Published online May 7, 2020. doi: 10.3748/wjg.v26.i17.1993
Peer-review started: January 20, 2020
First decision: April 4, 2020
Revised: April 9, 2020
Accepted: April 21, 2020
Article in press: April 21, 2020
Published online: May 7, 2020
Processing time: 107 Days and 11.5 Hours
Non-alcoholic fatty liver disease (NAFLD) is characterized by excessive storage of fatty acids in the form of triglycerides in hepatocytes. It is most prevalent in western countries and includes a wide range of clinical and histopathological findings, namely from simple steatosis to steatohepatitis and fibrosis, which may lead to cirrhosis and hepatocellular cancer. The key event for the transition from steatosis to fibrosis is the activation of quiescent hepatic stellate cells (qHSC) and their differentiation to myofibroblasts. Pattern recognition receptors (PRRs), expressed by a plethora of immune cells, serve as essential components of the innate immune system whose function is to stimulate phagocytosis and mediate inflammation upon binding to them of various molecules released from damaged, apoptotic and necrotic cells. The activation of PRRs on hepatocytes, Kupffer cells, the resident macrophages of the liver, and other immune cells results in the production of proinflammatory cytokines and chemokines, as well as profibrotic factors in the liver microenvironment leading to qHSC activation and subsequent fibrogenesis. Thus, elucidation of the inflammatory pathways associated with the pathogenesis and progression of NAFLD may lead to a better understanding of its pathophysiology and new therapeutic approaches.
Core tip: Non-alcoholic fatty liver disease (NAFLD) is a frequent disorder in western countries with a wide range of histopathological findings, varying from simple steatosis to fibrosis or even cirrhosis. Metabolic dysregulation, principally during obesity, triggers chronic inflammation in the liver, defined as steatohepatitis that favors the development of fibrosis and likely cirrhosis and hepatocellular cancer. In this review we summarize and discuss the current literature regarding the principal inflammatory pathways involved in the pathogenesis of NAFLD and progression to non-alcoholic steatohepatitis.
- Citation: Katsarou A, Moustakas II, Pyrina I, Lembessis P, Koutsilieris M, Chatzigeorgiou A. Metabolic inflammation as an instigator of fibrosis during non-alcoholic fatty liver disease. World J Gastroenterol 2020; 26(17): 1993-2011
- URL: https://www.wjgnet.com/1007-9327/full/v26/i17/1993.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i17.1993
Non-alcoholic fatty liver disease (NAFLD) is defined as fatty acid accumulation in hepatocytes, called steatosis, in the absence of significant alcohol consumption or other known liver diseases. It is mostly attributed to conditions such as obesity, insulin resistance, microbiome disturbances and genetic predisposition[1-3]. NAFLD covers a spectrum of liver disorders, ranging from benign steatosis to steatohepatitis (NASH) or even cirrhosis and affects more than 40% of the population in western countries and approximately 25% of the world population[4]. The simple form of NAFLD is characterized by hepatic steatosis in at least 5% of hepatocytes without ballooning, while NASH is characterized by hepatic steatosis in at least 5% of hepatocytes with hepatocyte injury independent of fibrosis[5].
Thirty percent of patients with NAFLD will eventually develop NASH[4]. In these NAFLD patients, a gradual recruitment of cellular components of the immune system leads to inflammation as well as to tissue fibrosis[4], which are the two fundamental characteristics of NASH. Up until now it has been difficult to distinguish NAFLD from NASH in clinical practice and liver biopsy remains the gold standard method for the diagnosis of NAFLD and its progression to NASH[4,6]. The histological features of NASH are hepatic steatosis, hepatocellular ballooning and lobular inflammation which constitute the main components of the widely used NAFLD Activity Score (NAS)[5,7]. Importantly, hepatocyte ballooning is a feature denoting cellular injury characterized by enlarged swollen hepatocytes with or without Mallory-Denk bodies (MDB) in the cytoplasm[8]. Both ballooning of hepatocytes and MDB are the two hallmarks of ongoing inflammation; nevertheless the presence of MDB is supportive but not required for the diagnosis of steatohepatitis[7,9].
A key event in the progression of steatosis into NASH is the differentiation of hepatic stellate cells (HSCs) to myofibroblasts. Under normal conditions, quiescent HSCs are localized in Disse’s space in the liver where they store around 80% of the body’s vitamin A. In conditions of chronic stimulation, HSCs proliferate and produce extracellular matrix (ECM) proteins which contribute to the emergence and progression to hepatic fibrosis[10]. Although myofibroblasts can also be produced by portal fibroblasts and vascular smooth muscle cells, the main source of ECM during NASH development are activated HSCs[11-14]. Several mechanisms, including obesity-related low-grade inflammation and insulin resistance, as well as changes in the intestinal microbiome may trigger this process[15]. This review summarizes the current literature regarding the inflammatory mechanisms contributing to the progression of steatosis into liver fibrosis and NASH.
Liver fibrosis is defined as damage caused by an excessive accumulation of connective tissue proteins in the liver, especially interstitial collagens that form fibrous scar and subsequent development of NASH[16,17]. A well described hypothesis for the transition of NAFLD to NASH, including fibrosis, is that of the “multiple hit hypothesis”. According to this hypothesis, NAFLD is induced by the simultaneous synergism of multiple factors such as insulin resistance, adipose tissue inflammation, oxidative damage as well as activation of Transforming growth factor-beta (TGF-β) in a pre-existing lipid-rich environment in the liver[18].
The initial event leading the transition of steatosis to NASH is the accumulation and storage of lipids as macrovesicular fat in the cytoplasm of the hepatocytes[10,19] which consists of fatty acids, ceramides, free-cholesterol, diacyl-glycerol and phospholipids[4]. This toxic lipid-induced hepatocyte injury, referred as lipotoxicity, leads to cellular stress, apoptosis and eventually cell death[20,21]. The apoptotic hepatocytes initiate an inflammatory process by secreting extracellular vesicles[4] which consist of exosomes, microvesicles or apoptotic bodies that contribute to intercellular communication in NASH pathogenesis[22,23]. More specifically, HSCs and Kupffer cells engulf the apoptotic bodies released from the hepatocytes, leading to the secretion of fibrogenic factors such as TGF-β, or inflammatory mediators such as Tumor necrosis factor-α (TNF-α)[24]. Additionally, cytokines and chemokines secreted by Kupffer cells promote the recruitment of other immune cells, further perpetuating the inflammatory process and HSC activation taking place under steatotic conditions in the liver[25]. Of note, obesity and metabolic dysregulation lead to alterations in the gut microbiome, thus provoking increased permeability of the small bowel and as a consequence further increasing fatty acid absorption as well as easier penetration by bacterial endotoxins[26]. These events may cause the gut microbiota to transverse the intestinal barrier and translocate to the liver thereby triggering the inflammatory response[27,28].
The “second hit” of the multiple hit hypothesis constitutes the continuous lipid buildup in hepatocytes during NAFLD thus inducing oxidative stress via mitochondrial overload leading to a “chronic-like” production of reactive oxygen species, cytokines and chemokines which are prerequisite mediators in NAFLD to NASH progression[29,30]. The increased oxidative stress, the cell death that ensues and the continuous unresolved inflammation perpetuate HSC activation that lead to fibrosis[31,32]. More precisely, in response to continuous exposure to cytokines and growth factors, qHSCs are getting activated and proliferate producing compounds of ECM[13], such as the collagen type I and type III, as well as Τissue inhibitor of metalloproteinases 1 (TIMP-1)[33], all contributing to fibrogenesis[32,33]. In addition, the engulfment of apoptotic bodies by HSCs confers on them a partial resistance to TNF and Fas ligand thereby gaining resistance against cell death[14]. Finally, the excessive production of ECM with a dominance of collagen leads to NAFLD-related liver fibrosis[19].
The role of inflammation is important in hepatic fibrogenesis during NAFLD[15]. Several immune cell populations of both the innate and adaptive immunity, already existing in the adult liver or recruited from the circulation during NAFLD, are implicated in this process[6,15]. Kupffer cells, recruited monocyte-derived macrophages, dendritic cells and neutrophils are major innate immune subpopulations involved in NAFLD to NASH transition, while T-cell subpopulations such as natural killer T (NKT) cells, T-helper 17 (Th17) cells and T-regulatory (Treg) cells are also of major importance[4,15]. Although the majority of the aforementioned cellular players are thought to provoke the emergence of hepatic fibrosis during NAFLD and metabolic dysregulation, a minority of them such as Treg, have a protective role, while evidence regarding others, such as dendritic cells remains controversial[4,6,15,34].
Pattern recognition receptors (PRRs), including Toll-like receptors (TLRs) and nucleotide-binding oligomerization domain-like receptors (NOD-like receptors or NLRs) located predominantly on Kupffer but also on HSCs are essential for NAFLD-related fibrosis by recognizing Pathogen-associated molecular patterns (PAMPs) and Damage-associated molecular patterns (DAMPs)[35]. PAMPs are external danger signals principally expressed by microbes such as bacteria and parasites, but they can also be lipids, lipoproteins, proteins and nucleic acids[36]. DAMPs on the other hand constitute internal pathogenic agents such as HMGB1, S100 protein, heat shock proteins, hyaluronan and fibronectin[27] and in the case of NAFLD can be produced by damaged hepatocytes[37]. Activation of TLRs and NLRs by PAMPs and DAMPs in Kupffer cells as well as in HSCs during NAFLD leads to the secretion of cytokines such as TNF-α and interleukin-1β (IL-1β), thus provoking the progression to NASH. We herein describe the molecular inflammatory events taking place upon TLR and NLR activation in the steatotic liver, as well as the role of cardinal cytokines that lead to the emergence and development of fibrosis during NAFLD.
The TLR receptors comprise a group of 11 proteins in humans and 13 proteins in mice. In the liver, TLRs serve as PRRs on Kupffer cells and HSCs, but are also expressed by other cell types such as dendritic cells, endothelial cells, and hepatocytes[38]. TLRs are divided into two subpopulations according to their cellular localization. TLR1, TLR2, TLR4, TLR5, TLR6 and TLR11 are expressed exclusively on the cell surface and mainly recognize PAMPs, while TLR3, TLR7, TLR8 and TLR9 are localized in intracellular vesicles such as endosomes or lysosomes and the endoplasmic reticulum (ER) and predominantly recognize DAMPs[27,39]. Upon stimulation they activate two signaling pathways; the molecule adaptor protein myeloid differentiation factor 88 (MyD88)-dependent signaling pathway and/or the MyD88-independent pathway involving the TIR domain-containing adaptor (TRIF) resulting in the production of type I Interferons (IFNs). The former is common to all TLRs, except TLR3, and leads to the production of inflammatory cytokines while the latter is associated with the production of IFN-β and the maturation of dendritic cells and occurs via the Toll/IL-1R domain-containing adaptor-inducing IFN-β (TRIF)-dependent signaling regulatory factor 3 (IRF-3) responsible for type I IFN synthesis as well as inflammatory cytokines through associated NF-κB activation[40,41]. TLR2, TLR4 and TLR9 are expressed in both Kupffer cells and HSCs and their roles in the development of NASH is summarized below.
Previous studies have shown a contributing role of TLR2 in the development of NASH. Miura et al[42] reported that TLR2 signaling in combination with palmitic acid increased the expression of proinflammatory cytokines including IL-1β, and an inflammasome component, Nod-like receptor protein 3 (NLRP3), in Kupffer cells but not in HSCs. TLR2-/- mice fed a choline-deficient, l-amino acid-defined (CDAA) diet, had reduced NAFLD activity score and diminished infiltration of inflammatory cells compared to wild-type mice. Concurrently, the expression of alpha-smooth muscle actin (α-SMA) was diminished, while the production of collagen a1 types I and IV mRNAs were reduced as was the expression of TGF-β1, TIMP-1 and Plasminogen Activator Inhibitor 1 (PAI-1) mRNA[42]. These data are in line with those of Ji et al[43] who showed that carbon tetrachloride (CCl4) administration in TLR2-/- mice resulted in diminished liver injury as indicated by reduced activation of HSCs, reduced deposition of collagen and reduced expression of several pro-fibrotic and pro-inflammatory genes including TNF-α, IL-6, Platelet-derived growth factor (PDGF), TGF-β and TIMP-1. Furthermore Ji et al[43] showed that the CCl4-induced phosphorylation of ERK1/2, p38 and JNK signaling pathways as well as impaired NF-κB activation were significantly diminished in TLR2−/− mice compared with WT mice, strongly suggesting that TLR2 may promote the fibrogenesis via activating MAPK and NF-κB signaling pathways[43]. Another study by Szabo et al[44] 2005 investigated the roles of TLR2 and TLR4 in liver damage and on cytokine induction in a methionine-choline deficient (MCD) diet-induced model of NASH. They reported that MCD diet-induced steatohepatitis in mice results in the sensitization of TLR4 but not to TLR2-induced liver injury. In contrast to the aforementioned studies they showed that steatohepatitis in TLR2-/- mice results in increased liver injury as evidenced by elevated ALT and TNF-α levels suggesting a potential protective role for TLR2 in fatty liver.
The contribution of TLR4 in NASH pathogenesis has been widely studied. The TLR4 receptor is primarily activated by lipopolysaccharide (LPS) of Gram negative bacteria, as well as by HMGB1, hyaluronan, saturated fatty acids, fibronectin, heat shock proteins 60 and 70, degraded matrix and DAMPs secreted by damaged cells[45,46]. However, bacterial products such as bacterial flagellin, bacterial toxins, and LPS or DNA from the gut remain the main promoters of TLR4 activation[46,47].
TLR4 is expressed by Kupffer cells and HSCs. The TLR4 dimer associates with the adaptor protein myeloid differentiation protein 2 (MD-2) on Kupffer cells and HSCs which in turn bind indirectly to the bacterial endotoxin lipid A. Lipid A is the lipophilic domain of circulating LPS and forms the main cell wall component of Gram negative bacteria. The resulting active TLR4/MD-2/LPS complex binds extracellularly and initiates a signaling cascade that leads to the activation of NF-κB and the production of pro-inflammatory cytokines leading to inflammatory and immune responses[48]. In this manner, Kupffer cells participate in pro-inflammatory and pro-fibrogenic cytokine production, while activated HSCs secrete ECM[27], as well as chemokines, promoting further chemotaxis of immune cells in the liver[46].
Liu et al[49] employing a NAFLD animal model provided convincing evidence of the involvement of TLR4 in NASH development. They investigated TLR4 signaling at different stages of NAFLD induced by a high-fat, high fructose (HFHFr) diet in TLR4-mutant and in control wild-type mice and assessed the pathological characteristics of the liver. After 8 weeks and 16 weeks of HFHFr feeding, the WT mice showed increased AST and ALT levels compared to TLR4-mutant mice. Furthermore, as early as week 4, histopathological evaluation showed that the HFHFr-fed wild type mice exhibited micro and macrovesicular steatosis; by week 8 they demonstrated hepatocellular ballooning and lobular inflammation and by week 16 they showed notable fibrosis while TLR4 mutant mice fed the same diet for the same length of time showed significantly reduced fibrosis. Their data suggest that TLR4 signaling is a major link between inflammation and fibrosis in NAFLD. Of note, the TLR4 receptor downregulates TGF-β pseudoreceptor Bambi via MyD88-NF-kB pathway suggesting that HSCs respond to TGF-β induced signals[46]. In addition, liver biopsies obtained from obese women undergoing RYGB (Roux-en-Y Gastric Bypass) operation showed increased TLR4 and IRF3 expression in subjects with NASH compared with those with NAFLD[50]. Interestingly, a study investigating the status of bacterial translocation in cirrhotic liver found that in NASH liver tissue, even if bacterial colonization was decreased, TLR4 mRNA and its protein product were increased compared to the control group[51].
TLR9 is located in the endoplasmic reticulum of dendritic cells, macrophages, endothelial cells and hepatocytes and principally recognizes non-methylated CpG sequences in DNA of bacteria[52,53]. LPS upregulates the expression of TLR9 in murine macrophages in a NF-kB- and MAPK-dependent manner[53]. Evidence obtained from the human hepatic stellate cell line LX-2 cells as well as from primary mouse HSCs, indicate that TLR9 also participates in HSC differentiation. DNA along with CpG fragments released by apoptotic hepatocytes led to an increase of TGF-β1 and collagen I mRNA in HSCs, implying activation of the latter via TLR9 stimulation[54]. In a murine experimental model of NASH induced by CDAA diet, the Kupffer cells of TLR9-/- mice showed reduced expression of IL-1β, while the mice showed less steatohepatitis and fibrosis in comparison to wild-type control mice[55]. Indeed, translocated bacterial DNA seems to bind to TLR9 of Kupffer cells promoting the secretion of IL-1β which in turn promotes hepatocyte damage and death via lipid accumulation, while inducing HSC activation, thus leading to steatohepatitis and fibrosis[55]. In another study by Gäbele et al[56], activation of HSCs derived from TLR9+/+ mice by CpGs of bacterial DNA led to increased monocyte chemoattractant protein-1 (MCP-1) mRNA compared to those from TLR9-/- mice, indicating that MCP-1 secretion from HSCs strongly depends on the activation of TLR9.
Nucleotide binding oligomerization domain-like receptors (NLRs) comprise a family of conserved, cytosolic innate immune PRRs essential in detection of PAMPs and DAMPs, including cytosolic microbial and danger components, as well as molecules emanating from damaged or disrupted cells[57]. All members of the NLR family are defined by a central NACHT or NOD domain responsible for oligomerization and nucleotide-binding which mediates the activation of the transduction complex. The majority of NLRs also have a C-terminal domain which is rich in leucine repeats (LRRs), acting as a sensor of ligands, whereas a caspase recruitment or pyrin or a baculovirus inhibitor repeats domain (CARD, PYD and BIR respectively) is situated in the N-terminal region of NLRs. Homotypic interactions resulting to downstream signaling are implemented by this N-terminal domain[58]. Importantly, depending on the type of the N-terminal domain, the NLR family is divided into 4 main subfamilies, namely NLR-A, NLR-B, NLR-C, and NLR-P (A for acidic transactivating domain, B for BIRs, C for CARD and P for PYD)[59], while NLR-X is an additional subfamily without any significant homology to the N-terminal domain of the other subfamilies[60,61].
NLRs include positive regulators of inflammation, such as the NOD-, LRR- and pyrin domain-containing protein 3 (NLRP3), and anti-inflammatory ones such as NLRX1 and NLRP12[62,63]. Upon activation, the majority of NLRs oligomerize to form multiprotein inflammasome complexes which are high-molecular-weight cytosolic multiprotein complexes in the cytosol of host cells that regulate pathogen recognition, host defense, and inflammatory processes. The activation of inflammasome occurs as a consequence of infection or other form of cellular stress and damage, such as fragments of double stranded DNA, amyloid β, hyaluronic acid and monosodium urate[47,64]. The NLRP3 is the most studied inflammasome to date. This cytosolic structure of proteins is formed in a two-step process including priming, as a result of overexpression by TLR signaling, and triggering, which is orchestrated by K+ efflux as a result of increased production of reactive oxygen species, originating from damaged mitochondria and lysosome destabilization both leading to inflammation. Assembly of the NLRP3 inflammasome interacts with caspase-1 leading to its activation and upon activation, caspase-1 promotes the maturation of the proinflammatory cytokines IL -1β and IL-18 following cleavage of their precursors Pro-IL-1β and Pro-IL-18[47,64,65]. In addition, caspase-1 activates gasdermin D which is responsible for pore formation leading to a form of cell death called pyroptosis. This proinflammatory type of cell death is a consequence of activation of inflammasome leading to the release of cytoplasmic components including the inflammatory cytokines[66-68].
Growing evidence indicates the association of the innate immune system in sensing cellular stress originating from deregulated metabolic conditions. In the case of NAFLD, upregulation and overactivity of cellular and molecular components of the immune system, like the NLR inflammasomes, is believed to be the “effector links” for the progression of steatosis into NASH.
NLR signaling and activation of inflammasomes is believed to take place not only in innate immune cells like macrophages and neutrophils but also in non-immune cells in the liver, such as hepatocytes, endothelial cells and HSCs[69]. An upregulation in the expression of NLRP3 inflammasome components has been observed in livers of mice fed a MCD diet, suggesting the participation of several hepatic cellular players, apart from immune cells, in the initiation of inflammation and progression to NASH[70]. Indeed, murine hepatocytes have demonstrated activation of the NLRP3 inflammasome and subsequent caspase-1-dependent secretion of IL-1β after treatment with palmitic acid and LPS, while danger signals that are released from hepatocytes under the same conditions are able to activate liver mononuclear cells in a paracrine-dependent manner[70]. Similarly, cultured HSCs deriving from rats show significant increase in expression of several NLR family members, including NLRP1, NLRP3 and NLRC4 after treatment with LPS, while hepatocytes were predominantly characterized by strong NLRP3 activation[71]. Furthermore, in palmitate-treated Kupffer cells, the release of IL-1β and IL-18 was shown to be dependent on NLRP3 inflammasome activation[72].
Genetic or pharmacological manipulations of NLR inflammasomes in mice have provided important information in scrutinizing their role in the progression of NAFLD. The contribution of inflammasome in metabolic dysfunction and NAFLD has been observed in knockout mice for NLRP3, which were fed a HFD, and displayed improved insulin resistance, accompanied by attenuated fat deposition in the liver and reduced adipocyte size in the adipose tissue[73]. Oppositely, continuous NLRP3 activation led to NASH development characterized by deteriorated inflammation and fibrosis in murine models of diet-induced NAFLD[74]. Along this line, a recent study in mice revealed that liver fibrosis and inflammation in a setting of experimental NASH were attenuated after administration of a molecular NLRP3 inhibitor[75]. Importantly, pyroptosis that is induced in hepatocytes upon NLRP3 activation and results in the release of inflammatory mediators outside of the pyroptotic cell, is thought to be a major mechanism of propagating inflammation and further perpetuating NLR signaling to adjacent cells in the liver, such as HSCs[74,76,77].
Apart from experimental animal studies, clinical studies in individuals with metabolic syndrome have indicated the causal link between IL-1β and IL-18, as products of inflammasome activation, to the development of metabolic dysregulation[78]. For instance, the grade of NLRP3 expression in adipose tissue of obese individuals correlates to the severity of type 2 diabetes mellitus in a direct fashion[79]. Accordingly, NLRP3 and caspase-1 expression levels are elevated in the liver of individuals with NASH[70]. In human HSC cultures, inflammasome components have been identified as essential for inflammatory and fibrotic rearrangements following application of monosodium urate crystals[80].
Several cytokines, such as IL-1, IL-6, PDGF and TGF-β, secreted both by immune cells as well as by parenchymal cells of the liver during NAFLD contribute to the progression of the disease into NASH by promoting hepatic fibrosis via the activation of HSCs[15]. Apart from the cytokines produced and secreted within the liver microenvironment, cytokines derived from adipose tissue are also important instigators of the aforementioned process. Especially under obese conditions, the adipose tissue is characterized by the production of TNF-α and IL-6 by adipocytes and macrophages which in turn target the liver inducing hepatic insulin resistance as well as fat deposition and fibrosis[35,81,82].
TNF-α and PDGF are involved in the earlier phases of NAFLD-related liver inflammation when the main changes are matrix degradation, migration and cell proliferation. On the other hand, TGF-β is critical in later stages of inflammation, when matrix accumulation outweighs degradation[83]. It should be emphasized that resident and recruited macrophages produce PDGF, TGF-α, TNF-α and insulin-like growth factor-1 (IGF-1) which function as mitogenic agents for HSCs. Interestingly, the HSCs themselves produce TGF-α and TGF-β after their activation. The latter acquires an autocrine action inducing HSCs proliferation[83]. Herein, we describe the implication of cardinal cytokines involved in HSC activation and their differentiation to myofibroblasts.
The importance of TNF-α in NASH and hepatic fibrosis is supported by many studies. A study including obese patients, demonstrated a significant increase of TNF-α mRNA expression in livers derived from individuals with significant hepatic fibrosis in comparison to those who were not characterized by liver fibrosis[84]. Similarly, in a cross-sectional study with patients with NASH, a correlation between TNF-α along with collagen type IV and the stage of fibrosis was found[85]. In wild type mice fed with CDAA, an increased activity of TNF-α converting enzyme, which cleaves pro-TNF-α into the active form of TNF-α, as well as increased production of TNF-α, collagen a1, and TGF-β have been reported[86].
In principle, TNF-α is mainly produced by macrophages as a response to different bacterial products such as LPS and exerts its action via the binding to TNF receptors (TNFR) 1 and 2[87]. In the case of hepatic injury, such as during NAFLD-induced hepatocyte damage, the released PAMPs and DAMPs induce the activation of innate immune cells that secrete cytokines such as TNF-α, IL-6 and IL-1α[36]. The main source of hepatic TNF-α are hepatocytes and Kupffer cells, while abdominal fat also participates[88].
TNF-α has been found to suppress the apoptosis of primary cultured HSCs through the increase of TIMP-1 mRNA expression[89], while simultaneously contributes to their survival and proliferation[32]. TNF-α-/- mice showed attenuated liver fibrosis after bile duct ligation. However, after administration of TNF-α, the expression of collagen a1 mRNA was reduced in rat HSCs. Consistently, TIMP-1 was increased in TNF-α+/+ mice in comparison to TNF-α-/- mice[90]. In models of hepatic cirrhosis, a continuous activation of HSCs was observed (as defined by α-SMA staining), as a result of persistent TIMP-1 mRNA expression[33]. Along this line, TNFR1 seems to be involved in HSC activation. HSCs derived from TNFR1- or TNFR1/TNFR2 double- knockout mice, but not from TNFR2 knockout mice, showed reduced mRNA expression of procollagen-a1 as compared to those derived from wild type mice[91]. Consistently, TNFR1/TNFR2 double- knockout mice are characterized by improved steatosis and fibrosis when exposed to a MCD diet, as compared to wild-type control mice[89].
Among the members of the IL-1 family, IL-1α and IL-1β are the most broadly studied in NAFLD. They are predominantly secreted by hepatic macrophages and play a major role in all stages of the disease including deterioration of insulin signaling, hepatic lipid accumulation and induction of fibrosis[92].
Kamari et al[93] investigated the role of the proinflammatory cytokines IL-1α and IL-1β in steatohepatitis. They reported that atherogenic diet-induced steatohepatitis in wild-type mice was associated with significant increases in the mRNA levels of hepatic IL-1α and IL-1β, while, oppositely, mice deficient in either IL-1α or IL-1β showed reduced transformation of steatosis to steatohepatitis and liver fibrosis in spite of increased cholesterol levels[93]. Indeed, IL-1β is thought to induce lipid accumulation in hepatocytes via IL-1 receptor (IL-1R). More precisely, under NAFLD conditions, Kupffer cells highly secrete IL-1β which in turn mediates the development of liver steatosis via NF-kB stimulation in hepatocytes that leads to suppression of peroxisome proliferator-activated receptor alpha activity[94]. In addition, IL-1β seems to contribute directly to the development of fibrosis. In rat HSCs, IL-1b was shown to induce MMP-13 gene expression, by acting via the JNK and p38 MAPK pathways, thus influencing the remodeling of ECM and promoting fibrosis[95]. Similarly, reduced liver steatosis and fibrosis was observed in IL-1R-deficient mice when diet-induced models of NASH were used[96,97].
On the contrary, the IL-1R antagonist (IL-1Ra) is thought to have an anti-inflammatory role in liver diseases[98] and mice deficient for IL-1Ra fed an atherogenic diet showed severe steatosis and fibrosis in the liver compared to wild type mice fed the same diet[99]. Nevertheless, in a study including 6447 men, the serum levels of IL-1Ra correlated with NASH and serum ALT independently of obesity, consumption of alcohol or insulin resistance[100].
IL-6 is a pro-inflammatory cytokine with an obscure role in NASH. During obesity, the protein levels of IL-6 in the adipose tissue correlate with the degree of insulin resistance[101], while its mRNA levels correlate with those of CRP[102]. A study using liver biopsies from patients with NAFLD showed elevated hepatic IL-6 levels in patients with NASH compared to those with only steatosis or normal liver biopsy, which also correlated with the circulating levels of IL-6[103]. Similarly, in obese patients, the blood levels of IL-6 seem to be higher in those with severe steatosis in comparison with those with mild steatosis[104]. Of note, adipose tissue IL-6 expression correlates to the degree of NAFLD progression among obese individuals[105]. Another study investigating the influence of diet and aerobic exercise with or without the administration of vitamin E on cytokines showed increased TNF-α, IL-8 and IL-6 levels, both in plasma and in peripheral blood monocytes, in patients with NASH compared to controls. However, after the intervention, only IL-6 in plasma was reduced[106].
Despite the clinical observations, mechanistic studies using animal models provide controversial evidence. Already in 2002, Wallenius et al[107] showed that genetic ablation of IL-6 in mice is associated with the development of mature onset obesity and insulin resistance. In mice fed a MCD diet, intraperitoneal administration of the IL-6 receptor antibody MR16-1 was shown to block the IL-6/gp130 pathway resulting in reduced hepatic injury, but at the same time increased lipid accumulation and hepatic steatosis[108]. Oppositely, when IL-6 was administered into HFD-fed mice led to upregulation of lipogenesis-related genes and deterioration of hepatic steatosis[109]. Interestingly, IL-6, in a Stat-3 dependent way, induces the expression of Indy, which is a citrate transporter receptor that favors hepatic lipogenesis[110].
TGF-β is major mediator of HSC activation and hepatic fibrosis in chronic liver diseases; nevertheless, it is involved in several cellular processes such as cell survival, proliferation and angiogenesis[111]. TGF-β signaling is taking place in a SMAD- and non-SMAD dependent way. The former is thought to be the “canonical”-TGF-β signaling pathway mediated by phosphorylation of the SMAD proteins, while the latter is mediated by activation of other pathways such as the MAPK or the PI3K/AKT pathways[112]. TGF-β exists in three isoforms, namely TGF-β1, 2, and 3 which share some common but not equal functions, with TGF-β1 being the most extensively studied in the field of hepatic fibrosis[111,112]. In the liver, Kupffer cells constitute the main source of TGF-β, while during fibrosis it can also be produced by stellate and endothelial cells[113]. In particular, during obesity and NAFLD, leptin deriving from the obese adipose tissue stimulates the production of TGF-β1 from Kupffer cells[114].
The involvement of TGF-β1 in hepatic fibrosis has been under intense investigation for more than two decades. Indeed, in 1992, Annoni et al[115] showed that liver biopsies from patients with active liver disease and fibrosis displayed increased hepatic expression of TGF-β1, which positively correlated to the mRNA levels of procollagen α1. Similarly, multiple studies have demonstrated that the hepatic mRNA levels of TGF-β are increased in patients with NASH and fibrosis[116,117]. Nevertheless, existing data regarding the diagnostic value of circulating TGF-β1 levels in reflecting the presence of fibrosis and the progression of steatosis into NASH are contra-dictory[118-121]. In line with the evidence obtained from human studies, CCl4-induced hepatic fibrosis in mice is associated with increased expression of TGF-β1 in the livers of these mice[122,123]. Along this line, TGF-β1 deficiency in mice leads to reduced hepatic expression of collagen a1 and α-SMA upon CCl4 administration, consistent with reduced fibrosis, while adenovirus-mediated TGF-β1-overexpression induced their expression[124]. During obesity and metabolic dysregulation, TGF-β exerts its action via the TGF-β-SMAD pathway and genetic deletion of SMAD3 in mice is associated with protection from insulin resistance and liver steatosis in HFD-induced obesity[125]. Noteworthy, wild-type mice fed a CDAA diet showed increased activation of SMAD2/3, deteriorated liver steatosis, inflammation as well as hepatocyte death and fibrosis compared to hepatocyte-specific TGF-β receptor type II-deficient mice[126,127]. Overall, TGF-β participates both in lipid accumulation as well as to NASH progression during NAFLD.
Platelet-derived growth factor (PDGF) is produced by hepatic macrophages, activated HSCs as well as by platelets. It boosts HSC migration and proliferation and a loss of vitamin A which is normally stored into quiescent HSCs[83,128]. PDGF is a dimeric polypeptide that can consist of the same or different subunits. Four different types of PDGF subunits have been identified namely PDGF-A, -B, -C and D, which can be combined into five different PDGF polymers, namely PDGF-AA, -BB, -AB, -CC, and –DD[128]. PDGF binds to PDGF receptors-a and –b, which are present on endothelial cells, macrophages and fibroblasts including the HSCs, and affects cell proliferation, cell migration, angiogenesis while it promotes alterations in membrane structure. In HSCs, it also participates in the synthesis of ECM by inducing secretion of collagen and other ECM components[10,128]. PDGF binding to its receptors activates predominantly the Ras-MAPK pathway leading to the aforementioned cellular reactions and molecular changes[128,129].
Several studies have highlighted the role of the PDGF family of ligands in liver fibrosis, including their action during metabolic dysregulation and NAFLD. Of note, PDGF-B and PDGF-D are major stimuli of HSCs’ proliferation and activation in contrast to PDGF-A and PDGF-C that do not equally provoke a fibrogenic response by the HSCs in vitro[130]. Nevertheless, hepatic overexpression not only of PDGF-B, but also of PDGF-A or PDGF-C in mice was able to induce fibrosis in the liver[131-133]. Consistently, antivirus-mediated suppression of PDGF-B production attenuated liver fibrosis in a short-term BDL model in rats[134]. Similarly, fibrosis was improved after vaccination with PDGF-B kinoid immunogens in mice that were subjected to CCl4-induced fibrosis[135]. In the context of NASH, increased expression of PDGF-AA in the liver is associated with elevated risk for the development of insulin resistance and steatohepatitis in humans[136], while PDGF-C seems to be an instigator of steatosis into NASH progression both in humans and rodents[132,137].
The gut flora is one of the main regulating factors for the development of NAFLD. Under normal conditions, the gut microbiota has beneficial effects to host health such as contribution to digestion as well as to immune defense by maintaining the integrity of gastrointestinal barrier and by participating in immunomodulation[138,139]. Although to a limited extent, bacterial products present in the gastrointestinal system are able to reach the liver via the portal vein. When the intestinal barrier, that normally plays a protective role against a plethora of pathogens, is disrupted and gut permeability is increased, bacterial translocation is possible[140]. Indeed, a meta-analysis based on human studies showed that patients with NAFLD and NASH had increased intestinal permeability compared to control subjects[141], while other studies have reported correlations between microbiota composition and NAFLD development[142,143]. For instance, in a study by Le Roy et al[142] C57BL/6J wild-type mice were fed a high-fat diet for 16 weeks and then divided into two groups according to the development of metabolic dysregulation and systemic inflammation. The first group that displayed hyperglycemia and inflammation was defined as “responder” and the second one displaying normal blood glucose as “non-responder”. When gut microbiota from these two groups were transferred to germ-free mice, the “responder-receiver” group displayed high blood glucose and insulin, along with liver steatosis, suggesting that the composition of the microbiome may influence glucose homeostasis and the development of hepatic steatosis. Another study by Boursier et al[143] reported a correlation between gut dysbiosis and the severity of NAFLD in humans. Briefly, in stool samples derived from NAFLD patients, the presence of Bacteroides was associated to that of NASH, while Ruminococcus abundance was correlated with important fibrosis.
Among the microbial components participating in NAFLD pathogenesis are LPS, peptidoglycan (PGN), flagellin, lipoteichoic acid, unmethylated CpG motifs, short-chain fatty acids (SCFAs), and bacterial DNA, having either detrimental or beneficial effect on liver steatosis[138,144]. LPS is a component of the outer membrane of Gram-negative bacteria[145] and its circulating levels have been reported to be increased during NAFLD in animal as well as in human studies[144,146]. Indeed, as mentioned above, LPS may promote the development of NAFLD via binding to TLR4 expressed both by immune as well as parenchymal cells of the liver[147,148]. Interestingly, a 4-week high fat diet in mice provokes elevation of plasma LPS and a shift to a more LPS-containing microbiome in the gut[146]. Of note, the same study showed that the presence of LPS-endotoxemia was of cardinal importance for the induction of hepatic steatosis and insulin resistance associated with the development of a low-grade inflammatory state in the liver and the adipose tissue, which was characterized by increased mRNA levels of TNF-α, IL-6 and PAI-1[146]. Besides, in vitro and in vivo evidence supports that a fatty acid rich microenvironment favors an augmented LPS absorption by enterocytes, promoting thus postprandial endotoxemia[149].
PGN is a cell component of both Gram-negative and Gram-positive bacteria providing rigidity of cell wall[145]. PGN can be recognized by NOD1, NOD2, and TLR2, inducing the expression of pro-inflammatory cytokines in a NF-Kβ/MAPK pathway-dependent way[145,150]. Along this line, a 4-week administration of PGN in normal chow-fed mice induced elevation of circulating transaminases and insulin levels, while it increased hepatic triglyceride deposition and the expression of lipogenesis-related genes. Thus, intestinal microbiota-derived PGN is able to promote hepatic lipogenesis and fibrosis via an NOD2-NFkΒ-PPΑRγ pathway-related mechanism[151].
SCFAs, including propionate, butyrate and acetate, are predominantly produced by anaerobic microbiota of the colon upon fragmentation of dietary fiber[152,153]. In contrast to LPS and PGN, the role of SCFAs in the development of NAFLD steatosis seems to be rather protective and anti-inflammatory. Indeed, in the epithelium of the gastrointestinal tract, SCFAs bind to the “metabolite-sensing” receptors GPR43 and GPR109A, inducing the expression of IL-18, thus protecting gut barrier integrity[153]. Besides, butyrate was found to induce colonic Treg cell differentiation, thereby contributing to intestinal immune homeostasis[154]. In addition, SCFAs trigger the secretion of Glucagon-Like Peptide-1 (GLP-1) by the intestinal enteroendocrine L-cells, which in turn ameliorates NAFLD development and progression by provoking fatty acid oxidation in the liver[155,156]. Interestingly, this phenomenon may function in a positive feedback mode since sodium butyrate was found to induce the hepatic expression of GLP-1 receptor and attenuate NAFLD in mice subjected to a high fat diet[157]. Similarly, in humans, propionate administration for 24 weeks triggered GLP-1 and peptide YY secretion, leading to attenuated hepatic lipid accumulation and improved insulin resistance[158].
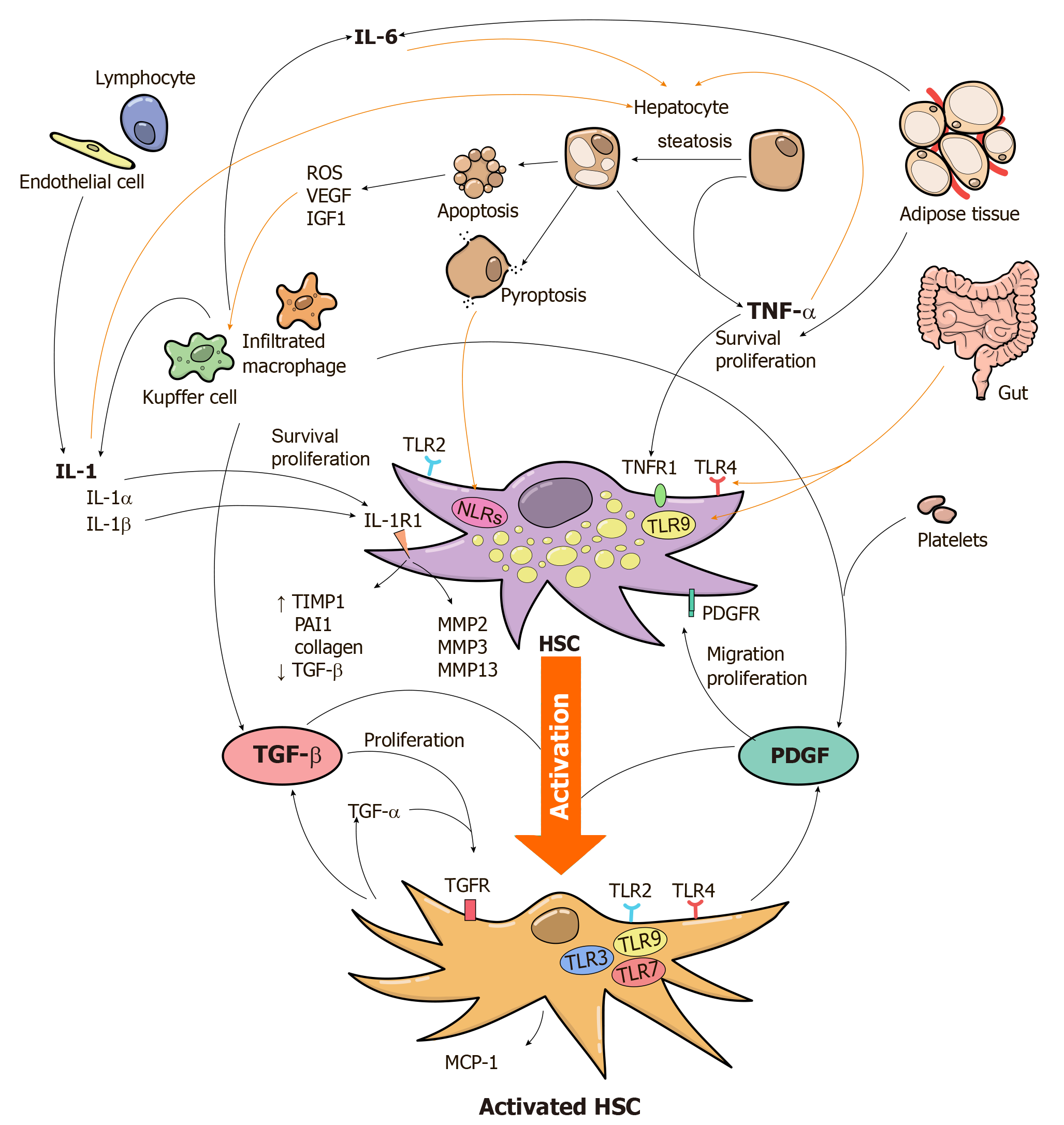
A plethora of molecules and signaling pathways are involved in the inflammatory process that accompanies the development of liver fibrosis during NAFLD (Figure 1 and Table 1). Signal transduction pathways downstream of TLRs and NLRs are of considerable interest for the activation and perpetuation of the innate immune response implicated in the development of liver fibrosis during metabolic dysregulation and liver steatosis and understanding of the mechanisms and molecules involved therein may lead to novel approaches against the progression of steatosis into NASH or cirrhosis.
| Mediator | Expression in the liver | Function during NAFLD |
| TLR2 | Kupffer cells, HSCs | Promotion of fibrogenesis via activation of MAPK and NF-κB signaling pathways |
| TLR4 | Kupffer cells, HSCs | Induction of inflammation and fibrosis in a NF-κB-dependent way |
| ΤLR9 | Kupffer cells, HSCs | HSC differentiation, secretion of IL-1β from Kupffer cells and MCP-1 from HSCs |
| NLRs | Innate immune cells hepatocytes, endothelial cells and HSCs | NAFLD and NASH development via inflammasome activation and release of IL-1β and IL-18 |
| TNF-α | Kupffer cells, hepatocytes | Promotion of liver fibrosis by inducing the survival and proliferation of HSCs |
| IL-1α/ IL-1β | Kupffer cells | Stimulation of hepatocyte lipid accumulation and induction of fibrosis via MMP production and suppression of PPARα in HSCs |
| IL-6 | Immune cells, Kupffer cells | Induction of hepatic lipogenesis in a Stat-3 dependent way |
| TGF-β | Kupffer cells, endothelial cells, HSCs | Induction of HSC activation and proliferation mainly via TGF-β-SMAD pathway |
| PDGF | Kupffer cells, activated HSCs, platelets | Induction of HSC migration, activation and proliferation via Ras-MAPK pathway |
The current strategy for the treatment of fibrosis is based on the modification of lifestyle factors, such as reduction of body weight in combination with exercise and healthy nutrition, as well as pharmaceutical improvement of insulin resistance. Specifically, a 3%-5% reduction of body weight alleviates steatosis; a greater reduction improves histopathological findings of NASH and fibrosis[5]. Metformin is not officially prescribed for NASH; pioglitazone induces histological changes in patients with or without diabetes mellitus, while there is no sufficient evidence for the use of GLP-1 agonists[5]. Several preclinical studies, predominantly in mouse models of fibrosis and NASH, provide innovative approaches for the management of inflammatory process during NAFLD-related fibrosis. For instance, the suppression of NLRP3 inflammasome by the pharmacological agent sulforaphane improved aspects of high-fat diet induced NAFLD in mice[159]. Similarly, administration of the selective NLRP3 inhibitor MCC950 in mice improved hepatic inflammation and fibrosis in two different models of NASH[75]. In addition, PDGF-B inhibition in mice led to attenuation of liver fibrosis[134,135], while strategies aiming the downregulation of PDGF such as pioglitazone can be part of the therapeutic strategy in NAFLD[160].
Apart from the necessity for identifying novel therapies against NASH, there is a need for the development of new, reliable, safe and less invasive diagnostic methods sensitive enough to detect NAFLD even at its initial stage, where it is thought to be reversible and benign. Currently a liver biopsy is considered the gold standard for the diagnostic confirmation and estimation of disease severity, as well as for the discrimination between NAFLD and NASH. Less invasive methods include blood tests of liver function, ultrasound, and proton magnetic resonance spectroscopy (H-MRS)[161]. Only cytokeratin-18 released during cell apoptosis and cell death can be used as a measure for histological changes, but it lacks specificity and sensitivity[161]. Other serum biomarkers under investigation include TGF-β and the associated markers R58 and L59/LAP-DPs; these are produced by the cleavage of Latency-associated protein (LAP) which is the pro-peptide of TGF-β[162,163].
Overall, metabolic inflammation is thought to be the causal mechanistic link for the progression of steatosis into NASH and scrutinization of the implicating factors may pave the way for the development of new diagnostic tools and therapeutic strategies for the prevention or treatment of the disease.
Manuscript source: Invited Manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Greece
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Esmat S, Gumerova A, Sitkin S S-Editor: Wang J L-Editor: A E-Editor: Ma YJ
| 1. | Angulo P, Lindor KD. Non-alcoholic fatty liver disease. J Gastroenterol Hepatol. 2002;17 Suppl:S186-S190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 311] [Cited by in RCA: 302] [Article Influence: 13.1] [Reference Citation Analysis (1)] |
| 2. | Ray K. NAFLD-the next global epidemic. Nat Rev Gastroenterol Hepatol. 2013;10:621. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 76] [Article Influence: 6.3] [Reference Citation Analysis (1)] |
| 3. | Papatheodoridi AM, Chrysavgis L, Koutsilieris M, Chatzigeorgiou A. The Role of Senescence in the Development of Nonalcoholic Fatty Liver Disease and Progression to Nonalcoholic Steatohepatitis. Hepatology. 2020;71:363-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 148] [Article Influence: 29.6] [Reference Citation Analysis (1)] |
| 4. | Ibrahim SH, Hirsova P, Gores GJ. Non-alcoholic steatohepatitis pathogenesis: sublethal hepatocyte injury as a driver of liver inflammation. Gut. 2018;67:963-972. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 208] [Article Influence: 29.7] [Reference Citation Analysis (1)] |
| 5. | Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, Harrison SA, Brunt EM, Sanyal AJ. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67:328-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3544] [Cited by in RCA: 4954] [Article Influence: 707.7] [Reference Citation Analysis (9)] |
| 6. | Koyama Y, Brenner DA. Liver inflammation and fibrosis. J Clin Invest. 2017;127:55-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 548] [Cited by in RCA: 913] [Article Influence: 114.1] [Reference Citation Analysis (0)] |
| 7. | Kleiner DE, Brunt EM, Van Natta M, Behling C, Contos MJ, Cummings OW, Ferrell LD, Liu YC, Torbenson MS, Unalp-Arida A, Yeh M, McCullough AJ, Sanyal AJ; Nonalcoholic Steatohepatitis Clinical Research Network. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41:1313-1321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6807] [Cited by in RCA: 8248] [Article Influence: 412.4] [Reference Citation Analysis (5)] |
| 8. | Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, Charlton M, Sanyal AJ; American Association for the Study of Liver Diseases; American College of Gastroenterology; American Gastroenterological Association. The diagnosis and management of non-alcoholic fatty liver disease: Practice guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Am J Gastroenterol. 2012;107:811-826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 270] [Cited by in RCA: 305] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 9. | Basaranoglu M, Turhan N, Sonsuz A, Basaranoglu G. Mallory-Denk Bodies in chronic hepatitis. World J Gastroenterol. 2011;17:2172-2177. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 25] [Cited by in RCA: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Borkham-Kamphorst E, Weiskirchen R. The PDGF system and its antagonists in liver fibrosis. Cytokine Growth Factor Rev. 2016;28:53-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 128] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 11. | Lee YA, Wallace MC, Friedman SL. Pathobiology of liver fibrosis: a translational success story. Gut. 2015;64:830-841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 601] [Cited by in RCA: 701] [Article Influence: 70.1] [Reference Citation Analysis (0)] |
| 12. | Iwaisako K, Jiang C, Zhang M, Cong M, Moore-Morris TJ, Park TJ, Liu X, Xu J, Wang P, Paik YH, Meng F, Asagiri M, Murray LA, Hofmann AF, Iida T, Glass CK, Brenner DA, Kisseleva T. Origin of myofibroblasts in the fibrotic liver in mice. Proc Natl Acad Sci USA. 2014;111:E3297-E3305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 309] [Cited by in RCA: 408] [Article Influence: 37.1] [Reference Citation Analysis (0)] |
| 13. | Friedman SL. Hepatic stellate cells: protean, multifunctional, and enigmatic cells of the liver. Physiol Rev. 2008;88:125-172. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2244] [Cited by in RCA: 2201] [Article Influence: 129.5] [Reference Citation Analysis (0)] |
| 14. | Arriazu E, Ruiz de Galarreta M, Cubero FJ, Varela-Rey M, Pérez de Obanos MP, Leung TM, Lopategi A, Benedicto A, Abraham-Enachescu I, Nieto N. Extracellular matrix and liver disease. Antioxid Redox Signal. 2014;21:1078-1097. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 125] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 15. | Nati M, Haddad D, Birkenfeld AL, Koch CA, Chavakis T, Chatzigeorgiou A. The role of immune cells in metabolism-related liver inflammation and development of non-alcoholic steatohepatitis (NASH). Rev Endocr Metab Disord. 2016;17:29-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 108] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 16. | Schuppan D. Structure of the extracellular matrix in normal and fibrotic liver: collagens and glycoproteins. Semin Liver Dis. 1990;10:1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 259] [Cited by in RCA: 239] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 17. | Friedman SL. Liver fibrosis -- from bench to bedside. J Hepatol. 2003;38 Suppl 1:S38-S53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1199] [Cited by in RCA: 1295] [Article Influence: 58.9] [Reference Citation Analysis (0)] |
| 18. | Buzzetti E, Pinzani M, Tsochatzis EA. The multiple-hit pathogenesis of non-alcoholic fatty liver disease (NAFLD). Metabolism. 2016;1038-1048. [DOI] [Full Text] |
| 19. | Schuppan D, Surabattula R, Wang XY. Determinants of fibrosis progression and regression in NASH. J Hepatol. 2018;68:238-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 258] [Cited by in RCA: 373] [Article Influence: 53.3] [Reference Citation Analysis (0)] |
| 20. | Yamada K, Mizukoshi E, Sunagozaka H, Arai K, Yamashita T, Takeshita Y, Misu H, Takamura T, Kitamura S, Zen Y, Nakanuma Y, Honda M, Kaneko S. Characteristics of hepatic fatty acid compositions in patients with nonalcoholic steatohepatitis. Liver Int. 2015;35:582-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 101] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 21. | Luedde T, Kaplowitz N, Schwabe RF. Cell death and cell death responses in liver disease: mechanisms and clinical relevance. Gastroenterology. 2014;147:765-783.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 456] [Cited by in RCA: 575] [Article Influence: 52.3] [Reference Citation Analysis (0)] |
| 22. | EL Andaloussi S, Mäger I, Breakefield XO, Wood MJ. Extracellular vesicles: biology and emerging therapeutic opportunities. Nat Rev Drug Discov. 2013;12:347-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1956] [Cited by in RCA: 2580] [Article Influence: 215.0] [Reference Citation Analysis (0)] |
| 23. | Hirsova P, Gores GJ. Death Receptor-Mediated Cell Death and Proinflammatory Signaling in Nonalcoholic Steatohepatitis. Cell Mol Gastroenterol Hepatol. 2015;1:17-27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 127] [Cited by in RCA: 161] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 24. | Canbay A, Feldstein AE, Higuchi H, Werneburg N, Grambihler A, Bronk SF, Gores GJ. Kupffer cell engulfment of apoptotic bodies stimulates death ligand and cytokine expression. Hepatology. 2003;38:1188-1198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 364] [Cited by in RCA: 352] [Article Influence: 16.0] [Reference Citation Analysis (1)] |
| 25. | Pellicoro A, Ramachandran P, Iredale JP, Fallowfield JA. Liver fibrosis and repair: immune regulation of wound healing in a solid organ. Nat Rev Immunol. 2014;14:181-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 777] [Cited by in RCA: 1005] [Article Influence: 91.4] [Reference Citation Analysis (0)] |
| 26. | Kirpich IA, Marsano LS, McClain CJ. Gut-liver axis, nutrition, and non-alcoholic fatty liver disease. Clin Biochem. 2015;48:923-930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 233] [Article Influence: 23.3] [Reference Citation Analysis (0)] |
| 27. | Pradere JP, Troeger JS, Dapito DH, Mencin AA, Schwabe RF. Toll-like receptor 4 and hepatic fibrogenesis. Semin Liver Dis. 2010;30:232-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 119] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 28. | Schwenger KJ, Clermont-Dejean N, Allard JP. The role of the gut microbiome in chronic liver disease: the clinical evidence revised. JHEP Rep. 2019;1:214-226. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 95] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 29. | Parola M, Robino G. Oxidative stress-related molecules and liver fibrosis. J Hepatol. 2001;35:297-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 541] [Cited by in RCA: 562] [Article Influence: 23.4] [Reference Citation Analysis (1)] |
| 30. | Ipsen DH, Lykkesfeldt J, Tveden-Nyborg P. Molecular mechanisms of hepatic lipid accumulation in non-alcoholic fatty liver disease. Cell Mol Life Sci. 2018;75:3313-3327. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 795] [Cited by in RCA: 980] [Article Influence: 140.0] [Reference Citation Analysis (1)] |
| 31. | Marí M, Caballero F, Colell A, Morales A, Caballeria J, Fernandez A, Enrich C, Fernandez-Checa JC, García-Ruiz C. Mitochondrial free cholesterol loading sensitizes to TNF- and Fas-mediated steatohepatitis. Cell Metab. 2006;4:185-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 477] [Cited by in RCA: 487] [Article Influence: 25.6] [Reference Citation Analysis (0)] |
| 32. | Seki E, Schwabe RF. Hepatic inflammation and fibrosis: functional links and key pathways. Hepatology. 2015;61:1066-1079. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 548] [Cited by in RCA: 742] [Article Influence: 74.2] [Reference Citation Analysis (0)] |
| 33. | Murphy FR, Issa R, Zhou X, Ratnarajah S, Nagase H, Arthur MJ, Benyon C, Iredale JP. Inhibition of apoptosis of activated hepatic stellate cells by tissue inhibitor of metalloproteinase-1 is mediated via effects on matrix metalloproteinase inhibition: implications for reversibility of liver fibrosis. J Biol Chem. 2002;277:11069-11076. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 328] [Cited by in RCA: 344] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 34. | Chatzigeorgiou A, Chung KJ, Garcia-Martin R, Alexaki VI, Klotzsche-von Ameln A, Phieler J, Sprott D, Kanczkowski W, Tzanavari T, Bdeir M, Bergmann S, Cartellieri M, Bachmann M, Nikolakopoulou P, Androutsellis-Theotokis A, Siegert G, Bornstein SR, Muders MH, Boon L, Karalis KP, Lutgens E, Chavakis T. Dual role of B7 costimulation in obesity-related nonalcoholic steatohepatitis and metabolic dysregulation. Hepatology. 2014;60:1196-1210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 58] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 35. | Ganz M, Szabo G. Immune and inflammatory pathways in NASH. Hepatol Int. 2013;7 Suppl 2:771-781. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 120] [Cited by in RCA: 150] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 36. | Fujii H, Kawada N. Inflammation and fibrogenesis in steatohepatitis. J Gastroenterol. 2012;47:215-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 116] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 37. | Li J, Lee DS, Madrenas J. Evolving Bacterial Envelopes and Plasticity of TLR2-Dependent Responses: Basic Research and Translational Opportunities. Front Immunol. 2013;4:347. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 58] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 38. | Kiziltas S. Toll-like receptors in pathophysiology of liver diseases. World J Hepatol. 2016;8:1354-1369. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 96] [Cited by in RCA: 128] [Article Influence: 14.2] [Reference Citation Analysis (2)] |
| 39. | Lee CC, Avalos AM, Ploegh HL. Accessory molecules for Toll-like receptors and their function. Nat Rev Immunol. 2012;12:168-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 297] [Cited by in RCA: 319] [Article Influence: 24.5] [Reference Citation Analysis (0)] |
| 40. | Adachi O, Kawai T, Takeda K, Matsumoto M, Tsutsui H, Sakagami M, Nakanishi K, Akira S. Targeted Disruption of the MyD88 Gene Results in Loss of IL-1- and IL-18-Mediated Function. Immunity. 1998;143-150. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 41. | Brown J, Wang H, Hajishengallis GN, Martin M. TLR-signaling networks: an integration of adaptor molecules, kinases, and cross-talk. J Dent Res. 2011;90:417-427. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 441] [Cited by in RCA: 439] [Article Influence: 31.4] [Reference Citation Analysis (0)] |
| 42. | Miura K, Yang L, van Rooijen N, Brenner DA, Ohnishi H, Seki E. Toll-like receptor 2 and palmitic acid cooperatively contribute to the development of nonalcoholic steatohepatitis through inflammasome activation in mice. Hepatology. 2013;57:577-589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 230] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 43. | Ji L, Xue R, Tang W, Wu W, Hu T, Liu X, Peng X, Gu J, Chen S, Zhang S. Toll like receptor 2 knock-out attenuates carbon tetrachloride (CCl4)-induced liver fibrosis by downregulating MAPK and NF-κB signaling pathways. FEBS Lett. 2014;588:2095-2100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 45] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 44. | Szabo G, Velayudham A, Romics L, Mandrekar P. Modulation of non-alcoholic steatohepatitis by pattern recognition receptors in mice: the role of toll-like receptors 2 and 4. Alcohol Clin Exp Res. 2005;29:140S-145S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 112] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 45. | Guo J, Friedman SL. Toll-like receptor 4 signaling in liver injury and hepatic fibrogenesis. Fibrogenesis Tissue Repair. 2010;3:21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 195] [Cited by in RCA: 243] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 46. | Seki E, De Minicis S, Osterreicher CH, Kluwe J, Osawa Y, Brenner DA, Schwabe RF. TLR4 enhances TGF-beta signaling and hepatic fibrosis. Nat Med. 2007;13:1324-1332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1361] [Cited by in RCA: 1557] [Article Influence: 86.5] [Reference Citation Analysis (1)] |
| 47. | Broz P, Dixit VM. Inflammasomes: mechanism of assembly, regulation and signalling. Nat Rev Immunol. 2016;16:407-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1529] [Cited by in RCA: 2485] [Article Influence: 276.1] [Reference Citation Analysis (0)] |
| 48. | Weiskirchen R, Tacke F. Cellular and molecular functions of hepatic stellate cells in inflammatory responses and liver immunology. Hepatobiliary Surg Nutr. 2014;3:344-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 117] [Reference Citation Analysis (0)] |
| 49. | Liu J, Zhuang ZJ, Bian DX, Ma XJ, Xun YH, Yang WJ, Luo Y, Liu YL, Jia L, Wang Y, Zhu ML, Ye DW, Zhou G, Lou GQ, Shi JP. Toll-like receptor-4 signalling in the progression of non-alcoholic fatty liver disease induced by high-fat and high-fructose diet in mice. Clin Exp Pharmacol Physiol. 2014;41:482-488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 66] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 50. | Sharifnia T, Antoun J, Verriere TG, Suarez G, Wattacheril J, Wilson KT, Peek RM, Abumrad NN, Flynn CR. Hepatic TLR4 signaling in obese NAFLD. Am J Physiol Gastrointest Liver Physiol. 2015;309:G270-G278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 194] [Article Influence: 19.4] [Reference Citation Analysis (1)] |
| 51. | Singh R, Bullard J, Kalra M, Assefa S, Kaul AK, Vonfeldt K, Strom SC, Conrad RS, Sharp HL, Kaul R. Status of bacterial colonization, Toll-like receptor expression and nuclear factor-kappa B activation in normal and diseased human livers. Clin Immunol. 2011;138:41-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 42] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 52. | Latz E, Schoenemeyer A, Visintin A, Fitzgerald KA, Monks BG, Knetter CF, Lien E, Nilsen NJ, Espevik T, Golenbock DT. TLR9 signals after translocating from the ER to CpG DNA in the lysosome. Nat Immunol. 2004;5:190-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1011] [Cited by in RCA: 1061] [Article Influence: 50.5] [Reference Citation Analysis (0)] |
| 53. | An H, Xu H, Yu Y, Zhang M, Qi R, Yan X, Liu S, Wang W, Guo Z, Qin Z, Cao X. Up-regulation of TLR9 gene expression by LPS in mouse macrophages via activation of NF-kappaB, ERK and p38 MAPK signal pathways. Immunol Lett. 2002;81:165-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 95] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 54. | Watanabe A, Hashmi A, Gomes DA, Town T, Badou A, Flavell RA, Mehal WZ. Apoptotic hepatocyte DNA inhibits hepatic stellate cell chemotaxis via toll-like receptor 9. Hepatology. 2007;46:1509-1518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 207] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 55. | Miura K, Kodama Y, Inokuchi S, Schnabl B, Aoyama T, Ohnishi H, Olefsky JM, Brenner DA, Seki E. Toll-like receptor 9 promotes steatohepatitis by induction of interleukin-1beta in mice. Gastroenterology. 2010;139:323-34.e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 527] [Cited by in RCA: 623] [Article Influence: 41.5] [Reference Citation Analysis (0)] |
| 56. | Gäbele E, Mühlbauer M, Dorn C, Weiss TS, Froh M, Schnabl B, Wiest R, Schölmerich J, Obermeier F, Hellerbrand C. Role of TLR9 in hepatic stellate cells and experimental liver fibrosis. Biochem Biophys Res Commun. 2008;376:271-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 111] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 57. | Ozawa Y, Koto T, Shinoda H, Tsubota K. Vision Loss by Central Retinal Vein Occlusion After Kaatsu Training: A Case Report. Medicine (Baltimore). 2015;94:e1515. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 58. | Schroder K, Tschopp J. The inflammasomes. Cell. 2010;140:821-832. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3880] [Cited by in RCA: 4548] [Article Influence: 303.2] [Reference Citation Analysis (0)] |
| 59. | Ting JP, Lovering RC, Alnemri ES, Bertin J, Boss JM, Davis BK, Flavell RA, Girardin SE, Godzik A, Harton JA, Hoffman HM, Hugot JP, Inohara N, Mackenzie A, Maltais LJ, Nunez G, Ogura Y, Otten LA, Philpott D, Reed JC, Reith W, Schreiber S, Steimle V, Ward PA. The NLR gene family: a standard nomenclature. Immunity. 2008;28:285-287. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 770] [Cited by in RCA: 701] [Article Influence: 41.2] [Reference Citation Analysis (0)] |
| 60. | Conforti-Andreoni C, Ricciardi-Castagnoli P, Mortellaro A. The inflammasomes in health and disease: from genetics to molecular mechanisms of autoinflammation and beyond. Cell Mol Immunol. 2011;8:135-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 84] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 61. | Tattoli I, Carneiro LA, Jéhanno M, Magalhaes JG, Shu Y, Philpott DJ, Arnoult D, Girardin SE. NLRX1 is a mitochondrial NOD-like receptor that amplifies NF-kappaB and JNK pathways by inducing reactive oxygen species production. EMBO Rep. 2008;9:293-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 237] [Cited by in RCA: 266] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 62. | Kelley N, Jeltema D, Duan Y, He Y. The NLRP3 Inflammasome: An Overview of Mechanisms of Activation and Regulation. Int J Mol Sci. 2019;20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 925] [Cited by in RCA: 2378] [Article Influence: 396.3] [Reference Citation Analysis (0)] |
| 63. | Nagai-Singer MA, Morrison HA, Allen IC. NLRX1 Is a Multifaceted and Enigmatic Regulator of Immune System Function. Front Immunol. 2019;10:2419. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 57] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 64. | Malik A, Kanneganti TD. Inflammasome activation and assembly at a glance. J Cell Sci. 2017;130:3955-3963. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 340] [Cited by in RCA: 366] [Article Influence: 45.8] [Reference Citation Analysis (0)] |
| 65. | Swanson KV, Deng M, Ting JP. The NLRP3 inflammasome: molecular activation and regulation to therapeutics. Nat Rev Immunol. 2019;19:477-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1426] [Cited by in RCA: 3177] [Article Influence: 635.4] [Reference Citation Analysis (0)] |
| 66. | Cookson BT, Brennan MA. Pro-inflammatory programmed cell death. Trends Microbiol. 2001;9:113-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 671] [Cited by in RCA: 1019] [Article Influence: 42.5] [Reference Citation Analysis (0)] |
| 67. | Jo EK, Kim JK, Shin DM, Sasakawa C. Molecular mechanisms regulating NLRP3 inflammasome activation. Cell Mol Immunol. 2016;13:148-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 708] [Cited by in RCA: 1040] [Article Influence: 104.0] [Reference Citation Analysis (0)] |
| 68. | Liu X, Zhang Z, Ruan J, Pan Y, Magupalli VG, Wu H, Lieberman J. Inflammasome-activated gasdermin D causes pyroptosis by forming membrane pores. Nature. 2016;535:153-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2315] [Cited by in RCA: 2353] [Article Influence: 261.4] [Reference Citation Analysis (0)] |
| 69. | Szabo G, Csak T. Inflammasomes in liver diseases. J Hepatol. 2012;57:642-654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 339] [Cited by in RCA: 404] [Article Influence: 31.1] [Reference Citation Analysis (0)] |
| 70. | Csak T, Ganz M, Pespisa J, Kodys K, Dolganiuc A, Szabo G. Fatty acid and endotoxin activate inflammasomes in mouse hepatocytes that release danger signals to stimulate immune cells. Hepatology. 2011;54:133-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 442] [Cited by in RCA: 534] [Article Influence: 38.1] [Reference Citation Analysis (0)] |
| 71. | Boaru SG, Borkham-Kamphorst E, Tihaa L, Haas U, Weiskirchen R. Expression analysis of inflammasomes in experimental models of inflammatory and fibrotic liver disease. J Inflamm (Lond). 2012;9:49. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 88] [Cited by in RCA: 116] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 72. | Cai C, Zhu X, Li P, Li J, Gong J, Shen W, He K. NLRP3 Deletion Inhibits the Non-alcoholic Steatohepatitis Development and Inflammation in Kupffer Cells Induced by Palmitic Acid. Inflammation. 2017;40:1875-1883. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 67] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 73. | Stienstra R, van Diepen JA, Tack CJ, Zaki MH, van de Veerdonk FL, Perera D, Neale GA, Hooiveld GJ, Hijmans A, Vroegrijk I, van den Berg S, Romijn J, Rensen PC, Joosten LA, Netea MG, Kanneganti TD. Inflammasome is a central player in the induction of obesity and insulin resistance. Proc Natl Acad Sci USA. 2011;108:15324-15329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 485] [Cited by in RCA: 581] [Article Influence: 41.5] [Reference Citation Analysis (0)] |
| 74. | Wree A, Eguchi A, McGeough MD, Pena CA, Johnson CD, Canbay A, Hoffman HM, Feldstein AE. NLRP3 inflammasome activation results in hepatocyte pyroptosis, liver inflammation, and fibrosis in mice. Hepatology. 2014;59:898-910. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 687] [Cited by in RCA: 762] [Article Influence: 69.3] [Reference Citation Analysis (0)] |
| 75. | Mridha AR, Wree A, Robertson AAB, Yeh MM, Johnson CD, Van Rooyen DM, Haczeyni F, Teoh NC, Savard C, Ioannou GN, Masters SL, Schroder K, Cooper MA, Feldstein AE, Farrell GC. NLRP3 inflammasome blockade reduces liver inflammation and fibrosis in experimental NASH in mice. J Hepatol. 2017;66:1037-1046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 546] [Cited by in RCA: 830] [Article Influence: 103.8] [Reference Citation Analysis (0)] |
| 76. | Baroja-Mazo A, Martín-Sánchez F, Gomez AI, Martínez CM, Amores-Iniesta J, Compan V, Barberà-Cremades M, Yagüe J, Ruiz-Ortiz E, Antón J, Buján S, Couillin I, Brough D, Arostegui JI, Pelegrín P. The NLRP3 inflammasome is released as a particulate danger signal that amplifies the inflammatory response. Nat Immunol. 2014;15:738-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 538] [Cited by in RCA: 639] [Article Influence: 58.1] [Reference Citation Analysis (0)] |
| 77. | Franklin BS, Bossaller L, De Nardo D, Ratter JM, Stutz A, Engels G, Brenker C, Nordhoff M, Mirandola SR, Al-Amoudi A, Mangan MS, Zimmer S, Monks BG, Fricke M, Schmidt RE, Espevik T, Jones B, Jarnicki AG, Hansbro PM, Busto P, Marshak-Rothstein A, Hornemann S, Aguzzi A, Kastenmüller W, Latz E. The adaptor ASC has extracellular and 'prionoid' activities that propagate inflammation. Nat Immunol. 2014;15:727-737. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 600] [Cited by in RCA: 618] [Article Influence: 56.2] [Reference Citation Analysis (0)] |
| 78. | Fève B, Bastard JP. The role of interleukins in insulin resistance and type 2 diabetes mellitus. Nat Rev Endocrinol. 2009;5:305-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 252] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 79. | Vandanmagsar B, Youm YH, Ravussin A, Galgani JE, Stadler K, Mynatt RL, Ravussin E, Stephens JM, Dixit VD. The NLRP3 inflammasome instigates obesity-induced inflammation and insulin resistance. Nat Med. 2011;17:179-188. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2148] [Cited by in RCA: 2053] [Article Influence: 146.6] [Reference Citation Analysis (0)] |
| 80. | Watanabe A, Sohail MA, Gomes DA, Hashmi A, Nagata J, Sutterwala FS, Mahmood S, Jhandier MN, Shi Y, Flavell RA, Mehal WZ. Inflammasome-mediated regulation of hepatic stellate cells. Am J Physiol Gastrointest Liver Physiol. 2009;296:G1248-G1257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 191] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 81. | Chung KJ, Nati M, Chavakis T, Chatzigeorgiou A. Innate immune cells in the adipose tissue. Rev Endocr Metab Disord. 2018;19:283-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 58] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 82. | Chatzigeorgiou A, Kandaraki E, Papavassiliou AG, Koutsilieris M. Peripheral targets in obesity treatment: a comprehensive update. Obes Rev. 2014;15:487-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 83. | Tsukamoto H. Cytokine regulation of hepatic stellate cells in liver fibrosis. Alcohol Clin Exp Res. 1999;23:911-916. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 112] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 84. | Crespo J, Cayón A, Fernández-Gil P, Hernández-Guerra M, Mayorga M, Domínguez-Díez A, Fernández-Escalante JC, Pons-Romero F. Gene expression of tumor necrosis factor alpha and TNF-receptors, p55 and p75, in nonalcoholic steatohepatitis patients. Hepatology. 2001;34:1158-1163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 485] [Cited by in RCA: 503] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 85. | Lesmana CR, Hasan I, Budihusodo U, Gani RA, Krisnuhoni E, Akbar N, Lesmana LA. Diagnostic value of a group of biochemical markers of liver fibrosis in patients with non-alcoholic steatohepatitis. J Dig Dis. 2009;10:201-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 53] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 86. | Jiang JX, Chen X, Fukada H, Serizawa N, Devaraj S, Török NJ. Advanced glycation endproducts induce fibrogenic activity in nonalcoholic steatohepatitis by modulating TNF-α-converting enzyme activity in mice. Hepatology. 2013;58:1339-1348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 87. | Schwabe RF, Brenner DA. Mechanisms of Liver Injury. I. TNF-alpha-induced liver injury: role of IKK, JNK, and ROS pathways. Am J Physiol Gastrointest Liver Physiol. 2006;290:G583-G589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 494] [Cited by in RCA: 561] [Article Influence: 29.5] [Reference Citation Analysis (0)] |
| 88. | Braunersreuther V, Viviani GL, Mach F, Montecucco F. Role of cytokines and chemokines in non-alcoholic fatty liver disease. World J Gastroenterol. 2012;18:727-735. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 282] [Cited by in RCA: 272] [Article Influence: 20.9] [Reference Citation Analysis (0)] |
| 89. | Tomita K, Tamiya G, Ando S, Ohsumi K, Chiyo T, Mizutani A, Kitamura N, Toda K, Kaneko T, Horie Y, Han JY, Kato S, Shimoda M, Oike Y, Tomizawa M, Makino S, Ohkura T, Saito H, Kumagai N, Nagata H, Ishii H, Hibi T. Tumour necrosis factor alpha signalling through activation of Kupffer cells plays an essential role in liver fibrosis of non-alcoholic steatohepatitis in mice. Gut. 2006;55:415-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 318] [Cited by in RCA: 352] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 90. | Osawa Y, Hoshi M, Yasuda I, Saibara T, Moriwaki H, Kozawa O. Tumor necrosis factor-α promotes cholestasis-induced liver fibrosis in the mouse through tissue inhibitor of metalloproteinase-1 production in hepatic stellate cells. PLoS One. 2013;8:e65251. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 73] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 91. | Tarrats N, Moles A, Morales A, García-Ruiz C, Fernández-Checa JC, Marí M. Critical role of tumor necrosis factor receptor 1, but not 2, in hepatic stellate cell proliferation, extracellular matrix remodeling, and liver fibrogenesis. Hepatology. 2011;54:319-327. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 107] [Cited by in RCA: 107] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 92. | Mirea AM, Tack CJ, Chavakis T, Joosten LAB, Toonen EJM. IL-1 Family Cytokine Pathways Underlying NAFLD: Towards New Treatment Strategies. Trends Mol Med. 2018;24:458-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 100] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 93. | Kamari Y, Shaish A, Vax E, Shemesh S, Kandel-Kfir M, Arbel Y, Olteanu S, Barshack I, Dotan S, Voronov E, Dinarello CA, Apte RN, Harats D. Lack of interleukin-1α or interleukin-1β inhibits transformation of steatosis to steatohepatitis and liver fibrosis in hypercholesterolemic mice. J Hepatol. 2011;55:1086-1094. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 241] [Cited by in RCA: 239] [Article Influence: 17.1] [Reference Citation Analysis (0)] |
| 94. | Stienstra R, Saudale F, Duval C, Keshtkar S, Groener JE, van Rooijen N, Staels B, Kersten S, Müller M. Kupffer cells promote hepatic steatosis via interleukin-1beta-dependent suppression of peroxisome proliferator-activated receptor alpha activity. Hepatology. 2010;51:511-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 326] [Cited by in RCA: 370] [Article Influence: 24.7] [Reference Citation Analysis (0)] |
| 95. | Tang N, Zhang YP, Ying W, Yao XX. Interleukin-1β upregulates matrix metalloproteinase-13 gene expression via c-Jun N-terminal kinase and p38 MAPK pathways in rat hepatic stellate cells. Mol Med Rep. 2013;8:1861-1865. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 96. | de Roos B, Rungapamestry V, Ross K, Rucklidge G, Reid M, Duncan G, Horgan G, Toomey S, Browne J, Loscher CE, Mills KH, Roche HM. Attenuation of inflammation and cellular stress-related pathways maintains insulin sensitivity in obese type I interleukin-1 receptor knockout mice on a high-fat diet. Proteomics. 2009;9:3244-3256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 40] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 97. | Gieling RG, Wallace K, Han YP. Interleukin-1 participates in the progression from liver injury to fibrosis. Am J Physiol Gastrointest Liver Physiol. 2009;296:G1324-G1331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 188] [Cited by in RCA: 225] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 98. | Niederreiter L, Tilg H. Cytokines and fatty liver diseases. Liver Research. 2018;2:14-20. [RCA] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 78] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 99. | Isoda K, Sawada S, Ayaori M, Matsuki T, Horai R, Kagata Y, Miyazaki K, Kusuhara M, Okazaki M, Matsubara O, Iwakura Y, Ohsuzu F. Deficiency of interleukin-1 receptor antagonist deteriorates fatty liver and cholesterol metabolism in hypercholesterolemic mice. J Biol Chem. 2005;280:7002-7009. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 76] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 100. | Pihlajamäki J, Kuulasmaa T, Kaminska D, Simonen M, Kärjä V, Grönlund S, Käkelä P, Pääkkönen M, Kainulainen S, Punnonen K, Kuusisto J, Gylling H, Laakso M. Serum interleukin 1 receptor antagonist as an independent marker of non-alcoholic steatohepatitis in humans. J Hepatol. 2012;56:663-670. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 87] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 101. | Bastard JP, Maachi M, Van Nhieu JT, Jardel C, Bruckert E, Grimaldi A, Robert JJ, Capeau J, Hainque B. Adipose tissue IL-6 content correlates with resistance to insulin activation of glucose uptake both in vivo and in vitro. J Clin Endocrinol Metab. 2002;87:2084-2089. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 295] [Cited by in RCA: 339] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 102. | Anty R, Bekri S, Luciani N, Saint-Paul MC, Dahman M, Iannelli A, Amor IB, Staccini-Myx A, Huet PM, Gugenheim J, Sadoul JL, Le Marchand-Brustel Y, Tran A, Gual P. The inflammatory C-reactive protein is increased in both liver and adipose tissue in severely obese patients independently from metabolic syndrome, Type 2 diabetes, and NASH. Am J Gastroenterol. 2006;101:1824-1833. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 140] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 103. | Wieckowska A, Papouchado BG, Li Z, Lopez R, Zein NN, Feldstein AE. Increased hepatic and circulating interleukin-6 levels in human nonalcoholic steatohepatitis. Am J Gastroenterol. 2008;103:1372-1379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 395] [Cited by in RCA: 444] [Article Influence: 26.1] [Reference Citation Analysis (0)] |
| 104. | García-Galiano D, Sánchez-Garrido MA, Espejo I, Montero JL, Costán G, Marchal T, Membrives A, Gallardo-Valverde JM, Muñoz-Castañeda JR, Arévalo E, De la Mata M, Muntané J. IL-6 and IGF-1 are independent prognostic factors of liver steatosis and non-alcoholic steatohepatitis in morbidly obese patients. Obes Surg. 2007;17:493-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 85] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 105. | Jorge ASB, Andrade JMO, Paraíso AF, Jorge GCB, Silveira CM, de Souza LR, Santos EP, Guimaraes ALS, Santos SHS, De-Paula AMB. Body mass index and the visceral adipose tissue expression of IL-6 and TNF-alpha are associated with the morphological severity of non-alcoholic fatty liver disease in individuals with class III obesity. Obes Res Clin Pract. 2018;12:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 106. | Kugelmas M, Hill DB, Vivian B, Marsano L, McClain CJ. Cytokines and NASH: a pilot study of the effects of lifestyle modification and vitamin E. Hepatology. 2003;38:413-419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 375] [Cited by in RCA: 362] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 107. | Wallenius V, Wallenius K, Ahrén B, Rudling M, Carlsten H, Dickson SL, Ohlsson C, Jansson JO. Interleukin-6-deficient mice develop mature-onset obesity. Nat Med. 2002;8:75-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 874] [Cited by in RCA: 901] [Article Influence: 39.2] [Reference Citation Analysis (0)] |
| 108. | Yamaguchi K, Itoh Y, Yokomizo C, Nishimura T, Niimi T, Fujii H, Okanoue T, Yoshikawa T. Blockade of interleukin-6 signaling enhances hepatic steatosis but improves liver injury in methionine choline-deficient diet-fed mice. Lab Invest. 2010;90:1169-1178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 103] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 109. | Vida M, Gavito AL, Pavón FJ, Bautista D, Serrano A, Suarez J, Arrabal S, Decara J, Romero-Cuevas M, Rodríguez de Fonseca F, Baixeras E. Chronic administration of recombinant IL-6 upregulates lipogenic enzyme expression and aggravates high-fat-diet-induced steatosis in IL-6-deficient mice. Dis Model Mech. 2015;8:721-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 32] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 110. | von Loeffelholz C, Lieske S, Neuschäfer-Rube F, Willmes DM, Raschzok N, Sauer IM, König J, Fromm MF, Horn P, Chatzigeorgiou A, Pathe-Neuschäfer-Rube A, Jordan J, Pfeiffer AFH, Mingrone G, Bornstein SR, Stroehle P, Harms C, Wunderlich FT, Helfand SL, Bernier M, de Cabo R, Shulman GI, Chavakis T, Püschel GP, Birkenfeld AL. The human longevity gene homolog INDY and interleukin-6 interact in hepatic lipid metabolism. Hepatology. 2017;66:616-630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 55] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 111. | Fabregat I, Moreno-Càceres J, Sánchez A, Dooley S, Dewidar B, Giannelli G, Ten Dijke P; IT-LIVER Consortium. TGF-β signalling and liver disease. FEBS J. 2016;283:2219-2232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 319] [Cited by in RCA: 481] [Article Influence: 53.4] [Reference Citation Analysis (0)] |
| 112. | Dewidar B, Meyer C, Dooley S, Meindl-Beinker AN. TGF-β in Hepatic Stellate Cell Activation and Liver Fibrogenesis-Updated 2019. Cells. 2019;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 214] [Cited by in RCA: 543] [Article Influence: 90.5] [Reference Citation Analysis (0)] |
| 113. | De Bleser PJ, Niki T, Rogiers V, Geerts A. Transforming growth factor-beta gene expression in normal and fibrotic rat liver. J Hepatol. 1997;26:886-893. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 132] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 114. | Wang J, Leclercq I, Brymora JM, Xu N, Ramezani-Moghadam M, London RM, Brigstock D, George J. Kupffer cells mediate leptin-induced liver fibrosis. Gastroenterology. 2009;137:713-723. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 153] [Cited by in RCA: 159] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 115. | Annoni G, Weiner FR, Zern MA. Increased transforming growth factor-beta 1 gene expression in human liver disease. J Hepatol. 1992;14:259-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 89] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 116. | Klein S, Mittendorfer B, Eagon JC, Patterson B, Grant L, Feirt N, Seki E, Brenner D, Korenblat K, McCrea J. Gastric bypass surgery improves metabolic and hepatic abnormalities associated with nonalcoholic fatty liver disease. Gastroenterology. 2006;130:1564-1572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 237] [Cited by in RCA: 201] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 117. | Cayón A, Crespo J, Mayorga M, Guerra A, Pons-Romero F. Increased expression of Ob-Rb and its relationship with the overexpression of TGF-beta1 and the stage of fibrosis in patients with nonalcoholic steatohepatitis. Liver Int. 2006;26:1065-1071. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 39] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 118. | Hasegawa T, Yoneda M, Nakamura K, Makino I, Terano A. Plasma transforming growth factor-beta1 level and efficacy of alpha-tocopherol in patients with non-alcoholic steatohepatitis: a pilot study. Aliment Pharmacol Ther. 2001;15:1667-1672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 299] [Cited by in RCA: 280] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 119. | Tarantino G, Conca P, Riccio A, Tarantino M, Di Minno MN, Chianese D, Pasanisi F, Contaldo F, Scopacasa F, Capone D. Enhanced serum concentrations of transforming growth factor-beta1 in simple fatty liver: is it really benign? J Transl Med. 2008;6:72. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 70] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 120. | Sepúlveda-Flores RN, Vera-Cabrera L, Flores-Gutiérrez JP, Maldonado-Garza H, Salinas-Garza R, Zorrilla-Blanco P, Bosques-Padilla FJ. Obesity-related non-alcoholic steatohepatitis and TGF-beta1 serum levels in relation to morbid obesity. Ann Hepatol. 2002;1:36-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 121. | Ajmera V, Perito ER, Bass NM, Terrault NA, Yates KP, Gill R, Loomba R, Diehl AM, Aouizerat BE; NASH Clinical Research Network. Novel plasma biomarkers associated with liver disease severity in adults with nonalcoholic fatty liver disease. Hepatology. 2017;65:65-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 132] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 122. | Czaja MJ, Flanders KC, Biempica L, Klein C, Zern MA, Weiner FR. Expression of tumor necrosis factor-alpha and transforming growth factor-beta 1 in acute liver injury. Growth Factors. 1989;1:219-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 62] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 123. | Niu L, Cui X, Qi Y, Xie D, Wu Q, Chen X, Ge J, Liu Z. Involvement of TGF-β1/Smad3 Signaling in Carbon Tetrachloride-Induced Acute Liver Injury in Mice. PLoS One. 2016;11:e0156090. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 44] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 124. | Hellerbrand C, Stefanovic B, Giordano F, Burchardt ER, Brenner DA. The role of TGFbeta1 in initiating hepatic stellate cell activation in vivo. J Hepatol. 1999;30:77-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 279] [Cited by in RCA: 317] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 125. | Tan CK, Leuenberger N, Tan MJ, Yan YW, Chen Y, Kambadur R, Wahli W, Tan NS. Smad3 deficiency in mice protects against insulin resistance and obesity induced by a high-fat diet. Diabetes. 2011;60:464-476. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 104] [Cited by in RCA: 125] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 126. | Yang L, Roh YS, Song J, Zhang B, Liu C, Loomba R, Seki E. Transforming growth factor beta signaling in hepatocytes participates in steatohepatitis through regulation of cell death and lipid metabolism in mice. Hepatology. 2014;59:483-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 216] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 127. | Yadav H, Quijano C, Kamaraju AK, Gavrilova O, Malek R, Chen W, Zerfas P, Zhigang D, Wright EC, Stuelten C, Sun P, Lonning S, Skarulis M, Sumner AE, Finkel T, Rane SG. Protection from obesity and diabetes by blockade of TGF-β/Smad3 signaling. Cell Metab. 2011;14:67-79. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 575] [Cited by in RCA: 564] [Article Influence: 40.3] [Reference Citation Analysis (0)] |
| 128. | Ying HZ, Chen Q, Zhang WY, Zhang HH, Ma Y, Zhang SZ, Fang J, Yu CH. PDGF signaling pathway in hepatic fibrosis pathogenesis and therapeutics (Review). Mol Med Rep. 2017;16:7879-7889. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 188] [Cited by in RCA: 170] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 129. | Failli P, Ruocco C, De Franco R, Caligiuri A, Gentilini A, Giotti A, Gentilini P, Pinzani M. The mitogenic effect of platelet-derived growth factor in human hepatic stellate cells requires calcium influx. Am J Physiol. 1995;269:C1133-C1139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 49] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 130. | Borkham-Kamphorst E, Meurer SK, Van de Leur E, Haas U, Tihaa L, Weiskirchen R. PDGF-D signaling in portal myofibroblasts and hepatic stellate cells proves identical to PDGF-B via both PDGF receptor type α and β. Cell Signal. 2015;27:1305-1314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 131. | Thieringer F, Maass T, Czochra P, Klopcic B, Conrad I, Friebe D, Schirmacher P, Lohse AW, Blessing M, Galle PR, Teufel A, Kanzler S. Spontaneous hepatic fibrosis in transgenic mice overexpressing PDGF-A. Gene. 2008;423:23-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 47] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 132. | Campbell JS, Hughes SD, Gilbertson DG, Palmer TE, Holdren MS, Haran AC, Odell MM, Bauer RL, Ren HP, Haugen HS, Yeh MM, Fausto N. Platelet-derived growth factor C induces liver fibrosis, steatosis, and hepatocellular carcinoma. Proc Natl Acad Sci USA. 2005;102:3389-3394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 254] [Cited by in RCA: 270] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 133. | Czochra P, Klopcic B, Meyer E, Herkel J, Garcia-Lazaro JF, Thieringer F, Schirmacher P, Biesterfeld S, Galle PR, Lohse AW, Kanzler S. Liver fibrosis induced by hepatic overexpression of PDGF-B in transgenic mice. J Hepatol. 2006;45:419-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 196] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 134. | Borkham-Kamphorst E, Stoll D, Gressner AM, Weiskirchen R. Antisense strategy against PDGF B-chain proves effective in preventing experimental liver fibrogenesis. Biochem Biophys Res Commun. 2004;321:413-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 74] [Article Influence: 3.5] [Reference Citation Analysis (1)] |
| 135. | Hao ZM, Fan XB, Li S, Lv YF, Su HQ, Jiang HP, Li HH. Vaccination with platelet-derived growth factor B kinoids inhibits CCl₄-induced hepatic fibrosis in mice. J Pharmacol Exp Ther. 2012;342:835-842. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 136. | Abderrahmani A, Yengo L, Caiazzo R, Canouil M, Cauchi S, Raverdy V, Plaisance V, Pawlowski V, Lobbens S, Maillet J, Rolland L, Boutry R, Queniat G, Kwapich M, Tenenbaum M, Bricambert J, Saussenthaler S, Anthony E, Jha P, Derop J, Sand O, Rabearivelo I, Leloire A, Pigeyre M, Daujat-Chavanieu M, Gerbal-Chaloin S, Dayeh T, Lassailly G, Mathurin P, Staels B, Auwerx J, Schürmann A, Postic C, Schafmayer C, Hampe J, Bonnefond A, Pattou F, Froguel P. Increased Hepatic PDGF-AA Signaling Mediates Liver Insulin Resistance in Obesity-Associated Type 2 Diabetes. Diabetes. 2018;67:1310-1321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 71] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 137. | Wright JH, Johnson MM, Shimizu-Albergine M, Bauer RL, Hayes BJ, Surapisitchat J, Hudkins KL, Riehle KJ, Johnson SC, Yeh MM, Bammler TK, Beyer RP, Gilbertson DG, Alpers CE, Fausto N, Campbell JS. Paracrine activation of hepatic stellate cells in platelet-derived growth factor C transgenic mice: evidence for stromal induction of hepatocellular carcinoma. Int J Cancer. 2014;134:778-788. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 138. | Zhu L, Baker RD, Baker SS. Gut microbiome and nonalcoholic fatty liver diseases. Pediatr Res. 2015;77:245-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 109] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 139. | Jandhyala SM, Talukdar R, Subramanyam C, Vuyyuru H, Sasikala M, Nageshwar Reddy D. Role of the normal gut microbiota. World J Gastroenterol. 2015;21:8787-8803. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1421] [Cited by in RCA: 1839] [Article Influence: 183.9] [Reference Citation Analysis (58)] |
| 140. | Seki E, Schnabl B. Role of innate immunity and the microbiota in liver fibrosis: crosstalk between the liver and gut. J Physiol. 2012;590:447-458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 270] [Cited by in RCA: 340] [Article Influence: 24.3] [Reference Citation Analysis (0)] |
| 141. | Luther J, Garber JJ, Khalili H, Dave M, Bale SS, Jindal R, Motola DL, Luther S, Bohr S, Jeoung SW, Deshpande V, Singh G, Turner JR, Yarmush ML, Chung RT, Patel SJ. Hepatic Injury in Nonalcoholic Steatohepatitis Contributes to Altered Intestinal Permeability. Cell Mol Gastroenterol Hepatol. 2015;1:222-232. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 195] [Cited by in RCA: 217] [Article Influence: 21.7] [Reference Citation Analysis (0)] |
| 142. | Le Roy T, Llopis M, Lepage P, Bruneau A, Rabot S, Bevilacqua C, Martin P, Philippe C, Walker F, Bado A, Perlemuter G, Cassard-Doulcier AM, Gérard P. Intestinal microbiota determines development of non-alcoholic fatty liver disease in mice. Gut. 2013;62:1787-1794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 601] [Cited by in RCA: 715] [Article Influence: 59.6] [Reference Citation Analysis (0)] |
| 143. | Boursier J, Mueller O, Barret M, Machado M, Fizanne L, Araujo-Perez F, Guy CD, Seed PC, Rawls JF, David LA, Hunault G, Oberti F, Calès P, Diehl AM. The severity of nonalcoholic fatty liver disease is associated with gut dysbiosis and shift in the metabolic function of the gut microbiota. Hepatology. 2016;63:764-775. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 763] [Cited by in RCA: 1052] [Article Influence: 116.9] [Reference Citation Analysis (0)] |
| 144. | Kolodziejczyk AA, Zheng D, Shibolet O, Elinav E. The role of the microbiome in NAFLD and NASH. EMBO Mol Med. 2019;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 222] [Cited by in RCA: 395] [Article Influence: 65.8] [Reference Citation Analysis (0)] |
| 145. | Ji Y, Yin Y, Li Z, Zhang W. Gut Microbiota-Derived Components and Metabolites in the Progression of Non-Alcoholic Fatty Liver Disease (NAFLD). Nutrients. 2019;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 157] [Article Influence: 26.2] [Reference Citation Analysis (0)] |
| 146. | Cani PD, Amar J, Iglesias MA, Poggi M, Knauf C, Bastelica D, Neyrinck AM, Fava F, Tuohy KM, Chabo C, Waget A, Delmée E, Cousin B, Sulpice T, Chamontin B, Ferrières J, Tanti JF, Gibson GR, Casteilla L, Delzenne NM, Alessi MC, Burcelin R. Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes. 2007;56:1761-1772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4095] [Cited by in RCA: 4564] [Article Influence: 253.6] [Reference Citation Analysis (1)] |
| 147. | Schoeler M, Caesar R. Dietary lipids, gut microbiota and lipid metabolism. Rev Endocr Metab Disord. 2019;20:461-472. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 372] [Cited by in RCA: 744] [Article Influence: 124.0] [Reference Citation Analysis (0)] |
| 148. | Thuy S, Ladurner R, Volynets V, Wagner S, Strahl S, Königsrainer A, Maier KP, Bischoff SC, Bergheim I. Nonalcoholic fatty liver disease in humans is associated with increased plasma endotoxin and plasminogen activator inhibitor 1 concentrations and with fructose intake. J Nutr. 2008;138:1452-1455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 312] [Cited by in RCA: 309] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 149. | Laugerette F, Vors C, Géloën A, Chauvin MA, Soulage C, Lambert-Porcheron S, Peretti N, Alligier M, Burcelin R, Laville M, Vidal H, Michalski MC. Emulsified lipids increase endotoxemia: possible role in early postprandial low-grade inflammation. J Nutr Biochem. 2011;22:53-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 204] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 150. | Girardin SE, Boneca IG, Viala J, Chamaillard M, Labigne A, Thomas G, Philpott DJ, Sansonetti PJ. Nod2 is a general sensor of peptidoglycan through muramyl dipeptide (MDP) detection. J Biol Chem. 2003;278:8869-8872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1755] [Cited by in RCA: 1772] [Article Influence: 80.5] [Reference Citation Analysis (0)] |
| 151. | Jin M, Lai Y, Zhao P, Shen Q, Su W, Yin Y, Zhang W. Effects of peptidoglycan on the development of steatohepatitis. Biochim Biophys Acta Mol Cell Biol Lipids. 2020;1865:158595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 152. | Zhou D, Fan JG. Microbial metabolites in non-alcoholic fatty liver disease. World J Gastroenterol. 2019;25:2019-2028. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 71] [Cited by in RCA: 68] [Article Influence: 11.3] [Reference Citation Analysis (1)] |
| 153. | Macia L, Tan J, Vieira AT, Leach K, Stanley D, Luong S, Maruya M, Ian McKenzie C, Hijikata A, Wong C, Binge L, Thorburn AN, Chevalier N, Ang C, Marino E, Robert R, Offermanns S, Teixeira MM, Moore RJ, Flavell RA, Fagarasan S, Mackay CR. Metabolite-sensing receptors GPR43 and GPR109A facilitate dietary fibre-induced gut homeostasis through regulation of the inflammasome. Nat Commun. 2015;6:6734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 715] [Cited by in RCA: 1004] [Article Influence: 100.4] [Reference Citation Analysis (0)] |
| 154. | Furusawa Y, Obata Y, Fukuda S, Endo TA, Nakato G, Takahashi D, Nakanishi Y, Uetake C, Kato K, Kato T, Takahashi M, Fukuda NN, Murakami S, Miyauchi E, Hino S, Atarashi K, Onawa S, Fujimura Y, Lockett T, Clarke JM, Topping DL, Tomita M, Hori S, Ohara O, Morita T, Koseki H, Kikuchi J, Honda K, Hase K, Ohno H. Commensal microbe-derived butyrate induces the differentiation of colonic regulatory T cells. Nature. 2013;504:446-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2951] [Cited by in RCA: 3792] [Article Influence: 316.0] [Reference Citation Analysis (0)] |
| 155. | Tolhurst G, Heffron H, Lam YS, Parker HE, Habib AM, Diakogiannaki E, Cameron J, Grosse J, Reimann F, Gribble FM. Short-chain fatty acids stimulate glucagon-like peptide-1 secretion via the G-protein-coupled receptor FFAR2. Diabetes. 2012;61:364-371. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1524] [Cited by in RCA: 1635] [Article Influence: 125.8] [Reference Citation Analysis (0)] |
| 156. | Svegliati-Baroni G, Saccomanno S, Rychlicki C, Agostinelli L, De Minicis S, Candelaresi C, Faraci G, Pacetti D, Vivarelli M, Nicolini D, Garelli P, Casini A, Manco M, Mingrone G, Risaliti A, Frega GN, Benedetti A, Gastaldelli A. Glucagon-like peptide-1 receptor activation stimulates hepatic lipid oxidation and restores hepatic signalling alteration induced by a high-fat diet in nonalcoholic steatohepatitis. Liver Int. 2011;31:1285-1297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 326] [Cited by in RCA: 328] [Article Influence: 23.4] [Reference Citation Analysis (0)] |
| 157. | Zhou D, Chen YW, Zhao ZH, Yang RX, Xin FZ, Liu XL, Pan Q, Zhou H, Fan JG. Sodium butyrate reduces high-fat diet-induced non-alcoholic steatohepatitis through upregulation of hepatic GLP-1R expression. Exp Mol Med. 2018;50:1-12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 162] [Cited by in RCA: 142] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 158. | Chambers ES, Viardot A, Psichas A, Morrison DJ, Murphy KG, Zac-Varghese SE, MacDougall K, Preston T, Tedford C, Finlayson GS, Blundell JE, Bell JD, Thomas EL, Mt-Isa S, Ashby D, Gibson GR, Kolida S, Dhillo WS, Bloom SR, Morley W, Clegg S, Frost G. Effects of targeted delivery of propionate to the human colon on appetite regulation, body weight maintenance and adiposity in overweight adults. Gut. 2015;64:1744-1754. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 940] [Cited by in RCA: 957] [Article Influence: 95.7] [Reference Citation Analysis (0)] |
| 159. | Yang G, Lee HE, Lee JY. A pharmacological inhibitor of NLRP3 inflammasome prevents non-alcoholic fatty liver disease in a mouse model induced by high fat diet. Sci Rep. 2016;6:24399. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 89] [Cited by in RCA: 131] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 160. | Deng W, Meng Z, Sun A, Yang Z. Pioglitazone suppresses inflammation and fibrosis in nonalcoholic fatty liver disease by down-regulating PDGF and TIMP-2: Evidence from in vitro study. Cancer Biomark. 2017;20:411-415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 161. | European Association for the Study of the Liver (EASL). European Association for the Study of Diabetes (EASD); European Association for the Study of Obesity (EASO). EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. 2016;64:1388-1402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2290] [Cited by in RCA: 3182] [Article Influence: 353.6] [Reference Citation Analysis (4)] |
| 162. | Yokoyama H, Masaki T, Inoue I, Nakamura M, Mezaki Y, Saeki C, Oikawa T, Saruta M, Takahashi H, Ikegami M, Hano H, Ikejima K, Kojima S, Matsuura T. Histological and biochemical evaluation of transforming growth factor-β activation and its clinical significance in patients with chronic liver disease. Heliyon. 2019;5:e01231. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 163. | Hara M, Inoue I, Yamazaki Y, Kirita A, Matsuura T, Friedman SL, Rifkin DB, Kojima S. L (59) TGF-β LAP degradation products serve as a promising blood biomarker for liver fibrogenesis in mice. Fibrogenesis Tissue Repair. 2015;8:17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |