Published online Apr 28, 2020. doi: 10.3748/wjg.v26.i16.1962
Peer-review started: February 3, 2020
First decision: February 27, 2020
Revised: March 26, 2020
Accepted: April 17, 2020
Article in press: April 17, 2020
Published online: April 28, 2020
Processing time: 84 Days and 17.8 Hours
The adenoma detection rate (ADR) is inversely associated with the incidence of interval colorectal cancer and serves as a benchmark quality criterion during screening colonoscopy. However, adenoma miss rates reach up to 26% and studies have shown that a second inspection of the right colon in retroflected view (RFV) can increase ADR.
To assess whether inspection of the whole colon in RFV compared to standard forward view (SFV) can increase ADR.
Patients presenting for screening or surveillance colonoscopy were invited to participate in this randomized controlled trial and randomized into two arms. In RFV arm colonoscopy was initially performed with SFV, followed by a second inspection of the whole colon in RFV. In the SFV arm first withdrawal was performed with SFV, followed by a second inspection of the whole colon again with SFV. Number, size and morphology of polyps found during first and second inspection in each colonic segment were recorded and all polyps were removed and sent for histopathology in separate containers.
Two hundred and five patients were randomly assigned to the RFV (n = 101) and SFV (n = 104) arm. In the RFV arm, both polyp detection rate (PDR) and ADR were increased under second inspection in RFV (PDR 1st SFV: 39.8%, PDR 2nd RFV: 46.6%; ADR 1st SFV: 35.2%, ADR 2nd RFV: 42%). Likewise, in the SFV arm, PDR and ADR were increased under second inspection (PDR 1st SFV: 37.5%, PDR 2nd SFV: 46.6%; ADR 1st SFV: 34.1%, ADR 2nd SFV: 44.3%) with no significant differences in ADR and PDR between the SFV and RFV arm. Mean number of adenomas per patient (APP) was increased in the RFV and SFV (APP RFV arm: 1st SFV: 1.71; 2nd RFV: 2.38; APP SFV arm: 1st SFV: 1.83, 2nd SFV:2.2). The majority of adenomas additionally found during second inspection in RFV or in SFV were located in the transverse and left-sided colon and were > 5 mm in size.
Second inspection of the whole colon leads to increased adenoma detection with no differences between SFV and RFV. Hence, increased detection is most likely a feature of the second inspection itself but not of the inspection mode.
Core Tip: This is the first study to systematically assess the effect of an additional retrograde inspection of the whole colon on adenoma detection rate compared to a second inspection in standard forward view. Our results show that both, additional inspection of the entire colon in retroflexion as well as in forward view leads to an increased adenoma detection rate with no differences between retrograde and forward inspection. Further, the majority of adenomas additionally found during second inspection in retroflexion or in forward view were located in the transverse and left-sided colon and were > 5 mm in size. These results clearly suggest that increased adenoma detection is most likely a feature of the second inspection itself but not of the inspection mode.
- Citation: Rath T, Pfeifer L, Neufert C, Kremer A, Leppkes M, Hoffman A, Neurath MF, Zopf S. Retrograde inspection vs standard forward view for the detection of colorectal adenomas during colonoscopy: A back-to-back randomized clinical trial. World J Gastroenterol 2020; 26(16): 1962-1970
- URL: https://www.wjgnet.com/1007-9327/full/v26/i16/1962.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i16.1962
The adenoma detection rate (ADR), defined as the percentage of individuals undergoing screening colonoscopy in which at least one adenoma is found, is inversely associated with the incidence in interval colorectal cancers (CRC). In this regard, it has been shown that a 1% increase of the ADR results in a decrease of interval CRC incidence by 3%[1]. Further, as shown in prospective long-term follow-up studies, removal of adenomatous polyps during colonoscopy reduces the incidence and mortality of CRC[2,3] and large cohort studies have shown that the CRC mortality can be reduced up to 70% by screening colonoscopy[4]. Based on these considerations, ADR has been implemented as a key benchmark criterion to assess quality during screening colonoscopy in clinical practice guideline across the globe[5,6]. However, at the same time, colonic neoplasia can frequently be missed during screening colonoscopy with miss rates for adenomas reaching up to 26%, as shown in a recent meta-analysis[7]. Several factors are considered to attribute to these high miss rates, among them human error and blind spots as major factors. Among the various means to limit miss rates, simple modification of standard colonoscopy such as change of patients’ position, appliance of abdominal compression or a second inspection of the colon in either standard forward view (SFV) or retroflected view (RFV) have shown to improve ADR[8-12]. The latter has been addressed by numerous studies and although it has been shown that a second inspection in SFV or RFV can significantly increase ADR, these studies have utilized second inspection predominantly in the right sided colon.
Within this study we assessed whether additional inspection of the whole colon in retroflexion compared to a second inspection in standard forward view can increase ADR.
The study was approved by the local ethics committee (IRB No. 366_18B) and was performed in accordance with the declaration of Helsinki. The study was registered at ClinicalTrials.gov under the following ID: NCT04107376. Patients presenting for colonoscopy in the Ludwig Demling Endoscopy Center of Excellence were included in this prospective back-to-back randomized controlled trial under the following inclusion criteria: Screening or surveillance colonoscopy, colonoscopy for the work-up of abdominal pain and/or change in bowel habits. Exclusion criteria were as followed: Inflammatory bowel diseases, known polyps or referral for polypectomy, presence of coagulopathy, inadequate bowel preparation with a total Boston Bowel Preparation Score (BBPS) < 6 or the presence of a segment with a BBPS < 2. Patients with diagnosis of CRC during colonoscopy were also excluded. Prior to study inclusion written informed consent was obtained from all participating subjects, minors were excluded. Figure 1 provides an overview of the screened and studied patient cohort according to the ‘CONSORT’ statement for randomized trials[13].
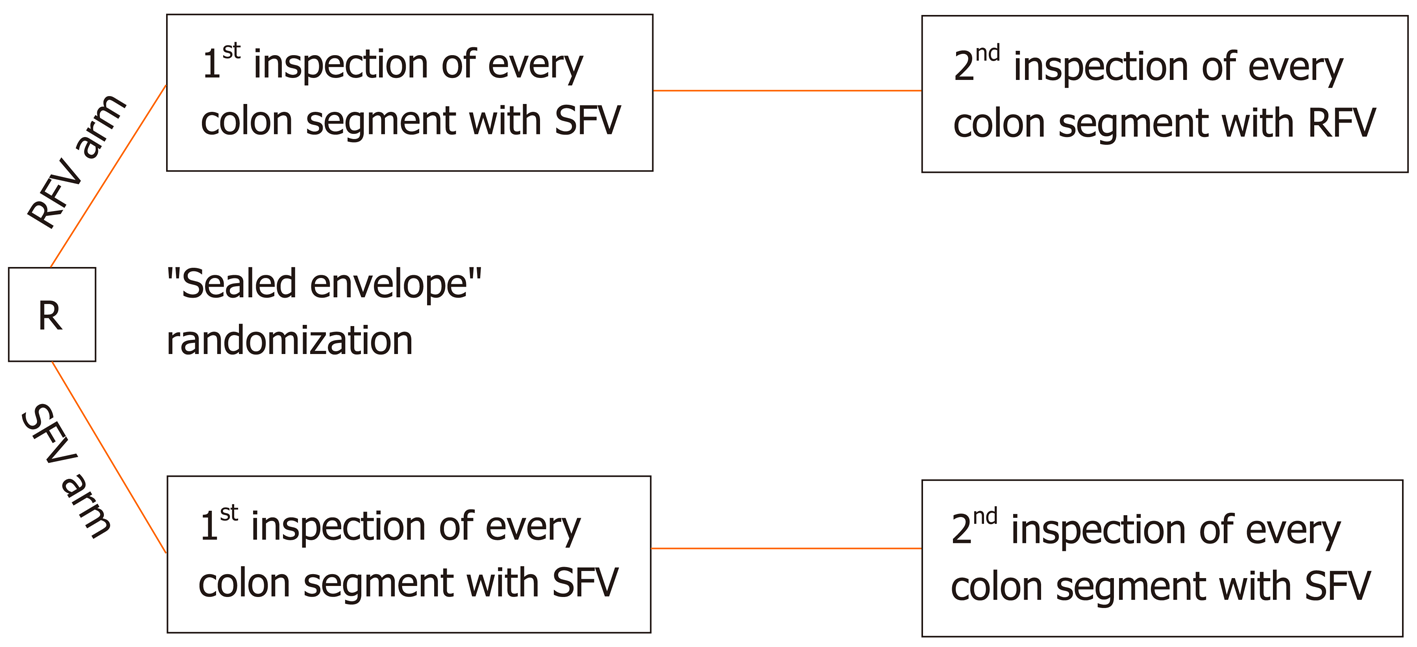
All patients received bowel preparation with low-volume PEG-based bowel lavage in a split dose regimen. On the day of endoscopy, patients were randomized using sealed envelopes into the following two arms (Figure 2): (1) RFV arm: Colonoscopy was initially performed with SFV, followed by a second inspection of the whole colon in RFV; and (2) SFV arm: Colonoscopy was initially performed with SFV, followed by a second inspection of the whole colon again with SFV. Allocation was concealed using opaque envelopes until just before initiation of the procedure. To systematically assess the influence of the inspection modality on polyp and adenoma detection within the different segments of the colon, the colon was divided into the following three segments: Caecum and ascending colon, transverse colon, descending and sigmoid colon (Figure 3). Every segment was first inspected with SFV followed by inspection of the same segment with either second SFV (SFV Arm) or in retroflexion (RFV arm) colonoscopy with first SFV. In the RFV arm a dedicated small bending HD colonoscope with an outer diameter of 11.6 mm (RetroView EC-34 i10T, Pentax Medical, Tokyo, Japan) while in the SFV arm, a regular HD colonoscope with an outer diameter of 13.2 mm was used (i10F2, Pentax Medical, Tokyo, Japan). Insertion time as well as withdrawal times in every segment under either SFV or RFV were recorded using a stop watch. During further cleaning of the colon, polyp assessment (morphology and size) and polyp removal, the stop watched was paused. Morphology of polyp and adenomas in each segment were assessed using the “Paris” criteria[14], polyp size was evaluated against an open biopsy forceps with a diameter of 7 mm. All polyps and adenomas found during colonoscopy were removed using either cold- or hot-snare polypectomy at the discretion of the endoscopist, formalin fixed in separate containers after removal and analysed by experienced gastrointestinal pathologists.
The primary endpoint was the ADR, defined as the proportion of patients with at least one adenoma. Secondary endpoints were the polyp detection rate, the mean number of adenomas per patient, the withdrawal time and the success of complete inspection of the whole colon in retroflexion.
All data are presented as mean, median, SD and range, as indicated in the respective figures and tables. Grouped continuous data were compared using the Mann–Whitney U-test. Intergroup and categorical comparisons were made using the χ2 and Fisher’s exact tests. A two-sided P < 0.05 was considered to be significant. The exact value was reported with P between 0.05 and 0.001, whereas P < 0.001 was reported for values below it. Interobserver variability in the ADR was calculated using “Kappa” statistics. The statistics were processed using the SPSS version 19 (SPSS Inc, Chicago, IL, United States).
A total of 205 patients consented to participate in the study and were randomized into the SFV arm (n = 104) and the RFV arm (n = 101). Of these, 29 patients had to be excluded due to inadequate bowel preparation (SFV arm: n = 10, RFV arm: n = 11) or the diagnosis of CRC (SFV arm: n = 5, RFV arm: n = 3) during endoscopy. Therefore, 176 patients were included in the final analysis (SFV arm: n = 88, RFV arm: n = 88). A flowchart of the patient inclusion according to the ‘CONSORT’ statement[13] is shown in Figure 1.
Baseline demographics of the patients randomized to the SFV and RFV arm showed no statistically significant differences: As shown in Table 1, in the SFV arm, 45% of patients were female (39 out of 88) with a mean age of 59.3 ± 15.1 years (range 18-86) whereas in the RFV arm, 42% of patients included for final analyses were female (37 out of 88) with a mean age of 59.9 ± 15.5 years (range 20-88). Withdrawal times showed no significant differences between the different inspection modalities in each colonic segment and in each study arm (Table 1).
| SFV arm | RFV arm | |||
| Patients, n (m/f) | 88 (39/49) | 88 (37/51) | ||
| Age, yr | ||||
| mean | 59.3 ± 15.2 | 59.9 ± 15.6 | ||
| range | 18-86 | 20-88 | ||
| Withdrawal time (min) | 1st SFV | 2nd SFV | 1st RFV | 2nd RFV |
| Cecum & ascending colon | 1:51 (1:05-2:27) | 1:47 (0:42-2:25) | 1:53 (1:27-2:17) | 1:52 (0:50-2:17) |
| Transverse colon | 1:46 (0:59-2:54) | 1:49 (1:05-2:41) | 1:50 (1:20-2:50) | 1:44 (0:30-2:49) |
| Descending & sigmoid colon | 2:36 (1:58-4:22) | 2:30 (1:00-3:41) | 2:23 (1:23-2:54) | 2:29 (1:31-2:59) |
In the RFV arm, second inspection of each colonic segment in retroflexion was possible in 86 out of 88 patients (97.7%). In one patient retroflexion in the caecum was not possible due to severe looping, in the other patient inspection of the sigmoid in retroflection was incomplete due to severe angulation. In both patients, the second examination was then performed with standard forward view.
In the RFV arm, PDR was 39.8% after the first inspection with standard forward view and increased to 46.6% after second inspection of the whole colon in retroflexion. Baseline ADR after first inspection in SFV was 35.2% in the RFV arm (Table 2). Second inspection of each colonic segment in retroflexion led to an additional detection of adenomas in six patients, which had no adenomas during first inspection with standard forward view; therefore, ADR was increased to 42% under second inspection of the colon in retroflexion (Table 2). Interobserver variability in the ADR between the six endoscopists showed substantial agreement during both, first and second withdrawal (first withdrawal: κ = 0.73, second withdrawal: κ = 0.69) in the RFV arm. Mean number of adenomas was 1.71 per patient after first inspection with standard forward view and increased to a mean of 2.38 adenomas per patient after second inspection of the colon in retroflexion in the RFV arm. Importantly, among the 35 in retroflexion additionally detected adenomas, the majority were greater than 5 mm (19/35, 54%), sessile or flat elevated (Paris Is: 18/35, 51%; Paris IIa: 15/35, 43%) and two sessile serrated adenomas (Table 3), thereby indicating that the adenomas additionally detected in retroflexion were indeed clinically relevant lesions.
| SFV arm | RFV arm | P value | |
| PDR | |||
| 1st Inspection | 33/88 = 37.5% | 35/88 = 39.8% | 0.870 |
| 2nd Inspection | 41/88 = 46.6% | 41/88 = 46.6% | 1.000 |
| ADR | |||
| 1st inspection | 30/88 = 34.1% | 31/88 = 35.2% | 1.000 |
| 2nd inspection | 39/88 = 44.3% | 37/88 = 42% | 0.8791 |
| SFV arm | RFV arm | |||
| 1st SFV | 2nd SFV | 1st SFV | 2nd RFV | |
| Adenoma size | ||||
| < 5 mm | 29 | 12 | 14 | 16 |
| 5-10 mm | 19 | 16 | 31 | 17 |
| > 10 mm | 7 | 3 | 8 | 2 |
| Adenoma localization | ||||
| Cecum and ascending colon | 18 | 9 | 21 | 11 |
| Transverse colon | 11 | 6 | 9 | 11 |
| Descending and sigmoid colon | 26 | 16 | 23 | 13 |
| Histology | ||||
| LGIEN | 53 | 27 | 48 | 33 |
| HGIEN | 1 | 2 | 2 | 0 |
| SSA wo dysplasia | 1 | 1 | 2 | 2 |
| SSA with dysplasia | 0 | 1 | 1 | 0 |
| Paris classification | ||||
| Is | 21 | 9 | 28 | 18 |
| Ip | 2 | 1 | 0 | 0 |
| IIa | 28 | 16 | 18 | 15 |
| IIb | 4 | 5 | 7 | 2 |
In the SFV arm, PDR after first inspection in SFV was 37.5% and increased to 46.6% after second inspection of the colon again in SFV. Baseline ADR after first inspection with SFV was 34.1% in the SFV arm. Second inspection of each colonic segment in SFV led to the detection of adenomas in additional nine patients in which no adenomas had been detected during first inspection with standard forward view. Thus, second inspection with standard forward view led to an increase in ADR to 44.3% in the SFV arm (Table 2). Interobserver variability in the ADR between the six endoscopists again showed substantial agreement during both, first and second withdrawal (first withdrawal: κ = 0.75, second withdrawal: κ = 0.71) in the RFV arm.
Mean adenoma per patient rate in the SFV arm was 1.83 adenomas per patient after first inspection in SFV mode and increased to a mean of 2.20 adenomas after second inspection in SFV view. Among the 31 adenomas additionally detected during second forward inspection, the majority were greater than 5 mm (19/31, 61%), sessile or flat elevated (Paris Is: 9/31, 29%; Paris IIa: 16/31, 52%). Further, histology of additionally found lesions during second SFV inspection showed two adenomas with high-grade dysplasia and two sessile serrated adenomas, one of which exhibited dysplasia (Table 3).
As summarized in a recent systematic review and meta-analysis, additional retrograde inspection of the right colon after first inspection in standard forward view is not only a safe but also effective procedure that can significantly increase ADR[15]. In this regard, it has been shown from a total of 3660 colonoscopies that standard colonoscopy with additional right-sided retroflexion compared to conventional colonoscopy alone, that a pooled per-adenoma miss rate of 17% is present in the right colon by not performing right colon retroflexion[15]. At the same time, several studies have shown that a second inspection of the right-sided colon in standard forward view can likewise increase ADR[11,16] and the increase of ADR through a second inspection of the right sided colon with a second forward inspection has been confirmed by a recent meta-analysis[17].
This has led to the theory that the increase of ADR is more likely attributable to the second inspection itself and the associated increase in withdrawal time but not a function of the mode of inspection (SFV vs RFV) during second withdrawal. Further evidence to support this comes from another recent meta-analysis comparing the diagnostic yield of a second forward view compared with retroflexion examination for the detection of right-sided adenomas[18]. As shown in this report, a second forward view and retroflexed view of the right side of the colon were both associated with improvement in ADR and importantly, when the adenoma miss rate between the second forward view and retroflexion were compared, no statistically significant difference was found[18]. In their totality, these studies suggest that the key aspect for increasing the ADR in the right sided colon is the second inspection itself but not the mode of inspection.
However, all of the above-mentioned studies were limited to studying the effects of a second inspection only in the right-sided colon. To date, data on a potential increase of ADR through second inspection of the transverse and left-sided colon and especially the comparison of a second inspection in SFV and RFV in other segments than the right colon are completely missing to date.
To fill this gap, we set off to systematically assess the effects of a second retrograde inspection of the whole colon on ADR. In order to control for the effect of second inspection itself, we designed this as a randomized back-to-back study in which in both arms, colonoscopy was initially performed with standard forward view and followed by a second inspection of the whole colon in either retroflected view (RFV arm) or a second inspection with further standard forward view (SFV arm). As shown by the withdrawal time in the two arms, inspection times were virtually identically between the different inspection modalities in each colonic segment, thereby suggesting that inspection times were well controlled and therefore most likely do not represent a significant bias for primary outcome in the two arms of our study. Our results clearly show that both, second inspection of the colon with RFV as well as second inspection SFV leads to an increase of ADR by 7% to 10% with no significant differences between second withdrawal in RFV or SFV. Therefore, these data not only corroborate the findings from similar studies in the right colon, but also extends this to the transverse and left-sided colon. Remarkably, out of 35 (RFV) and 31 (SFV) polyps additionally detected during second inspection of the whole colon, 2/3 of lesions were located in the transverse and left-sided colon, thereby clearly showing that a second inspection also of these segments is an effective procedure to further detect a substantial number of polyps. Further, as shown by the polyp characteristics, adenomas found during second inspection in either SFV or RFV were not only diminutive or small lesions, but also clinically relevant lesions such as adenomas > 10 mm, adenomas with advanced histology such as HGIEN or SSAs. In their totality, these data support the concept that second inspection of the whole colon in either retroflexion or standard forward view is an easy but effective procedure for increased detection of relevant pathology throughout the colon. Recently, it has been verified on the level of a meta-analysis that serum CrP levels are positively associated with advanced colorectal adenoma risk and subgroup and stratified analyses revealed a potential influence of smoking status and aspirin use on the association between CRP levels and colorectal adenoma risk[19]. Hence, it can be envisioned that in the future second inspection of the whole colon in either forward or retroflected view might represent an easy and effective means to increase detection of clinically relevant lesions especially in patients at risk for developing advanced adenomas as identified by Godos and co-workers[19].
At the same time, limitations of the current study also need to be addressed. Although the study was designed as a randomized controlled back-to-back study, with its setting at a single academic center, results might not be directly applicable to the community setting. However, this aspect might be mitigated by the fact that five different endoscopists performed colonoscopies in the current study. Nevertheless, it seems clear that larger multi-center studies are highly warranted to further corroborate our findings.
In summary, our study shows that second inspection of the whole colon leads to increased adenoma detection with additional and clinically relevant lesions found throughout the entire colon. Further, our results clearly show that re-inspection of the colon in retroflexion is not superior over a second examination in standard forward view, thereby suggesting that the increase in adenoma detection is most likely attributable to the second inspection itself and independent of the inspection mode. Hence, second inspection of the colon can be considered as an easy approach to increase ADR and effectiveness of screening or surveillance colonoscopy.
Due to its inverse association with the incidence of interval colorectal cancer (CRC), the adenoma detection rate (ADR) serves as a key benchmark criterion for quality assessment in screening and surveillance colonoscopy worldwide. In this regard it has been shown that a 1% increase of the ADR results in a decrease of interval CRC incidence by 3%. At the same time, colonic neoplasia can frequently be missed during screening colonoscopy with miss rates for adenomas reaching up to 26% and human error as well as blind spots are considered the major factors contributing to these high miss rates.
Among the various means to limit miss rates, simple modification of standard colonoscopy such as change of patients’ position, appliance of abdominal compression or a second inspection of the colon in either standard forward view (SFV) or retroflected view (RFV) have shown to improve ADR. The latter has been addressed by several studies and although it has been shown that a second inspection in SFV or RFV can significantly increase ADR, these studies have utilized second inspection predominantly in the right sided colon. Within this study we therefore analyzed whether additional inspection of the whole colon in RFV can increase ADR compared to an additional inspection in SFV.
In this study we aim to assess whether inspection of the whole colon in RFV compared to standard forward view SFV can increase ADR.
To address the question whether additional retrograde inspection of the whole colon can significantly increase ADR, we designed this study as prospective randomized back-to-back trial, in which patients were randomized used sealed envelopes into the following arms: (1) RFV arm: Colonoscopy was initially performed with SFV, followed by a second inspection of the whole colon in RFV; and (2) SFV arm: Colonoscopy was initially performed with SFV, followed by a second inspection of the whole colon again with SFV. Insertion time as well as withdrawal times in every segment under either SFV or RFV were recorded using a stop watch and all polyps and adenomas found were removed using either cold- or hot-snare polypectomy.
205 patients were randomly assigned to the RFV (n = 101) and SFV (n = 104) arm. In the RFV arm, both polyp detection rate (PDR) and ADR were increased under second inspection in RFV. Likewise, in the SFV arm, PDR and ADR also increased under second inspection and importantly, no significant differences in ADR and PDR between the SFV and RFV arm were found. Consistent with this, the mean number of adenomas per patient (APP) was increased in both, the RFV and SFV (APP RFV arm: 1st SFV: 1.71; 2nd RFV: 2.38; APP SFV arm: 1st SFV: 1.83, 2nd SFV: 2.2). The majority of adenomas additionally found during second inspection in RFV or in SFV were located in the transverse and left-sided colon and were > 5 mm in size.
Second inspection of the whole colon in either standard forward view or retroflected view leads to increased adenoma detection with no significant differences between these two inspections modalities. Hence, increased detection is most likely a feature of the second inspection itself but not of the inspection mode.
A second inspection of the colon in either standard forward view or retroflected view can be considered as an easy approach to increase ADR. Further large multi-center studies should assess whether this approach can increase effectiveness of screening or surveillance colonoscopy and reduce CRC mortality.
The authors gratefully acknowledge the help of the endoscopy staff at the Ludwig Demling Endoscopy Center of Excellence in conducting this study.
Manuscript source: Invited Manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Germany
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Biondi A, Slomiany BL, Uppara M S-Editor: Wang YQ L-Editor: A E-Editor: Zhang YL
| 1. | Corley DA, Jensen CD, Marks AR, Zhao WK, Lee JK, Doubeni CA, Zauber AG, de Boer J, Fireman BH, Schottinger JE, Quinn VP, Ghai NR, Levin TR, Quesenberry CP. Adenoma detection rate and risk of colorectal cancer and death. N Engl J Med. 2014;370:1298-1306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1251] [Cited by in RCA: 1553] [Article Influence: 141.2] [Reference Citation Analysis (0)] |
| 2. | Winawer SJ, Zauber AG, Ho MN, O'Brien MJ, Gottlieb LS, Sternberg SS, Waye JD, Schapiro M, Bond JH, Panish JF. Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Workgroup. N Engl J Med. 1993;329:1977-1981. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3107] [Cited by in RCA: 3120] [Article Influence: 97.5] [Reference Citation Analysis (1)] |
| 3. | Zauber AG, Winawer SJ, O'Brien MJ, Lansdorp-Vogelaar I, van Ballegooijen M, Hankey BF, Shi W, Bond JH, Schapiro M, Panish JF, Stewart ET, Waye JD. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med. 2012;366:687-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1952] [Cited by in RCA: 2278] [Article Influence: 175.2] [Reference Citation Analysis (1)] |
| 4. | Nishihara R, Wu K, Lochhead P, Morikawa T, Liao X, Qian ZR, Inamura K, Kim SA, Kuchiba A, Yamauchi M, Imamura Y, Willett WC, Rosner BA, Fuchs CS, Giovannucci E, Ogino S, Chan AT. Long-term colorectal-cancer incidence and mortality after lower endoscopy. N Engl J Med. 2013;369:1095-1105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 968] [Cited by in RCA: 1153] [Article Influence: 96.1] [Reference Citation Analysis (0)] |
| 5. | Kaminski MF, Thomas-Gibson S, Bugajski M, Bretthauer M, Rees CJ, Dekker E, Hoff G, Jover R, Suchanek S, Ferlitsch M, Anderson J, Roesch T, Hultcranz R, Racz I, Kuipers EJ, Garborg K, East JE, Rupinski M, Seip B, Bennett C, Senore C, Minozzi S, Bisschops R, Domagk D, Valori R, Spada C, Hassan C, Dinis-Ribeiro M, Rutter MD. Performance measures for lower gastrointestinal endoscopy: a European Society of Gastrointestinal Endoscopy (ESGE) Quality Improvement Initiative. Endoscopy. 2017;49:378-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 337] [Cited by in RCA: 481] [Article Influence: 60.1] [Reference Citation Analysis (0)] |
| 6. | Rex DK, Boland CR, Dominitz JA, Giardiello FM, Johnson DA, Kaltenbach T, Levin TR, Lieberman D, Robertson DJ. Colorectal Cancer Screening: Recommendations for Physicians and Patients From the U.S. Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2017;153:307-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 392] [Cited by in RCA: 512] [Article Influence: 64.0] [Reference Citation Analysis (0)] |
| 7. | Zhao S, Wang S, Pan P, Xia T, Chang X, Yang X, Guo L, Meng Q, Yang F, Qian W, Xu Z, Wang Y, Wang Z, Gu L, Wang R, Jia F, Yao J, Li Z, Bai Y. Magnitude, Risk Factors, and Factors Associated With Adenoma Miss Rate of Tandem Colonoscopy: A Systematic Review and Meta-analysis. Gastroenterology. 2019;156:1661-1674.e11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 367] [Article Influence: 61.2] [Reference Citation Analysis (0)] |
| 8. | Chandran S, Parker F, Vaughan R, Mitchell B, Fanning S, Brown G, Yu J, Efthymiou M. Right-sided adenoma detection with retroflexion versus forward-view colonoscopy. Gastrointest Endosc. 2015;81:608-613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 64] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 9. | Harrison M, Singh N, Rex DK. Impact of proximal colon retroflexion on adenoma miss rates. Am J Gastroenterol. 2004;99:519-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 116] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 10. | Hewett DG, Rex DK. Miss rate of right-sided colon examination during colonoscopy defined by retroflexion: an observational study. Gastrointest Endosc. 2011;74:246-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 126] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 11. | Kushnir VM, Oh YS, Hollander T, Chen CH, Sayuk GS, Davidson N, Mullady D, Murad FM, Sharabash NM, Ruettgers E, Dassopoulos T, Easler JJ, Gyawali CP, Edmundowicz SA, Early DS. Impact of retroflexion vs. second forward view examination of the right colon on adenoma detection: a comparison study. Am J Gastroenterol. 2015;110:415-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 82] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 12. | Lee HS, Jeon SW, Park HY, Yeo SJ. Improved detection of right colon adenomas with additional retroflexion following two forward-view examinations: a prospective study. Endoscopy. 2017;49:334-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Schulz KF, Altman DG, Moher D; CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5694] [Cited by in RCA: 6431] [Article Influence: 428.7] [Reference Citation Analysis (108)] |
| 14. | The Paris endoscopic classification of superficial neoplastic lesions: esophagus, stomach, and colon: November 30 to December 1, 2002. Gastrointest Endosc. 2003;58:S3-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1117] [Cited by in RCA: 1319] [Article Influence: 60.0] [Reference Citation Analysis (4)] |
| 15. | Cohen J, Grunwald D, Grossberg LB, Sawhney MS. The Effect of Right Colon Retroflexion on Adenoma Detection: A Systematic Review and Meta-analysis. J Clin Gastroenterol. 2017;51:818-824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 45] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 16. | Clark BT, Parikh ND, Laine L. Yield of repeat forward-view examination of the right side of the colon in screening and surveillance colonoscopy. Gastrointest Endosc. 2016;84:126-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 17. | Ai X, Qiao W, Han Z, Tan W, Bai Y, Liu S, Zhi F. Results of a second examination of the right side of the colon in screening and surveillance colonoscopy: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2018;30:181-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 18. | Desai M, Bilal M, Hamade N, Gorrepati VS, Thoguluva Chandrasekar V, Jegadeesan R, Gupta N, Bhandari P, Repici A, Hassan C, Sharma P. Increasing adenoma detection rates in the right side of the colon comparing retroflexion with a second forward view: a systematic review. Gastrointest Endosc. 2019;89:453-459.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 53] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 19. | Godos J, Biondi A, Galvano F, Basile F, Sciacca S, Giovannucci EL, Grosso G. Markers of systemic inflammation and colorectal adenoma risk: Meta-analysis of observational studies. World J Gastroenterol. 2017;23:1909-1919. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 29] [Cited by in RCA: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |