Different tissue types and local environments will affect the ablation effect of IRE[44]. For example, the presence of metal stents in the ablation zone of tumor tissue can affect the temperature around the electrode and residual tissue, but the stents themselves do not significantly increase the temperature[45]. The presence of blood vessels in the ablation area can also lead to inadequate perivascular treatment, which can be prevented by injections of low-conductivity isotonic fluid into hepatic vessels[46].
IRE equipment needs to be continuously optimized and improved. For the electrode, the four-electrode array can satisfy the requirements of a larger ablation area within a clinically acceptable time[47]. The use of internally cooled bipolar applicators can reduce tissue temperature (by approximately 10 degrees Celsius) while maintaining good ablation results[48]. It is important to note that the surface temperature of the ordinary electrode will increase significantly, so care should be taken to keep important structures at a distance of 4 mm away from the electrode during ablation[49]. Also, stereotactic navigation and robotic assistance can place electrodes more accurately and quickly than conventional IRE methods while reducing the radiation dose[50,51]. As a novel IRE method, high-frequency irreversible electroporation (H-FIRE) can eliminate muscle contractions that occur during conventional IRE ablation[52,53]. The application of insulated needle electrodes in H-FIRE is expected to further reduce the occurrence of muscle contraction complications[54]. Moreover, the H-FIRE method combined with a single electrode and grounding pad has been demonstrated to be successful for hepatic tissue in vivo and can be helpful in situations when placing more than one electrode can be risky[55].
The effect of IRE ablation on the body's immune response has attracted attention. By ablating the livers of miniature pigs and mice, researchers found that two to seven days after IRE ablation, the abnormal Th2 status of animals with HCC was reversed to Th1 status, possibly promoting tumor elimination because the release of pro-inflammatory cytokines in the ablation area stimulated an immune response[56]. Furthermore, the serum output of HCC patients after ablation showed a sharp rise in macrophage migration inhibitory factor followed by a rapid decline, which may contribute to the repair of the ablation area[57]. Additionally, another experiment on IRE ablation in mice showed that the increase in inflammatory cells and cytokines in the IRE ablation area may not only cause tumorigenic effects on the body but also cause the body to generate an immune response[58]. Furthermore, injecting immunogenic adjuvant agents into the tumor before IRE or combining IRE with allogeneic natural killer cell immunotherapy can enhance the body's immune response, allowing for better control of the tumor[59,60].
ECT is a local treatment for solid tumors that applies short high-intensity pulsed electric fields to improve the transmembrane transfer of cytotoxic drugs (e.g., bleomycin and cisplatin) (Figure 1B)[61,62]. This technique can significantly improve the ability of chemotherapy drugs to kill cancer cells, especially bleomycin[63,64]. ECT has been widely used in the treatment of superficial skin tumors and is expected to play an active role in liver tumors.
The effects of ECT on HCC in animal models have been studied for more than 20 years. A study of a rat model of HCC found that the ECT group achieved a complete response rate of 69.2%, confirming the effectiveness of ECT in treating HCC[65]. In subsequent studies, good therapeutic effects were also observed in rabbits with transplanted liver tumors and rats with hepatic metastases of colorectal cancer[66,67]. Moreover, studies have shown that ECT does not cause significant damage to normal liver tissue outside the tumor[68] and may stimulate the body's immune system[69]. A recent study evaluated whether ECT caused damage to the large blood vessels and bile ducts of the liver through post-ablation liver histology and blood sample tests. Despite the insertion of electrodes into the hepatic vena cava, the researchers found no thrombosis and no significant damage to the blood vessels or bile ducts in the parenchyma. The study further confirmed the safety of ECT for normal liver tissue[70]. Furthermore, the safety of ECT was also verified by radiological findings[71]. Additionally, for tumor blood vessels, ECT can not only cause vasoconstriction in the short term like electroporation but can also further reduce blood flow in the long term. As HCC is a vascular cancer, this characteristic highlights the great potential of ECT as a treatment for HCC[72]. Clearly, the results of the study support the feasibility of using ECT as a modality for treating HCC.
The clinical application of ECT in the treatment of HCC has been limited. In the treatment of hepatic metastases of colorectal cancer with ECT, investigators found no serious complications associated with ECT either intraoperatively or postoperatively. In addition, pathological analysis showed that 9.9 ± 12.2% (AM ± SD) of the metastatic foci remained in the treatment group, and radiological results showed that 85% of the 27 metastatic foci had a complete response[73]. Another recent clinical study evaluated the safety and efficacy of ECT in the treatment of six patients with portal vein tumor thrombosis at the hepatic hilum, including three who had sustained thrombus reduction and two who had completely unblocked portal veins; none of these patients developed local recurrence[74]. Based on the previous positive results of ECT, Djokic et al[75] conducted a prospective study on ECT for HCC. The median size of the treated lesions was 24 mm (range 8-41 mm), and the lesions were located near the major hepatic vessels or peripherally. The results showed that at 3 to 6 mo, eight of ten patients achieved complete remission without serious treatment-related complications[75]. These three kinds of liver lesions were treated with ECT and good results were achieved, indicating that ECT could be applied to liver diseases.
With short pulse durations, nsPEF modulates cell signaling from the plasma membrane to intracellular structures and can affect cell functions[76]. nsPEF-induced apoptosis is independent of plasma membrane electroporation and thermal changes and occurs by recruiting intracellular and plasma membrane apoptosis signaling mechanisms (Figure 1C)[77].
The effects of nsPEFs on cells are multifold. After treating human HCC cells with different pulse parameters, He et al[78] observed changes in cell apoptosis morphology, mitochondrial membrane potential, intracellular calcium ion concentration, and key apoptotic factors and found that the mechanism of cell apoptosis might be a mitochondrial-dependent pathway[78]. In addition, Steuer et al[79] studied changes in cellular elasticity and tumorigenic properties of monolayer rat hepatic epithelial cells treated with nsPEFs. The results showed that the cell elasticity and cytoskeleton changed within 1 h after treatment. Fortunately, the cells did not develop the same malignant features as metastases[79]. Another study found that nsPEFs may temporarily inhibit WB-F344 cell communication by activating mitogen-activated protein kinase[80]. Moreover, by evaluating the electrical parameters, bioimpedance analyses can effectively detect changes in cell-cell contact and paracellular permeability[81]. Using CCK-8, FCM, JC-1, and fluorescent probes to detect the effects after treatment, a recent in vitro study examined the different effects of both nsPEFs and baicalin on hepatoma cells and hepatocytes. The results showed that almost all HCC cells in the nsPEFs treatment group died from necrosis, while most hepatocytes died from apoptosis. The combined treatment of nsPEFs and baicalin not only further enhanced the inhibitory effect of nsPEFs on HCC cells but also reduced the damaging effect of nsPEFs on liver cells[82]. The clinical application of this novel treatment may reduce the damage to normal tissues and enhance the ablation effect on tumor tissues.
In an animal study, Chen et al[83] induced tumor formation in C57BL/6 mice with hepal-6 HCC cells and then ablated tumor tissue with certain nsPEF parameters. The ultrasound results showed that the cure rate of HCC in mice was 75% and there was no recurrence within 9 mo. In addition, the immunohistochemical results suggest that nsPEF plays a role mainly by inducing apoptosis and inhibiting angiogenesis. The results provide a theoretical basis for nsPEFs in other preclinical and clinical studies. Encouragingly, in a nude mouse xenograft model using a highly metastatic HCC cell line, Yin et al[84] found that nsPEFs can inhibit tumor growth locally in a dose-dependent manner and reduce distant lung metastasis[84]. However, Chen et al[85] found that repeated pulse applications at small doses can increase the infiltration of tumor macrophages[85]. One study suggested that the mechanism of HCC apoptosis included an intrinsic apoptosis mechanism(s) and caspase-independent mechanisms. Notably, rats that had been treated with nsPEF ablation could not regrow tumors when reinjected with N1-S1 HCC cells.
Given the presence of immune cells and granzyme B-expressing cells after ablation, researchers believe that this finding is due to an acquired antitumor response[86]. Nuccitelli et al[87] demonstrated directly for the first time that nsPEF ablation could inhibit the growth of secondary tumors by triggering the production of CD8+ T-cells. The authors found that when CD8+ cytotoxic T-cells were present in the rats, the average size of the secondary tumor was 3% of the size of the primary tumor, and when CD8+ cytotoxic T-cells were absent, the second tumor was 54% of the size of the first tumor. Immunohistochemistry also confirmed the presence of large numbers of CD8+ T-cells in slow-growing secondary tumors. Furthermore, the researchers also found that the mice developed an immune response when injected with tumor cells treated with nsPEFs. The results remained the same even after the anti-CD8 antibodies were injected to deplete CD8+ T-cells[87]. The abovementioned studies undoubtedly confirmed the advantages of nsPEFs in the ablation of HCC.
At present, when used as palliative option for patients with HCC who cannot be treated with conventional therapies, IRE has increasingly shown positive clinical effects, especially for small HCC, as the operational and testing equipment has been updated. However, due to the lack of randomized controlled trials on thermal ablation technologies, the indications for IRE need to be explored and verified in more clinical studies[88-90]. In addition, further studies are needed to evaluate the possible immune effects. For HCC, ECT is a safe and effective approach in preclinical studies, but further validation is needed in clinical studies. As a new treatment method that can induce cell death in many ways and may stimulate the body to produce immune effects, nsPEFs show great potential in the treatment of HCC. However, we have not yet demonstrated the effectiveness of nsPEFs in clinical studies. In the future, to ensure the safety and effectiveness of the application of pulsed electric field ablation in the treatment of HCC, we need to further explore the immune efficacy that pulsed electric field ablation may have in the body.
We thank the associate editor and the reviewers for their useful feedback that improved this paper.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Marin JJG, Sartori S S-Editor: Zhang L L-Editor: Wang TQ E-Editor: Zhang YL
| 1. | Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, Brenner H, Dicker DJ, Chimed-Orchir O, Dandona R, Dandona L, Fleming T, Forouzanfar MH, Hancock J, Hay RJ, Hunter-Merrill R, Huynh C, Hosgood HD, Johnson CO, Jonas JB, Khubchandani J, Kumar GA, Kutz M, Lan Q, Larson HJ, Liang X, Lim SS, Lopez AD, MacIntyre MF, Marczak L, Marquez N, Mokdad AH, Pinho C, Pourmalek F, Salomon JA, Sanabria JR, Sandar L, Sartorius B, Schwartz SM, Shackelford KA, Shibuya K, Stanaway J, Steiner C, Sun J, Takahashi K, Vollset SE, Vos T, Wagner JA, Wang H, Westerman R, Zeeb H, Zoeckler L, Abd-Allah F, Ahmed MB, Alabed S, Alam NK, Aldhahri SF, Alem G, Alemayohu MA, Ali R, Al-Raddadi R, Amare A, Amoako Y, Artaman A, Asayesh H, Atnafu N, Awasthi A, Saleem HB, Barac A, Bedi N, Bensenor I, Berhane A, Bernabé E, Betsu B, Binagwaho A, Boneya D, Campos-Nonato I, Castañeda-Orjuela C, Catalá-López F, Chiang P, Chibueze C, Chitheer A, Choi JY, Cowie B, Damtew S, das Neves J, Dey S, Dharmaratne S, Dhillon P, Ding E, Driscoll T, Ekwueme D, Endries AY, Farvid M, Farzadfar F, Fernandes J, Fischer F, G/Hiwot TT, Gebru A, Gopalani S, Hailu A, Horino M, Horita N, Husseini A, Huybrechts I, Inoue M, Islami F, Jakovljevic M, James S, Javanbakht M, Jee SH, Kasaeian A, Kedir MS, Khader YS, Khang YH, Kim D, Leigh J, Linn S, Lunevicius R, El Razek HMA, Malekzadeh R, Malta DC, Marcenes W, Markos D, Melaku YA, Meles KG, Mendoza W, Mengiste DT, Meretoja TJ, Miller TR, Mohammad KA, Mohammadi A, Mohammed S, Moradi-Lakeh M, Nagel G, Nand D, Le Nguyen Q, Nolte S, Ogbo FA, Oladimeji KE, Oren E, Pa M, Park EK, Pereira DM, Plass D, Qorbani M, Radfar A, Rafay A, Rahman M, Rana SM, Søreide K, Satpathy M, Sawhney M, Sepanlou SG, Shaikh MA, She J, Shiue I, Shore HR, Shrime MG, So S, Soneji S, Stathopoulou V, Stroumpoulis K, Sufiyan MB, Sykes BL, Tabarés-Seisdedos R, Tadese F, Tedla BA, Tessema GA, Thakur JS, Tran BX, Ukwaja KN, Uzochukwu BSC, Vlassov VV, Weiderpass E, Wubshet Terefe M, Yebyo HG, Yimam HH, Yonemoto N, Younis MZ, Yu C, Zaidi Z, Zaki MES, Zenebe ZM, Murray CJL, Naghavi M. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-years for 32 Cancer Groups, 1990 to 2015: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol. 2017;3:524-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2838] [Cited by in RCA: 2950] [Article Influence: 368.8] [Reference Citation Analysis (0)] |
| 2. | Valery PC, Laversanne M, Clark PJ, Petrick JL, McGlynn KA, Bray F. Projections of primary liver cancer to 2030 in 30 countries worldwide. Hepatology. 2018;67:600-611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 233] [Article Influence: 33.3] [Reference Citation Analysis (0)] |
| 3. | Yang JD, Hainaut P, Gores GJ, Amadou A, Plymoth A, Roberts LR. A global view of hepatocellular carcinoma: trends, risk, prevention and management. Nat Rev Gastroenterol Hepatol. 2019;16:589-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2184] [Cited by in RCA: 2880] [Article Influence: 480.0] [Reference Citation Analysis (17)] |
| 4. | Santi V, Trevisani F, Gramenzi A, Grignaschi A, Mirici-Cappa F, Del Poggio P, Di Nolfo MA, Benvegnù L, Farinati F, Zoli M, Giannini EG, Borzio F, Caturelli E, Chiaramonte M, Bernardi M; Italian Liver Cancer (ITA. LI.CA) Group. Semiannual surveillance is superior to annual surveillance for the detection of early hepatocellular carcinoma and patient survival. J Hepatol. 2010;53:291-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 210] [Cited by in RCA: 237] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 5. | Serper M, Taddei TH, Mehta R, D'Addeo K, Dai F, Aytaman A, Baytarian M, Fox R, Hunt K, Goldberg DS, Valderrama A, Kaplan DE; VOCAL Study Group. Association of Provider Specialty and Multidisciplinary Care With Hepatocellular Carcinoma Treatment and Mortality. Gastroenterology. 2017;152:1954-1964. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 196] [Article Influence: 24.5] [Reference Citation Analysis (0)] |
| 6. | Breen DJ, Lencioni R. Image-guided ablation of primary liver and renal tumours. Nat Rev Clin Oncol. 2015;12:175-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 70] [Article Influence: 7.0] [Reference Citation Analysis (1)] |
| 7. | Tabrizian P, Jibara G, Shrager B, Schwartz M, Roayaie S. Recurrence of hepatocellular cancer after resection: patterns, treatments, and prognosis. Ann Surg. 2015;261:947-955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 345] [Cited by in RCA: 653] [Article Influence: 65.3] [Reference Citation Analysis (0)] |
| 8. | Sapisochin G, Bruix J. Liver transplantation for hepatocellular carcinoma: outcomes and novel surgical approaches. Nat Rev Gastroenterol Hepatol. 2017;14:203-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 221] [Cited by in RCA: 331] [Article Influence: 41.4] [Reference Citation Analysis (0)] |
| 9. | Nault JC, Sutter O, Nahon P, Ganne-Carrié N, Séror O. Percutaneous treatment of hepatocellular carcinoma: State of the art and innovations. J Hepatol. 2018;68:783-797. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 282] [Article Influence: 40.3] [Reference Citation Analysis (0)] |
| 10. | Kang TW, Lim HK, Lee MW, Kim YS, Rhim H, Lee WJ, Gwak GY, Paik YH, Lim HY, Kim MJ. Aggressive Intrasegmental Recurrence of Hepatocellular Carcinoma after Radiofrequency Ablation: Risk Factors and Clinical Significance. Radiology. 2015;276:274-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 106] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 11. | Wu S, Hou J, Ding Y, Wu F, Hu Y, Jiang Q, Mao P, Yang Y. Cryoablation Versus Radiofrequency Ablation for Hepatic Malignancies: A Systematic Review and Literature-Based Analysis. Medicine (Baltimore). 2015;94:e2252. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 12. | Forner A, Reig M, Bruix J. Hepatocellular carcinoma. Lancet. 2018;391:1301-1314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2800] [Cited by in RCA: 4079] [Article Influence: 582.7] [Reference Citation Analysis (6)] |
| 13. | Seror O. Ablative therapies: Advantages and disadvantages of radiofrequency, cryotherapy, microwave and electroporation methods, or how to choose the right method for an individual patient? Diagn Interv Imaging. 2015;96:617-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 67] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 14. | Maor E, Ivorra A, Leor J, Rubinsky B. The effect of irreversible electroporation on blood vessels. Technol Cancer Res Treat. 2007;6:307-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 235] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 15. | Kourounis G, Paul Tabet P, Moris D, Papalambros A, Felekouras E, Georgiades F, Astras G, Petrou A. Irreversible electroporation (Nanoknife® treatment) in the field of hepatobiliary surgery: Current status and future perspectives. J BUON. 2017;22:141-149. [PubMed] |
| 16. | Kalra N, Gupta P, Gorsi U, Bhujade H, Chaluvashetty SB, Duseja A, Singh V, Dhiman RK, Chawla YK, Khandelwal N. Irreversible Electroporation for Unresectable Hepatocellular Carcinoma: Initial Experience. Cardiovasc Intervent Radiol. 2019;42:584-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 46] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 17. | Sutter O, Calvo J, N'Kontchou G, Nault JC, Ourabia R, Nahon P, Ganne-Carrié N, Bourcier V, Zentar N, Bouhafs F, Sellier N, Diallo A, Seror O. Safety and Efficacy of Irreversible Electroporation for the Treatment of Hepatocellular Carcinoma Not Amenable to Thermal Ablation Techniques: A Retrospective Single-Center Case Series. Radiology. 2017;284:877-886. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 111] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 18. | Mafeld S, Wong JJ, Kibriya N, Stenberg B, Manas D, Bassett P, Aslam T, Evans J, Littler P. Percutaneous Irreversible Electroporation (IRE) of Hepatic Malignancy: A Bi-institutional Analysis of Safety and Outcomes. Cardiovasc Intervent Radiol. 2019;42:577-583. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 37] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 19. | Sugimoto K, Moriyasu F, Kobayashi Y, Saito K, Takeuchi H, Ogawa S, Ando M, Sano T, Mori T, Furuichi Y, Nakamura I. Irreversible electroporation for nonthermal tumor ablation in patients with hepatocellular carcinoma: initial clinical experience in Japan. Jpn J Radiol. 2015;33:424-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 40] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 20. | Frühling P, Nilsson A, Duraj F, Haglund U, Norén A. Single-center nonrandomized clinical trial to assess the safety and efficacy of irreversible electroporation (IRE) ablation of liver tumors in humans: Short to mid-term results. Eur J Surg Oncol. 2017;43:751-757. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 57] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 21. | Alnaggar M, Qaid AM, Chen J, Niu L, Xu K. Irreversible electroporation of malignant liver tumors: Effect on laboratory values. Oncol Lett. 2018;16:3881-3888. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 22. | Froud T, Venkat SR, Barbery KJ, Gunjan A, Narayanan G. Liver Function Tests Following Irreversible Electroporation of Liver Tumors: Experience in 174 Procedures. Tech Vasc Interv Radiol. 2015;18:140-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Narayanan G, Bhatia S, Echenique A, Suthar R, Barbery K, Yrizarry J. Vessel patency post irreversible electroporation. Cardiovasc Intervent Radiol. 2014;37:1523-1529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 90] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 24. | Distelmaier M, Barabasch A, Heil P, Kraemer NA, Isfort P, Keil S, Kuhl CK, Bruners P. Midterm Safety and Efficacy of Irreversible Electroporation of Malignant Liver Tumors Located Close to Major Portal or Hepatic Veins. Radiology. 2017;285:1023-1031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 72] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 25. | Scheffer HJ, Nielsen K, de Jong MC, van Tilborg AA, Vieveen JM, Bouwman AR, Meijer S, van Kuijk C, van den Tol PM, Meijerink MR. Irreversible electroporation for nonthermal tumor ablation in the clinical setting: a systematic review of safety and efficacy. J Vasc Interv Radiol. 2014;25:997-1011; quiz 1011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 339] [Cited by in RCA: 279] [Article Influence: 25.4] [Reference Citation Analysis (0)] |
| 26. | Wu LM, Zhang LL, Chen XH, Zheng SS. Is irreversible electroporation safe and effective in the treatment of hepatobiliary and pancreatic cancers? Hepatobiliary Pancreat Dis Int. 2019;18:117-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 27. | Lee YJ, Lu DS, Osuagwu F, Lassman C. Irreversible electroporation in porcine liver: short- and long-term effect on the hepatic veins and adjacent tissue by CT with pathological correlation. Invest Radiol. 2012;47:671-675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 28. | Zhang Y, White SB, Nicolai JR, Zhang Z, West DL, Kim DH, Goodwin AL, Miller FH, Omary RA, Larson AC. Multimodality imaging to assess immediate response to irreversible electroporation in a rat liver tumor model. Radiology. 2014;271:721-729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 29. | Granata V, de Lutio di Castelguidone E, Fusco R, Catalano O, Piccirillo M, Palaia R, Izzo F, Gallipoli AD, Petrillo A. Irreversible electroporation of hepatocellular carcinoma: preliminary report on the diagnostic accuracy of magnetic resonance, computer tomography, and contrast-enhanced ultrasound in evaluation of the ablated area. Radiol Med. 2016;121:122-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 42] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 30. | Appelbaum L, Ben-David E, Sosna J, Nissenbaum Y, Goldberg SN. US findings after irreversible electroporation ablation: radiologic-pathologic correlation. Radiology. 2012;262:117-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 70] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 31. | Lin MX, Kuang M, Xu M, Zhuang BW, Tian WS, Ye JY, Xie XH, Xie XY. Ultrasound and Contrast-Enhanced Ultrasound for Evaluation of Irreversible Electroporation Ablation: In Vivo Proof of Concept in Normal Porcine Liver. Ultrasound Med Biol. 2016;42:2639-2649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 32. | Schmidt CR, Shires P, Mootoo M. Real-time ultrasound imaging of irreversible electroporation in a porcine liver model adequately characterizes the zone of cellular necrosis. HPB (Oxford). 2012;14:98-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 33. | Au JT, Kingham TP, Jun K, Haddad D, Gholami S, Mojica K, Monette S, Ezell P, Fong Y. Irreversible electroporation ablation of the liver can be detected with ultrasound B-mode and elastography. Surgery. 2013;153:787-793. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 34. | Sugimoto K, Moriyasu F, Kobayashi Y, Kasuya K, Nagakawa Y, Tsuchida A, Hara T, Iobe H, Oshiro H. Assessment of various types of US findings after irreversible electroporation in porcine liver: comparison with radiofrequency ablation. J Vasc Interv Radiol. 2015;26:279-87.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 35. | Lee YJ, Lu DS, Osuagwu F, Lassman C. Irreversible electroporation in porcine liver: acute computed tomography appearance of ablation zone with histopathologic correlation. J Comput Assist Tomogr. 2013;37:154-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 36. | Dollinger M, Jung EM, Beyer L, Niessen C, Scheer F, Müller-Wille R, Stroszczynski C, Wiggermann P. Irreversible electroporation ablation of malignant hepatic tumors: subacute and follow-up CT appearance of ablation zones. J Vasc Interv Radiol. 2014;25:1589-1594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 37. | Felker ER, Dregely I, Chung DJ, Sung K, Osuagwu FC, Lassman C, Sayre J, Wu H, Lu DS. Irreversible Electroporation: Defining the MRI Appearance of the Ablation Zone With Histopathologic Correlation in a Porcine Liver Model. AJR Am J Roentgenol. 2017;208:1141-1146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 38. | Padia SA, Johnson GE, Yeung RS, Park JO, Hippe DS, Kogut MJ. Irreversible Electroporation in Patients with Hepatocellular Carcinoma: Immediate versus Delayed Findings at MR Imaging. Radiology. 2016;278:285-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 37] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 39. | Granata V, Fusco R, Catalano O, Piccirillo M, De Bellis M, Izzo F, Petrillo A. Percutaneous ablation therapy of hepatocellular carcinoma with irreversible electroporation: MRI findings. AJR Am J Roentgenol. 2015;204:1000-1007. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 40] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 40. | Vogel JA, van Veldhuisen E, Alles LK, Busch OR, Dijk F, van Gulik TM, Huijzer GM, Besselink MG, van Lienden KP, Verheij J. Time-Dependent Impact of Irreversible Electroporation on Pathology and Ablation Size in the Porcine Liver: A 24-Hour Experimental Study. Technol Cancer Res Treat. 2019;18:1533033819876899. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 41. | Wang X, Su Z, Lyu T, Figini M, Procissi D, Shangguan J, Sun C, Wang B, Shang N, Gu S, Ma Q, Gordon AC, Lin K, Wang J, Lewandowski RJ, Salem R, Yaghmai V, Larson AC, Zhang Z. 18F-FDG PET Biomarkers Help Detect Early Metabolic Response to Irreversible Electroporation and Predict Therapeutic Outcomes in a Rat Liver Tumor Model. Radiology. 2018;287:137-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 42. | Hu S, Sun C, Wang B, Zhou K, Pan L, Shangguan J, Yang J, Yaghmai V, Figini M, Zhang Z. Diffusion-Weighted MR Imaging to Evaluate Immediate Response to Irreversible Electroporation in a Rabbit VX2 Liver Tumor Model. J Vasc Interv Radiol. 2019;30:1863-1869. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 43. | Figini M, Zhou K, Pan L, Sun C, Wang B, Hu S, Yang J, Shangguan J, Eresen A, Velichko Y, Yaghmai V, Zhang Z. Transcatheter intra-arterial perfusion (TRIP)-MRI biomarkers help detect immediate response to irreversible electroporation of rabbit VX2 liver tumor. Magn Reson Med. 2020;84:365-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 44. | Ben-David E, Ahmed M, Faroja M, Moussa M, Wandel A, Sosna J, Appelbaum L, Nissenbaum I, Goldberg SN. Irreversible electroporation: treatment effect is susceptible to local environment and tissue properties. Radiology. 2013;269:738-747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 87] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 45. | Scheffer HJ, Vogel JA, van den Bos W, Neal RE 2nd, van Lienden KP, Besselink MG, van Gemert MJ, van der Geld CW, Meijerink MR, Klaessens JH, Verdaasdonk RM. The Influence of a Metal Stent on the Distribution of Thermal Energy during Irreversible Electroporation. PLoS One. 2016;11:e0148457. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 46. | Qasrawi R, Silve L, Burdío F, Abdeen Z, Ivorra A. Anatomically Realistic Simulations of Liver Ablation by Irreversible Electroporation: Impact of Blood Vessels on Ablation Volumes and Undertreatment. Technol Cancer Res Treat. 2017;16:783-792. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 47. | Appelbaum L, Ben-David E, Faroja M, Nissenbaum Y, Sosna J, Goldberg SN. Irreversible electroporation ablation: creation of large-volume ablation zones in in vivo porcine liver with four-electrode arrays. Radiology. 2014;270:416-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 60] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 48. | O'Brien TJ, Bonakdar M, Bhonsle S, Neal RE 2nd, Aardema CH Jr, Robertson JL, Goldberg SN, Davalos RV. Effects of internal electrode cooling on irreversible electroporation using a perfused organ model. Int J Hyperthermia. 2018;35:44-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 49. | Kos B, Voigt P, Miklavcic D, Moche M. Careful treatment planning enables safe ablation of liver tumors adjacent to major blood vessels by percutaneous irreversible electroporation (IRE). Radiol Oncol. 2015;49:234-241. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 72] [Cited by in RCA: 55] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 50. | Beyer LP, Pregler B, Michalik K, Niessen C, Dollinger M, Müller M, Schlitt HJ, Stroszczynski C, Wiggermann P. Evaluation of a robotic system for irreversible electroporation (IRE) of malignant liver tumors: initial results. Int J Comput Assist Radiol Surg. 2017;12:803-809. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 51. | Beyer LP, Pregler B, Nießen C, Schicho A, Haimerl M, Jung EM, Stroszczynski C, Wiggermann P. Stereotactically-navigated percutaneous Irreversible Electroporation (IRE) compared to conventional IRE: a prospective trial. PeerJ. 2016;4:e2277. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 52. | Arena CB, Sano MB, Rossmeisl JH Jr, Caldwell JL, Garcia PA, Rylander MN, Davalos RV. High-frequency irreversible electroporation (H-FIRE) for non-thermal ablation without muscle contraction. Biomed Eng Online. 2011;10:102. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 201] [Cited by in RCA: 223] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 53. | Siddiqui IA, Latouche EL, DeWitt MR, Swet JH, Kirks RC, Baker EH, Iannitti DA, Vrochides D, Davalos RV, McKillop IH. Induction of rapid, reproducible hepatic ablations using next-generation, high frequency irreversible electroporation (H-FIRE) in vivo. HPB (Oxford). 2016;18:726-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 45] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 54. | Yao C, Dong S, Zhao Y, Lv Y, Liu H, Gong L, Ma J, Wang H, Sun Y. Bipolar Microsecond Pulses and Insulated Needle Electrodes for Reducing Muscle Contractions During Irreversible Electroporation. IEEE Trans Biomed Eng. 2017;64:2924-2937. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 47] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 55. | DeWitt MR, Lattouche E, Kaufman JD, Fesmire CC, Swet J, Kirks R, Baker E, Vrochides D, Iannitti D, McKillop I, Davalos RV, Sano M. Simplified Non-Thermal Tissue Ablation With A Single Insertion Device Enabled By Bipolar High-Frequency Pulses. IEEE Trans Biomed Eng. 2019;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 56. | Chen X, Ren Z, Yin S, Xu Y, Guo D, Xie H, Zhou L, Wu L, Jiang J, Li H, Sun J, Zheng S. The local liver ablation with pulsed electric field stimulate systemic immune reaction against hepatocellular carcinoma (HCC) with time-dependent cytokine profile. Cytokine. 2017;93:44-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 57. | Sugimoto K, Kakimi K, Takeuchi H, Fujieda N, Saito K, Sato E, Sakamaki K, Moriyasu F, Itoi T. Irreversible Electroporation versus Radiofrequency Ablation: Comparison of Systemic Immune Responses in Patients with Hepatocellular Carcinoma. J Vasc Interv Radiol. 2019;30:845-853.e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 58. | Bulvik BE, Rozenblum N, Gourevich S, Ahmed M, Andriyanov AV, Galun E, Goldberg SN. Irreversible Electroporation versus Radiofrequency Ablation: A Comparison of Local and Systemic Effects in a Small-Animal Model. Radiology. 2016;280:413-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 96] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 59. | Vivas I, Iribarren K, Lozano T, Cano D, Lasarte-Cia A, Chocarro S, Gorraiz M, Sarobe P, Hervás-Stubbs S, Bilbao JI, Casares N, Lasarte JJ. Therapeutic Effect of Irreversible Electroporation in Combination with Poly-ICLC Adjuvant in Preclinical Models of Hepatocellular Carcinoma. J Vasc Interv Radiol. 2019;30:1098-1105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 60. | Alnaggar M, Lin M, Mesmar A, Liang S, Qaid A, Xu K, Chen J, Niu L, Yin Z. Allogenic Natural Killer Cell Immunotherapy Combined with Irreversible Electroporation for Stage IV Hepatocellular Carcinoma: Survival Outcome. Cell Physiol Biochem. 2018;48:1882-1893. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 50] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 61. | Mir LM, Orlowski S, Belehradek J Jr, Paoletti C. Electrochemotherapy potentiation of antitumour effect of bleomycin by local electric pulses. Eur J Cancer. 1991;27:68-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 432] [Cited by in RCA: 417] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 62. | Belehradek M, Domenge C, Luboinski B, Orlowski S, Belehradek J Jr, Mir LM. Electrochemotherapy, a new antitumor treatment. First clinical phase I-II trial. Cancer. 1993;72:3694-3700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 63. | Gehl J, Skovsgaard T, Mir LM. Enhancement of cytotoxicity by electropermeabilization: an improved method for screening drugs. Anticancer Drugs. 1998;9:319-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 160] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 64. | Jaroszeski MJ, Dang V, Pottinger C, Hickey J, Gilbert R, Heller R. Toxicity of anticancer agents mediated by electroporation in vitro. Anticancer Drugs. 2000;11:201-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 115] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 65. | Jaroszeski MJ, Gilbert RA, Heller R. In vivo antitumor effects of electrochemotherapy in a hepatoma model. Biochim Biophys Acta. 1997;1334:15-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 53] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 66. | Ramirez LH, Orlowski S, An D, Bindoula G, Dzodic R, Ardouin P, Bognel C, Belehradek J Jr, Munck JN, Mir LM. Electrochemotherapy on liver tumours in rabbits. Br J Cancer. 1998;77:2104-2111. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 95] [Cited by in RCA: 84] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 67. | Chazal M, Benchimol D, Baqué P, Pierrefite V, Milano G, Bourgeon A. Treatment of hepatic metastases of colorectal cancer by electrochemotherapy: an experimental study in the rat. Surgery. 1998;124:536-540. [PubMed] |
| 68. | Jaroszeski MJ, Coppola D, Nesmith G, Pottinger C, Hyacinthe M, Benson K, Gilbert R, Heller R. Effects of electrochemotherapy with bleomycin on normal liver tissue in a rat model. Eur J Cancer. 2001;37:414-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 69. | Engström PE, Ivarsson K, Tranberg KG, Stenram U, Salford LG, Persson BR. Electrically mediated drug delivery for treatment of an adenocarcinoma transplanted into rat liver. Anticancer Res. 2001;21:1817-1822. [PubMed] |
| 70. | Zmuc J, Gasljevic G, Sersa G, Edhemovic I, Boc N, Seliskar A, Plavec T, Brloznik M, Milevoj N, Brecelj E, Kos B, Izlakar J, Jarm T, Snoj M, Stukelj M, Miklavcic D, Cemazar M. Large Liver Blood Vessels and Bile Ducts Are Not Damaged by Electrochemotherapy with Bleomycin in Pigs. Sci Rep. 2019;9:3649. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 42] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 71. | Brloznik M, Boc N, Sersa G, Zmuc J, Gasljevic G, Seliskar A, Dezman R, Edhemovic I, Milevoj N, Plavec T, Erjavec V, Pavlin D, Bosnjak M, Brecelj E, Tratar UL, Kos B, Izlakar J, Stukelj M, Miklavcic D, Cemazar M. Radiological findings of porcine liver after electrochemotherapy with bleomycin. Radiol Oncol. 2019;53:415-426. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 72. | Jarm T, Cemazar M, Miklavcic D, Sersa G. Antivascular effects of electrochemotherapy: implications in treatment of bleeding metastases. Expert Rev Anticancer Ther. 2010;10:729-746. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 141] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 73. | Edhemovic I, Brecelj E, Gasljevic G, Marolt Music M, Gorjup V, Mali B, Jarm T, Kos B, Pavliha D, Grcar Kuzmanov B, Cemazar M, Snoj M, Miklavcic D, Gadzijev EM, Sersa G. Intraoperative electrochemotherapy of colorectal liver metastases. J Surg Oncol. 2014;110:320-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 128] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 74. | Tarantino L, Busto G, Nasto A, Fristachi R, Cacace L, Talamo M, Accardo C, Bortone S, Gallo P, Tarantino P, Nasto RA, Di Minno MN, Ambrosino P. Percutaneous electrochemotherapy in the treatment of portal vein tumor thrombosis at hepatic hilum in patients with hepatocellular carcinoma in cirrhosis: A feasibility study. World J Gastroenterol. 2017;23:906-918. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 45] [Cited by in RCA: 50] [Article Influence: 6.3] [Reference Citation Analysis (1)] |
| 75. | Djokic M, Cemazar M, Popovic P, Kos B, Dezman R, Bosnjak M, Zakelj MN, Miklavcic D, Potrc S, Stabuc B, Tomazic A, Sersa G, Trotovsek B. Electrochemotherapy as treatment option for hepatocellular carcinoma, a prospective pilot study. Eur J Surg Oncol. 2018;44:651-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 59] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 76. | Beebe SJ, White J, Blackmore PF, Deng Y, Somers K, Schoenbach KH. Diverse effects of nanosecond pulsed electric fields on cells and tissues. DNA Cell Biol. 2003;22:785-796. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 151] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 77. | Beebe SJ, Fox PM, Rec LJ, Willis EL, Schoenbach KH. Nanosecond, high-intensity pulsed electric fields induce apoptosis in human cells. FASEB J. 2003;17:1493-1495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 340] [Cited by in RCA: 271] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 78. | He L, Xiao D, Feng J, Yao C, Tang L. Induction of apoptosis of liver cancer cells by nanosecond pulsed electric fields (nsPEFs). Med Oncol. 2017;34:24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 79. | Steuer A, Wende K, Babica P, Kolb JF. Elasticity and tumorigenic characteristics of cells in a monolayer after nanosecond pulsed electric field exposure. Eur Biophys J. 2017;46:567-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 80. | Steuer A, Schmidt A, Labohá P, Babica P, Kolb JF. Transient suppression of gap junctional intercellular communication after exposure to 100-nanosecond pulsed electric fields. Bioelectrochemistry. 2016;112:33-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 81. | Shi F, Steuer A, Zhuang J, Kolb JF. Bioimpedance Analysis of Epithelial Monolayers after Exposure to Nanosecond Pulsed Electric Fields. IEEE Trans Biomed Eng. 2018;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 82. | Wang Y, Yin S, Zhou Y, Zhou W, Chen T, Wu Q, Zhou L, Zheng S. Dual-function of Baicalin in nsPEFs-treated Hepatocytes and Hepatocellular Carcinoma cells for Different Death Pathway and Mitochondrial Response. Int J Med Sci. 2019;16:1271-1282. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 83. | Chen X, Zhuang J, Kolb JF, Schoenbach KH, Beebe SJ. Long term survival of mice with hepatocellular carcinoma after pulse power ablation with nanosecond pulsed electric fields. Technol Cancer Res Treat. 2012;11:83-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 54] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 84. | Yin S, Chen X, Hu C, Zhang X, Hu Z, Yu J, Feng X, Jiang K, Ye S, Shen K, Xie H, Zhou L, James Swanson R, Zheng S. Nanosecond pulsed electric field (nsPEF) treatment for hepatocellular carcinoma: a novel locoregional ablation decreasing lung metastasis. Cancer Lett. 2014;346:285-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 53] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 85. | Chen X, Yin S, Hu C, Chen X, Jiang K, Ye S, Feng X, Fan S, Xie H, Zhou L, Zheng S. Comparative study of nanosecond electric fields in vitro and in vivo on hepatocellular carcinoma indicate macrophage infiltration contribute to tumor ablation in vivo. PLoS One. 2014;9:e86421. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 86. | Chen R, Sain NM, Harlow KT, Chen YJ, Shires PK, Heller R, Beebe SJ. A protective effect after clearance of orthotopic rat hepatocellular carcinoma by nanosecond pulsed electric fields. Eur J Cancer. 2014;50:2705-2713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 63] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 87. | Nuccitelli R, Berridge JC, Mallon Z, Kreis M, Athos B, Nuccitelli P. Nanoelectroablation of Murine Tumors Triggers a CD8-Dependent Inhibition of Secondary Tumor Growth. PLoS One. 2015;10:e0134364. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 74] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 88. | Niessen C, Beyer LP, Pregler B, Dollinger M, Trabold B, Schlitt HJ, Jung EM, Stroszczynski C, Wiggermann P. Percutaneous Ablation of Hepatic Tumors Using Irreversible Electroporation: A Prospective Safety and Midterm Efficacy Study in 34 Patients. J Vasc Interv Radiol. 2016;27:480-486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 44] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 89. | Eller A, Schmid A, Schmidt J, May M, Brand M, Saake M, Uder M, Lell M. Local control of perivascular malignant liver lesions using percutaneous irreversible electroporation: initial experiences. Cardiovasc Intervent Radiol. 2015;38:152-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 90. | Cannon R, Ellis S, Hayes D, Narayanan G, Martin RC 2nd. Safety and early efficacy of irreversible electroporation for hepatic tumors in proximity to vital structures. J Surg Oncol. 2013;107:544-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 241] [Cited by in RCA: 245] [Article Influence: 20.4] [Reference Citation Analysis (0)] |